In our recent editorial [1] we discussed the importance of knowledge mobilization (KM; defined as ‘a proactive process that involves efforts to transform practice through the circulation of knowledge within and across practice domains’ [2]) to the implementation of best practice to drive up the quality of care for patients. We acknowledged the role and importance of recognizing real-world context, providing examples of individual, organizational and national contextual factors that influence KM.
Since the publication of that editorial, the context of healthcare both nationally and internationally has changed substantially. The covid-19 pandemic has, and will continue to have, a significant impact on KM and the design and delivery of healthcare services. The commonly cited conclusion in KM is that ‘context is everything’, and we would like to add to this discussion and build upon our previous editorial in light of the covid-19 situation. This piece explores the impact of covid-19 on KM, in the context of musculoskeletal services, and the ways in which organizations can ‘lock in’ learning, after arguably the biggest challenge that healthcare services have ever experienced.
Over recent weeks, we have seen the ability of healthcare systems to rapidly and efficiently reconfigure services and pathways at pace and scale, in response to the urgent need to address the challenges posed by covid-19. Increased flexibility within healthcare systems to accommodate change has enabled knowledge to be translated and implementation decisions to be made, with traditional system processes and ‘red tape’ no longer being prohibitive. A potential enabler of this in the UK has been the cancellation of the NHS debt, which may have freed up both thinking and action by reducing a barrier to organizational change. Several other facilitators of KM that have arisen as a result of the change in context and have assisted the implementation of new ways of working are discussed below.
Collaborative approaches such as coproduction and working across boundaries (e.g. between healthcare and industry) bring domain-specific contextual knowledge together in a shared goal to ensure appropriate outputs for end users [3]. National and international collaboration has accelerated the uptake of innovation, product design and new models of care. We are witnessing improved health data sharing with NHS England (NHSE) to identify ‘at risk’ patients, enhanced communication between primary and secondary care, and massive and unprecedented collaboration in the musculoskeletal sector, for example coproduced content between Versus Arthritis and the British Society for Rheumatology regarding covid-19 risk, and between NHSE, NHS Improvement and the Chartered Society of Physiotherapy regarding self-management support (https://www.csp.org.uk/conditions/managing-pain-home).
Examples of widespread international collaboration include the rapid formation of an international registry of covid-19 in rheumatology patients (Covid-19 Global Rheumatology Alliance, https://rheum-covid.org/). Furthermore, the Joint Effort Initiative, a collaboration between international researchers and clinicians with an interest in the implementation of osteoarthritis models of care (endorsed by Osteoarthritis Research Society International) [4], has produced an international repository of online osteoarthritis programmes for healthcare professionals seeking solutions for patients who are unable to access ‘traditional’ interventions (https://www.keele.ac.uk/pcsc/research/impactacceleratorunit/ ).
The demand and ‘permission’ for service change has resulted in an increased capacity of organizations to identify and utilize relevant knowledge to address changing circumstances and optimize clinical care within the restraints of the pandemic [5, 6,]. The process of how knowledge is recognized, valued and applied to improve performance within organizations is well described in absorptive capacity theory [7], illustrating how the capacity of healthcare organizations affects their ability to translate different types of knowledge. This has been supported in the current context by the rapid availability of resources due to funding for technology. Innovations such as telemedicine and telehealth (telecommunication systems used to deliver healthcare remotely) [8] have been implemented swiftly across healthcare services globally, as a direct result of covid-19 [9]. Virtual healthcare services, including remote video or telephone consultations, are being embraced like never before in order for patients to have access to clinicians whilst staying at home [10]. Arguably, this change was largely inevitable and has been part of national and international healthcare strategies for some time [10], yet the necessity and belief in the capacity to drive evidence-based innovation, which has been technologically feasible for several years, was previously lacking .
