Abstract
Objectives
We describe our approach in using health information technology to provide a continuum of services during the coronavirus disease 2019 (COVID-19) pandemic. COVID-19 challenges and needs required health systems to rapidly redesign the delivery of care.
Materials and Methods
Our health system deployed 4 COVID-19 telehealth programs and 4 biomedical informatics innovations to screen and care for COVID-19 patients. Using programmatic and electronic health record data, we describe the implementation and initial utilization.
Results
Through collaboration across multidisciplinary teams and strategic planning, 4 telehealth program initiatives have been deployed in response to COVID-19: virtual urgent care screening, remote patient monitoring for COVID-19–positive patients, continuous virtual monitoring to reduce workforce risk and utilization of personal protective equipment, and the transition of outpatient care to telehealth. Biomedical informatics was integral to our institutional response in supporting clinical care through new and reconfigured technologies. Through linking the telehealth systems and the electronic health record, we have the ability to monitor and track patients through a continuum of COVID-19 services.
Discussion
COVID-19 has facilitated the rapid expansion and utilization of telehealth and health informatics services. We anticipate that patients and providers will view enhanced telehealth services as an essential aspect of the healthcare system. Continuation of telehealth payment models at the federal and private levels will be a key factor in whether this new uptake is sustained.
Conclusions
There are substantial benefits in utilizing telehealth during the COVID-19, including the ability to rapidly scale the number of patients being screened and providing continuity of care.
Keywords: telehealth, informatics, pandemic, health systems
INTRODUCTION
The World Health Organization declared coronavirus disease 2019 (COVID-19) a global pandemic on March 11, 2020.1 To ensure safety and meet patient needs, health systems adjusted care processes and deployed new approaches to screen and care for COVID patients, and continue to meet routine care needs.2 On March 17, 2020, telehealth benefits were expanded for Medicare patients, and these regulatory and reimbursement mechanisms allowed healthcare organizations to support the conversion of ambulatory clinic visits to telehealth platforms.3 The Medical University of South Carolina (MUSC), like many healthcare institutions, experienced a dramatic reduction in ambulatory operations following government social distancing guidelines and increased demand for COVID-19 screening and testing. As 1 of 2 federally recognized telehealth Centers of Excellence,4 MUSC integrated and deployed telehealth into multiple facets of our institutional response to COVID-19. We deployed 4 COVID-19 telehealth programs and 4 biomedical informatics innovations during the initial weeks of the pandemic. The purpose of this study is to describe our approach to using health information technology to provide a continuum of services for COVID-19. We describe our processes, utilization, and lessons learned in using telehealth for screening and testing, reducing healthcare worker exposure, and transforming outpatient to virtual or telehealth care.
MATERIALS AND METHODS
Study site
MUSC began its first telehealth programs in 2005 as a strategy to mitigate health disparities experienced by many South Carolinians.5–7 Over the last 15 years, we have been on the vanguard of developing and deploying telehealth programs, and in 2019 had 390 000 telehealth interactions, offered 119 telehealth services in 42 (of 46) SC counties, at 346 sites (40 hospitals, 161 outpatient clinics, 112 schools, 33 other).
Telehealth response
When the first U.S. COVID-19 case was reported in January 2020, we initiated telehealth COVID-19 response activities. Initial steps included ensuring that all providers had telehealth clinical privileges, inventorying technology, outlining a telehealth response plan, and redeploying personnel to support new initiatives. We identified telehealth modalities and biomedical informatics resources that we could re-engineer or develop de novo to deploy for our telehealth COVID-19 response. Four telehealth initiatives have been deployed thus far: virtual urgent care, remote patient monitoring, continuous virtual monitoring (aka “tele-sitter”), and ambulatory care transformation. While these are synergistic programs, operationally different clinical teams support the different patient care needs.
