Abstract
Background
The fear of insecurity and uncertainty caused by the 2019 coronavirus disease (COVID-19), the separation and loss of certain important relationships, and great changes in lifestyle have awakened strong emotional responses, which may cause psychological problems in the general population. However, there is little research on how people who pay attention to anxiety and depression cope with the negative psychological impact during an epidemic or major disaster. This study aimed to identify what behaviors can effectively reduce negative emotions during an epidemic.
Methods
From 1 February to 8 March 2020, we conducted a web-based survey and collected information on general demographic data. Probable depression, anxiety symptoms, and coping behaviors were assessed with the Patient Health Questionnaire-9, Generalized Anxiety Disorder-7, and self-made coping behaviors questionnaires.
Result
Among 17 249 responders, 7923 and 9326 completed assessments of depression and anxiety respectively, and all responders completed the coping behaviors questionnaires. Our survey population showed a high prevalence rate of possible depression disorders (2746 of 7923, 34.66%) and anxiety disorders (5309 of 9326, 56.93%). Compared with other groups, the elderly, women, people of lower education, and people with lower income were more likely to suffer depression and/or anxiety. In terms of marital status, the cohabiting group showed the highest rate of depression and/or anxiety. Among the careers, students and housewives were high-risk groups suffering from depression and/or anxiety. After adjusting for social-demographic factors (e.g. age, sex), depression and anxiety were positively associated with self-injury, doing housework, and having sex or masturbating, and negatively associated with singing, drawing, or writing, dating friends online, singing, attending lectures, and doing yoga.
Conclusion
Our findings identified some spontaneous coping behaviors that can probably relieve the psychological impact of vulnerable groups during the COVID-19 epidemic.
Keywords: depression, anxiety, behavior, COVID-19
Introduction
The 2019 coronavirus disease (COVID-19) has spread globally, and the WHO defined COVID-19 as a pandemic on 30 January 2020.1 As of 9 April 2020, 1 431 254 cases of COVID-19 have been confirmed in over 110 countries and regions, with a total death toll of 85 089. Many countries (e.g. China, Italy, and Germany) have taken unprecedented measures in an attempt to prevent quick spread of the disease, specifically, lockdown, temporary closure of schools/factories, and restriction of residents' activities. These strategies have been shown to be effective at reducing the spread of infectious diseases. However, the rapid spread of the disease and unprecedented interventions have affected the lifestyle of the general population comprehensively and awakened strong negative emotional responses.
Like other physical health problems, infectious diseases (e.g. COVID-19, severe acute respiratory syndrome (SARS)) also lead to some psycho-social problems. During the SARS outbreak, higher stress levels, poor sleep, and depressed mood were found among confirmed cases.2 About 23.04% of medical staff have been reported to suffer anxiety during the COVID-19 outbreak.3 Besides the most involved people (e.g. frontline responders and confirmed cases), the general population are also suffering from psychological pressure, such as anxiety and depression.4 All round the world, many people are required to stay at home, socially isolated to protect themselves from being infected, resulting in distressed states.5 As more and more people work/study at home with restricted social activities, the negative emotions experienced by these individuals are being compounded.6 Previous studies found that elderly women with high levels of education were more likely to perceive the threat of SARS and suffer from anxiety.7 The ongoing COVID-19 epidemic is causing strong emotional reactions, thus identification of the general population who are at higher risk of mental health issues would be timely.8 Facing a sudden outbreak, individuals have had to change their way of life and adopt appropriate behaviors to cope with negative emotions (e.g. depression, anxiety). However, there is currently no research in this area. In the present study, our first aim was to identify characteristics of the population who are most susceptible to psychological problems. The second aim was to identify what behaviors could effectively reduce negative emotions among those susceptible to depression and/or anxiety during the epidemic.
