Abstract
Introduction
This ecological study investigates the association between smoking prevalence and COVID-19 occurrence and mortality in 38 European nations as of May 30, 2020.
Methods
Data were collected from Our World in Data. Regression analysis was conducted to adjust for potential confounding factors such as economic activity (gross domestic product), the rate of COVID-19 testing, and the stringency of COVID-19 control policies.
Results
There was a statistically significant negative association between smoking prevalence and the prevalence of COVID-19 across the 38 European nations after controlling for confounding factors (p = 0.001). A strong association was found between the prevalence of COVID-19 per million people and economic activity (p = 0.002) and the rate of COVID-19 testing (p = 0.0006). Nations with stricter policy enactment showed fewer COVID-19 cases per million people, but the association was not significant (p = 0.122). Delaying policy enactment was associated with a greater prevalence of COVID-19 (p = 0.0535). Evidence of a direct association between smoking prevalence and COVID-19 mortality was not found (p = 0.626). There was a strong positive association between COVID-19 mortality rate and the prevalence of COVID-19 cases (p < 0.0001) as well as the proportion of the population over 65 years of age (p = 0.0034) and a negative association with the rate of COVID-19 testing (p = 0.0023).
Conclusions
We found a negative association between smoking prevalence and COVID-19 occurrence at the population level in 38 European countries. This association may not imply a true or causal relationship, and smoking is not advocated as a prevention or treatment of COVID-19.
Implications
Given the evidence of this ecological study, and of several other studies that found an underrepresentation of smoking prevalence in hospitalized cases, it may be worth examining, in laboratory experiments and controlled human trials, if nicotine offers any protection against COVID-19. Most importantly, to date, no study, including this one, supports the view that smoking acts as a treatment intervention or prophylaxis to reduce the impact or ameliorate the negative health impacts of COVID-19.
Introduction
There are numerous published studies on the link between smoking and COVID-19, the respiratory illness caused by the SARS-CoV-2 virus, but as Berlin et al. note, there is uncertainty about what conclusions to draw.1 Evidence from hospital COVID-19 cases in China,2 Padova, Italy,3 and New York City4 suggest that smoking prevalence may be lower compared with the general population. Lippi and Henry,5 in a meta-analysis of five studies, found no significant association between smoking and increased risk of developing severe COVID-19. In contrast, a meta-analysis by Vardavas and Nikitara,6 and another recent meta-analysis of 19 papers comparing the risk of progression of COVID-19 among smokers relative to individuals that never smoked,7 concluded that smoking is most likely associated with increase severity and poorer outcomes of COVID-19.
The relationship between smoking and COVID-19 is further complicated when considering that smoking is known to increase the occurrence of multiple respiratory illnesses8 and can lead to an increased risk of lung cancer.9 One factor associated with progression of COVID-19 pneumonia is a patient’s smoking history.10,11 However, the observation of reduced prevalence of smoking among hospitalized COVID-19 cases has resulted in the hypothesis that the intake of nicotine or other constituents in smoke by active smokers may reduce the likelihood of developing COVID-19 disease,3,5,12 although no mechanism to explain how this might happen exists. Clues may lie with the nicotinic receptor.13
Methods
An ecological study was conducted including European Union (EU) and Eurozone (EURO) nations. Cognizant that these areas have rich cultural diversity, including smoking habits, we wanted to ascertain any link between the occurrence of COVID-19 cases per million people as of May 30, 2020 and smoking prevalence across the general population using regression analysis and controlling for confounding factors such as economic activity, the rate of COVID-19 testing, and strength of COVID-19 control policies. Furthermore, we investigated the association between smoking prevalence and COVID-19 mortality per million people, through regression analysis controlling for COVID-19 cases per million people as well as other confounding factors.
The study included 38 European, 27 EU, and 19 EURO nations (Supplementary Table S1). All data were obtained from Our World in Data on May 30, 2020. Total COVID-19 cases, deaths, and tests reported on this date were converted to values per million people to control for population size. Smoking prevalence was measured using the 2016 prevalence rate or percentage of smokers among the adult population and converted to the number of smokers per million people. The variable “proportion of the population > 65 years of age” was constructed in a similar way to reflect the proportion of elderly people in the population. Economic activity was measured using, as a surrogate, gross domestic product (GDP). Policies in the European nations were controlled using the maximum COVID-19 Response Stringency-Index (SI) version 6 (May 28, 2020) that a nation reached from January 1, 2020 to May 27, 2020 (Supplementary Figure 1) as well as a measure of delay of enactment of COVID-19 control policies measured by the number of days until the occurrence of the first nonzero value in the SI from January 1 when nations could have acted.
