Abstract
Background
Descriptions of coronavirus disease 2019 (COVID-19) have focused on the nonpregnant adult population. This study aims to describe the clinical characteristics and perinatal outcomes of COVID-19 in pregnancy.
Methods
We searched databases from December 2019 to 30 April 2020. Eligible studies reported clinical characteristics, radiological findings, and/or laboratory testing of pregnant women during infection. Data were pooled across studies using a random-effects model.
Results
Twenty-four studies (136 women) were included. The most common symptoms were fever (62.9%) and cough (36.8%). Laboratory findings included elevated C-reactive protein (57%) and lymphocytopenia (50%). Ground-glass opacity was the most common radiological finding (81.7%). Preterm birth rate was 37.7% and cesarean delivery rate was 76%. There was 1 maternal death. There were 2 fetal COVID-19 cases.
Conclusions
The clinical picture in pregnant women with COVID-19 did not differ from the nonpregnant population; however, the rate of preterm birth and cesarean delivery are considerably higher than international averages.
Keywords: coronavirus, pregnant, neonates, transmission
Clinical presentation and outcomes in pregnant women with COVID-19 were similar to the general population. There is a lack of evidence to support transmission from patient to fetus. More studies are needed to examine the effect of COVID-19 on pregnant women.
In December 2019, a virus of unknown origin was detected in Wuhan, China, and causing a cluster of pneumonia cases [1]. Shortly thereafter, the virus was classified as part of the novel enveloped RNA betacoronavirus family [2] and named the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); its associated disease is called coronavirus disease 2019 (COVID-19). The World Health Organization has recently declared COVID-19 as a pandemic [3]. As of 22 June 2020, >8 million confirmed cases had been documented globally with >400 000 deaths [4].
Many studies have reported the clinical characteristics, laboratory findings, and radiological imaging associated with COVID-19 in both the nonpregnant adult and pediatric populations. Clinical characteristics are quite similar in adults and children; the most common symptoms include fever and cough, usually dry [5–9]. Laboratory findings also appear to be similar, with lymphopenia and elevated C-reactive protein being the most common findings [5–9]. In addition, more than half of adults and children demonstrate ground-glass opacity on computed tomography (CT) of the chest [5–9].
Pregnancy poses a unique situation where the management of an affected patient is influenced by 2 patients: the mother and her fetus. Additionally, the normal pregnancy adaptations of the immune system pregnancy may theoretically cause clinical dilemmas and remains poorly understood. There is an urgent need for certain questions to be addressed: Do pregnant patients have similar clinical presentations, and are they more likely to experience adverse maternofetal or obstetrical outcomes? Understanding the clinical course of COVID-19 in the pregnant population is imperative for health providers to be able to care for the mother and her unborn fetus in a standardized way. This study aims to describe the clinical characteristics, laboratory abnormalities, radiological findings, and outcomes of pregnancy during COVID-19 to aid practitioners in managing these unique patients. To our knowledge, this is the largest systematic review and meta-analysis of its kind in pregnancy.
METHODS
Search Strategy and Data Sources
A comprehensive search of several databases from 1 December 2019 to 30 April 2020 was conducted and limited to English-language publications. The databases included Ovid Medline and Epub Ahead of Print, In-Process and Other Non-Indexed Citations; Ovid Embase; Ovid Cochrane Central Register of Controlled Trials; and Scopus. The search strategy was conducted by a medical reference librarian. Controlled vocabulary supplemented with keywords was used to search for SARS-CoV-2 infection and pregnancy. The search strategy and terms used are available in Supplementary Item 1.
Eligibility Criteria and Quality Assessment
Eligible studies had to meet all of the following inclusion criteria: (1) participants must be women who were pregnant; (2) reverse-transcription polymerase chain reaction (RT-PCR)–confirmed COVID-19 infection through throat or nasal swabs; and (3) report of neonatal outcomes. The quality of each study was independently evaluated by 2 authors (R. M. and N. M.) using the methodological quality and synthesis of case series and case reports described by Murad et al [10]. This article followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Statistical Analysis
Means of continuous variables and rates of binary variables were pooled using the random-effects model, and the generic inverse variance method of DerSimonian and Laird [11]. Proportions underwent logit transformation prior to meta-analysis. The heterogeneity of effect size estimates across the studies was quantified using the Q statistic and the I2 index (P < .10 was considered significant). A value of I2 of 0–25% indicates minimal heterogeneity, 26%–50% moderate heterogeneity, and 51%–100% substantial heterogeneity [12]. Data analysis was performed using Open Meta analyst software (CEBM, Brown University, Providence, Rhode Island).
RESULTS
Study Selection and Characteristics
The initial search yielded 1082 potentially relevant articles from which 24 unique studies involving 136 pregnant women met eligibility criteria [13–36]. Details of the study selection process are depicted in Supplementary Item 2. The baseline characteristics of the included studies are described in Table 1. The maternal age ranged from 25 to 34 years, and the gestational age at admission ranged from 30 to 40 weeks.
Table 1.
Baseline Characteristics of Included Studies
| Author, Year | Country | Study Design | No. of Subjects | Mean Age, y | Mean Gestational Age on Admission, wk |
|---|---|---|---|---|---|
| Chen et al, 2020 [13] | China | RC | 9 | 29.89 | 37.11 |
| Chen et al, 2020 [14] | China | RC | 17 | 29.1 | NA |
| Liu et al, 2020 [15] | China | RC | 10 | 29.69 | 33.85 |
| Wang et al, 2020 [16] | China | Case report | 1 | 34 | 40 |
| Wang et al, 2020 [17] | China | Case report | 1 | 28 | 30 |
| Zhu et al, 2020 [18] | China | RC | 9 | 30.89 | NA |
| Liu et al, 2020 [19] | China | Case series | 3 | 32.67 | NA |
| Iqbal et al, 2020 [20] | United States | Case report | 1 | 34 | 39 |
| Chen et al, 2020 [21] | China | RC | 5 | 28.8 | NA |
| Chen et al, 2020 [22] | China | Case series | 4 | 29 | NA |
| Dong et al, 2020 [23] | China | Case report | 1 | 29 | 34 |
| Fan et al, 2020 [24] | China | Case series | 2 | 31.5 | 36.5 |
| Karami et al, 2020a [25] | Iran | Case report | 1 | 27 | 30 |
| Khan et al, 2020 [26] | China | Case series | 3 | 29.33 | 37 |
| Lee et al, 2020 [27] | Republic of Korea | Case report | 1 | 28 | 36 |
| Li et al, 2020 [28] | China | Case-control study | 16 | 30.9 | 35.5 |
| Liu et al, 2020 [29] | China | RC | 11 | 32 | 37 |
| Yu et al, 2020 [30] | China | RC | 7 | 32.14 | 39 |
| Peng et al, 2020 [31] | China | Case report | 1 | 25 | NA |
| Wu et al, 2020 [32] | China | RC | 23 | 29 | 33 |
| Xiong et al, 2020 [33] | China | Case report | 1 | 25 | 33 |
| Yang et al, 2020 [34] | China | PC | 7 | NA | NA |
| Zambrano et al, 2020 [35] | Honduras | Case report | 1 | 41 | 31 |
| Li et al, 2020 [36] | China | Case report | 1 | 30 | 35 |
Abbreviations: NA, not available; PC, prospective cohort study; RC, retrospective cohort study.
