(See the Major Article by Lee et al on pages e132–40.)
The unprecedented enactment of social-distancing measures in response to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic—including city lockdowns, school closures, stay-at-home orders, case isolation, quarantine of contacts, etc—was aimed at reducing the transmission of the virus and its burden on healthcare systems. Since influenza and other common respiratory pathogens share a similar mode of transmission with SARS-CoV-2, their transmission could be indirectly impacted by those measures. And while novel surveillance systems have been implemented to monitor SARS-CoV-2 activity, pre-existing surveillance systems have the advantage of allowing comparison to trends in prior years to assess the impact of social-distancing measures on the activity of influenza and other respiratory pathogens.
Syndromic surveillance is an important public health tool for the early detection, monitoring, and characterization of outbreaks and supports targeted investigations that may include detailed clinical and laboratory assessments. Syndromic surveillance is especially informative when diagnostic tests are not available, applied selectively, or difficult to implement on a broad scale. Globally, syndromic surveillance systems of influenza-like illness (ILI) are maintained to characterize the onset, circulation, and characteristics of influenza activity. These activities are typically complemented with surveillance of laboratory-confirmed detection of influenza infections. Maintained over multiple years, these surveillance systems help identify syndromic and viral activity that deviates from previous years’ patterns.
In this issue of Clinical Infectious Diseases, Hyunju Lee and colleagues describe the use of national influenza surveillance data to assess the impact of social-distancing measures, implemented in response to the SARS-CoV-2 pandemic, on seasonal influenza activity in Korea [1]. Previous reports have demonstrated that the implementation of social-distancing measures was associated with reductions in SARS-CoV-2 infections [2–4]. In this study, investigators compared the distribution of circulating influenza viruses, duration of the epidemics, patterns of ILI activity, and hospitalizations between the current 2019–2020 influenza season and previous seasons. The study shows that, during the period of enforced social distancing, the current influenza season terminated earlier than anticipated and ILI activity and influenza-related hospitalizations were reduced relative to previous seasons.
This work complements previous reports from Singapore, Hong Kong, China, Taiwan, and Japan in which the successful implementation of social-distancing measures led to reductions in SARS-CoV-2 activity and to substantial declines in influenza activity compared with prior influenza seasons [5–9]. The well-organized and determined community and public health responses in these regions and countries, including Korea, now serve as models for the pandemic response elsewhere.
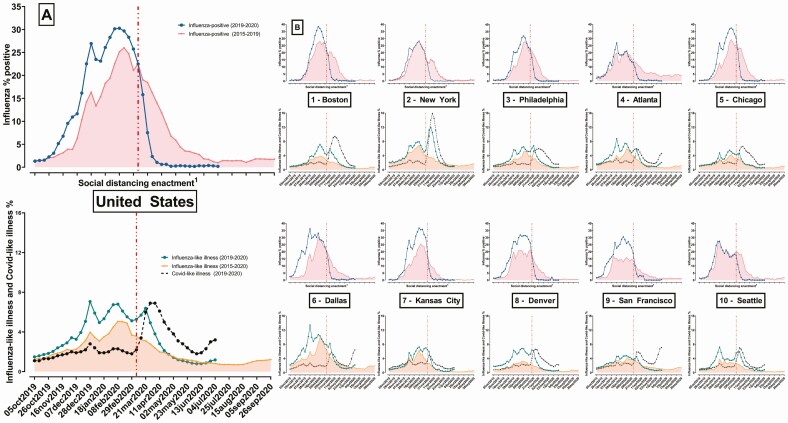
In the United States, the Centers for Disease Control and Prevention conducts surveillance of influenza and other respiratory infections. Publicly available viral and syndromic surveillance data can be used to examine the impact of social-distancing measures and compute (1) the weekly percentage of total respiratory specimens that test positive for influenza type A and B, (2) the weekly percentage of visits among outpatient providers with evidence of fever with either a cough or sore throat (ILI), and (3) the weekly percentage of emergency department visits with evidence of a coronavirus diagnosis code or fever with either of the following: cough, shortness of breath, or difficulty breathing (coronavirus disease 2019 [COVID-19]–like illness [CLI]) [10]. Prior to enactment of social-distancing measures, the median weekly percentage of influenza positive specimens was elevated in 2019–2020 (Figure 1A) relative to weekly median historic levels nationally (2015–2019) and in 8 human health services (HHS) regions (Figure 1B). After social-distancing implementation, the percentage was substantially lower than historical levels nationally and in every region (Figure 1B). The percentage of encounters with ILI was elevated relative to historical levels nationally and in every region prior to social-distancing enactment. However, since social-distancing enactment (as of 4 July 2020), the national ILI level returned to historical levels, although following the recent relaxation of social distancing measures ILI started increasing again in certain regions, including the Atlanta, Dallas, Kansas City, and Seattle regions (Figure 1B). For the more specific COVID-19–related syndromic surveillance, the percentage of encounters with CLI did not increase substantially until March (Figure 1). Similar to ILI, COVID-19–like illnesses had declined following enactment of social distancing, although the decline lagged relative to the observed ILI decline. CLI activity also started increasing in several regions during the last weeks.
