Abstract
Background
Severe acute respiratory syndrome–related coronavirus 2 (SARS-CoV-2) was found to be the causative microorganism of coronavirus disease 2019 (COVID-19), which started to spread in Wuhan, China. This study was to evaluate the effectiveness of questionnaire, symptoms-based screening, and polymerase chain reaction (PCR) screening of returnees from COVID-19-endemic areas on a chartered flight, to examine the proportion of infected persons and the proportion of asymptomatic persons among infected persons who returned from Wuhan.
Methods
A retrospective cohort study was done in 7 tertiary medical institutions in Japan. A total of 566 Japanese who returned from Wuhan participated in the study.
Results
Overall, 11 of the 566 passengers had a positive SARS-CoV-2 PCR result for pharyngeal swabs and 6 were asymptomatic. Only fever differed between SARS-CoV-2-positive and -negative individuals (P < .043). Six of the 11 PCR-positive individuals were asymptomatic; 4 remained positive on day 10, and 1 asymptomatic person tested positive up to day 27. Two of the 11 were negative on the first PCR test and positive on the second.
Conclusions
Our results will be important insights on screening returnees from locked-down cities, as well as providing important data on the proportion of asymptomatic individuals infected with SARS-CoV-2. A 13-day observation period and a second round of PCR may be effective to screen patients, including asymptomatic infections.
Keywords: COVID-19, Wuhan, SARS-CoV-2, returnees, lockdown
BACKGROUND
At the end of December 2019, pneumonia of an unknown cause started to spread in Wuhan, China [1], and on January 8, 2020, severe acute respiratory syndrome–related coronavirus 2 (SARS-CoV-2) was found to be the causative microorganism [2]. Initially, 49%–66% of affected individuals were reported to be associated with the seafood market [3, 4], and it is believed that the majority of cases since January have been transmitted from person to person [5, 6]. On January 30, 2020, the World Health Organization (WHO) declared it a Public Health Emergency of International Concern (PHEIC) [7]. As of February 15, 2020, the epidemic has spread worldwide, and there have been cases of human-to-human transmission outside China [8]. The Wuhan City government announced on January 21 that access to Wuhan would be partially restricted, and on January 23 the government reported that Wuhan outbound railway stations and airports as well as all public transport in the city would stop. This decision made it difficult for foreigners living in Wuhan to return to their home countries. On January 28, after negotiations with the Chinese government, the Japanese government announced that it would send charter flights to Wuhan to repatriate Japanese residents who wished to leave the city. The government of Japan decided to conduct a SARS-CoV-2 polymerase chain reaction (PCR) test on all returnees, even if they were asymptomatic. This study was based on the results of a SARS-CoV-2 PCR test performed on returnees from Wuhan and a follow-up study after returning to Japan. The purpose of this study was to determine the prevalence of COVID-19 among returnees from Wuhan and the clinical course of asymptomatic individuals.
METHODS
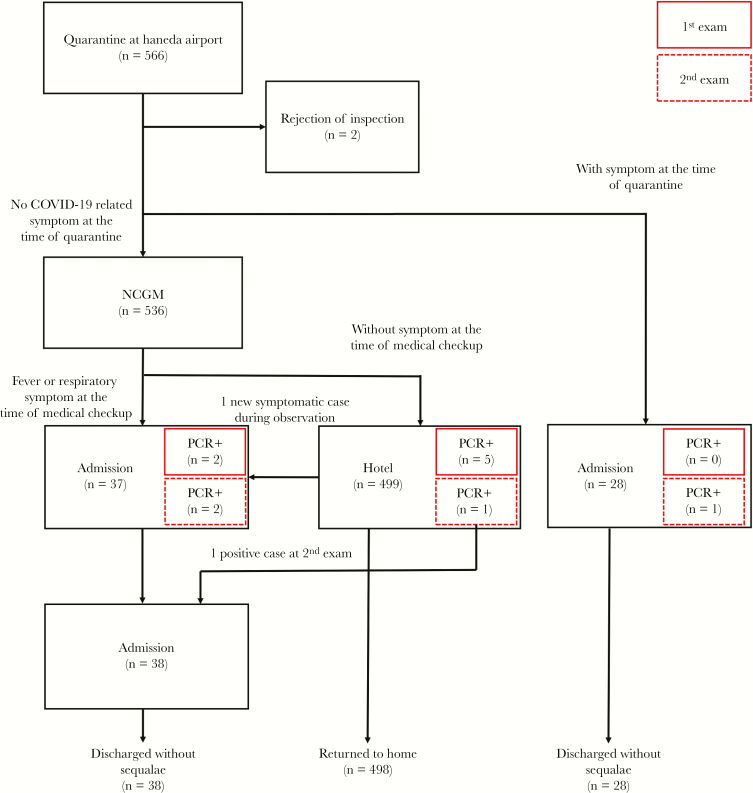