aStudy retracted.
Risk of Bias
Results of the quality assessment of all included studies are shown in Table 2. All of the case series were judged to have good quality. The patients appeared to represent the whole experience of the investigator, the exposure and outcome were adequately ascertained, and the length of follow-up was adequate.
Table 2.
Methodological Quality Assessment Tool Results
| Author, Year | Question 1 | Question 2 | Question 3 | Question 4 | Question 5 |
|---|---|---|---|---|---|
| Chen et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Chen et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Liu et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Wang et al, 2020 | Yes | Yes | Yes | No | No |
| Wang et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Zhu et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Liu et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Iqbal et al, 2020 | Yes | Yes | Yes | Yes | No |
| Chen et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Chen et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Dong et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Fan et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Karami et al, 2020a | Yes | Yes | Yes | Yes | Yes |
| Khan et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Lee et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Li et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Liu et al, 2020 | Yes | Yes | Yes | No | No |
| Yu et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Peng et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Wu et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Xiong et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Yang et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Zambrano et al, 2020 | Yes | Yes | Yes | Yes | Yes |
| Li et al, 2020 | Yes | Yes | Yes | Yes | Yes |
Question 1: Does the patient(s) represent(s) the whole experience of the investigator (center)?
Question 2: Was the exposure adequately ascertained?
Question 3: Was the outcome adequately ascertained?
Question 4: Was follow-up long enough for outcomes to occur?
Question 5: Is the case(s) described with sufficient detail to allow other investigators to replicate the research or to allow practitioners make inferences related to their own practice?
aStudy retracted.
Clinical Characteristics
The demographic and clinical characteristics of the patients are described in Table 3. All patients were hospitalized during the course of delivery and treatment. Sixty-two patients were residents of Wuhan, China. Among the patients who lived in Wuhan, all had a community exposure, defined as being located within a setting with a known outbreak, and only 1 woman had direct contact with a known infected person. Fever was the most common presenting symptom, seen in 62.9% (95% confidence interval [CI], .477–.759; I2 = 47.24%) on admission, followed by cough in 36.8% of patients (95% CI, .253–.500; I2 = 29.31%), and sore throat in 22.6% (95% CI, .078–.502; I2 = 27.92%). Less frequently reported symptoms included dyspnea (15.7% [95% CI, .067–.328]; I2 = 23.46%) and diarrhea (15.6% [95% CI, .075–.295]; I2 = 0%]) (Figure 1). Overall, 19.7% had at least 1 coexisting illness; frequently reported illnesses included hypothyroidism, hepatitis B virus infection, hypertension, gestational diabetes, autoimmune disease, and chronic obstructive pulmonary disease.
Table 3.
Demographics and Clinical Characteristics of Included Patients
| Author, Year | Exposure to the Environment (Unknown Contact) | Direct Contact With Infected People | Fever | Dry Cough | Sore Throat | Dyspnea | Myalgia | Diarrhea |
|---|---|---|---|---|---|---|---|---|
| Chen et al, 2020 [13] | Yes (4) | Yes (5) | 7 | 4 | 2 | 1 | 3 | 1 |
| Chen et al, 2020 [14] | NA | 3 | 4 | 4 | NA | 1 | NA | 1 |
| Liu et al, 2020 [15] | Yes (10) | 6 | 10 | 1 | NA | 1 | NA | NA |
| Wang et al, 2020 [16] | Yes (1) | No | 1 | NA | NA | NA | NA | NA |
| Wang et al, 2020 [17] | Yes (1) | Yes | 1 | NA | NA | NA | NA | NA |
| Zhu et al, 2020 [18] | NA | NA | 8 | 1 | NA | NA | NA | NA |
| Liu et al, 2020 [19] | Yes (3) | No | 2 | 2 | NA | NA | NA | NA |
| Iqbal et al, 2020 [20] | No | No | 1 | 1 | NA | NA | 1 | NA |
| Chen et al, 2020 [21] | NA | NA | 0 | 2 | NA | NA | NA | NA |
| Chen et al, 2020 [22] | NA | NA | 3 | 2 | NA | 1 | 2 | NA |
| Dong et al, 2020 [23] | Yes | No | 1 | NA | 1 | NA | NA | NA |
| Fan et al, 2020 [24] | No | Yes (2) | 2 | NA | NA | NA | NA | NA |
| Karami et al, 2020a [24] | NA | NA | 1 | 1 | NA | NA | 1 | NA |
| Khan et al, 2020 [26] | NA | NA | 2 | 3 | 1 | NA | NA | NA |
| Lee et al, 2020 [27] | NA | NA | 1 | 1 | 0 | NA | NA | NA |
| Li et al, 2020 [28] | NA | NA | 4 | 0 | 1 | 0 | NA | NA |
| Liu et al, 2020 [29] | NA | NA | 9 | 6 | NA | NA | 3 | 3 |
| Yu et al, 2020 [30] | Yes (7) | No | 6 | 1 | NA | 1 | NA | 1 |
| Peng et al, 2020 [31] | NA | NA | 1 | NA | NA | 1 | NA | NA |
| Wu et al, 2020 [32] | No | Yes (3) | 4 | 6 | NA | NA | NA | NA |
| Xiong et al, 2020 [33] | Yes (1) | No | 1 | 1 | NA | NA | NA | NA |
| Yang et al, 2020 [34] | Yes (7) | No | 5 | 1 | NA | NA | NA | 1 |
| Zambrano et al, 2020 [35] | No | Yes (1) | 1 | 1 | NA | NA | 1 | NA |
| Li et al, 2020 [36] | Yes | Yes (1) | 0 | 1 | NA | 1 | NA | NA |
Abbreviation: NA, not available.
aStudy retracted.