Results
Supplementary Table S2 shows some initial descriptive statistics of the top five high and low smoking prevalence nations. At one extreme, 43.4% of the adult population of Greece smokes, but it had the lowest prevalence of COVID-19 cases per million people (280) on May 30, 2020, but on the other extreme is Iceland, with only 14.7% of its population that smokes, but with a prevalence of COVID-19 cases per million people that is 19 times larger than that of Greece. The five nations with the highest smoking prevalence are located in the eastern part of Europe with an average smoking prevalence of 39.5% of the adult population, 1084 COVID-19 cases per million, 29 COVID-19 deaths per million people, 29,375 tests per million people and an average GDP per capita of $18,733. In contrast, the five nations with the lowest smoking prevalence are from the wealthier part of Europe. These countries have an average smoking prevalence rate of 18.6% (i.e., almost 50% lower), an average GDP per person of $49 100 (i.e., a 2.6 times higher standard of living), an average of 2754 COVID-19 cases per million people (i.e., 2.5 times larger), 133 COVID-19 mortalities per million people (i.e., 4.7 times higher), and have conducted 77 546 COVID-19 tests per million people (i.e., 2.6 times more). In terms of policy to contain the spread of COVID-19, the top five smoking prevalence nations have a higher maximum SI on average and less delay to act, as measured by the number of days since first policy enactment as per the SI. The simple Pearson’s linear correlation coefficient between smoking prevalence and the prevalence of COVID-19 cases (in logs) is −0.575 (p < 0.0001) with 95% confidence interval (−0.756, −0.313).
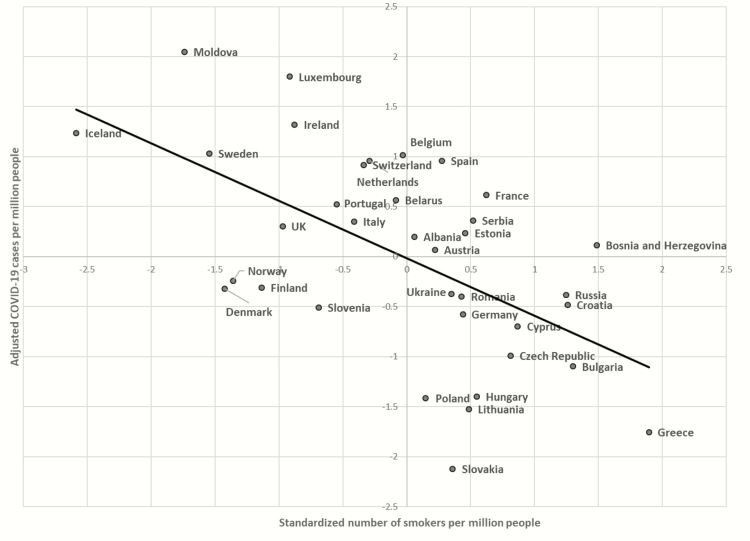
Regression results for 36 European nations, due to missing SI values for two nations, showed an explained variation of approximately 58% in the prevalence rate of COVID-19 cases per million people across these diverse nations by the independent variables (Supplementary Table S3). Nations with a higher number of smokers per million people showed fewer COVID-19 cases per million people (p = 0.001; Figure 1), after controlling for the confounding factors. High smoking prevalence was associated with a lower prevalence of COVID-19 per million people and vice versa. The effect size indicated that a nation that had 10% more smokers per million people experienced a 15% lower COVID-19 prevalence per million people for the 36 European nations. This size effect increased to 16% for the EU nations (p = 0.0287) and to 22% for the Eurozone nations (p = 0.0086). Figure 1 shows that high smoking prevalence and a low prevalence of COVID-19 cases occurred mostly in Eastern European nations, whereas low smoking prevalence and a high occurrence of COVID-19 cases per million people occurred in wealthier European nations, after adjusting the prevalence rate of COVID-19 cases for the impact of confounding factors (and reconfirming the descriptive statistics in Supplementary Table S2).