Methods
Participants and procedures
Through use of online social media, WeChat, we recruited participants with the Haola applet. The research was approved by the Ethics Committee of Sichuan University. The targeted group was Chinese WeChat users aged ≥18 years, who represent about 76.9% of the Chinese population in this age group. Data were stored on the secure server of Sichuan University. We conducted this web-based survey from 1 February to 8 March 2020. We collected general demographic information, and assessed probable depression, anxiety symptoms and behaviors. Our survey was aimed at people who worried about their psychological state. Probable depression, anxiety symptoms, and coping behaviors were assessed with the Patient Health Questionnaire-9, Generalized Anxiety Disorder-7, and self-made coping behaviors questionnaires. Of the 17 249 responders, 7923 and 9326 completed the questionnaires on depression and anxiety, respectively, and all responders completed the coping behaviors questionnaire.
Measures
Patient Health Questionnaire-9
For depression assessment, we used Patient Health Questionnaire-9 (PHQ-9), which is a 9-item self-report depressive symptoms scale.9 A score ≥10 is an indication of a likely depression disorder.10,11 PHQ-9 has good reliability and validity among the Chinese population.12,13 The Cronbach's α value was 0.674 for PHQ-9.
Generalized Anxiety Disorder-7
We used the Generalized Anxiety Disorder-7 (GAD-7) scale, which is a 7-item anxiety tool to assess anxiety symptoms. A score ≥7 indicates a clinically significant anxiety disorder.11,14 GAD-7 is well-validated according to the DSM-IV diagnostic criteria and sensitive to general population.15–18 Studies have shown that GAD-7 has good reliability and validity in China.12,13 The Cronbach's α value is 0.713 for GAD-7.
Coping behaviors questionnaire
A self-constructed coping behaviors questionnaire was designed to assess behavior during the epidemic, including: Which of the following ways would you use to ease your depression/anxiety? (1) Singing; (2) Self-injury; (3) Drawing or writing; (4) Dating friends online; (5) Listening to music; (6) Watching TV or movie; (7) Writing diary; (8) Doing housework; (9) Meditating; (10) Attending online lectures or activities; (11) Online shopping; (12) Having sex or masturbating; (13) Doing yoga. All answers were coded as binary variables (0 = No; 1 = Yes).
Analysis
The analyses were done with R-software 3.6. ANOVA analysis was used for comparisons between two groups. Analyses were two-tailed with α = 0.05. Logistic regression analysis was conducted with depression/anxiety as the outcome. Model 1 was not adjusted; Model 2 was adjusted for sex, age, education, and income.
Results
Basic demographic characteristics
The prevalence rates of depression and anxiety were 34.66% (2746 of 7923) and 56.93% (5309 of 9326), respectively. Compared to other groups for each characteristic, the elderly, women, people of lower education, and those with lower income were more likely to suffer depression and/or anxiety. In terms of marital status, the cohabiting group showed the highest rate of depression and/or anxiety. Among the careers, students and housewives were high-risk groups suffering from depression and/or anxiety (Table 1).