Biomedical informatics
MUSC’s Biomedical Informatics Center (BMIC)8 was integral to our institutional COVID-19 response, repurposing research teams to support clinical care. The BMIC developed and deployed several innovations. A population management tool was established via a dedicated registry in the Epic electronic health record (EHR) for patients with potential or confirmed COVID-19 diagnosis. This supported the telehealth screening, testing, remote home monitoring, and convalescence phases of disease and included a dashboard to follow patients based on risk and disease progression. Additionally, expansion of EHR capabilities for longitudinal care occurred. A telehealth and Epic MyChart (patient portal) (Epic Systems, Verona, WI) home monitoring system embedded in our EHR allowed nurses to enroll, triage, and follow COVID-19 patients at home using patient-reported outcome measures reported daily for 14 days. Next, we developed and integrated a smartphone app and patient sensors. The app extended the capabilities of the MyChart system with Bluetooth pulse oximeters and digital thermometers. Nurse case managers could choose to prescribe either the MyChart system or the app from Epic. Data from the app were passed back into Epic, through Microsoft Azure (Microsoft Corporation, Redmond, WA), after data cleaning and trend analyses.
The dedicated registry of COVID-19 patients is populated using the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)–positive diagnostic test as the trigger as well as all patients using virtual urgent care for COVID-19 suspicions (Supplementary Appendix). All COVID-19 nasopharyngeal testing submitted through MUSC was pulled into the registry for potential enrollment in home monitoring. Furthermore, all positive laboratory results, regardless of patient entry point (virtual urgent care, drive-up testing, emergency department, inpatient admission, or preoperative testing) populate the same registry. This comprehensive registry of patients was further parsed into smaller operational subgroups: (1) patients already contacted with results, (2) patients hospitalized at MUSC, (3) patients currently enrolled in remote patient monitoring (RPM), and (4) patients who discontinued from RPM (eg convalescent).
Finally, we applied artificial intelligence expertise to data coming from MUSC’s virtual urgent care platform (Zipnosis, Minneapolis, MN), which while rich in clinical information, was locked in the “free text” record. Our researchers developed natural language processing tools to extract symptoms, risk factors, and medication treatments from notes to add to the COVID-19 registry. A team applied deep learning neural networks to notes and developed models to predict which patients would eventually have positive SARS-CoV-2 results. Deep learning neural network algorithms offered substantial improvements over the rule-based algorithms and subsequently were used to prioritize scheduling of testing.9
Data
Our telehealth and information solutions systems were assessed for functionality and readiness to serve as data collection and monitoring systems along 2 dimensions: (1) patient-centered clinical service delivery and (2) management and research data collection capability. Our telehealth tracking, reporting, and service management systems and their linkages with our EHR system were assessed and new measures, and codes were added to ensure that SARS-CoV-2 tests would be captured for rapid reporting, and that telehealth process and delivery changes implemented were logged in “real time.”
We include COVID-19 related virtual visits, testing referrals, lab orders, positive tests, in-patient and remote home monitoring interactions, and ambulatory telehealth visits that occurred between March 7 and April 22, 2020. To calculate the relationship between the telehealth workforce risk-reduction service and personal protective equipment (PPE) cost savings, we utilize a micro-costing approach using standard cost weights representative of U.S. national costs and prices in April 2020.
RESULTS
Screening: COVID-19 and virtual urgent care
We redesigned our existing virtual urgent care (VUC) with the overall goal of keeping patients with symptoms away from typical healthcare access points such as clinics, urgent care settings, and emergency departments in order to reduce risk. VUC traditionally provides rapid access to care for low-risk clinical conditions (eg, urinary tract infections) among low-risk patient populations. Our VUC program, established in 2015, is supported by a team of emergency department–based advanced practice providers (APPs). Zipnosis is our technical platform because it provides both asynchronous (ie adaptive interview, chat) and synchronous (ie video, phone) capabilities. VUC served as a portal of entry into our EHR as the system creates a record for all new patients, allowing for test ordering, resulting, communication to the patient, population of the COVID-19 registry, and continuity with the remote patient monitoring program.
