Abstract
Background
the epidemiological characteristics of older patients with COVID-19 was far from clear.
Objective
to explore the epidemiology of older patients with COVID-19 in Wuhan, China.
Design
a retrospective cross-sectional study.
Setting
a population-based study.
Subjects
the resident older patients (>65 years) diagnosed with COVID-19.
Methods
city-wide case series reported to Wuhan Center for Disease Control and Prevention from 12 December 2019 to 17 March 2020 were included. The epidemic curves were constructed by dates of disease onset.
Results
14,238 confirmed COVID-19 cases were older persons. The number of male cases were slightly less than female cases (1:1.01). The attack rate of COVID-19 in the older persons was 11.49‰ in Wuhan. There was a rapid increase of disease at the early stage of the epidemic and then a gradual and steady decrease was performed. 3,723 (26.15%) and 734 (5.16%) patients were diagnosed as severe and critical cases, respectively. The attributable crude fatality ratio of COVID-19 in the older population was 222.57/100,000, and the crude fatality ratio of COVID was 19.37%. The proportion of severe and critical cases, and fatality ratio were both higher in downtown area and increased with age.
Conclusions
the older persons are sensitive to COVID-19. The proportion of severe and critical cases and fatality ratio are higher than that in children and younger adults. Strengthen the protection and control strategies for the older adults are of priorities. More detailed epidemiological and clinical information should be measured in further studies.
Keywords: COVID-19, epidemiological, older people
Key points
The epidemiological characteristics of older patients with COVID-19 were far from clearly.
The attack rate of COVID-19 in older adults in Wuhan, China was 11.49%, and 31.31% patients were diagnosed as severe.
The crude fatality ratio was gradually increased with age, and higher in male or downtown.
The attributable crude fatality ratio and the crude fatality ratio were 222.37/100,000 and 19.37%.
Introduction
In the end of December 2019, clustering pneumonia cases of unknown aetiology emerged in Wuhan, Hubei province, China [1]. On 7th January 2020, the pathogenic agent was identified as the 2019 novel coronavirus (2019-nCoV), then named as SARS-CoV-2 on 11th February 2020 by World Health Organization (WHO). The illness associated with SARS-CoV-2 was named as the 2019 coronavirus disease (COVID-19). Early evidences showed that compared with SARS and MERS, COVID-19 was more contagious [2]. COVID-19 had spread rapidly from Wuhan to six continents and attracted global attention. Since 28th February 2020, WHO had increased the assessment of the risk of spread and risk of impact of COVID-19 to ‘very high’ at the global level. Up to 8th April, 2020, the number of COVID-19 cases surpassed 1,350,000 globally [3].
Available information show that because of the decline of immune function and the coexistence of underlying diseases, older persons are more susceptible to infection and are more likely to develop critical illness or even death [4]. Facing the global ageing, it is highly important to pay attention to the older persons for the prevention and control of COVID-19. However, the epidemiology of the COVID-19 among older persons remains far from clear. In this study, we explored the epidemiological characteristics of 14,238 resident older persons with COVID-19 in Wuhan, China.
Methods
A retrospective study on the epidemiological characteristics of resident older persons with COVID-19 in Wuhan was conducted. Resident older persons were defined as >65 years and at least 6 months residence in Wuhan. Since 18th March 2020, the suspected cases in Wuhan were cleared. The city-wide case series of resident older patients with COVID-19 reported to the Wuhan Center for Disease Control and Prevention (CDC) from 12th December 2019 to 17th March 2020 were extracted. Finally, 14,238 confirmed cases were included in this study. This study was approved by the institutional review boards of Wuhan CDC. And the results were reported according to the STROBE statement. Date of final follow-up of death was 18th April 2020.
According to Chinese clinical guidance for COVID-19 diagnosis and treatment, the cases were diagnosed on the basis of epidemiological history and clinical manifestations.
Epidemiological history: (1) travel or residence history of Wuhan and surrounding areas, or other communities where COVID-19 case(s) were reported within 14 days before the onset of illness; (2) history of contact with COVID-19 infected patients (nucleic acid detection positive) within 14 days before the onset of illness; (3) history of contact with the patients presenting fever or respiratory symptoms, who travel to or reside in Wuhan and surrounding areas, or in other communities where COVID-19 case(s) were reported within 14 days before the onset of illness; (4) clustering onset.
