Abstract
Background
The global pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused significant morbidity and mortality, not only through devastating lung injury, but also due to multiple malfunctions in the cardiovascular system. The primary aetiology is believed to be mediated through lung alveolar injury; however, a few published reports have linked SARS-CoV-2 to significant organ dysfunction, venous thrombo-embolism, and coagulopathy. In view of the fact that the utility of tissue plasminogen activator in this population is not well studied, we present this case of rapid improvement in oxygenation after successful lytic therapy for thrombus in transit in this patient with SARS-CoV-2.
Case summary
We discuss a patient admitted with SARS-CoV-2 pneumonia. Due to the development of dramatic hypoxia, he underwent echocardiography which demonstrated extensive thrombus in transit. He received successful thrombolytic therapy with tissue plasminogen activator, with subsequent improvement in oxygenation. The patient was successfully discharged home on 2 L of oxygen via nasal cannula, and continues to improve at follow-up with his cardiologist and primary care physician.
Conclusion
This case not only highlights embolic causes of hypoxia in SARS-CoV-2, but demonstrates the important utility of an echocardiogram and tissue plasminogen activator in this population.
Keywords: SARS-CoV-2, Coronavirus, Thrombus in transit, Echocardiography, Case report
Learning points
Recognize embolic causes of hypoxia in the SARS-CoV-2 population.
Recognize the diagnostic importance of echocardiography and the potential therapeutic role of tissue plasminogen activator in the SARS-CoV-2 population.
Introduction
The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was declared a pandemic by the World Health Organization on 11 March 2020.1,2 While the majority of infected patients do not require hospitalization, those admitted to the hospital typically present with shortness of breath.3 A significant proportion of hospitalized patients develop hypoxia (27.4%), with 14.2 % requiring intensive care, and a substantial number progress to acute respiratory distress syndrome (ARDS).3 Preliminary postmortem autopsies have demonstrated deposition of fibrin in the airspaces of lung parenchyma with fibrin–platelet microthrombi in the pulmonary vasculature which may be contributing to the hypoxia.4 Although the utility of tissue plasminogen activator (TPA) for thrombus in transit in other clinical settings has previously been reported,5 the literature regarding cardiovascular events in SARS-CoV-2 remains scarce; we therefore describe the case of a 64-year-old male who presented with SARS-CoV-2 pneumonia, who was found to have extensive clot in transit on echocardiography and underwent successful lytic therapy.
Timeline
| Day | Events |
|---|---|
| 1 |
|
| 2 |
|
| 3 | Persistent sinus tachycardia was treated with metoprolol |
| 5 |
|
| 6 |
|
| 9 | Transitioned to apixaban |
| 11 | Discharged home |
Case presentation
A 64-year-old male with a history of well-controlled diabetes mellitus and hypertension presented with 10 days of cough and congestion after attending a regional conference. Despite driving to the meeting, he had multiple interactions with individuals from Italy. He visited his primary care physician, who diagnosed community-acquired pneumonia, and prescribed a 5-day course of levofloxacin 750 mg daily and prednisone 50 mg. Over the next week his symptoms did not improve, and he presented to the emergency room after battling symptoms for 17 days. His vitals on presentation demonstrated a temperature of 36.6°C, heart rate of 102 b.p.m., a respiratory rate of 20 breaths/min, and blood pressure of 126/77 mmHg. Cardiovascular exam was reported as normal; however, his lung exam demonstrated scattered rhonchi. His medications on admission were aspirin 81 mg daily, atorvastatin 20 mg daily, metformin 1000 mg b.i.d., linagliptin 5 mg daily, and isinopril 20 mg daily.
Differential diagnosis included SARS-CoV-2 pneumonia, community-acquired pneumonia, pulmonary embolism, acute heart failure exacerbation, acute coronary syndrome, myocarditis, and pericardial disease.