Re-engineering VUC to support screening for COVID-19 required numerous changes. We created and trained an emergency staffing pool of APPs from across the health system, as anticipated volumes would overwhelm the established VUC APP pool. This included privileging, credentialing, completing scope of practice agreements, finalizing a payment model, and receiving approval on a provider compensation mechanism through both our university and practice plan entities who employ the APPs. After a call to action on March 6, 2020, we trained over 100 APPs in <2 weeks. Next, we removed historical VUC restrictions based on age, comorbid conditions, and presence of dyspnea from the COVID-19 screener. Given the high-risk nature of COVID-19, we implemented a quality assurance program to review patient care decisions in real time, communicate information and clarifications with patients, and improve overall processes, as well as develop screening pathways for Spanish-speaking patients, vulnerable populations (eg homeless shelters), and patients without Internet access (ie phone screenings).
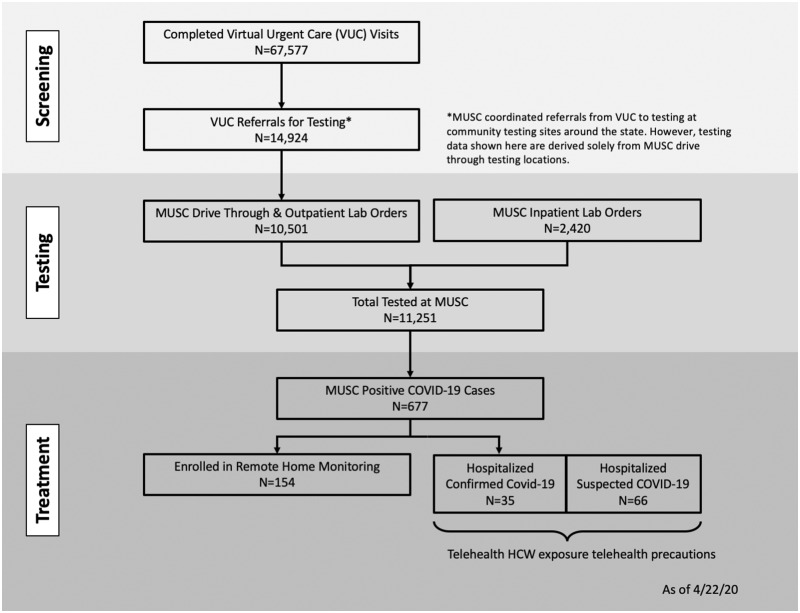
Between March 7 and April 22, 2020, 67 577 patients completed a VUC visit, of whom 14 924 met the criteria for COVID-19 testing. The availability of a COVID-19 virtual evaluation was promoted through institutional communications, local media, and state officials as a public health tool for South Carolina citizens to receive a no-charge virtual screening. Figure 1 provides the continuum of our COVID-19 care processes and patient volumes associated with each phase.
Figure 1.
Continuum of coronavirus disease 2019 (COVID-19) care processes between March 7 and April 22, 2020. HCW: healthcare worker; MUSC: Medical University of South Carolina; VUC: virtual urgent care.
SARS-CoV-2 testing
Institutional drive-through respiratory specimen collection sites were established at locations throughout the state. Further optimization enabled patients who qualified for testing to immediately receive a “ticket” allowing them to select a testing facility and self-schedule their test through our EHR patient portal. Via drive-through testing and outpatient labs, 10 501 patients were tested, an additional 2420 tests were performed among inpatients.
Treatment: Outpatients with COVID-19 and remote patient monitoring
We have substantial institutional experience with RPM for a variety of patient conditions including diabetes, hypertension, mental health, asthma, and pediatric burns to name a few.10–16 As part of our COVID-19 response, we developed an RPM program for outpatients with COVID-19.
The foundation of our COVID-19 RPM program is a parsimonious set of patient-reported outcomes (PROs) derived from a validated community acquired pneumonia patient questionnaire.17 This 5-item survey closely queries changes in patient reported dyspnea and is thus highly relevant to COVID-19, in which the most common cause of morbidity and mortality is progressive respiratory failure.18 This simple and feasible PRO became the foundation for monitoring the vast majority of COVID-19 patients who have mild-to-moderate symptoms.18 We also identified Bluetooth-enabled home pulse oximeters that met requisite technical, security, and usability requirements. We created a risk stratification tool based on underlying patient conditions and offer home pulse oximetry to select subgroups: high risk for COVID-19 complications, posthospitalization receiving oxygen therapy at home, and post–emergency department evaluation without hospitalization. Finally, a number of patients invited to participate in the RPM program already had thermometers and home pulse oximeters, and so we added patient reported biometric data into the PRO tool.