This retrospective cohort study included Japanese Wuhan residents who returned to Tokyo International Airport (HND) from the Wuhan Tianhe International Airport (WUH). At WUH, people with symptoms clearly indicative of coronavirus disease 2019 (COVID-19) were not allowed to leave Wuhan. At the HND Quarantine Station, returnees who were suspected of having COVID-19 with fever and respiratory symptoms such as cough or sore throat were transported to several medical institutions in Tokyo (Figure 1). Returnees who were judged to have no symptoms were transported to the National Center for Global Health and Medicine (NCGM), Shinjuku, Tokyo, where they underwent thermometry and completed a medical questionnaire about contact history and symptoms while on their bus. Nurses checked the returnee questionnaires and took body temperatures during transport; those with respiratory symptoms (nasal discharge, sore throat, cough, etc.) or fever ≥37.5°C were taken to an examination room, where a physician performed a pharyngeal swab and rapid tests for influenza. Except for cases where clinical symptoms were clearly judged unlikely to be indicative of COVID-19, the individuals were admitted to the NCGM or to other hospitals in Tokyo for isolation. Those who had no problems according to the questionnaire or a normal temperature on the bus were examined in a large hall, and pharyngeal swabs were collected. Anyone with any respiratory tract symptoms or fever >37.5°C at the time of the physician’s consultation in the large hall were further examined in the consultation room and admitted to the NCGM or other hospitals in Tokyo, except for cases where clinical symptoms were clearly judged not to be COVID-19. Those who did not need hospitalization after the consultation at NCGM were moved to another accommodation facility and were instructed by the government not to leave the room for 12 days. Individuals who developed a fever or respiratory symptoms during the 12 days of quarantine at the accommodation were hospitalized for PCR and were admitted to an isolation room if SARS-CoV-2 was positive. On the 13th day after returning to Japan, a second PCR of the pharyngeal swab was performed, and those who tested negative were released from isolation at the accommodation facility and returned home. Those who tested positive were hospitalized and isolated.
Figure 1.
Flow of 566 people returning from Wuhan on a charter flight. Cases surrounded by red line represent polymerase chain reaction positives. Abbreviation: PCR, polymerase chain reaction.
Collected pharyngeal swabs were sent to the National Institute of Infectious Diseases (NIID), Tokyo, Japan, for real-time reverse transcriptase (RT)–PCR of SARS-CoV-2. Real-time RT-PCR for SARS-CoV-2 was performed using a QuantiTect probe 1-step RT-PCR kit (Qiagen) with the following probe and primer sets: WuhanCoV-spk2-f 5’-TTTCCTCGTGAAGGTGTCTTTGT-3′, WuhanCoV-spk2-r 5’-TGTGGTTCATAAAAATTCCTTTGTG-3′, and WuhanCoV-spk2-hex-p 5’-HEX-TCAAATGGCACACACTGGTTTGT-BHQ1 targeting spike gene (24843–24916 in GenBank accession MN908947); WuhanCoV-N1f 5′-GGCCGCAAATTGCACAAT-3’, WuhanCoV-N1r 5′-CCAATGCGCGACATTCC-3’, and WuhanCoV-N1pr-fam 5′-FAM-CCCCCAGCGCTTCAGCGTTCT-TAMRA-3’ targeting nucleoprotein gene (29191–29251 in MN908947). Symptomatic patients with positive PCR results were confirmed as having COVID-19 and continued their hospitalization and isolation. Treatment was decided at the discretion of each hospital. Data on the clinical course from the date of onset were collected.