Figure 1.
Forest plot of the clinical characteristics present at time of admission. Abbreviations: CI, confidence interval; Ev, xxx; Trt, xxx.
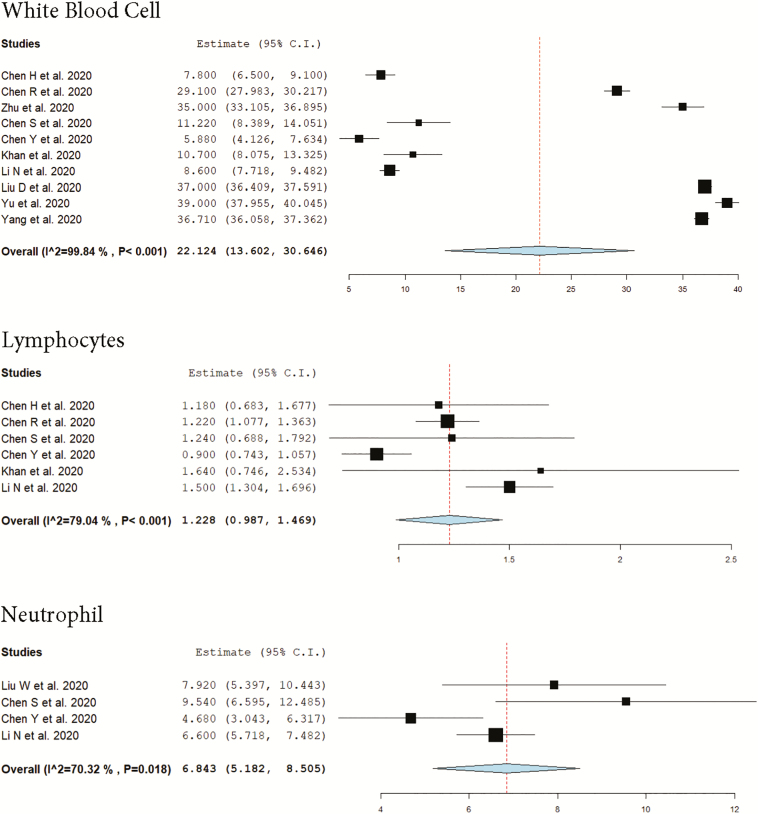
Laboratory and Radiological Findings
Table 4 describes the laboratory and radiologic findings on admission. The mean lymphocyte count was 1.233 × 109 cells/L (95% CI, .991–1.475; I2 = 76.09%). The pooled mean leukocyte count was 10.438 × 109 cells/L (95% CI, 8.744–12.132; I2 = 0%). Lymphocytopenia was present in 36 patients, with a pooled proportion of 50% (95% CI, .331–.669; I2 = 39.44%), and no cases of leukopenia were identified. However, elevated neutrophil levels were reported in 67.8% of the patients (95% CI, .478–.829; I2 = 0%). More than half of the patients had elevated levels of C-reactive protein, with a pooled proportion of 57% (95% CI, .454–.678; I2 = 0%), which ranged from 2.975 to 32.28 mg/L; less commonly encountered were elevations in the levels of alanine aminotransferase (ALT) (22.3% [95% CI, .123–.369]; I2 = 0%), aspartate aminotransferase (AST) (23.3% [95% CI, .128–.386]; I2 = 0%), and a D-dimer ratio that ranged between 840 and 1710 μg/L. The mean level of ALT was 48.345 U/L (95% CI, –3.293 to 99.984; I2 = 99.94%), while the mean AST level was 34.114 U/L (95% CI, 22.972–45.256; I2 = 95.53%) (Figure 2).
Table 4.
Radiologic and Laboratory Findings on Admission
| Author, Year | GGO, No. | Infiltrated Shadows, No. | Subpleural, No. | Lymphocytes, ×109/L | Neutrophils, ×109/L | Leukocytosis, ×109/L | CRP, mg/L | ALT, U/L | AST, U/L |
|---|---|---|---|---|---|---|---|---|---|
| Chen et al, 2020 [13] | 6 | 1 | 1 | 1.18 | NA | NA | 18.61 | 253.78 | 171 |
| Chen et al, 2020 [14] | NA | NA | NA | 1.22 | NA | 10.9 | 27.2 | 20.6 | 23.4 |
| Liu et al, 2020 [15] | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Wang et al, 2020 [16] | 1 | NA | NA | 0.97 | 9.97 | NA | 11.5 | NA | NA |
| Wang et al, 2020 [17] | 1 | NA | NA | 0.86 | 9.14 | 10.6 | 19.6 | NA | NA |
| Zhu et al, 2020 [18] | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Liu et al, 2020 [19] | 3 | NA | NA | 4.87 | 7.92 | 9.92 | 13.1 | 9.83 | 20.6 |
| Iqbal et al, 2020 [20] | 1 | NA | NA | 1.1 | 8.8 | NA | 25.6 | 23 | 24 |
| Chen et al, 2020 [21] | 5 | NA | NA | 1.24 | 9.54 | NA | 32.28 | 10.26 | 20.22 |
| Chen et al, 2020 [22] | 4 | NA | NA | 0.9 | 4.68 | NA | 26.75 | 21.75 | 26.5 |
| Dong et al, 2020 [23] | 1 | NA | NA | 1.08 | 6.57 | NA | 57 | 40 | 38 |
| Fan et al, 2020 [24] | 1 | 1 | NA | NA | NA | NA | NA | NA | NA |
| Karami et al, 2020a [25] | 1 | NA | NA | 0.72 | NA | 3 | 31 | 68 | 52 |
| Khan et al, 2020 [26] | 3 | NA | NA | 1.64 | NA | NA | 17.3 | 10.67 | 23.33 |
| Lee et al, 2020 [27] | 1 | NA | NA | NA | NA | NA | 1.5 | NA | NA |
| Li et al, 2020 [28] | 16 | NA | NA | 1.5 | 6.6 | NA | 4.8 | 11.6 | 16.3 |
| Liu et al, 2020 [29] | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Yu et al, 2020 [30] | 7 | NA | NA | NA | NA | NA | 31.79 | NA | NA |
| Peng et al, 2020 [31] | 1 | NA | NA | NA | NA | NA | NA | NA | NA |
| Wu et al, 2020 [32] | 23 | NA | NA | NA | NA | NA | 2.975 | NA | NA |
| Xiong et al, 2020 [33] | 0 | 1 | NA | 1.91 | NA | NA | 21.8 | 15 | 21 |
| Yang et al, 2020 [34] | 7 | NA | NA | NA | NA | NA | NA | NA | NA |
| Zambrano et al, 2020 [35] | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Li et al, 2020 [36] | NA | 1 | NA | 1.1 | 7.1 | 8.7 | 18.59 | 15 | 19 |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, C-reactive protein; GGO, ground glass opacity; NA, not available.