From an operational standpoint, patients may complete the PRO tool via their MyChart account or via the smartphone app developed by the BMIC. Patients enrolling in the app-based RPM program were provided with a 2-dimensional secure barcode that linked information entered into the app with their Epic accounts. Reminders to complete the PRO tool were pushed to the patient daily, and there was no limit on number of PRO tool completions per patient per day. Therefore, if symptoms worsen, patients could enter an updated PRO survey and the RPM nursing staff will reach out via phone.
As described previously, our biomedical informatics innovations enabled the development of a COVID-19 patient registry in Epic. Patients who completed a virtual urgent care evaluation for possible COVID-19 and screened as potentially positive populated the initial registry cohort. The registry was tiered such that patients testing COVID-19–positive populated the BMIC designed clinical dashboard which is utilized for purposes of the RPM program and supporting COVID-19 research initiatives. After confirming that patients testing COVID-19–positive had been informed of these results, RPM nurses contacted them to offer them the opportunity to enroll in our RPM program.
Our first weeks of experience in providing RPM for COVID-19 patients has provided the following observations. Out of the 677 COVID-19–positive patients in our registry, we offered the program to 336 patients. Reasons for exclusion in RPM monitoring included missing contact information, pediatric cases, and current admission in an inpatient or long-term care facility. Of the patients offered access, 154 patients were enrolled, of whom 10.4% were designated as high risk for complications based on underlying age or health conditions. Among this cohort of patients, we have had 709 nurse-to-patient encounters, 22 were referred for physician review, 6 were physician-to-patient phone calls, and 4 were referred to their local emergency department and hospitalized. Among the 182 patients that opted not to enroll in the program, the most common reason was that they were feeling better but were appreciative of the resource offering.
Risk reduction: Using telehealth to reduce healthcare worker COVID-19 exposure and PPE usage
In 2017, we developed a continuous virtual monitoring (CVM) program for remote oversight of hospitalized patients at increased risks of falls. The technology was developed and customized internally to insure reliable and high quality continuous audiovisual streaming, robust security/privacy protections, and ease of use for clinicians. This program has experienced significant institutional uptake, and in 2019, a total of 4721 inpatient days were monitored on 23 units, inpatient psychiatry wards, and the emergency department.
For purposes of responding to COVID-19, we conscripted the CVM technology and resource management systems and deployed these to inpatient negative pressure rooms (n = 30) where hospitalized patients are admitted for COVID-19 testing, COVID-19 cohort inpatient units, and emergency department COVID-19 screening tents. Specific technical components include Cisco DX desktop monitors (Cisco, San Jose, CA) that are placed in nursing stations and mobile carts with the CVM program’s 2-way audiovisual technologies placed in patient care areas. With regard to resource management, Cisco DX monitors and carts are deployed to patient areas with active COVID-19 care needs. This is achieved by having our lead CVM technicians communicate on a per-shift basis with the inpatient supervisors to ensure optimal resource use.
The Cisco DX monitors have each cart preprogrammed so that the clinician only needs to tap the appropriate cart icon and the cart is automatically “called” for audiovisual communication between clinicians and patients. In contrast to the CVM program, the COVID-19 CVM video feed is not automatically turned on, and 2-way communication is only activated by the desktop Cisco DX as necessary. However, we have anecdotally observed that in our COVID-19 cohort intensive care unit, staff often utilize the continuous communication options when fully donned in PPE at patient’s bedsides to request supplies and report patient care information.