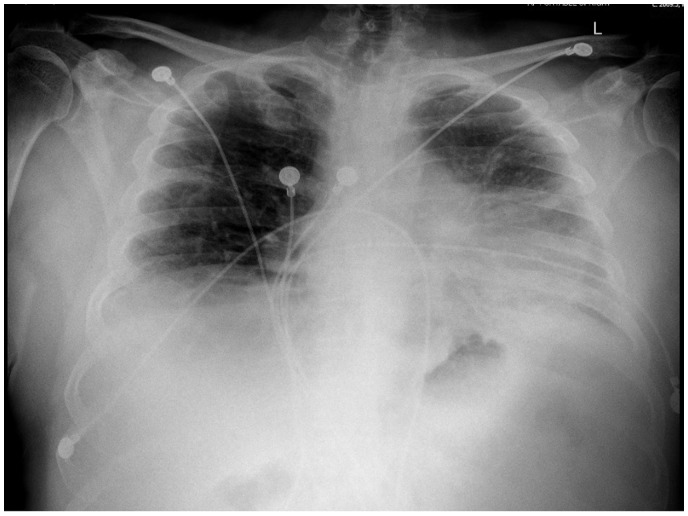
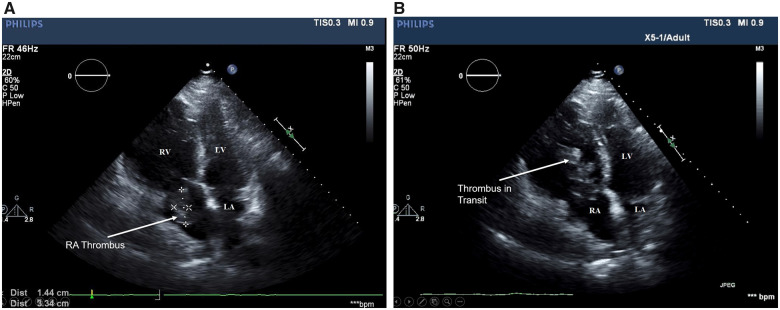
His chest radiogram (Figure 1) demonstrated bilateral opacities, left worse than right. He was given ceftriaxone 1 g every 24 h and azithromycin 500 mg once, and was admitted to the general medical ward. He was continued on his home aspirin 81 mg, atorvastatin 20 mg, and lisinopril 20 mg, in addition to being placed on an insulin lispro sliding algorithm and enoxaparin 40 mg subcutaneously daily for deep vein thrombosis prophylaxis. On hospital day 1, an infectious disease consultant recommended SARS-CoV-2 nasal swab PCR testing. The following day, his SARS-CoV-2 test returned positive and 2.5 L of O2 by nasal cannula was required for an oxygen saturation of 80% with ambulation. Azithromycin and ceftriaxone were discontinued, and he was managed with an albuterol metered dose inhaler 2.5 mg every 6 h. On hospital day 3, a persistent sinus tachycardia (110 b.p.m.) was unfortunately only treated with metoprolol tartrate 12.5 mg b.i.d. On hospital day 5, tachycardia worsened with heart rates in the 130s, hypoxia requiring 15 L by non-rebreather mask, and acute kidney injury with creatinine elevation to 1.7 from 1.1 mg/dL (normal range 0.5–1.3 mg/dL). Cardiology consultation recommended an echocardiogram and D-dimer. The echocardiogram demonstrated severe right ventricular dilation (Figure 2, Supplementary material online, Movie 1), right ventricular dysfunction, severe pulmonary hypertension, and extensive clot in transit (Figure 3A and B; Supplementarty material online, Movie 1) in the right atrium. D-dimer returned at 14 000 ng/mL (normal range <500 ng/mL). Worsening hypoxia and acute kidney injury precluded a CT pulmonary embolism scan. Thrombolytic therapy with tissue plasminogen activator (TPA) followed by a heparin drip was recommended by the Heart Team (Cardiology and Cardiothoracic surgery consultation teams). Oxygenation improved and required only a 2 L nasal cannula within 24 h. On hospital day 6, an echocardiogram demonstrated resolution of the right atrial thrombus (Figure 4, Supplementarty material online, Movie 2) with improvement in pulmonary artery pressures. On hospital day 9, he was transitioned to apixaban with a planned duration for 3–6 months. The patient was discharged home on 2 L of oxygen on hospital day 11. He followed up with his cardiologist via telephone encounter 5 days after discharge and continues to improve. His last encounter was 1 month after hospitalization with his primary care physician where his dyspnoea has improved and no longer requires oxygen by nasal cannula. He is scheduled to see vascular medicine to discuss the risk/benefit of prolonged anticoagulation.
Figure 1.
Chest radiogram showing bilateral opacities.
Figure 2.
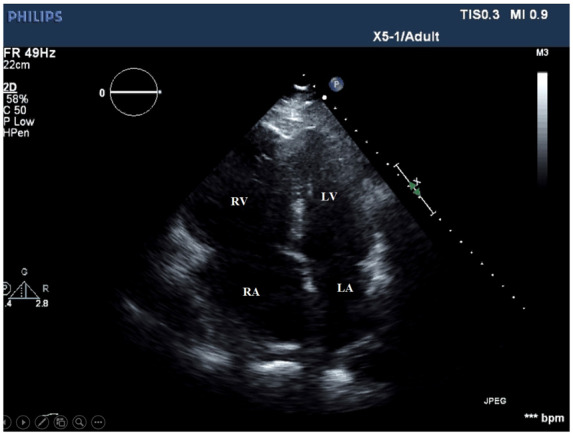
Four-chamber view showing RV and RA enlargement. RA, right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle.
Figure 3.
Four-chamber view demonstrating RA thrombus (A) and thrombus in transit (B). RA, right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle.