aStudy retracted.
Figure 2.
Forest plot of the laboratory findings present at time of admission. Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CI, confidence interval.
Of 136 chest CT scans performed at the time of admission, 98% revealed abnormal results. The most common pattern seen on chest CT scan was ground-glass opacity (GGO) and was present in 81.7% of patients (95% CI, .701–.895; I2 = 0%). Of the 82 patients who presented with GGO, 52 patients presented with bilateral GGO and 10 patients presented with unilateral GGO. There were no specific data regarding the classification of the location of the GGO in the 20 remaining patients. The second most common pattern on chest CT was infiltrated shadows, seen in 42.5% (95% CI, .126–.791; I2 = 29.55%) (Figure 3).
Figure 3.
Forest plot of the radiological findings present at time of admission. Abbreviations: CI, confidence interval; Ev, xxx; Trt, xxx.
Treatments Provided and Maternal Outcomes
Most patients were delivered via a cesarean delivery with a rate of 76.3% (95% CI, .658–.842; I2 = 10.24%). Fifty-nine patients received antibiotic therapy (87.7% [95% CI, .755–.943]; I2 = 0%) and 45 patients received antiviral therapy (67.5% [95% CI, .484–.821]; I2 = 33.44%). Details of antiviral therapy are provided in Table 5. Oxygen therapy, either through nasal cannula or face mask, was administered in 36 patients (73.1% [95% CI, .391–.920]; I2 = 57.64%) (Table 5). Fifteen patients received corticosteroids (50.5% [95% CI, .285–.723]; I2 = 30.81%), of which 5 patients received betamethasone. Specific indication for use of corticosteroid administration included fetal lung maturation, acute flare of autoimmune disease, prophylaxis for pneumonia, pneumonia, and to relieve inflammation. Two patients required intubation and mechanical ventilation due to multiorgan failure. One woman died due to multiorgan failure and acute respiratory distress syndrome (ARDS) (mortality, 11.1% [95% CI, .063–.187]; I2 = 0%). As shown in Table 5, premature rupture of membrane, fetal distress, and stillbirth were the most common complications during pregnancy.
Table 5.
Treatments and Pregnancy-related Complications
| Author, Year | Cesarean Delivery, No. | Antiviral Therapy, No. | Specific Antiviral Medications | Antibiotic Therapy, No. | Oxygen Therapy, No. | Mechanical Ventilation, No. | Premature Membrane Rupture, No. | Fetal Distress, No. | Stillbirth, No. |
|---|---|---|---|---|---|---|---|---|---|
| Chen et al, 2020 [13] | 9 | 6 | NA | 9 | 9 | 0 | 2 | 2 | 0 |
| Chen et al, 2020 [14] | 17 | NA | NA | NA | NA | 0 | NA | NA | NA |
| Liu et al, 2020 [15] | 10 | NA | NA | NA | NA | 1 | 1 | 3 | 1 |
| Wang et al, 2020 [16] | 1 | 1 | Recombinant human IFN | NA | NA | 0 | 0 | 0 | 0 |
| Wang et al, 2020 [17] | 1 | 1 | Lopinavir and ritonavir | NA | NA | 0 | 0 | 0 | 1 |
| Zhu et al, 2020 [18] | 7 | 5 | Oral oseltamivir | NA | NA | 0 | 3 | 0 | 0 |
| Liu et al, 2020 [19] | 2 | 3 | Arbidol (n = 2) Atomized inhalation of IFN (n = 1) | 2 | 3 | 0 | 0 | 0 | 0 |
| Iqbal et al, 2020 [20] | 0 | NA | NA | NA | NA | 0 | 0 | 0 | 0 |
| Chen et al, 2020 [21] | 2 | 0 | NA | 5 | 0 | 0 | 0 | 0 | 0 |
| Chen et al, 2020 [22] | 3 | NA | NA | NA | NA | 0 | NA | NA | NA |
| Dong et al, 2020 [23] | 1 | 1 | NA | 1 | 1 | 0 | 0 | 0 | 0 |
| Fan et al, 2020 [24] | 2 | 2 | Oral oseltamivir | 2 | NA | 0 | 0 | 0 | 0 |
| Karami et al, 2020a [25] | 0 | 1 | Oseltamivir, lopinavir/ritonavir, hydroxychloroquine | 1 | 1 | 1 | 0 | 0 | 0 |
| Khan et al, 2020 [26] | 0 | 3 | NA | 3 | 3 | 0 | 0 | 0 | 0 |
| Lee et al, 2020 [27] | 1 | NA | NA | NA | NA | 0 | 0 | 0 | 0 |
| Li et al, 2020 [28] | 14 | 1 | NA | 16 | 0 | 0 | 1 | 0 | 0 |
| Liu et al, 2020 [29] | 10 | 11 | NA | 11 | 11 | 0 | NA | NA | NA |
| Yu et al, 2020 [30] | 7 | 7 | NA | 7 | 7 | 0 | 0 | 0 | 0 |
| Peng et al, 2020 [31] | 1 | 1 | IFN nebulization, oral lopinavir | 1 | 1 | 0 | NA | NA | NA |
| Wu et al, 2020 [32] | 18 | NA | NA | NA | NA | 0 | NA | NA | NA |
| Xiong et al, 2020 [33] | 0 | 1 | NA | 1 | NA | 0 | 1 | 0 | 0 |
| Yang et al, 2020 [34] | 7 | NA | NA | NA | NA | 0 | NA | NA | NA |
| Zambrano et al, 2020 [35] | 0 | NA | NA | NA | NA | 0 | NA | NA | NA |
| Li et al, 2020 [36] | 1 | 1 | Lopinavir, ritonavir | NA | NA | 0 | NA | NA | NA |
Abbreviations: IFN, interferon; NA, not available.
aStudy retracted.