Asymptomatic persons with a positive PCR result were admitted to a medical institution for follow-up and isolation. For asymptomatic PCR-negative persons who stayed at the accommodation facility, the PCR test was repeated on the 13th day. Those with negative results were allowed to return home, and those with positive results were transported to a medical institution for follow-up and isolation. As with symptomatic patients, clinical data were collected starting on the date of return. Because under Japan’s infectious disease law COVID-19 patients could not be discharged from the hospital until 2 negative PCR tests were confirmed, PCR tests were performed 24 hours after symptom improvement for symptomatic patients and asymptomatic patients as appropriate after hospitalization.
This study was approved by the ethics committee of the NCGM and all hospital institutions involved (approval No. NCGM-G-003475-00), and informed written consent was obtained from all returnees, except for 2 who refused medical consultation.
The basic characteristics of PCR-positive and -negative cases were examined using the Fisher exact test for categorical variables and Mann-Whitney U test for quantitative variables.
RESULTS
A total of 566 Japanese Wuhan residents returned to HND from WUH on January 29, (n = 206), January 30 (n = 210), and January 31 (n = 150), 2020. Two were excluded from this study because they refused the PCR test. After going through quarantine for about 2 hours each, 28 people at a quarantine station had symptoms of SARS-CoV-2 and were transported to a medical facility in Tokyo. A total of 536 people judged to have no symptoms suspicious of SARS-CoV-2 at the quarantine station were transported to the NCGM, while 36 patients with a fever >37.5°C or any respiratory symptoms were hospitalized at the NCGM or other Tokyo medical facilities. Moreover, 500 were judged to be asymptomatic and moved to an accommodation facility after sample collection (Figure 1). Table 1 shows the characteristics of the persons evacuated from Wuhan to Japan. The proportion of PCR-positive individuals who used any drug was higher than that of those who tested negative with the PCR. When the basic characteristics of the patients (age, sex, contact histories, symptoms) were compared between the 2 groups, no significant differences were observed, except for the number of patients who had a fever (P < .043).
Table 1.
Characteristics of Evacuated People From Wuhan to Japan, January 2020
| PCR Positive | PCR Negative | P Valuea | |
|---|---|---|---|
| No. | 11 | 553 | |
| Median age (range), y | 49 (30–65) | 42 (1–70) | .042 |
| Male, No. (%) | 8 (72.7) | 511 (92.4) | .050 |
| Arrival date, No. (%) | |||
| Jan 29 | 5 (45.5) | 199 (36.0) | |
| Jan 30 | 3 (27.3) | 207 (37.4) | |
| Jan 31 | 3 (27.3) | 147 (26.6) | |
| Contact history, No. (%) | |||
| Contact with person(s) with respiratory symptoms | 1 (9.1) | 73 (13.2) | 1.0 |
| Contact with COVID-19 patients | 1 (9.1) | 24 (4.3) | .396 |
| Fever (quartile range), ºC | 36.9 (36.7–37.3) | 36.7 (36.5–36.9) | <.043 |
| Respiratory symptoms, No. (%) | 3 (27.3) | 60 (10.8) | .114 |
| Cough | 2 (18.2) | 37 (6.7) | .173 |
| Runny nose | 1 (9.1) | 26 (4.7) | .420 |
| Sore throat | 0 (0) | 15 (2.7) | 1.0 |
| Sputum | 0 (0) | 2 (.4) | 1.0 |
| Headache, No. (%) | 0 (0) | 5 (.9) | 1.0 |
| Fatigue, No. (%) | 0 (0) | 14 (2.5) | 1.0 |
| Other, No. (%) | 0 (0) | 11 (2.0) | 1.0 |
| Any drug use, No. (%) | 2 (18.2) | 16 (2.9) | .045 |
Abbreviations: COVID-19, coronavirus disease; PCR, polymerase chain reaction.
aFisher exact test for categorical variables and Mann-Whitney U test for quantitative variables.