The change in healthcare context has led to shared drivers, priorities and agendas across multiple stakeholder groups, in turn affecting the ways in which decisions are made. External technocratic levers, such as contractual requirements, are no longer the driver for change. Instead the motivation for change has come from within organizations, its direction informed by pragmatic, ‘coal face’ knowledge (and science) to accelerate decision making, all in response to the emergency circumstances. Resistance to change is lowered by both the collective sense of urgency and a reduced tolerance for reluctant individuals to dissent at a time of crisis. In recognizing that knowledge is dynamic and responsive to changing individual, professional and organizational demands, several forms of contextual knowledge (including research evidence and personal experience) are being readily amalgamated to ensure utility and relevance in practice.
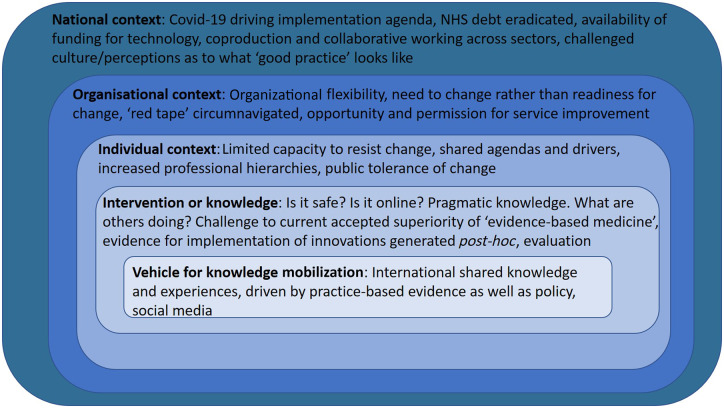
Considering the factors discussed, we have developed the figure from our previous editorial further to represent our reflections on the changed healthcare context in recent months. Figure 1 illustrates the contextual factors that affect KM during the covid-19 pandemic.
Fig. 1.
Factors affecting knowledge mobilization during covid-19
So, what may, or should, happen next?
Whilst we have outlined several facilitators of KM as a response to a change in context, it is important to consider the overall impact of rapid implementation, including the potential detrimental impacts. Implementing poorly evidenced interventions may subsequently prove to be at best ineffective, and at worst harmful. Furthermore, there may be opportunity costs for individual patient care associated with prioritizing services for covid-19 [11], and marginalized groups (including those without access to digital technologies and alternative communication requirements) may be excluded. Collaborative approaches have been seen between professional organizations and across sectors; however, the speed and urgency of change may have limited the scope for public involvement. Implementation has been driven by government, clinical or academic agendas, which can lead to patients and the public feeling excluded and services not aligned to their needs.
Established and protracted NHS pathways to innovation are now temporarily challenged by a context that is ‘pro-change’, whereby services and processes are being transformed at pace. The scale and speed of the uptake of innovative ways of working in response to covid-19 has led to gains that might otherwise have taken years to achieve. Despite the perceived public acceptance of new models of care, uncertainty exists regarding the anticipated, and unanticipated, short and longer term impacts of implementing new ways of working. With calls to ‘lock in’ learning as the pandemic subsides [12], continued acceptance and sustainability requires us to judge the merit and worth of change to maximize learning and guide future decision making. The extent to which new models of care should and do become embedded in routine practice or form hybrids of old and new models will be an evolving process in which KM can play its part. Successful transition will also depend on how next steps are coproduced with patients and the public.
Organizational learning regarding implementation requires ongoing reflection and continuous re-adjusting in the light of emerging evidence [13]. Robust evaluation and revision are key to ensuring that the impact (both positive and negative) of all change is assessed, shared and learned from. Clinicians and the services they lead have proved to be not only resilient, but highly adaptable when the context demanded it, accepting and applying different sources of knowledge to inform change. This reflects the role that context plays and the multifaceted, dynamic nature of KM in practice. However, maintaining change requires us to overcome the power of organizational memory ‘of how we used to’. It is important to refresh our organizational memory and ensure that we retain learning from the past 4 months to show that we can continue to rapidly acquire and use evidence.