Table 1.
Sample demographics by depression/anxiety status.
| Characteristics | Category | Depression (n = 7923) | P | Anxiety (n = 9326) | P | ||
|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | ||||
| Sex | Male | 1682 (72.2%) | 649 (27.8%) | 0.000 | 1748 (51.7%) | 1631 (69.3%) | 0.000 |
| Female | 3495 (62.5%) | 2097 (37.5%) | 2269 (38.2%) | 3678 (30.7%) | |||
| Age (year) | 18–24 | 1297 (73.9%) | 458 (26.1%) | 0.000 | 764 (34.1%%) | 1476 (65.9%) | 0.000 |
| 25–44 | 3130 (64.7%) | 1708 (35.3%) | 2199 (41.2%) | 3132 (58.8%) | |||
| 45–64 | 744 (56.6%) | 571 (43.4%) | 963 (59.2%) | 664 (40.8%) | |||
| 65+ | 6 (40.0%) | 9 (60.0%) | 91 (71.1%) | 37 (28.9%) | |||
| Education | Lower secondary school | 1949 (65.2%) | 1039 (34.8%) | 0.000 | 412 (39.1%) | 642 (60.9%) | 0.002 |
| Junior school | 998 (60.2%) | 659 (39.8%) | 545 (42.1%) | 751 (57.9%) | |||
| Bachelors | 1914 (67.9%) | 905 (32.1%) | 1661 (44.2%) | 2093 (55.8%) | |||
| Masters | 275 (67.2%) | 134 (32.8%) | 408 (47.5%) | 451 (52.5%) | |||
| Doctorate | 41 (82.0%) | 9 (18.0%) | 49 (51.0%) | 47 (49.0%) | |||
| Marital status | Single | 1551 (58.8%) | 1087 (41.2%) | 0.000 | 1244 (36.7%) | 2147 (63.3%) | 0.000 |
| Married | 3230 (70.9%) | 1327 (29.1%) | 2481 (47.8%) | 2704 (52.2%) | |||
| Cohabiting | 116 (52.3%) | 106 (47.7%) | 91 (31.2%) | 201 (68.8%) | |||
| Divorced | 252 (54.7%) | 209 (45.3%) | 170 (43.0%) | 225 (57.0%) | |||
| Widowed | 28 (62.2%) | 17 (37.8%) | 31 (49.2%) | 32 (50.8%) | |||
| Occupation | Medical staff | 896 (69.7%) | 394 (30.3%) | 0.000 | 673 (46.9%) | 763 (53.1%) | 0.000 |
| Teachers | 280 (61.5%) | 175 (38.5%) | 217 (39.9%) | 327 (60.1%) | |||
| Students | 451 (56.7%) | 344 (43.3%) | 367 (34.6%) | 695 (65.4%) | |||
| Information technology (IT) | 150 (58.6%) | 106 (41.4%) | 203 (38.3%) | 327 (61.7%) | |||
| Retail business | 622 (69.0%) | 279 (31.0%) | 574 (39.9%) | 864 (60.1%) | |||
| Housewife | 285 (56.9%) | 216 (43.1%) | 180 (35.3%) | 330 (64.7%) | |||
| Civil servant | 213 (63.6%) | 122 (36.4%) | 305 (45.4%) | 367 (54.6%) | |||
| Farmers and workers | 741 (73.7%) | 265 (26.3%) | 828 (52.7%) | 743 (47.3%) | |||
| Financial practitioner/media | 748 (65.2%) | 399 (34.8%) | 518 (43.0%) | 687 (57.0%) | |||
| Other | 791 (63.9%) | 446 (36.1%) | 152 (42.5%) | 206 (57.5%) | |||
| Income (yuan/yr) | 0–40,000 | 2027 (59.8%) | 1364 (40.2%) | 0.000 | 1288 (38.7%) | 2037 (61.3%) | 0.000 |
| 50,000–10,000 | 854 (68.9%) | 385 (31.1%) | 840 (46.3%) | 976 (53.7%) | |||
| 11,000–20,000 | 282 (75.6%) | 91 (24.4%) | 320 (51.9%) | 297 (48.1%) | |||
| 21,000–40,000 | 62 (74.7%) | 21 (25.3%) | 74 (53.6%) | 64 (46.4%) | |||
| 41,000–80,000 | 1915 (68.8%) | 867 (31.2%) | 1448 (43.5%) | 1884 (56.5%) | |||
| >80,000 | 37 (67.3%) | 18 (32.7%) | 47 (48.0%) | 51 (52.0%) | |||
Association between negative psychological state and behaviors
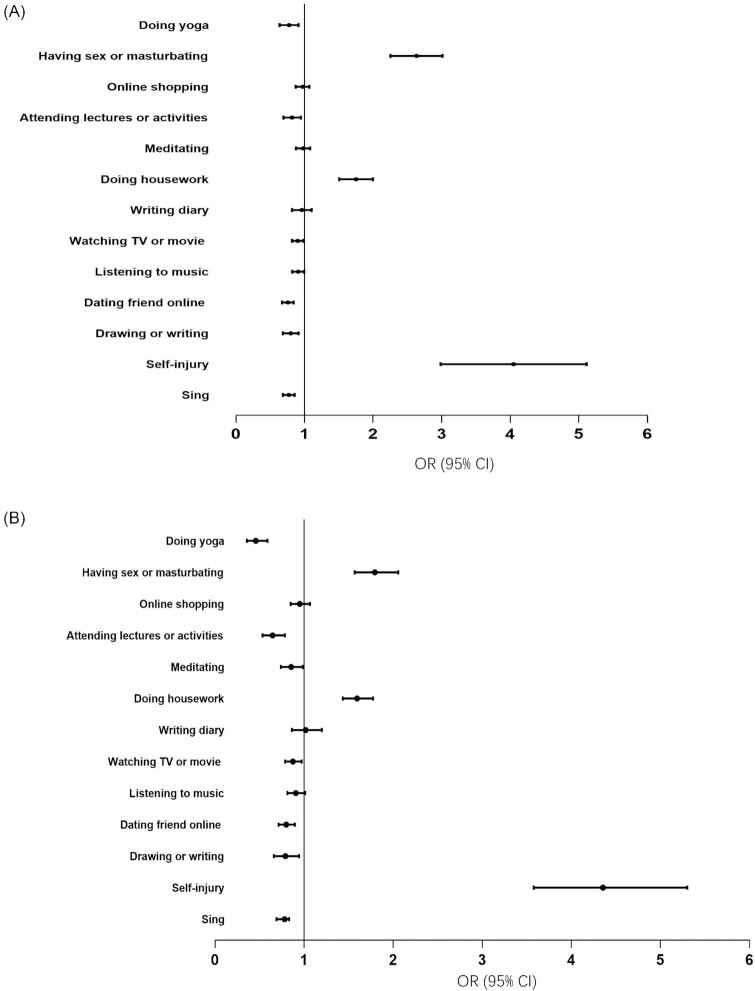