Three out of the 206 passengers on the first flight had a positive SARS-CoV-2 PCR result for pharyngeal swabs collected on January 29. One of them was already isolated in a private patient room of a medical institution as a symptomatic patient (patient S1), but 2 were asymptomatic and stayed at the accommodation facility. The 2 asymptomatic individuals were transported to a medical institution, where they were isolated and carefully monitored (patients A1 and A2). Among those patients transported directly from the quarantine station to a medical institution, all had negative results on the first test. Among them, 1 person who had pneumonia and was strongly suspected of COVID-19 was retested and found to be positive (patient S2) on January 31. One of the patients staying at the accommodation who was reported to be ill with a fever and sore throat was transported to the hospital and isolated on February 6 (Patient S3); subsequently, pharyngeal swabs collected on February 7 tested positive for PCR. In addition, 201 people who tested negative on the first PCR were all negative on PCR tests performed in February 11. Only 2 asymptomatic patients of the 210 passengers on the second flight had positive PCR results on January 30; they were transported from the accommodation facility to a medical facility (patients A3 and A4) on January 31. Another person who initially had negative pharyngeal swab results was retested because of the development of pneumonia and was found to be positive (patient S4) on February 3. Fortunately, 207 people who tested negative on the first PCR all tested negative on February 12. Two of the 150 passengers on the third flight were positive with the first PCR test: 1 was already isolated in a medical institution (patient S5), and the other was asymptomatic and stayed in an accommodation facility (patient A5). One asymptomatic person of the 148 people who tested negative on the first PCR tested positive on a second PCR on February 13 (A6). The details of the 11 PCR-positive patients (S1–S5, A1–A6) are summarized in Table 2.
Table 2.
Detail Clinical Information of PCR Positive 11 Patients
| Age | Gender | Arrival Date | Onset | First PCRScreening on Arrival | Additional PCRBased on Clinical Symptoms | Second PCRScreening at Day 12 | Comorbidities | Exposure With Confirmed Cases in Wuhan | Exposure to ILI | URI Symptoms at First Consultation | BT at First Consultation, ℃ | Complication | Outcome | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptomatic | S1 | 50s | M | 29 Jan | 29 Jan | Positive (29 Jan) | NA | NA | None | No | No | Runny nose,sore throat | 37.1 | Viral pneumonia | Discharged on 22 Feb |
| S2 | 40s | M | 29 Jan | 26 Jan | Negative (29 Jan) | Positive (31 Jan) | NA | None | No | No | Cough,headache, conjunctivitis | 37.6 | Viral pneumonia | Discharged on 13 Feb | |
| S3 | 50s | M | 29 Jan | 6 Feb | Negative (29 Jan) | Positive (7 Feb) | NA | None | No | No | Cough, shortness of breath | 38.5 | Viral pneumonitis | Discharged on 14 Feb | |
| S4 | 50s | F | 30 Jan | 30 Jan | Negative (30 Jan) | Positive (3 Feb) | NA | None | Yes (19 Jan) | No | Diarrheacoughsore throat | 37.5 | Viral pneumonia | Discharged on 14 Feb | |
| S5 | 40s | M | 31 Jan | 31 Jan | Positive (31 Jan) | NA | NA | None | No | No | Cough | 38.2 | Viral pneumonitis | Discharged on 22 Feb | |
| Asymptomatic | A1 | 40s | M | 29 Jan | 31 Jan | Positive (29 Jan) | NA | NA | None | No | No | None | 36.3 | None | Discharged on 1 Mar |
| A2 | 50s | F | 29 Jan | None | Positive (29 Jan) | NA | NA | None | No | No | None | 36.4 | None | Discharged on 13 Feb | |
| A3 | 30s | M | 30 Jan | None | Positive (30 Jan) | NA | NA | None | No | No | None | 37.1 | None | Discharged on 14 Feb | |
| A4 | 50s | M | 30 Jan | 31 Jan | Positive (30 Jan) | NA | NA | None | No | No | None | 36.9 | None | Discharged on 26 Feb | |
| A5 | 30s | M | 31 Jan | None | Positive (31 Jan) | NA | NA | Mild liver disease | No | No | None | 36.6 | None | Discharged on 19 Feb | |
| A6 | 60s | F | 31 Jan | None | Negative (31 Jan) | NA | Positive (13 Feb) | None | No | No | None | 36.6 | None | Discharged on 21 Feb |
Abbreviations: BT, body temperature; Feb, February; F, female; ILI, influenza-like illness; Jan, January; M, male; Mar, March; PCR, polymerase chain reaction; URI, upper respiratory infection.