Clinical manifestation: (1) presenting with fever and/or respiratory symptoms; (2) with imaging features of COVID-19 pneumonia; (3) in early stage of the disease, leukocytes count was normal or decreased, and the lymphocyte count was decreased.
A case that meted any one of the epidemiology history criteria and any two of the clinical manifestations could be identified as a suspected case. If there was no clear epidemiological history, three of the clinical manifestation was required. Suspected case with one of the following aetiology evidences in nasal and pharyngeal swabs could be identified as confirmed cases: (1) Reverse Transcription-Polymerase Chain Reaction detection was positive for COVID-19 nucleic acid; (2) the viral gene identified by gene sequencing was highly homologous with known COVID-19.
The clinical classification of COVID-19 was classified to five types: (1) asymptomatic infection—without any clinical symptoms or signs and chest imaging was normal, while the SARS-CoV-2 nucleic acid test was positive; (2) mild—the clinical symptoms were mild, and there was no sign of pneumonia on chest imaging; (3) moderate—had fever and respiratory symptoms, and there was sign of pneumonia on chest imaging; (4) severe—meet any of the following criteria: (a) shortness of breath, respiratory rate ≥30 times/min; (b) oxygen saturation ≤93% at rest; (c) arterial partial pressure of oxygen/fraction of inspiration O2 (PaO2/FiO2) ≤300 mmHg; (d) pulmonary imaging showed significant progression of lesion >50% within 24–48 hours; (5) critical—patients meet any of the following conditions: (a) respiratory failure requiring mechanical ventilation; (b) shock; (c) combined with other organ failure and needed intensive care unit monitoring and treatment.
Statistical analysis
Descriptive analysis of age, sex, dates of disease onset, clinical classification and location (downtown including Jianghan, Jiangan, Qiaokou, Hanyang, Wuchang, Qingshan, Hongshan districts; suburb including Dongxihu, Hannan, Caidian, Jiangxia, Huangpi, Xinzhou districts) distribution was performed. The epidemic curves were constructed by dates of disease onset. The date of disease onset was defined as the self-report date of fever or cough onset, and for asymptomatic infection it was defined as the date of laboratory test positive. Attach rate was the number of confirmed cases divided the number of resident older persons in Wuhan in 2019. Crud fatality ratio was calculated by dividing the number of confirmed deaths by the total number of confirmed cases. COVID-19 attributable crude fatality ratio was the number of confirmed deaths divided the number of resident older persons in Wuhan in 2019. Analyses were performed with SAS software, Version 9.4 for Windows (SAS Institute Inc., Cary, NC, USA).
Results
Characteristics of older COVID-19 cases
By 17th March 2020, 14,238 resident older patients with COVID-19 were reported to Wuhan CDC. The attack rate of COVID-19 in the older persons was 11.49‰ (14,238/1,239,171). Among them, the number of male cases were slightly less than female cases, and the sex ratio was 1:1.01. 3,723 (26.15%) and 734 (5.16%) patients were diagnosed as severe and critical cases, respectively. And 81.54% patients were from the downtown of Wuhan (Table 1).
Table 1 .
Characteristics of the older COVID-19 cases (N = 14,238)
| Characteristics | N (%) |
|---|---|
| Age (years) | |
| 65–69 | 5,974 (41.96) |
| 70–74 | 3,620 (25.42) |
| 75–79 | 2009 (14.11) |
| 80–84 | 1,492 (10.48) |
| ≥85 | 1,143 (8.03) |
| Sex | |
| Male | 7,177 (50.41) |
| Female | 7,061 (49.59) |
| Clinical manifestations | |
| Asymptomatic | 202 (1.42) |
| Mild | 5,562 (39.06) |
| Moderate | 3,926 (27.57) |
| Severe | 3,723 (26.15) |
| Critical | 734 (5.16) |
| Missing | 91 (0.64) |
| Location | |
| Downtown area | 11,610 (81.54) |
| Suburb area | 2,628 (18.46) |
| Disease onset perioda | |
| Ascending period | 1,454 (10.21) |
| Peak period | 9,510 (66.79) |
| Descending period | 3,274 (23.00) |
aAscending period, before 20th January; peak period, 20th January to 7th February; descending, after 8th February.