Neonatal Outcomes
All neonates were all delivered in a negative-pressure isolation room, and all studies reported separation and lack of contact between the mothers and the neonates. Thirty-one of 94 neonates were delivered preterm (<37 weeks) (37.7% of neonates [95% CI, .269–.500]; I2 = 10.77%). Five newborns were delivered early preterm (<34 weeks). The birthweight of the neonates averaged 3127.639 g (95% CI, 2941.238–3314.041; I2 = 84.44%). The neonatal clinical characteristics and laboratory findings, as well as the perinatal complications, are shown in Table 6. The white blood cell count averaged 15.303 (95% CI, 12.852–17.755; I2 = 38.02%). In addition, the procalcitonin averaged 0.289 (95% CI, .211–.366; I2 = 0%). The hemoglobin concentration averaged 174.109 g/L (95% CI, 163.535–184.683; I2 = 33.82%), and the mean platelet count was 224.297 × 109 cells/L (95% CI, 191.729–256.866; I2 = 68.91%). In addition, the ALT and AST averaged 11.627 U/L (95% CI, 7.322–15.933; I2 = 67.95%) and 52.232 U/L (95% CI, 39.202–65.263; I2 = 20.05%), respectively. Elevated levels of AST were identified in 56.1% (95% CI, .321–.776; I2 = 0%) of patients. The lymphocyte and neutrophil counts averaged 3.278 × 109 cells/L (95% CI, 2.627–3.928; I2 = 0%) and 10.416 × 109 cells/L (95% CI, 7.495–13.338; I2 = 51.79%), respectively (Figure 4). Two newborns tested positive for COVID-19 (11.5% [95% CI, .067–.192]; I2 = 0). Both neonates were delivered via cesarean delivery. The amniotic fluid, placenta fluid, umbilical cord, and gastric juice were all tested for COVID-19 and tested negative in all the studies. The Apgar score at 1 minute was 8.811 (95% CI, 8.382–9.240; I2 = 88.87%) and at 5 minutes was 9.516 (95% CI, 9.136–9.895; I2 = 82.91%). In addition, no severe neonatal asphyxia occurred in any of the neonates across the studies. Three fetal deaths were reported; their respective gestational ages were 34 weeks, 31 weeks, and 30 weeks. Neonatal intensive care unit admission occurred in 63.7% (95% CI, .378–.835; I2 = 29.38%) of patients. The fetal death rate was 11.7% (95% CI, .068–.192; I2 = 0%) (Figure 5). Two neonatal deaths were due to multiple organ failure and disseminated intravascular coagulation. The third neonatal death occurred immediately after delivery. The neonate was cyanotic and had an Apgar score of 0 at 1 and 5 minutes, respectively.
Table 6.
Clinical Characteristics and Laboratory Findings of Neonates Born to Clinically Symptomatic Mothers
| Author, Year | Mean Gestational Age at Birth, wk | Mean Weight at Birth, g | Hb, g/L | Platelets, ×109/L | ALT, U/L | AST, U/L | Apgar Score at 1 Min | Apgar Score at 5 Min | Preterm labor (<37 wk), No. | COVID-19 Testing of Respiratory Tract | NICU Care, No. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chen et al, 2020 [13] | 37.11 | 3011 | NA | NA | NA | NA | 9 | 10 | 4 | Negative | NA |
| Chen et al, 2020 [14] | NA | 3030 | NA | NA | NA | NA | 9 | 10 | 3 | Negative | 17 |
| Liu et al, 2020 [15] | NA | NA | NA | NA | NA | NA | 9 | NA | 6 | Negative | NA |
| Wang et al, 2020 [16] | 40 | NA | NA | NA | NA | 143 | 8 | 9 | NA | Positive | NA |
| Wang et al, 2020 [17] | 30 | 1830 | NA | NA | NA | NA | 9 | 10 | 1 | Negative | NA |
| Zhu et al, 2020 [18] | 35 | 2423 | 166.3 | 218.5 | 7.98 | 45.05 | 9 | 9 | 6 | Negative | NA |
| Liu et al, 2020 [19] | 38 | 3390 | 171 | 187.67 | 17.67 | 107 | 8 | 9 | NA | Negative | NA |
| Iqbal et al, 2020 [20] | NA | NA | NA | NA | NA | NA | 8 | 9 | 0 | Negative | 1 |
| Chen et al, 2020 [21] | 39 | 3691 | NA | NA | NA | NA | 10 | 10 | NA | Negative | NA |
| Chen et al, 2020 [22] | 37.75 | 3400 | 181.7 | 253.33 | 14.67 | 60 | 8 | 9 | NA | Negative | 2 |
| Dong et al, 2020 [23] | NA | 3120 | NA | NA | 11 | 65 | 9 | 10 | NA | Negative | 1 |
| Fan et al, 2020 [24] | NA | 3145 | NA | NA | NA | NA | 9 | 10 | NA | Negative | NA |
| Karami et al, 2020a [25] | NA | NA | NA | NA | NA | NA | 0 | 0 | NA | Negative | NA |
| Khan et al, 2020 [26] | NA | 3373 | NA | NA | NA | NA | 8.67 | 9.67 | 1 | Negative | NA |
| Lee et al, 2020 [27] | NA | 3130 | NA | NA | NA | NA | 9 | 10 | 1 | Negative | 1 |
| Li et al, 2020 [28] | 38 | 3078 | NA | NA | NA | NA | 9.6 | 10 | 4 | Negative | NA |
| Liu et al, 2020 [29] | NA | NA | NA | NA | NA | NA | NA | 9 | NA | Negative | NA |
| Yu et al, 2020 [30] | NA | 3264 | NA | NA | NA | NA | 8–9 | 9–10 | 0 | Positive | 0 |
| Peng et al, 2020 [31] | 35 | 2600 | NA | NA | NA | NA | 9 | 10 | 1 | Negative | 1 |
| Wu et al, 2020 [32] | NA | NA | NA | NA | NA | NA | NA | 9–10 | NA | Negative | NA |
| Xiong et al, 2020 [33] | 38 | 3070 | NA | NA | 9 | 53 | 9 | 10 | 0 | Negative | 0 |
| Yang et al, 2020 [34] | 36.71 | 2096 | NA | NA | 11.2 | 59 | 8.29 | 9.29 | 2 | Negative | 5 |
| Zambrano et al, 2020 [35] | 32 | 1500 | NA | NA | NA | NA | NA | NA | 1 | Negative | NA |
| Li et al, 2020 [36] | 35 | NA | NA | NA | NA | NA | NA | NA | 1 | Negative | NA |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; COVID-19, coronavirus disease 2019; Hb, hemoglobin; NA, not available; NICU, neonatal intensive care unit.