Figure 1.
A, National current weekly percentage of influenza-positive respiratory specimens and ILI- and CLI-related outpatient encounters in the United States (2015–2020). B, Regional current and historical weekly percentage of influenza-positive respiratory specimens and ILI- and CLI-related outpatient encounters in the United States (2015–2020). Notes: Influenza positive (blue solid lines), ILI (green solid lines), and CLI (black dashed lines) (2019–2020): the value for each week during the 2019–2020 viral respiratory season. Influenza-positive (red solid lines), ILI (orange solid lines) (2015–2019): the median value for each week in the prior 4 influenza seasons (2015–2019). Surveillance data sources: Laboratory-confirmed influenza compiled from NREVSS and WHO Collaborating Laboratory surveillance data, ILI compiled from ILInet, and CLI compiled from the National Syndromic Surveillance Program. Regions: Defined based on the US Health and Human Services regions: 1-Boston—Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont; 2-New York—New Jersey, New York, Puerto Rico, Virgin Islands; 3-Philadelphia—Delaware, Washinton DC, Maryland, Pennsylvania, Virginia, West Virginia; 4-Atlanta—Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, Tennessee; 5-Chicago—Illinois, Indiana, Michigan, Minnesota, Ohio, Wisconsin; 6-Dallas—Arkansas, Louisiana, New Mexico, Oklahoma, Texas; 7-Kansas City—Iowa, Kansas, Missouri, Nebraska; 8-Denver—Colorado, Montana, North Dakota, South Dakota, Utah, Wyoming; 9-San Francisco—Arizona, California, Hawaii, Nevada, American Samoa, Commonwealth of the Northern Mariana Islands, Federated States of Micronesia, Guam, Marshall Islands, and Republic of Palau; 10-Seattle—Alaska, Idaho, Oregon, Washington. 1Social distancing enactment: The period before the enactment of social distancing at the regional level was measured as the time prior to and including the week of the first statewide school closure or mass gathering restriction for each region. Abbreviations: CLI, Covid-like illness; Covid, coronavirus disease; ILI, influenza-like illness; WHO, World Health Organization.
Although there are differences in the design and adoption of social-distancing measures across settings and populations, the consistency of the observed impact on the transmission of influenza, SARS-CoV-2, and likely other respiratory pathogens seems evident and intuitive. While many social-distancing measures are very disruptive and difficult to sustain, Lee and colleagues’ work underscores that basic principles of self-protection against respiratory infections, such as hand hygiene and cough etiquette, recommendations for persons with respiratory symptoms to stay at home until symptoms subside, and use of masks or cloth face covering in all cases of close person-to-person contact, rapidly adopted in response to the pandemic are becoming part of our lifestyle as we adapt to a “new normal.” The wide adoption and practice of these recommendations could lead to a new paradigm for the activity of SARS-CoV-2 and other respiratory infections in the near future, with lower activity compared with historical records. As we reflect on the suffering inflicted by the ongoing pandemic and we contemplate the relaxation of harsh social-distancing measures, the value of these simple, scalable, inexpensive common-sense measures may be the lesson that we all need to learn and adopt.
While surveillance data are helpful to identify abnormal activity of certain diseases of public health interest, and to demonstrate the impact of major interventions, such as implementation of social-distancing measures, it is important to understand the limitations and strengths of specific surveillance systems. Monitoring a new disease that rapidly reaches pandemic proportions is difficult for surveillance systems that rely on patients presenting to healthcare settings and getting tested. Due to fear or other reasons, patients may avoid or delay healthcare encounters unless strictly necessary, and changes in testing practices could also affect the data captured by surveillance systems. Complementing laboratory-based surveillance with syndromic surveillance data is helpful, but additional research is necessary to clarify and characterize the general healthcare utilization patterns during the pandemic.