The temporal distribution of onset data
The first older case was onset on 12th December 2019, and a trend of the rapid increase of cases onset after that day. On 25th January 2020, there was a small peak, and an abnormally high value occurred on 1 February 2020, then a gradual and steady decrease since 2 February 2020. Hence, we divided the epidemic process into ascending period (before 20 January), peak period (20 January–7 February), and descending period (after 7 February).
In total, 28.30% (14,238/50,315) cases were older adults. The proportion of the older in the total patients decreased from 100.0% (3/3) on 16th December 2019 to 17.20% (48/279) on 21th February 2020. But the proportion raised again after 22th February 2020 with the number of total diagnoses dropped significantly (Figure 1a).
Figure 1 .
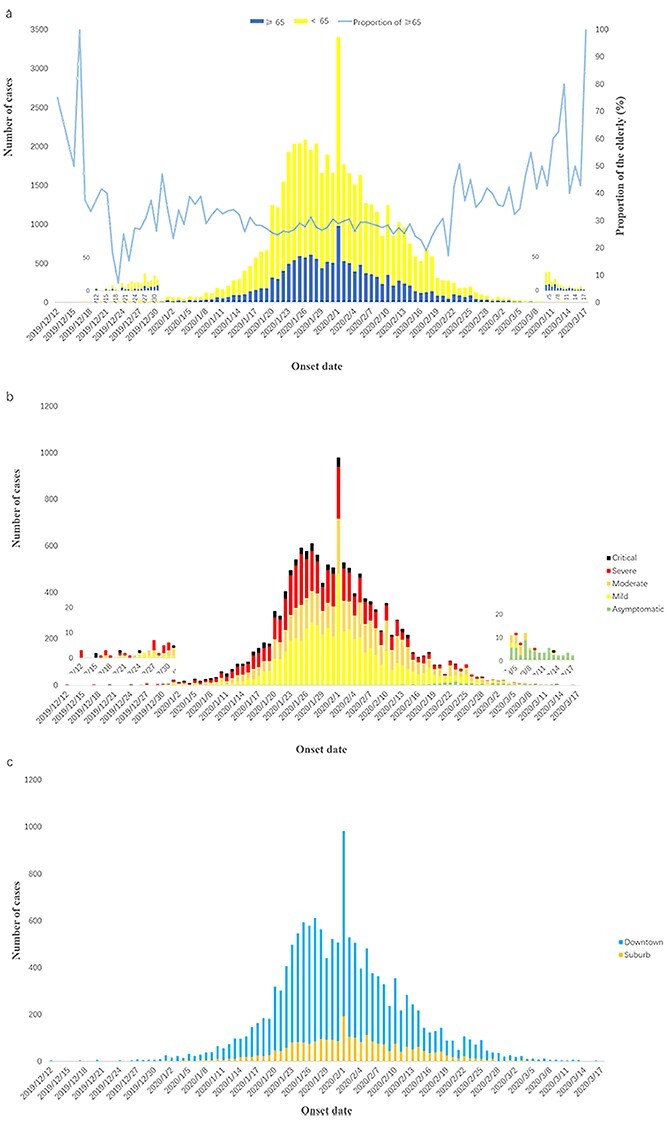
The temporal distribution of onset data of resident older COVID-19 cases in Wuhan. (a) Proportions in total cases (b) by clinical manifestations (c) by locations.
All the three older patients, which onset on 12 December 2019, were severe cases. Throughout the whole process, the older patients were mainly mild and moderate cases. And the proportion of severe and critical cases climbed up and then decreased. On 17th January 2020, there were two cases of asymptomatic infection reported among the older persons for the first time, and the proportion of asymptomatic infection gradually increased during the epidemic descending period. As shown in Figure 1b.
Characteristics of older COVID-19 cases in different locations
As performed in Figure 1c, the onset time of cases in suburb was later and the trend of zeroing was earlier than that in the downtown area.
The attack rate of older people in downtown was 15.99‰ (11,610/725,883) and was >5.12‰ (2,628/513,288) of the suburb area. The number of cases stratified by age, sex and clinical manifestation types were all higher in downtown area. In addition, the proportion of severe and critical cases in downtown was also higher than that in suburb area. Details were shown in Table 2.
Table 2 .