aStudy retracted.
Figure 4.
Forest plot of neonatal laboratory findings present after birth. Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CI, confidence interval.
Figure 5.
Forest plot of neonatal outcomes after birth. Abbreviations: CI, confidence interval; COVID-19, coronavirus disease 2019; NICU, neonatal intensive care unit.
DISCUSSION
SARS-CoV-2 is a highly infective virus causing the greatest pandemic of the century. As of now, we are in the midst of it, seeking to determine treatments and novel ways to manage this deadly disease. In this contemporary meta-analysis, we have concluded the following: (1) Pregnant patients with COVID-19 most commonly present with fever, dry cough, and sore throat; (2) the most common radiological finding in this group of patients was the presence of GGO on CT; and (3) the perinatal risk is great, as the risk of prematurity and cesarean delivery are high. To our knowledge, this is the largest meta-analysis of its kind to describe the effects of COVID-19 on pregnancy. We believe that this study provides insight for developing the backbone for counseling and management of pregnant patients at risk for acquiring the disease.
The immunosuppressed state of pregnancy confers high risk for the development of severe complications of infectious diseases, such as influenza and severe acute respiratory syndrome (SARS) [37]. During the SARS pandemic of 2003, 40% of affected pregnant women required mechanical ventilation and had a case-fatality rate of 30%, compared to 13% and 11%, respectively, of a nonpregnant cohort [38]. Interestingly, our study did not demonstrate significantly worsened outcomes in COVID-19–affected pregnant patients when compared to nonpregnant patients reported in the literature. Our population has similar clinical presentations, laboratory abnormalities, and radiological findings compared with infected nonpregnant cohorts in the current literature [39]. Additionally, the maternal complication rate seems to be comparable to nonpregnant adults [39]. One theory is that the immunologic adaptations of pregnancy that help mothers from rejecting the fetus, a foreign entity containing paternal antigens, may also aid in mounting a less robust immune response to the virus, consequently leading to less destructive effects on the body [40]. Another is that pregnancy-related organ adaptive changes may result in protection against the virus and its effects [40].
Within our subset of 136 SARS-CoV-2–infected pregnant women, a single case of maternal death secondary to ARDS and multiorgan failure was reported, resulting in a considerably lower mortality rate in comparison to previous pandemics. Moreover, with 2 patients requiring intubation and mechanical ventilation, morbidity appeared to be lower than anticipated. Although a proportion of women had comorbidities present, some of which were obstetrical in etiology, they still did not experience life-threatening manifestations of COVID-19. A recently published case series described 2 cases of COVID-19–related cardiomyopathy in pregnant women [41]. However, both of these patients possessed multiple risk factors for cardiac disease, and it remained unclear as to whether cardiomyopathy occurred as a direct complication of COVID-19, or secondary to multiorgan dysfunction. Another interesting observation was the high rate of preterm birth in this group of patients, much higher than the general pregnant population (12% in the United States and lower in other developed countries). A direct causal link between infection and premature labor has been well established in the literature [42], and it is estimated that at least 40% of premature births are associated with intrauterine infection or inflammation [43]. Additionally, the high rate of cesarean delivery should not go unnoticed. Three-quarters of infected patients underwent a cesarean delivery, more than double that of the general pregnant population. Cesarean delivery, while a commonly procedure worldwide, is still a major surgery with significantly higher morbidity than a vaginal delivery, both in the short term, such as infections and bleeding, and in the long term, such as the risk of development of placenta accreta spectrum disorder in future pregnancy.
It is difficult to make conclusions on the risk of having a pregnancy affected by COVID-19 or pregnancy that is not, owing to the heterogeneity of the studies included in this meta-analysis. Although in the reported cases most neonates fared well, with the exception of 3 of them, the most worrying aspect of our finding is the high rate of preterm birth. Prematurity in and of itself is the most common cause of morbidity and mortality in neonates worldwide, both short-term and long-term. Since the immunological immaturity of neonates renders them susceptible to infections, vertical transmission is a particularly concerning complication of viral infections that occur during pregnancy [44]. In all cases, the amniotic fluid, placenta, and umbilical cord samples all tested negative for SARS-CoV-2, while 2 neonates had RT-PCR–confirmed SARS-CoV-2 infection. Based on these findings, it is impossible to conclude that these neonates acquired the infection during fetal life. Three neonatal deaths with gestational ages of 34 weeks, 31 weeks, and 30 weeks were reported in our analysis. Two fetal deaths occurred due to multiple organ failure and disseminated intravascular coagulation, and the third was a perinatal death occurring within 24 hours of birth. This is an alarming finding as neonates born at this gestational age typically have low death rates; however, due to insufficient information in the respective reports, we could not conclusively contribute these deaths to COVID-19–related complications. Previous studies on other coronavirus infections, such as Middle East respiratory syndrome and SARS coronaviruses, have demonstrated a lack of vertical transmission in pregnant women [45, 46]. Although the occurrence of vertical transmission at present seems rather unlikely, the significant implication in potentially leading to preterm birth and neonatal infection warrants continued investigation. Additionally, given the uncertainty of long-term neonatal outcomes in COVID-19, neonates should be monitored for any possible congenital defects.