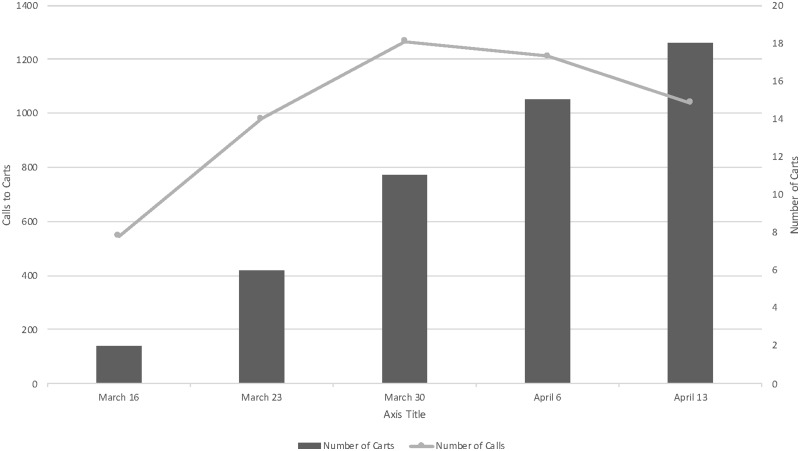
Implementation of this program began the week of March 16, 2020, and there has been accelerated utilization (Figure 2). Cumulatively, there have been 5042 calls into the CVM carts by a healthcare professional caring for COVID-19 patients. This represents a significant reduction in healthcare worker exposure and time spent donning and doffing PPE, and conservation of a substantial amount of PPE, assuming that these workers would have otherwise gone into the patient’s room. The estimated cost savings for this program as of April 22, 2020, were $105 624, not including any potential savings from avoided COVID-19 cases among healthcare workers. We estimated 354 monitoring cart days, at a cost of $14.11 per patient per day, including cleaning and setup. A total of 5042 PPE changes were avoided, with savings of $49 311 using a cost of $9.78 based on post–COVID-19 pandemic prices for mask, gown, gloves, and face shield,19 and $61 449 saved in nursing time from not donning (4 minutes) and doffing (6 minutes) PPE, estimated at a cost $12.19 per call based on median nurse salary rates and the Centers for Disease Control and Prevention–recommended PPE approach.20
Figure 2.
Implementation of monitoring carts and number of weekly calls: March 6 to April 13, 2020.
Outpatient care transformation: Converting to provider-patient video visits to support ambulatory care during COVID-19
MUSC leveraged the expanded federal telehealth policies to support the health system charge to increase ambulatory operational capacity to 80% of prepandemic levels through the integration of telehealth within all 48 ambulatory clinical divisions. The scale to accomplish the telehealth conversion across MUSC’s ambulatory setting, over a 30-day timeline, was transformative.
The process of implementing large-scale conversion of in-person visits to telehealth visits began in mid-March. The scope of the initiative was the conversion of in-person visits to synchronous video visits when appropriate. To initiate the telehealth conversion, a task force was constructed with governance representation from ambulatory care administration, clinical informatics, and telehealth. Subcommittees were formed to focus on provider and patient education, billing and compliance, and platform implementation. Physician leaders were identified in each clinical division and a through a series of webinars were able to coach their peers to enhance adoption. Initially implementation was focused on the processes and capabilities available through the existing video platform embedded within our patient portal.
As implementation progressed through the ambulatory divisions, limitations related to the existing video platform for large academic healthcare settings were quickly encountered. For some providers, the video platform embedded in the patient portal and was well adopted, and other clinics identified constraints within the platform to support common academic processes (ie visitation and review from both resident and attending). Additional system limitations were noted around ease of use, and technical and bandwidth accessibility when used at scale. To improve the system capabilities and technical barriers identified, a second, independent video platform was deployed (Doxy.me). The second platform already had an institutional instance on campus; moreover, the platform had capabilities to support security requirements, clinical academic processes, and ease of use, and had reliable technical capabilities.21 Infrastructure was then implemented to establish common workflows, patient and provider education, a standardized staffing support model, and adaptation of the EHR visit types to facilitate routing for billing. While providers were encouraged to use the newer platform, those who preferred to stay within the initial video platform were supported, and the processes and EHR were developed to support both systems.
A variety of approaches were used to educate patients. First, the video platform was converted to a web-based platform, which included built-in patient education features. Individual clinics onboarded patient education scripting, and clinic support staff prepped patients in advance of the visit. Technology checks were used by a minority of clinics. One barrier was that the patients do not have the ability to test their own connection in the video portal.