Figure 1.
Number of smokers versus COVID-19 cases in European nations. All variables were transformed to natural logarithms. COVID-19 cases per million people was adjusted for the influence of other confounding factors and standardized against standardized number of smokers per million people. The partial correlation coefficient is −0.576 (p < 0.001) with a 95% confidence interval (−0.761, −0.306), very similar to the simple Pearson correlation coefficient −0.575 (p < 0.001) with a 95% CI (−0.756, −0.313), indicating that the confounding factors controlled for did not distort the simple linear association that had been detected, either because these confounding factors are uncorrelated with the smoking prevalence rate or have an offseting impact on the COVID-19 prevalence when the smoking rate was correlated with the confounding factors. Smoking prevalence was negatively correlated with the rate of COVID-19 testing but was positively correlated with Max Stringency-Index.
Regarding the other potential explanatory factors, results show that more economic activity, as measured by the GDP of a nation, was associated with a higher prevalence of COVID-19 cases per million people relative to nations with lower GDP (p = 0.002). Nations with a higher rate of COVID-19 testing had a higher prevalence of COVID-19 cases per million people (p = 0.0006) after controlling for the size of the economy, smoking habits, and policies to contain the spread of the virus. There was an association between a more stringent COVID-19 policy response, as measured by the maximum SI index during the January 1 to May 30 period (Supplementary Figure 1), and less COVID-19 cases per million people, but this was not statistically significant (p = 0.122). There was no statistically significant association between degree of delay in policy enactment and COVID-19 prevalence.
Results for analyses restricted to the 25 EU nations were similar, with smoking prevalence retaining its significant association with COVID-19 prevalence (p =0.0287), but the two policy response variables were non-significant. Considering the 17 EURO nations, the results still hold for smoking prevalence (p = 0.0086), but there was evidence of association of increased occurrence of COVID with greater degree of delay in the policy response (p = 0.0535).
Supplementary Table S2 also shows that nations with more COVID-19 cases per million people had more COVID-19 deaths per million people after controlling for all other factors. We found no evidence of a direct association between smoking prevalence and COVID-19 mortality in all 36 European countries or the EU or Eurozone nations (e.g., p = 0.6260 for all European nations). Other results include the following. Nations with a greater population >65 years of age per million people had a significantly higher COVID-19 mortality per million people in the 38 European nations group (p = 0.003). Tests per million people was significantly negatively associated with deaths per million people, except within the Eurozone countries (i.e., p = 0.0023 for the 38 European nations, p = 0.0057 for the EU nations and p = 0.1014 for the Eurozone nations).
Discussion
We found a statistically significant negative correlation between the level of smoking in the adult population and prevalence of reported COVID-19 cases as of May 30, 2020 across 36 European nations after controlling for potential confounders such as economic activity, the rate of COVID-19 testing and strength of containment policies. The data did not show any association between smoking prevalence and COVID-19 mortality per million people. Furthermore, the evidence shows that a higher COVID-19 testing rate, acting as a potential indicator of policy action, results in a lower mortality rate when controlling for the COVID-19 prevalence rate and the other confounding factors. Nations with a higher age ≥65 population have a higher mortality rate when all 38 nations were examined but were not significant at the 5% level for the two other subgroups. This is most likely due to the greater variation in population >65 years of age per million people among all 38 nations than in the EU or Eurozone nations making it difficult to detect a potential association.
The study has a number of limitations. As Berlin et al. stated,3 conclusions cannot be drawn about any association as these studies, including this ecological study, which is at the macro level, are descriptive in nature and cross-sectional. Although an attempt was made to control for the most important factors such as size of the economy, policies, and the rate of COVID-19 testing, there could still be other important missing confounding factors that have not been controlled for, or residual confounding factors due to inadequate measurement of potential confounding factors.
Potential confounding factors omitted from this study include levels of air pollution, levels of comorbid diseases, COVID-19 clustering within a nation, and rate of international traveler arrivals. Ideally, an adjustment for the general level of interaction within each country’s population would need to be carried out, but such data are not easily available in practice.