Notably, among the 11 PCR-positive individuals, 5 had symptoms due to COVID-19 at the time of sample collection (patients S1–S5). At the time of admission, 3 had a fever ≥37.5°C, 3 had cough, and 2 had sore throat. Four of the 5 symptomatic individuals had pneumonia on admission, and the other (S1) developed pneumonia on the ninth day. All 5 symptomatic patients were mild and discharged without any sequela. They did not receive mechanical ventilation and were not admitted to the intensive care unit.
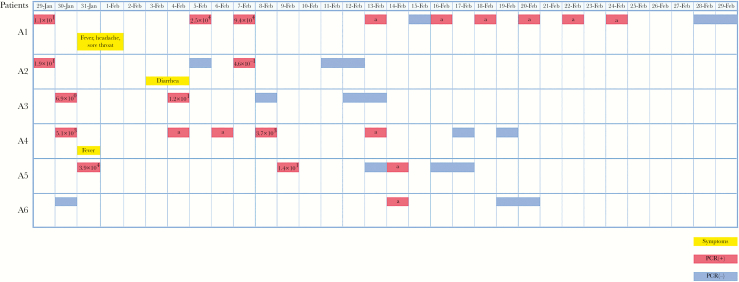
Patient A1, who was initially asymptomatic, had a fever of 38.9°C with headache and sore throat 3 days after the first PCR screening test. The result of the rapid influenza test was negative. Fever and other symptoms lasted for only 1 day, after which they disappeared. Patient A2 had diarrhea (5 times per day) without fever or any other respiratory symptoms at day 6, which lasted about 1 day. Patient A4 had a fever of 38°C when transported from the accommodation facility to the hospital (day 2), but the temperature immediately dropped to 37.2°C, and no fever or respiratory symptoms were seen thereafter. The remaining 3 of the 6 were consistently asymptomatic from the date of admission to the date of discharge. These 6 asymptomatic individuals were carefully monitored at the hospital, pharyngeal swabs were collected, and PCR tests were conducted as appropriate, and where possible, the viral load was measured (not necessarily measured every time) (Figure 2). The PCR tests of pharyngeal swabs of 3 asymptomatic individuals yielded positive results for 10 days. One of them was positive for SARS-CoV-2 by PCR on day 27. As of March 8, none of the patients who tested negative for the second PCR had been diagnosed with COVID-19.
Figure 2.
Clinical symptoms and virus copy numbers in pharyngeal swab samples of 5 patients with severe acute respiratory syndrome–related coronavirus 2 (SARS-CoV-2) infection. Copy numbers in 1 μL of the swab samples were measured with real-time reverse transcription polymerase chain reaction (RT-PCR) targeting the SARS-CoV2 N1 gene. aPositive results of A1, 4, 5, and 6 patients were obtained with real-time RT-PCR, but not quantified.
DISCUSSION
We reported the results of 2 PCR tests on 564 returnees from Wuhan and the course of positive results of the 564 returnees, 11 were of whom were PCR-positive (2.0%), which far exceeded our expectations. According to WHO situation report, the number of confirmed SARS-CoV-2 patients in mainland China on January 29 was 5997 [9], which accounts for only 0.054% of the population of Wuhan and is significantly different from the positive rate of Japanese returnees. However, an analysis indicated that there were already 75 815 infected people in Wuhan as of January 25, 2020 [10]. From our reported number of positive PCR results, it is estimated that Wuhan has more infections than reported. As of March 21, 2020, several cities around the world have locked down in addition to Wuhan. Our results will provide important insights on responding to returnees from these locked-down cities.