By the 30-day mark, clinic volumes for the enterprise were at 69% of the prepandemic levels, with 67% of the volume obtained through virtual care. Many departments had achieved 80% of prepandemic levels. Some departments such as psychiatry and primary care were exceeding their prepandemic clinical volumes. The interdisciplinary teams continue the collaboration in the growth and integration of the telehealth video platforms within the ambulatory setting at MUSC. In addition, medical students were brought on to assist with ambulatory video visits for departments who made specific requests that included an educational experience. This included assisting with patient education and the ambulatory video visit workflow. As the pandemic continues, a transition from rapid acceleration toward data-driven optimization is underway and includes identifying low uptake divisions and overcoming barriers, re-engineering patient communication and scheduling, and strategizing approaches to blend in-person and video visit clinic panels.
We maintain a dashboard of video to telephone conversion rates and at peak use 68% of all visits were done virtually, and of those 10%-15% are audio calls. Loss interactions are monitored as the rate of scheduled visits that are completed. From this metric, visit loss is <7%, which compares favorably to in-person baseline.
DISCUSSION
Health systems are attempting to find rapid responses to manage COVID-19 needs using telehealth and informatics.22–25 While many video or telephone only platforms struggled with the sudden spike in volume of visits, we were well positioned to serve our state’s population. Within a short time frame, we leveraged the health system’s existing telehealth and informatics infrastructure to deploy a continuum of services for the COVID-19 screening and treatment, which provides a unique combination of services across care settings. The asynchronous functionality was crucial during the initial wave of virtual urgent care screenings for COVID-19 due to very high patient volumes, during which it would have been impossible to accommodate through video or chat functions. The need for a quality assurance team also emerged quickly as an essential resource to oversee the program from a safety perspective. Additionally, this team was able to quickly pivot with regard to referral for testing, as our local testing capacity expanded and recommendations for which patients should be tested changed accordingly. The health system, like many around the world, established and is expanding walk-up and drive-through testing sites, and by using virtual urgent care as a common portal of entry, the system was able to streamline access. Finally, one important benefit of establishing a COVID-19 EHR registry derived from the initial virtual urgent visit was that a continuum of care was enabled, such that patient test results could be quickly viewed and the patient contacted with their status.
Collaboration between telehealth and biomedical informatics led to the adoption of RPM services to support COVID-19 patients that were well enough to remain at home. From a public health perspective, keeping patients at home helps preserve valuable medical resources for more severely ill patients, reduces well population exposures, and enhances the effectiveness of social distancing interventions. From a patient perspective, the RPM keeps patients connected to care, monitors for potential clinical decline, provides education and emotional support, and enables both video evaluation or safe referral for in-person evaluation when clinical status warrants. Our goal is to offer this supportive resource to patient’s within and external to our health system. This has required identifying patient primary care providers for RPM nurse backup when patient issues warrant escalation to a physician as well as deploying a team of primary care physicians when patients do not have one. Additionally, our biomedical informatics team has encountered substantial barriers with regards to deploying our app-based tool, primarily related to the companies that host these resources. Overall, the program has been extremely well received by patients, many of whom are understandably anxious about their diagnosis. Another benefit of both the registry and the RPM program has been a ready pool of volunteers for our health system’s convalescent plasma program and other emerging research opportunities.
Perhaps the greatest impact of our COVID-19 portfolio of programs has been the ability to conserve PPE during a time when the resources are scarce and healthcare systems are experiencing significant price gouging.19 Through adaptation of the existing CVM equipment, patients and healthcare workers were able to have 2-way conversations in nonemergency situations and thereby reduce the number of times employees had to enter the patient rooms. These benefits extended to bedside staff, consulting physician teams, and the treating physician team. For the subset of critically ill COVID-19 patients, staff were able to use the technology to have continuously open lines of communication between the fully donned bedside provider and staff outside. This enabled better overall resource management. An unintended consequence of deploying this system was the inevitable mission creep in which clinicians sought to deploy the technology for reasons other than the prespecified use case of reducing healthcare worker COVID-19 exposure. By developing a clear strategy and related goals, we largely eliminated mission creep concerns.