One of the most important confounding factors are the stringency policies, as assessed by the SI, to contain the COVID-19 pandemic within the participating countries which this study attempted to control for. However, we were unable to establish an association with a high degree of confidence. Most likely, this is because there was limited variation in the strength of policy responses between nations (Supplementary Figure S1). Another problem is that the policy response for most governments was likely to be reactive, rather than proactive, and most stringent policies may have been enacted in response to a high prevalence of COVID-19, making it difficult to detect a cross-sectional association between policies and the prevalence of COVID-19. Also, we did not control for the rate of relaxation of COVID-19 containment policies. The data show that all of the European nations examined in this research relaxed their containment policies before May 30, as per the SI. A potential issue with the strong negative association between smoking prevalence and the occurrence of COVID-19 in European nations is that confounding factors are poorly measured and residual confounding may be present. For example, it is possible that the level of testing might not be measuring the level of effective testing, or that the test employed may not be specific enough.14 One possibility is that lower income countries, despite having fewer tests per million people, may also have poorer quality tests and less well-targeted testing. Hence, an adjustment exclusively based on the number of tests would not fully capture differences between countries in the effectiveness of the testing regime.
Finally, in this study, we examined the factors that are associated with total cases per million people at a single point in time, namely observations on May 30, 2020. It is possible that our results may be affected by the subsequent progression of the COVID-19 epidemic in each country. This could be investigated in a subsequent study once the epidemic has subsided. This highlights the importance of further investigations to assess whether the findings of this preliminary ecological study are supported by data in subsequent epidemiological research. For example, further ecological studies could be carried out to investigate variation in COVID-19 occurrence and mortality with smoking prevalence in the United States at the general population level, similar to this study.
In conclusion, given the evidence from this ecological study, and of several other studies that found an underrepresentation of smoking prevalence in hospitalized cases, it may be worth examining in laboratory experiments and controlled human trials if nicotine or other compounds in cigarette smoke offer any protection against COVID-197,13. However, we stress that no study, including this one, supports the view that smoking acts as a treatment intervention or prophylaxis to reduce the impact or ameliorate the negative health impacts of COVID-19.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Acknowledgment
The authors thank the editors and peer reviewer for excellent advice and assistance over several rounds of revisions.
Declaration of Interests
None declared.
Data Availability
Data file is available upon reasonable request.
References
- 1. Berlin I, Thomas D, Le Faou AL, Cornuz J. COVID-19 and smoking [published online ahead of print April 3, 2020]. Nicotine Tob Res. 2020. doi: 10.1093/ntr/ntaa059/5815378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. New Engl J Med. 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rossato M, Russo L, Mazzocut S, et al. Current smoking is not associated with COVID-19. Eur Respir J. 2020;55:2001290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of Covid-19 in New York City. N Engl J Med. 2020;382(24):2372–2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Internal Med. 2020;75:107–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vardavas CI, Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis. 2020;18:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Patanavanich R, Glantz SA. Smoking is associated with COVID-19 progression: a meta-analysis [published online ahead of print May 11, 2020]. Nicotine Tob Res. 2020. doi: 10.1093/ntr/ntaa082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Peiffer G, Underner M, Perriot J. The respiratory effects of smoking. Rev Pneumol Clin. 2020;74(3):133–144 (in French with English abstract). [DOI] [PubMed] [Google Scholar]
- 9. O’Keeffe LM, Taylor G, Huxley RR, Mitchell P, Woodward M, Peters SAE. Smoking as a risk factor for lung cancer in women and men: a systematic review and meta-analysis. BMJ Open. 2018;8(10):e021611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leung JM, Yang C-X, Tam A, et al. ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19. Eur Respir J. 2020;55(5):2000688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu W, Tao ZW, Wang L, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J. 2020;133(9):1032–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Leung JM, Yang C-X, Sin DD. Reply to: “Current smoking is not associated with COVID-19.” Eur Respir J. 2020;55:2001340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lutchman D. Could the smoking gun in the fight against Covid-19 be the (rh) ACE2? Eur Respir J. 2020. doi: 10.1183/13993003.01560-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zitek T. The appropriate use of testing for COVID-19. West J Emerg Med. 2020;21(3):470–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data file is available upon reasonable request.