Those responsible for the design, delivery and improvement of musculoskeletal services, in conjunction with patients, carers and the public, should use this period of change as an opportunity to learn from the best and ‘lock in’ change that delivers meaningful benefit to patients and payers. Whilst there is a risk of change fatigue, further change is inevitable. Strategic leadership is required at international, national, local and organizational levels to ensure that we continue to learn, ask the right questions to guide decision making and respond accordingly. We have seen that when necessary, we can rapidly make changes, reflect on them and change again. The current urgent context will soon fade. Before it does, we need to evaluate these new practices and find ways to ‘lock in’ learning, so that we continue to create and mobilize knowledge to meet our patients’ needs.
Acknowledgements
L.S. is funded by a National Institute for Health Research (NIHR) School for Primary Care Launching Fellowship. K.D. is part funded by the National Institute for Health Research (NIHR) Applied Research Centre (ARC) West Midlands. K.D. was also part funded by an NIHR Knowledge Mobilisation Research Fellowship (KMRF-2014-03-002) and is an NIHR Senior Investigator. C.S. is an NIHR Clinical Lecturer. The views expressed are those of the authors and not necessarily those of the NIHR, the NHS or the Department of Health and Social Care . We would like to thank the anonymous reviewer for their helpful suggestions.
Funding: No specific funding was received from any funding bodies in the public, commercial or not-for-profit sectors to carry out the work described in this manuscript.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1. Sharp CA, Swaithes L, Ellis B, Dziedzic K, Walsh N.. Implementation research: making better use of evidence to improve healthcare. Rheumatology 2020;59:1799–801. [DOI] [PubMed] [Google Scholar]
- 2. Swan J, Newell S, Nicolini D.. Mobilizing knowledge in health care: challenges for management and organization. Oxford: Oxford University Press, 2016. [Google Scholar]
- 3. Holmes BJ, Best A, Davies H. et al. Mobilising knowledge in complex health systems: a call to action. Evid Policy 2017;13:539–60. [Google Scholar]
- 4. Swaithes L, Dziedzic K, Cottrell E, Quicke J.. Response to: Losina E. Why past research successes do not translate to clinical reality: gaps in evidence on exercise program efficiency. Osteoarthritis and Cartilage 2019; 27: 1–2. Osteoarthritis Cartilage 2019;27:e7–e8. [DOI] [PubMed] [Google Scholar]
- 5. Currie G, Croft C, Chen Y, Kiefer T, Staniszewska S, Lilford R.. The capacity of health service commissioners to use evidence: a case study. Southampton (UK: ): NIHR Journals Library, 2018. [PubMed] [Google Scholar]
- 6. Lamount T. Learning from social sciences at a time of crisis. thebmjopinion, 2020. https://blogs.bmj.com/bmj/2020/04/24/tara-lamont-learning-from-social-sciences-at-a-time-of-crisis/ (4 June 2020, date last accessed).
- 7. Zahra SA, George G.. Absorptive capacity: a review, reconceptualization, and extension. Acad Manag Rev 2002;27:185–203. [Google Scholar]
- 8. Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S.. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015;(9):CD002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Greenhalgh T, Wherton J, Shaw S, Morrison C.. Video consultations for covid-19. BMJ 2020;368:m998. [DOI] [PubMed] [Google Scholar]
- 10. Webster P. Virtual health care in the era of COVID-19. Lancet 2020;395:1180–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS Confederation. Health and Social Care Select Committee Inquiry – Delivering Core NHS and Care Services during the Pandemic and Beyond. London: NHS Confederation, 2020. https://www.nhsconfed.org/-/media/Confederation/Files/Public-Affairs/NHS-Confederation-submission-to-inquiry-on-Delivering-Core-NHS-and-Care-Services-during-the-Pandemic.pdf (1 June 2020, date last accessed).
- 12. Stevens S, Pritchard A. Second phase of NHS response to COVID19. London: NHS Confederation, 2020. https://www.england.nhs.uk/coronavirus/publication/second-phase-of-nhs-response-to-covid-19-letter-from-simon-stevens-and-amanda-pritchard/ (27 May 2020, date last accessed).
- 13. Carroll J, Edmondson AC.. Leading organisational learning in health care. BMJ Qual Saf 2002;11:51–6. [DOI] [PMC free article] [PubMed] [Google Scholar]