In Korea, the United States, and most other settings, several social-distancing measures were implemented in rapid sequence, making it difficult to isolate the impact of specific measures due to their temporal and regional aggregation. Although the described comparisons are ecologic in nature, the population-level assessment of the impact of these broad recommendations may be more relevant than individual-level evaluations. Finally, it is important to understand that there may be substantive surveillance variation over time and across regions (Figure 1), and thus national figures may not represent the local or regional situation.
Looking beyond influenza, these surveillance systems will be important in different regions and countries as they initiate or continue relaxing social-distancing requirements. In the United States, a 2-week downward trend in ILI and CLI activity was recommended as 1 indicator for reopening [11]. Despite declines following social distancing, CLI activity levels remained substantially elevated or started increasing in certain regions through the beginning of July 2020, suggesting that high activity levels could rapidly resume once distancing measures are removed. In contrast with the abrupt interruption of influenza activity, the lag time between social-distancing enactment and declines in CLI activity in certain regions highlights the differential SARS-CoV-2 transmission patterns relative to influenza. This delayed impact requires careful attention by policy makers considering the removal and subsequent reenactment of social-distancing measures.
Influenza and syndromic surveillance data suggest that widespread social-distancing measures were effective at reducing influenza and SARS-CoV-2 activity in Korea and elsewhere. These surveillance data will remain important for monitoring the pandemic as social-distancing measures are relaxed.
Notes
Financial support. A. D. W. was supported in part by a PhRMA Foundation Fellowship award and the Vanderbilt Faculty Research Scholars Program. J. E. received consulting fees from the Office of the National Coordinator for Health Information Technology. C. G. G. was supported in part by the National Institutes of Health (National Institute of Allergy and Infectious Diseases [NIAID] grant number K24AI148459). C. G. G. has received consulting fees from Pfizer, Sanofi, and Merck and received research support from Sanofi-Pasteur, Campbell Alliance, the Centers for Disease Control and Prevention, the National Institutes of Health, the Food and Drug Administration, and the Agency for Healthcare Research and Quality.
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. Lee H, Lee H, Song K-H, et al. Impact of Public Health Interventions on Seasonal Influenza Activity During the SARS-CoV-2 Outbreak in Korea. Clinical Infectious Diseases. 2021; 72:e132–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev 2020; 4:CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China [manuscript published online ahead of print 4 May 2020]. Nature 2020. doi: 10.1038/s41586-020-2293-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Matrajt L, Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg Infect Dis 2020; 26. doi: 10.3201/eid2608.201093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Roy Jiunn Jye S, Calvin JC, Stefan M, Rachael P, Vernon L. Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg Infect Dis 2020; 26. doi: 10.3201/eid2608.201229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sakamoto H, Ishikane M, Ueda P. Seasonal influenza activity during the SARS-CoV-2 outbreak in Japan. JAMA 2020; 323:1969–71. doi: 10.1001/jama.2020.6173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shu-Chen K, Shu-Man S, Li-Hsin C, Chao AH. Collateral benefit of COVID-19 control measures on influenza activity, Taiwan. Emerg Infect Dis 2020; 26: 10.3201/eid2608.201192. doi: 10.3201/eid2608.201192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sun J, Shi Z, Xu H. Non-pharmaceutical interventions used for COVID-19 had a major impact on reducing influenza in China in 2020 [manuscript published online ahead of print 24 April 2013]. J Travel Med 2020; taaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health 2020; 5:e279–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Surveillance data from: (1) NREVSS and WHO Collaborating Laboratories; (2) US Outpatient Influenza-like Illness Surveillance Network (ILInet); (3) US National Syndromic Surveillance Program. CDC. CDC Influenza Tracker and Syndromic Surveillance. Published 2020. Available at: https://www.cdc.gov/flu/weekly/fluactivitysurv.htm. Accessed 10 July 2020.
- 11. Guidelines: opening up America again. White House; 2020. Available at: https://www.whitehouse.gov/openingamerica/. Accessed 5 July 2020. [Google Scholar]