Characteristics of older COVID-19 cases in different locations
| Characteristics | Downtown (N/%) (N = 11,610) | Suburb (N/%) (N = 2,628) |
|---|---|---|
| Age (years) | ||
| 65–69 | 4,820 (41.52) | 1,154 (43.91) |
| 70–74 | 2,910 (25.06) | 710 (27.02) |
| 75–79 | 1,631 (14.05) | 378 (14.38) |
| 80–84 | 1,249 (10.76) | 243 (9.25) |
| ≥85 | 1,000 (8.61) | 143 (5.44) |
| Sex | ||
| Male | 5,830 (50.22) | 1,347 (51.26) |
| Female | 5,780 (49.78) | 1,281 (48.74) |
| Clinical manifestations | ||
| Asymptomatic | 168 (1.45) | 34 (1.29) |
| Mild | 4,330 (37.30) | 1,232 (46.88) |
| Moderate | 3,311 (28.52) | 615 (23.40) |
| Severe | 3,121 (26.88) | 602 (22.91) |
| Critical | 606 (5.22) | 128 (4.87) |
| Missing | 74 (0.63) | 17 (0.65) |
Characteristics of older COVID-19 cases in different age groups
As shown in Table 3, among the older patients <70 years, the attack rate of female was higher than that of male, but it was lower among those >70 years. And the attack rate was highest in >85 years old group for male, female and total population.
Table 3 .
Characteristics and attack rates of older COVID-19 cases in different age groups
| 65–69 years | 70–74 years | 75–79 years | 80–84 years | ≥85 years | Total | |
|---|---|---|---|---|---|---|
| Clinical manifestations (N/%) | ||||||
| Asymptomatic | 70 (1.17) | 35 (0.97) | 19 (0.95) | 34 (2.28) | 44 (3.85) | 202 (1.42) |
| Mild | 2,602 (43.56) | 1,400 (38.67) | 743 (36.98) | 488 (32.71) | 329 (28.78) | 5,562 (39.06) |
| Moderate | 1,712 (28.66) | 1,031 (28.48) | 508 (25.29) | 385 (25.80) | 290 (25.37) | 3,926 (27.57) |
| Severe | 1,348 (22.56) | 935 (25.83) | 591 (29.42) | 465 (31.17) | 384 (33.60) | 3,723 (26.15) |
| Critical | 208 (3.48) | 193 (5.33) | 132 (6.57) | 110 (7.37) | 91 (7.96) | 734 (5.16) |
| Missing | 34 (0.57) | 26 (0.72) | 16 (0.80) | 10 (0.67) | 5 (0.44) | 91 (0.64) |
| Sex (N/%) | ||||||
| Male | 2,889 (48.36) | 1904 (52.60) | 1,057 (52.61) | 752 (50.40) | 575 (50.31) | 7,177 (50.41) |
| Female | 3,085 (51.64) | 1716 (47.40) | 952 (47.39) | 740 (49.60) | 568 (49.69) | 7,061 (49.59) |
| Total population (N/%) | ||||||
| Male | 268,188 (51.18) | 152,519 (50.06) | 98,040 (48.65) | 60,073 (45.35) | 34,448 (45.05) | 613,268 (49.49) |
| Female | 255,812 (48.82) | 152,180 (49.94) | 103,494 (51.35) | 72,403 (54.65) | 42,014 (54.95) | 625,903 (50.51) |
| Attack rate (‰) | ||||||
| Male | 10.77 | 12.48 | 10.78 | 12.52 | 16.69 | 11.70 |
| Female | 12.06 | 11.28 | 9.20 | 10.22 | 13.52 | 11.28 |
| Total | 11.40 | 11.88 | 9.97 | 11.26 | 14.95 | 11.49 |
The proportion of severe and critical cases was gradually increased with age. And the proportion of severe and critical cases in the older persons >85 years was up to 33.60% and 7.96% respectively.
Characteristics of older COVID-19 deaths
The onset time of the first death case was 20th December 2019, and its time of death was 7th January 2020. In all deaths, the interval from onset to death was from 0 to 95 days, with a median of 15 days.
The attributable crude fatality ratio of COVID-19 in the older population was 222.57/100,000, and the crude fatality ratio of COVID was 19.37%. The attributable crude fatality ratio and case fatality ratio both gradually increased with age, and higher in male or downtown. The most death cases were onset during the peak period. But the crude fatality ratio was highest (30.95%) in the cases which onset during the ascending period. Details are shown in Table 4.
Table 4 .