Returnees were first sent to a quarantine station where patients suspected to have COVID-19 were transported to a hospital in Tokyo. Additionally, of the 28 people transported from the quarantine to the hospital, only 1 was positive for COVID-19. Ten of the 11 persons with positive result were sent to the NCGM with a low likelihood of infection, and the quarantine station detected 9.1% of those positive for COVID-19. Although Quilty et al. [11] estimated that 46% of patients will be missed in quarantine screening, this cohort study may have reduced the rate of detection because of the higher proportion of asymptomatic individuals. To find and isolate COVID-19 patients among the returnees, they were asked to fill out a simple questionnaire after they were transported from the quarantine station to the NCGM. However, there was no difference between the positive and negative cases regarding the history of contact with patients and the history of contact with patients with influenza-like illness symptoms. The presence of upper respiratory symptoms was not effective for screening, but fever might be effective; among the PCR-positive symptomatic cases, all had fever, but the respiratory tract symptoms varied, and 1 patient initially had diarrhea only aside from fever. This suggests the difficulty of detecting COVID-19 by symptoms alone. Naturally, it is not possible to detect asymptomatic patients among PCR-positive cases using a questionnaire. In the early stages of the COVID-19 epidemic, many cases were associated with the seafood market, and it was speculated that some wildlife in the seafood market was the source of infection. At this time, the host of SARS-CoV-2 had not been determined, but it was known that bat coronavirus had high homology with SARS-CoV-2 [12, 13] and that bats were sold in the seafood market. However, as the seafood market was closed on January 1, 2020 [5], and >14 days had passed since the closure, this questionnaire did not include a history of visit to the seafood market. Nevertheless, we found 11 SARS-CoV-2 PCR-positive cases. This suggests that the outbreak was already being driven by human-to-human infection, regardless of the origin of index cases. Among the 11 positives, the first PCR screening found 7 positives, but 4 were negative. In other words, 1 screening PCR test missed 36% of true positives who were still in the incubation period at the time of the first PCR screening or just because of false-negative results. Based on reports that 95% of cases develop within 12.5 days of exposure [5], we performed a second PCR test on the 13th day of return. Hoehl et al. reported 126 evacuated Germany passengers from Wuhan to Frankfurt [14]. In this report, 1.8% of returnees had passed the symptoms-based screening and were later found to have evidence of SARS-CoV-2 on pharyngeal swab. In our study, of the 11 positives among 564 passengers, 10 passed quarantine screening, 7 passed symptoms-based screening at NCGM, and 2 had a negative initial PCR. Our report is consistent with their report that symptom-based screening was ineffective and that about 2% of returnees from Wuhan were positive. However, to screen patients with high infection rates, such as those returning from Wuhan, a single PCR test may miss cases that develop after the incubation period, and a second PCR might be effective.
Furthermore, of the 11 cases in this study, only 1 was exposed to a confirmed case of COVID-19. In addition, we found SARS-CoV-2 in 2.0% of all subjects. These results might suggest 3 hypotheses. First, contact history is not a significant risk factor for infection. Previous reports have suggested that few people in contact with COVID-19 patients develop COVID-19 [15] and that certain clusters are prone to outbreaks [16]. Transmission might depend on the environment at the time of contact with the confirmed patient. Second, SARS-CoV-2 can be transmitted from cases other than those with symptoms. Rothe et al. [17] reported that asymptomatic individuals were infectious. In addition, patients 3 and 4 had no exposure to the index case, and only patient 2 had contact with patient 1, who was then asymptomatic. This suggests that COVID-19 is infectious during the asymptomatic period or that it is infectious even during the incubation period. In addition, several reports suggesting infection from asymptomatic infected people have been published [18,19]. Other respiratory viruses such as seasonal influenza can also be transmitted by asymptomatic cases [20]; therefore, it is possible that asymptomatic individuals with the same respiratory SARS-CoV-2 infection are infectious. Third, returnees might have underestimated or forgotten their contact history. As the evacuation process in these circumstances is stressful for healthy and asymptomatic people, their self-reported contact history could be biased. Additionally, it is possible that they simply forgot their contact history.