Figure 4.
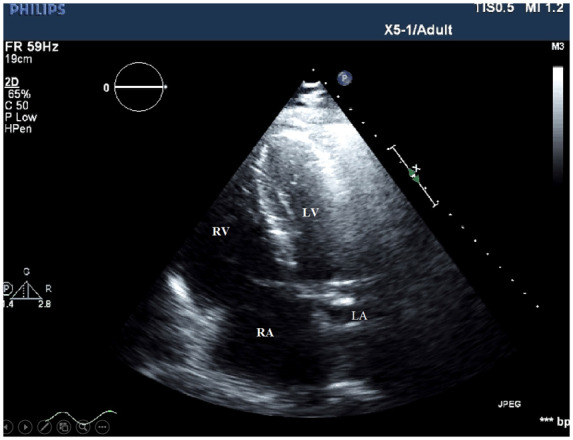
Four-chamber view following thrombolysis. RA, right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle.
Discussion
Despite a global pandemic of >2 million cases6 of SARS-CoV-2, there remains a paucity of literature on the mechanisms underpinning the high associated morbidity and mortality. Although the majority of patients suffer from hypoxia related to SARS-CoV-2 pneumonia, consideration must be given to other cardiovascular complications which may contribute to hypoxia.7 Limited reports have cited increased risk of coagulopathy and thrombo-embolism;8 therefore, obstructive embolism/microthrombi may exacerbate the severe ventilation–perfusion mismatch.9 This patient had severe right ventricular enlargement and dysfunction, severe pulmonary hypertension, and a large thrombus in transit demonstrated on echocardiography. It remains unclear whether the aetiology of the thrombus was secondary to coronavirus hypercoagulability, endothelial injury, or stasis from his previous travel, or a combination of these factors. Evolving literature has demonstrated the importance of echocardiography in determining right heart dysfunction and pulmonary hypertension in the SARS-CoV-2 population,1 which may not be from ARDS alone. Therefore, heightened awareness of thrombo-embolism in the SARS-CoV-2 population is critical. The acute and dramatic resolution of hypoxia in our patient after TPA supports the conclusion of hypoxia from embolism rather than progressive SARS-CoV-2 pneumonia. In view of the fact that the utility of TPA in this population is not well studied,10 we present this case of rapid improvement in oxygenation after successful lytic therapy for thrombus in transit in this patient with SARS-CoV-2.
Conclusion
We present this remarkable case of a 64-year-old male admitted with SARS-CoV-2 pneumonia, who was found to have extensive clot in transit on echocardiography, and underwent successful thrombolytic therapy. This case not only highlights embolic causes of hypoxia in SARS-CoV-2, but demonstrates the important diagnostic utility of an echocardiogram and the potential therapeutic role of TPA in this population.
Lead author biography

Scott Janus is originally from Chicago, Illinois. He is currently chief cardiology fellow at University Hospital Cleveland Medical Center Case Western University and serves on the ACC Ohio Fellow in Training Council. Outside of research, he enjoys spending time with his family.
Supplementary material
Supplementary material is available at European Heart Journal – Cardiovascular Imaging online.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Supplementary Material
References
- 1. Driggin E, Madhavan M V, Bikdeli B, Laracy J, Bondi-zoccai G, Tyler S, Der Nigoghossian C, Zidar DA, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA.. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) andemic. J Am Coll Cardiol 2020;75:2352–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 3. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW the Northwell COVID-19 Research Consortium Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, Coppa K, Diefenbach MA, Dominello AJ, Duer-Hefele J, Falzon L, Gitlin J, Hajizadeh N, Harvin TG, Hirschwerk DA, Kim EJ, Kozel ZM, Marrast LM, Mogavero JN, Osorio GA, Qiu M, Zanos TP.. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA 2020323:2052–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fox SE, Akmatbekov A, Harbert JL, Li G, Brown JQ.. Pulmonary and cardiac pathology in Covid-19: the first autopsy series from New Orleans. MedRxiv 2020; 10.1101/2020.04.06.20050575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vaidya G, Brown L.. To lyse or not to lyse: the dangerous right venricular thrombus. J Am Coll Cardiol 2018;71:A2463. [Google Scholar]
- 6.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report – 87. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200416-sitrep-87-covid-19.pdf?sfvrsn=9523115a_2
- 7. Xie Y, Wang X, Yang P, Zhang S.. COVID-19 complicated by acute pulmonary embolism. Radiol Cardiothorac Imaging 2020;2:e200067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cui S, Chen S, Li X, Liu S, Wang F.. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost 2020;18:1421–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, Baxter-Stoltzfus A.. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res 2020;doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK, Veress LA, Yaffe MB, Moore HB, Barrett CD.. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost 2020;doi: 10.1111/jth.14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.