During a time of social distancing, we transformed ambulatory care delivery to achieve 69% of pre-COVID levels. This finding is similar to other systems that have rapidly transitioned in-person ambulatory visits to video visits.22,23 Yet these results remain rare, national trends show the number of visits to ambulatory practices declined by nearly 60% over this same time period, and telehealth services have not been able to fully displace in-person care.2 We anticipate that our efforts transitioning large swaths of our in-person ambulatory visits to video visits will ultimately be the most enduring aspect of the telehealth implementations to date. While we have experienced the typical challenges around technology and scheduling, uptake has nonetheless been brisk. Finally, strategies to include patient populations without ready access to video conferencing technologies remains an important barrier without a clear solution.
Although the utilization of telehealth to improve access to care is often touted in the literature, the adoption has remained slow, with only 8% of Americans reporting to have participated in a video visit.22,24COVID-19 has led to rapid growth in telehealth utilization and adoption by new providers.26 The expansion of telehealth reimbursement options at federal and private levels will be key determinant in whether this new uptake is sustained.
This study has several limitations. First the reporting of COVID-19 measures is not standardized27; therefore, our definitions may differ from others conducting similar work. Second, the real-time nature of the data reporting has the potential to undercount or miscategorize information. However, we utilized trained informaticists to export and clean the data to minimize risk. Last, this study describes the experiences and early results from one health system. It is possible the results are not generalizable to others. Yet, we suggest that other health systems have the opportunity to learn from our experiences to inform their own work.
CONCLUSION
COVID-19 has led to rapid expansion and utilization of telehealth and health informatics services. We found substantial benefits in utilizing telehealth during the COVID-19 pandemic, including the ability to rapidly scale the number of patients being screened, providing continuity of care during times of social distancing, and the ability to monitor and track patients through linking telehealth systems to the EHR.
FUNDING
This publication was supported by the Health Resources and Services Administration of the U.S. Department of Health and Human Services as part of the National Telehealth Center of Excellence Award (U66 RH31458-01-00). The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by Health Resources and Services Administration, U.S. Department of Health and Human Services, or the U.S. Government. This publication was supported, in part, by the National Center for Advancing Translational Sciences of the National Institutes of Health under Grant Number UL1 TR001450. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
AUTHOR CONTRIBUTIONS
All authors provided substantial contributions to the study design, acquisition, analysis, and interpretation of data; drafting and revising the manuscript; and final approval for publication and agree to be accountable for all aspects of the work.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
CONFLICT OF INTEREST STATEMENT
None declared.
Supplementary Material
REFERENCES
- 1.World Health Organization. WHO Director-General’s Opening Remarks at Media Briefing on COVID-19. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020 Accessed April 25, 2020.
- 2. Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. What impact has COVID-19 Had on outpatient visits. The Commonwealth Fund; 2020. https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits Accessed April 27, 2020.
- 3.Centers for Medicare and Medicaid Services. President Trump Expands Telehealth Benefits for Medicare Beneficiaries. CMS Newsroom. 2020. https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak Accessed April 27, 2020.
- 4.Health Resources and Service Administration. Telehealth Center of Excellence-MUSC. 2020. https://www.hrsa.gov/library/telehealth-coe-musc Accessed April 25, 2020.
- 5. Adams RJ, Debenham E, Chalela J, et al. REACH MUSC: a telemedicine facilitated network for stroke: initial operational experience. Front Neur 2012; 3: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lesher AP, Fakhry SM, DuBose-Morris R, et al. Development and evolution of a statewide outpatient consultation service: leveraging telemedicine to improve access to specialty care. Popul Health Manag 2020; 23 (1): 20–8. [DOI] [PubMed] [Google Scholar]
- 7. Valenta S, Harvey J.. 2019. Adapting ITIL for effective telehealth service management. Presented at the 2019 Health Information Management Systems Society Global Conference; February 11-15, 2019; Orlando, FL.