Characteristics of older COVID-19 deaths
| Characteristics | N (%) | Fatality ratio (%) | Attributable crude fatality ratio (/100,000) |
|---|---|---|---|
| Age (years) | |||
| 65–69 | 668 (24.22) | 11.18 | 127.48 |
| 70–74 | 663 (24.04) | 18.31 | 217.59 |
| 75–79 | 508 (18.42) | 25.29 | 252.07 |
| 80–84 | 475 (17.22) | 31.86 | 358.56 |
| >85 | 444 (16.10) | 38.81 | 580.68 |
| Sex | |||
| Male | 1,745 (63.27) | 24.31 | 284.54 |
| Female | 1,013 (36.73) | 14.35 | 161.85 |
| Location | |||
| Downtown | 2,366 (85.79) | 20.38 | 460.95 |
| Suburb | 392 (14.21) | 14.92 | 54.00 |
| Disease onset perioda | |||
| Ascending period | 450 (16.32) | 30.95 | 36.31 |
| Peak period | 1890 (68.53) | 19.87 | 152.52 |
| Descending period | 418 (15.16) | 12.77 | 33.73 |
| Total | 2,758 (100.00) | 19.37 | 222.57 |
aAscending period, before 20th January; peak period, 20th January to 7th February; descending, after 8th February.
Discussion
So far, this is the first retrospective study on the epidemiological characteristics of older persons with COVID-19 in China. Wuhan, as the first outbreak area and one of the most serious areas, the data of this region have certain reference value for the COVID-19 prevention and control of the other regions. As of 18th March 2020, 14,238 confirmed older adults included in this study. Though most cases were mild, the severe and critical cases in older patients were as much as 31.31%, which was significantly higher than that in children (5.9%) [5]. According to the situation report of WHO in 8th April 2020, the facility ratio of the global population was 5.85%. And the facility ratio of older persons in Wuhan was almost four times that of the total population. Hence, strengthen the protection and screening of the older adults are the top priorities for the COVID-19 prevention and control.
SARS-CoV-2, a novel coronavirus, belongs to the coronavirus β genus. It shares >85% homology with SARS-like coronavirus isolated form bat (bat-SL-CoVZC45) [6]. Evidences show that the epidemic of COVID-19 may be associated with Huanan Seafood Wholesale Market where wildlife trade exists. Until now the intermediate hosts are still unclear and a research concluded that pangolin might be one of the potential sources of SARS-CoV-2 [7]. The epidemic is ongoing worldwide rapidly. WHO has declared the COVID-19 as a public health emergency of international concern. The Chinese and Wuhan governments have taken a series of measures to control the spread of COVID-19. 29th December 2019, first case was reported to Wuhan CDC and the city-wide cases search began. Huanan Seafood Wholesale Market was closed on 1th January 2020. And on 20th January 2020, COVID-19 was classified as class B infectious disease, but was managed as class A. On 24th January 2020, tiered medical services was adopted. On 2th February 2020, all close contacts in Wuhan were centralised isolated, observed and treated. On 4th February 2020, Huoshenshan Hospital, which was a newly built hospital for COVID-19 admission, began to accept the first batch of patients. On 5th February 2020, mobile cabin hospital came into service. These measures could effectively classify and isolated the infected persons, and the epidemic began to be controlled in Wuhan.
The older COVID-19 patients are more likely to develop severe, critical type or even death. This may be related to the poor immune function of older adults that weaken their respond to pathogens. Besides, compared with children and younger cases, the older patients always complicate with many underlying diseases, and the clinical manifestations are more likely to be severe once infected. Moreover, older adults are easier to ignore the early symptoms of COVID-19 and will miss the best time to seek medical advice. In the initial stage of COVID-19, the proportion of severe or critical type is higher, which may be related with the lack of treatment conditions and guidelines in the face of the new disease.
The results showed slightly less older males affected SARS-CoV-2 than females, which was contrary to other studies [5, 8, 9]. However, the other studies included the suspected cases. And whether the distribution between different sexes was significant still need further discussion.
Temporal distribution of older COVID-19 disease showed in the early stage of the epidemic, there was a trend of rapid increase both for the number of onset and for the proportion of severe and critical cases. Since early February 2020, the trend had been declining. It indicated that the disease control measures implemented by the government were effective.