There were 6 cases of asymptomatic COVID-19; these 6 asymptomatic individuals had 2 consultations at the quarantine station and at the NCGM before being transported to a hospital and were arguably asymptomatic at the time of the SARS-CoV-2 PCR test. In similar coronavirus infections, namely severe acute respiratory syndrome and Middle East respiratory syndrome, a certain percentage of infected people have asymptomatic infections [21,22]; thus, it was not surprising that there were individuals with COVID-19 who were asymptomatic. Two of them had a fever during the course, and the viral load indicates that the patients developed COVID-19. This fact suggests that PCR-positive findings on pharyngeal swabs might reflect very early onset. Nishiura et al. estimated the serial interval to be 4 days shorter than the incubation period, which might reflect the fact that there were a certain number of cases with SARS-CoV-2 in the pharynx before the day of onset of symptoms [23]. Meanwhile, the remaining 4 patients remained asymptomatic. Three of the 6 asymptomatic infections remained positive for SARS-CoV-2 PCR on pharyngeal swab for >15 days, and 1 of them was positive for 27 days. In addition, 4 out of 6 asymptomatic individuals were PCR-positive 10 days after their first positive test. Zou et al. reported that SARS-CoV-2 was detected on nasopharyngeal and pharyngeal swabs of asymptomatic patients for 4 days (from 7 to 11 days after contact with COVID-19 patients) [5]. It is reasonable to conclude that the 2 individuals who developed SARS-CoV-2 symptoms were still PCR-positive, but it is surprising that the 2 cases who did not develop SARS-CoV-2 symptoms were also positive 10 days later. These results suggest that if an asymptomatic person were infectious, the infection would persist for an extended period. The viral shedding duration and transmission potential of SARS-CoV-2 infection may be longer than those of other respiratory viruses such as seasonal influenza [20].
Our study has some limitations. First, PCR screening was performed using pharyngeal swab samples in this study. The use of lower respiratory tract specimens is optimal for diagnosing COVID-19 [2]. Pharyngeal swabs are less sensitive than nasal swabs [24] and lower respiratory tract specimens; thus, this method may not be able to detect all infected individuals among returnees. Second, as mentioned above, our contact history tracing was based on self-reported answers and thus could have been biased. Although contact history does not seem to be as useful as we expected for identification of infected cases, further investigation would be desirable for this issue. Third, after the second positive PCR, the observation was concluded, and no one in the population has subsequently been diagnosed with COVID-19; however, if any of these individuals had asymptomatic infection after the second PCR, this study did not detect it.
In conclusion, we screened 564 returnees from Wuhan, of whom 11 were positive for SARS-CoV-2. Our report provides important evidence on the existence of asymptomatic individuals infected with SARS-CoV-2 and insights into the epidemic situation, where infected people are spreading the infection in Wuhan at least among the Japanese resident community. A 13-day observation period and a second round of PCR may be effective to screen all patients, including those with asymptomatic infections.
Acknowledgments
We acknowledge Dr. Masayuki Hojo, Dr. Shinyu Izumi, Dr. Masao Hashimoto, Dr. Jin Takasaki, Dr. Manabu Suzuki, Dr. Keita Sakamoto, Dr. Hiroyuki Shichino, Dr. Junko Yamanaka, Dr. Masao Kaneshige, Dr. Kobayashi Toshiaki, Dr. Yukio Hiroi, Dr. Sakurako Emoto, Dr. Koichiro Tomiyama, Dr. Makoto Tokuhara, Dr. Fumihiko Nakamura, Dr. Motoyuki Tsuboi, Dr. Masataro Norizuki, Dr. Yoshiaki Gu, Dr. Nobuaki Matsunaga, Dr. Yoshiki Kusama, Dr. Yumiko Fujitomo, Dr. Ayako Okuhama, Dr. Kohei Kanda, Ms. Yuko Sugiki, Ms. Chiharu Nonaka, and all health care workers at the NCGM who were involved in this study. We thank the COVID-19 NIID Evacuation Flight Laboratory Testing Team (NEFLATT; Dr. Akira Ainai, Dr. Shun Iida, Dr. Hideki Hasegawa, Dr. Naoko Iwata-Yoshikawa, Dr. Tsutomu Kageyama, Dr. Takayuki Kanno, Dr. Fumihiro Kato, Dr. Hiroshi Katoh, Dr. Shutoku Matsuyama, Dr. Noriyo Nagata, Dr. Noriko Nakajima, Dr. Yuichiro Nakatsu, Dr. Naganori Nao, Dr. Noriyuki Otsuki, Dr. Shinji Saito, Dr. Masafumi Sakata, Ms. Kaori Sano, Ms. Yuko Sato, Dr. Kenji