- 8.Medical University of South Carolina. Biomedical Informatics Center. 2020. https://medicine.musc.edu/departments/centers/bmic Accessed April 27, 2020.
- 9. Obeid JS, Davis M, Turner M, et al. An artificial intelligence approach to COVID-19 infection risk assessment in virtual visits: A case report [published online ahead of print May 25, 2020]. J Am Med Inform Assoc 2020. doi: 10.1093/jamia/ocaa105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Adams ZW, McClure EA, Gray KM, Danielson CK, Treiber FA, Ruggiero KJ.. Mobile devices for the remote acquisition of physiological and behavioral biomarkers in psychiatric clinical research. J Psychiatr Res 2017; 85: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chandler J, Sox L, Kellam K, Feder L, Nemeth L, Treiber F.. Impact of a culturally tailored mHealth medication regimen self-management program upon blood pressure among hypertensive Hispanic adults. Int J Environ Res Public Health 2019; 16 (7): 1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dahne J, Lejuez CW, Diaz VA, et al. Pilot randomized trial of a self-help behavioral activation mobile application for utilization in primary care. Behav Ther 2019; 50 (4): 817–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Egede LE, William JS, Voronca DC, Knapp RG, Fernandes JK.. Randomized controlled trial of technology-assisted case management in low income adults with Type 2 Diabetes. Diabetes Technol Ther 2017; 19 (8): 476–82. [DOI] [PubMed] [Google Scholar]
- 14. Garcia DI, Howard HR, Cina RA, et al. Expert outpatient burn care in the home through mobile health technology. J Burn Care Res 2018; 39 (5): 680–4. [DOI] [PubMed] [Google Scholar]
- 15. Gros DF, Lancaster CL, López CM, Acierno R.. Treatment satisfaction of home-based telehealth versus in-person delivery of prolonged exposure for combat-related PTSD in veterans. J Telemed Telecare 2018; 24 (1): 51–5. [DOI] [PubMed] [Google Scholar]
- 16. Teufel Ii RJ, Patel SK, Shuler AB, et al. Feasibility of real-time smartphone asthma monitoring for high risk children. JMIR Pediatr Parent 2018; 1 (2): e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lamping DL, Schroter S, Marquis P, Marrel A, Duprat-Lomon I, Sagnier P-P.. The community-acquired pneumonia symptom questionnaire: a new, patient-based outcome measure to evaluate symptoms in patients with community-acquired pneumonia. Chest 2002; 122 (3): 920–9. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19). 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html Accessed April 27, 2020.
- 19. Berklan JM. Analysis: PPE costs increase over 1,000% during COVID-19 crisis. McKnights Long-term Care News. 2020. https://www.mcknights.com/news/analysis-ppe-costs-increase-over-1000-during-covid-19-crisis/ Accessed April 27, 2020.
- 20.Centers for Disease Control and Prevention. Using Personal Protective Equipment (PPE). 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html Accessed April 19, 2020.
- 21. Agnisarman S, Narasimha S, Madathil C, et al. Toward a more usable home-based video telemedicine system: a heuristic evaluation of the clinician user interfaces of home-based video telemedicine system. JMIR Hum Factors 2017; 4 (2): e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mann DM, Chen J, Chunara R, Testa PA, Nov O.. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc 2020; 27(7): 1132–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reeves JJ, Hollandsworth HM, Torriani FJ, et al. Rapid response to COVID-19 health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc 2020; 27: 853–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc 2020; 27 (6): 957–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.AmericanWell. Amwell Telehealth Index: 2019. Consumer Survey 2019. https://business.amwell.com/resources/telehealth-index-2019-consumer-survey/ Accessed April 27, 2020.
- 26. Hollander JE, Sites FD.. The transition from reimagining to recreating health care is now. Catalyst NEJM 2020. Apr 8. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0093 Accessed April 27, 2020. [Google Scholar]
- 27. Wissel B, Camp V, Kouril PJ, et al. An interactive online dashboard for tracking COVID-19 in U.S. counties, cities and states in real time. J Am Med Inform Assoc 2020; 27(7): 1121–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.