Vaginal delivery and the interventions that may occur during the process, such as rupture of membranes, episiotomy, and placement of internal fetal monitors, play an important role in vertical transmission via the transplacental route of certain maternal infections to the fetus, namely blood-borne infections such as human immunodeficiency virus and hepatitis B and C [47]. In our study, both fetal COVID-19–confirmed cases were delivered via cesarean delivery. However, due to the small sample size for patients who delivered vaginally (n = 18), it is difficult to make any conclusions in that regard. Further studies should attempt to delineate these 2 groups for clarification. This is an important issue that obstetricians should take into account when considering the course of treatment for any patient with a confirmed viral infection.
Recently published reviews on this topic have reported similar findings [48–50]. However, unlike the present review, no categorization was made regarding the specific CT findings. The strengths of our study are as follows: (1) This is the largest study of its kind to date to explore pregnancy and perinatal outcomes of SARS-CoV-2 infections; (2) the patients and their neonates who were included had confirmed positive or negative RT-PCR SARS-CoV-2, preventing any uncertainty regarding the group of patients who had a clinical presentation but were not representative of the entire cohort; (3) to our knowledge, this is the first meta-analysis to look at the pooled effect of COVID-19 across all eligible studies; and (4) our study reports medication use for treatment of COVID-19 that includes antiviral therapy and corticosteroid use in more depth than existing studies.
Our systematic review and meta-analysis has some limitations. The main limitation is primarily the lack of high-quality data in the included studies. Due to the urgent timeline for data extraction and the complications requiring preterm labor, some cases had incomplete documentation of the epidemiological history, laboratory testing, and outcomes. In addition, our meta-analysis had a limited number of studies, most of which were either case series or case reports. This makes it difficult to draw any conclusions regarding clinical presentation and outcomes of patients. Additionally, patients who were asymptomatic or had mild cases and who did not require hospitalization were not accounted for due to publication bias. Last, due to the nature of the virus and the urgent need for more studies, our meta-analysis might have missed studies that were recently published in the literature, particularly in languages other than English.
As this global pandemic continues to spread, there will be a need for additional information on the effects of COVID-19 on pregnant women and their infants. Sufficiently understanding the clinical presentations and outcomes of SARS-CoV-2 infection among pregnant women and their neonates, along with pathological and molecular characterization of the virus, is valuable in determining the disease trajectory within this subset of patients. Currently, the American College of Obstetricians and Gynecologists has developed an algorithm to aid practitioners in evaluating and treating pregnant women with known exposure or symptoms consistent with COVID-19 infection [51]. The algorithm includes assessing patients’ symptoms such as fever and cough; conducting an illness severity assessment; and, based on degree of severity, assessing clinical and social risks [51]. With the disease burden increasing every day, the probability of a second wave of COVID-19 infection this upcoming winter, and the ongoing debate regarding whether pregnant front-line healthcare workers should continue working, are important matters that will hopefully be answered as more studies emerge. This review aims to provide physicians with an understanding of the clinical presentation and outcomes of pregnant women with confirmed COVID-19 and their neonates, to help them make better decisions when devising a counseling and treatment plan for their patients.
In summary, this meta-analysis demonstrates that pregnant women with COVID-19 have similar clinical characteristics and outcomes as the nonpregnant population and there appears to be little evidence of vertical transmission. However, when compared to the general pregnant population, infected women are at significantly higher risk for cesarean delivery and preterm birth. We urge obstetricians to continue reporting their data, especially that of asymptomatic patients or those with mild disease, so we are better able to understand this novel virus and hopefully improve outcomes.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Author contributions. R. M. and N. M. conceived the study, searched the literature, extracted the data, assessed the quality of the studies, and drafted the manuscript. D. G. searched the literature. R. M. and M. H. M. performed the statistical analysis and drafted the manuscript. L. A., L. D., E. B., J. F., and F. F. drafted the manuscript. All authors read and approved the final manuscript.
Acknowledgments. The authors thank Daniella Gerberi for the literature search. This review does not contain any studies with human participants or animals.
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395:565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. Coronavirus disease (COVID-19) outbreak Available at: https://www.who.int. Accessed 25 April 2020.
- 4. World Health Organization. Coronavirus disease (COVID-19) situation report 154 Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200622-covid-19-sitrep-154.pdf?sfvrsn=d0249d8d_2. Accessed 22 June 2020.
- 5. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 2020; 323:1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323:1239–42. [DOI] [PubMed] [Google Scholar]
- 8. Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lu X, Zhang L, Du H, et al. SARS-CoV-2 infection in children. N Engl J Med 2020; 382:1663–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med 2018; 23:60–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7:177–88. [DOI] [PubMed] [Google Scholar]
- 12. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet 2020; 395:809–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chen R, Zhang Y, Huang L, Cheng B, Xia Z, Meng Q. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing cesarean delivery: a case series of 17 patients. Can J Anaesth 2020; 67:655–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu Y, Chen H, Tang K, Guo Y. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy [manuscript published online ahead of print 4 March 2020]. J Infect 2020. doi: 10.1016/j.jinf.2020.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang S, Guo L, Chen L, et al. A case report of neonatal COVID-19 infection in China [manuscript published online ahead of print 12 March 2020]. Clin Infect Dis 2020. doi: 10.1093/cid/ciaa225. [DOI] [Google Scholar]
- 17. Wang X, Zhou Z, Zhang J, Zhu F, Tang Y, Shen X. A case of 2019 novel coronavirus in a pregnant woman with preterm delivery [manuscript published online ahead of print 28 March 2020]. Clin Infect Dis 2020. doi: 10.1093/cid/ciaa200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhu H, Wang L, Fang C, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr 2020; 9:51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu W, Wang Q, Zhang Q, et al. Coronavirus disease 2019 (COVID-19) during pregnancy: a case series. Preprints.org [Preprint] Posted 25 February 2020. Available at: https://www.preprints.org/manuscript/202002.0373/v1. Accessed 4 May 2020.