Compared with the downtown area, the COVID-19 epidemic of suburb area started late and faded early. And the attack rate and proportion of severe/critical in suburb area were both lower. Early in the epidemic, cross-infection in fever clinics largely promoted the outbreak of COVID-19. And most of the medical institutions in Wuhan were located in downtown. So due to the higher population density and mobility, the older persons in downtown area might have a higher exposure chance. Hence, the tighter controls in downtown area are needed.
Though in our study, the proportion of asymptomatic infection gradually increased in the descending period, it did not mean the increase of asymptomatic infected cases. This phenomenon was largely correlated to the increasing nucleic acid tests of SARS-CoV-2 in non-symptom population. Without census, there is no definitive data on the number of asymptomatic infections so far. Existed evidences showed that SARS-CoV-2 viral loads of symptomatic and asymptomatic patients were similar, which raised profound challenges to the COVID-19 prevention and control [10, 11]. And the researchers predicted that covert coronavirus infections could be seeding new outbreaks [12]. The older adults often need the care of other family members, screening of their caretaker is important.
This study has several strengths. First, the cases were all confirmed which ensure the accuracy of the data. Second, this was the first study focussed on the epidemiological characteristics of older persons’ COVID-19 in China. Finally, the stratified analyses on sex, age, clinical manifestations, location and temporal distribution were conducted.
This study also has some limitations. First, there were no clinical characteristics of the older persons with COVID-19 and we cannot do in-depth analysis. Second, the information on older patients’ exposure history was not available and the incubation period was not examined in this study. Finally, in the early stage, because the shortage of medicals resources and the deficiency of detection reagents, some cases, especially the death cases, were missing. To gain a better understanding of older adults with COVID-19, more detailed epidemiological and clinical information should be analysed in further studies.
In conclusions, older people are sensitive to COVID-19. The distribution varies with time. Though most cases are mild, the severe and critical cases in older patients are as much as 31.31% and the facility ratio is higher than that in children and younger adults. Furthermore, the epidemic of downtown is even worse than suburb. Strengthen the protection and control strategies for the older persons are of top priorities for the COVID-19 prevention and control.
Contributor Information
Yan Guo, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Xinghua Liu, Department of Gastrointestinal, Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
Mengyao Deng, School of Medicine, Wuhan University of Science and Technology, Wuhan, China; Research Center for Health Promotion in Women, Youth and Children, Wuhan University of Science and Technology, Wuhan, China.
Pulin Liu, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Fang Li, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Nianhua Xie, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Yanhui Pang, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Xiaoxia Zhang, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Wen Luo, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Ying Peng, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Yaqiong Yan, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Gang Li, Wuhan Centers for Disease Prevention and Control, Wuhan, China.
Mei Yang, School of Medicine, Wuhan University of Science and Technology, Wuhan, China; Research Center for Health Promotion in Women, Youth and Children, Wuhan University of Science and Technology, Wuhan, China.
Declaration of Conflicts of Interest
None.
Declaration of sources of funding
This work was supported by the National Natural Science Fund (grant number 81703239). The funder of the study had no role in the study design, execution, analysis, data interpretation or writing of the report.
References
- 1. Zhu N, Zhang D, Wang W, Li X. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382: 727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet 2020; 395: 470–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization . Coronavirurs Disease 2019 (COVID-19) Situation Report-79. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (8 April 8 2020, date last accessed).
- 4. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 5. Dong Y, Mo X, Hu Yet al. Epidemiology of COVID-19 among children in China. Pediatrics 2020; 145: e20200702. [DOI] [PubMed] [Google Scholar]
- 6. Lu R, Zhao X, Li Jet al. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395: 565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lam TT, Shum MH, Zhu HCet al. Identifying SARS-CoV-2 related coronaviruses in Malayan pangolins. Nature 2020. doi: 10.1038/s41586-020-2169-0. [DOI] [PubMed] [Google Scholar]
- 8. The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team . The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly 2020; 2: 113–22. [PMC free article] [PubMed] [Google Scholar]
- 9. Guan WJ, Ni ZY, Hu Yet al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020; 382: 1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zou L, Ruan F, Huang Met al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med 2020; 382: 1177–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rothe C, Schunk M, Sothmann Pet al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med 2020; 382: 970–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Qiu J. Covert coronavirus infections could be seeding new outbreaks. Nature 2020. doi: 10.1038/d41586-020-00822-x. [DOI] [PubMed] [Google Scholar]