Someya, Dr. Maino Tahara, Dr. Kenta Takahashi, Dr. Ikuyo Takayama, Dr. Makoto Takeda, Dr. Michiko Tanaka, Dr. Minoru Tobiume, Dr. Kenzo Tokunaga, Dr. Yuji Wada) at the National Institute of Infectious Diseases and Kazuhisa Yoshimura, Kenji Sadamasu, Takashi Chiba, Mami Nagashima, and the Tokyo Metropolitan Institute of Public Health for performing the SARS-CoV-2 PCR test on passengers at the time of arrival in Japan. We also thank Dr. Kazuhisa Yokota, Dr. Aya Tamiya, and Dr. Yoshito Aramaki of Ebara Hospital and Dr. Taiichiro Kobayashi, Dr. Masaru Tanaka, and Dr. Sho Fujiwara of Tokyo Metropolitan Cancer and Infectious Diseases Center, Komagome Hospital, for their clinical support.
Financial support. This work was supported by a grant from the Japan National Center for Global Health and Medicine (grant No. 29–1018). The work was supported in part by the Emerging/Re-emerging Infectious Diseases Project of Japan, from the Japan Agency for Medical Research and Development (grant No. JP19fk0108104).
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. World Health Organization. Pneumonia of unknown cause—China. Available at: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/. Accessed 15 March 2020.
- 2. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382:727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020; 382:1199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323:1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) Available at: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). Accessed 14 March 2020.
- 8. Phan LT, Nguyen TV, Luong QC, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med 2020; 382:872–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization. Novel coronavirus (2019-nCoV) situation report—9 Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200129-sitrep-9-ncov-v2.pdf?sfvrsn=e2c8915_2. Accessed 14 March 2020.
- 10. Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 2020; 395:689–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Quilty BJ, Clifford S, Flasche S, Eggo RM; CMMID nCoV working group. effectiveness of airport screening at detecting travellers infected with novel coronavirus (2019-nCoV). Eurosurveillance 2020; 25:2000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395:565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020; 579:270–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hoehl S, Berger A, Kortenbusch M, et al. Evidence of SARS-CoV-2 infection in returning travelers from Wuhan, China. N Engl J Med 2020; 382:1278–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Burke RM, Midgley CM, Dratch A, et al. Active monitoring of persons exposed to patients with confirmed COVID-19 - United States, January-February 2020. MMWR Morb Mortal Wkly Rep 2020; 69:245–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Japanese National Institute of Infectious Diseases. Field briefing: diamond princess COVID-19 cases, 20 Feb update Available at: https://www.niid.go.jp/niid/en/2019-ncov-e/9417-covid-dp-fe-02.html. Accessed 1 March 2020.
- 17. Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med 2020; 382:970–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020; 323:1406–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yu P, Zhu J, Zhang Z, Han Y, Huang L. A familial cluster of infection associated with the 2019 novel coronavirus indicating potential person-to-person transmission during the incubation period. J Infect Dis 2020; 221:1757–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ip DK, Lau LL, Leung NH, et al. Viral shedding and transmission potential of asymptomatic and paucisymptomatic influenza virus infections in the community. Clin Infect Dis 2017; 64:736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wilder-Smith A, Teleman MD, Heng BH, et al. Asymptomatic SARS coronavirus infection among healthcare workers, Singapore. Emerg Infect Dis 2005; 11:1142–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Al-Tawfiq JA, Gautret P. Asymptomatic Middle East respiratory syndrome coronavirus (MERS-CoV) infection: extent and implications for infection control: a systematic review. Travel Med Infect Dis 2019; 27:27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nishiura H, Linton NM, Akhmetzhanov AR. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis 2020; 93:284–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med 2020; 382:1177–9. [DOI] [PMC free article] [PubMed] [Google Scholar]