- 20. Iqbal SN, Overcash R, Mokhtari N, et al. An uncomplicated delivery in a patient with Covid-19 in the United States. N Engl J Med 2020; 382:e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen S, Liao E, Cao D, Gao Y, Sun G, Shao Y. Clinical analysis of pregnant women with 2019 novel coronavirus pneumonia [manuscript published online ahead of print 28 March 2020]. J Med Virol 2020. doi: 10.1002/jmv.25789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chen Y, Peng H, Wang L, et al. Infants born to mothers with a new coronavirus (COVID-19). Front Pediatr 2020; 8:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dong L, Tian J, He S, et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA 2020; 323:1846–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fan C, Lei D, Fang C, et al. Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? [manuscript published online ahead of print 27 March 2020]. Clin Infect Dis 2020. doi: 10.1093/cid/ciaa226. [DOI] [Google Scholar]
- 25. Karami P, Naghavi M, Feyzi A, et al. WITHDRAWN: Mortality of a pregnant patient diagnosed with COVID-19: a case report with clinical, radiological, and histopathological findings [manuscript published online ahead of print 11 April 2020]. Travel Med Infect Dis 2020. doi: 10.1016/j.tmaid.2020.101665. Retracted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Khan S, Peng L, Siddique R, et al. Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to-neonatal intrapartum transmission of COVID-19 during natural birth. Infect Control Hosp Epidemiol 2020; 41:748–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lee DH, Lee J, Kim E, Woo K, Park HY, An J. Emergency cesarean section on severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2) confirmed patient [manuscript published online ahead of print 31 March 2020]. Korean J Anesthesiol 2020. doi: 10.4097/kja.20116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Li N, Han L, Peng M, et al. Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case-control study [manuscript published online ahead of print 30 March 2020]. Clin Infect Dis 2020. doi:10.1093/cid/ciaa352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liu D, Li L, Wu X, et al. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis [manuscript published online ahead of print 18 March 2020]. AJR Am J Roentgenol 2020. doi: 10.2214/AJR.20.23072. [DOI] [PubMed] [Google Scholar]
- 30. Yu N, Li W, Kang Q, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis 2020; 20:559–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Peng Z, Wang J, Mo Y, et al. Unlikely SARS-CoV-2 vertical transmission from mother to child: a case report. J Infect Public Health 2020; 13:818–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wu X, Sun R, Chen J, Xie Y, Zhang S, Wang X. Radiological findings and clinical characteristics of pregnant women with COVID-19 pneumonia. Int J Gynaecol Obstet 2020; 150:58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Xiong X, Wei H, Zhang Z, et al. Vaginal delivery report of a healthy neonate born to a convalescent mother with COVID-19 [manuscript published online ahead of print 10 April 2020]. J Med Virol 2020. doi: 10.1002/jmv.25857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Yang P, Wang X, Liu P, et al. Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. J Clin Virol 2020; 127:104356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zambrano LI, Fuentes-Barahona IC, Bejarano-Torres DA, et al. A pregnant woman with COVID-19 in Central America [manuscript published online ahead of print 25 March 2020]. Travel Med Infect Dis 2020. doi: 10.1016/j.tmaid.2020.101639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Li Y, Zhao R, Zheng S, et al. Lack of vertical transmission of severe acute respiratory syndrome coronavirus 2, China. Emerg Infect Dis 2020; 26:1335–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kourtis AP, Read JS, Jamieson DJ.. Pregnancy and infection. N Engl J Med 2014; 370:2211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lam CM, Wong SF, Leung TN, et al. A case-controlled study comparing clinical course and outcomes of pregnant and non-pregnant women with severe acute respiratory syndrome. BJOG 2004; 111:771–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Yang H, Wang C, Poon LC. Novel coronavirus infection and pregnancy. Ultrasound Obstet Gynecol 2020; 55:435–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jamieson DJ, Theiler RN, Rasmussen SA. Emerging infections and pregnancy. Emerg Infect Dis 2006; 12:1638–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Juusela A, Nazir M, Gimovsky M, et al. Two cases of coronavirus 2019–related cardiomyopathy in pregnancy. Am J Obstet Gynecol MFM 2020; 2:100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Romero R, Mazor M, Munoz H, Gomez R, Galasso M, Sherer DM. The preterm labor syndrome. Ann N Y Acad Sci 1994; 734:414–29. [DOI] [PubMed] [Google Scholar]
- 43. Lamont RF. Infection in the prediction and antibiotics in the prevention of spontaneous preterm labour and preterm birth. BJOG 2003; 110(Suppl 20):71–5. [DOI] [PubMed] [Google Scholar]
- 44. Huleihel M, Golan H, Hallak M. Intrauterine infection/inflammation during pregnancy and offspring brain damages: possible mechanisms involved. Reprod Biol Endocrinol 2004; 2:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Li AM, Ng PC. Severe acute respiratory syndrome (SARS) in neonates and children. Arch Dis Child Fetal Neonatal Ed 2005; 90:F461–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Stockman LJ, Lowther SA, Coy K, Saw J, Parashar UD. SARS during pregnancy, United States. Emerg Infect Dis 2004; 10:1689–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Silasi M, Cardenas I, Kwon JY, Racicot K, Aldo P, Mor G. Viral infections during pregnancy. Am J Reprod Immunol 2015; 73:199–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zaigham M, Andersson O. Maternal and perinatal outcomes with COVID‐19: a systematic review of 108 pregnancies. Acta Obstet Gynecol Scand 2020; 99:823–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Di Mascio D, Khalil A, Saccone G, et al. Outcome of coronavirus spectrum infections (SARS, MERS, COVID 1 -19) during pregnancy: a systematic review and meta-analysis [manuscript published online ahead of print 25 March 2020]. Am J Obstet Gynecol MFM 2020. doi: 10.1016/j.ajogmf.2020.100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Parazzini F, Bortolus R, Mauri PA, Favilli A, Gerli S, Ferrazzi E. Delivery in pregnant women infected with SARS-CoV-2: a fast review. Int J Gynaecol Obstet 2020; 150:41–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. American College of Obstetricians and Gynecologists. COVID-19 algorithm Available at: https://www.acog.org/-/media/project/acog/acogorg/files/pdfs/clinical-guidance/practice-advisory/covid-19-algorithm.pdf?la=en&hash=2D9E7F62C97F8231561616FFDCA3B1A6. Accessed 24 April 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.