The associations between negative psychological state and behaviors are shown in Fig. 1. After adjusting for social-demographic factors (e.g. age, sex), depression was found to be positively associated with self-injury (OR = 4.356), doing housework (OR = 1.595), and having sex or masturbating (OR = 1.795). Depression was negatively associated with singing (OR = 0.781), drawing or writing (OR = 0.79), dating friends online (OR = 0.800), listening to music (OR = 0.907), watching TV or movie (0.875), meditating (OR = 0.855), attending lectures (OR = 0.646), and doing yoga (OR = 0.458). After adjusting for social-demographic factors (e.g. age, sex), anxiety was positively associated with self-injury (OR = 3.955), doing housework (OR = 1.74), and having sex or masturbating (OR = 2.614). Anxiety was negatively associated with singing (OR = 0.767), drawing or writing (OR = 0.793), dating friends online (OR = 0.754), listening to music (OR = 0.905), watching TV or movie (OR = 0.898), attending lectures or activities (OR = 0.813), and doing yoga (OR = 0.766). The detailed results of the unadjusted model and adjusted model are given in Supplementary Table 1.
Figure 1.
Association between negative psychological state and behaviors. (A) Anxiety and behaviors; (B) depression and behaviors.
Discussion
From our results, 34.66% of respondents reported moderate and above depressive symptoms and 56.93% of respondents reported mild and above anxiety symptoms. According to the China Mental Health Survey, in 2013, weighted 12-month prevalence of depressive disorders was 3.6% and weighted 12-month prevalence of anxiety disorders was 5.0%.19 This indicates that our report of depressive and anxiety symptoms is higher than might be expected. This could be explained by the following three reasons: first, most of the individuals who chose to answer the questionnaire were those who suspected that they had psychological problems or were troubled by psychological problems; second, we used self-assessment questionnaires rather than structured interviews; third, this could be an effect of the sudden outbreak of life-threatening COVID-19 and the unprecedented measures to combat the disease implemented by the government. We found that women, the elderly, the housewives, people who had lower levels of education or income, or people whose marital status was cohabiting, had a higher risk of suffering from depression and/or anxiety. It is hard for elderly women with lower levels of education to find jobs. A housewife usually relies on her husband's income. Such economic dependence and instability places these women at higher risk for depression and anxiety. Fewer extra-familial social contacts and certain reproductive-related hormonal changes could further increase the risk of depression and anxiety. It was also noted that students were a susceptible population for anxiety and depression during the pandemic. This could be because most cities in China shut down schools and chose to conduct online teaching. The sudden change in learning style and worries about academic progression could have an adverse influence on the psychological state of students.
Behaviors associated with lowered risk of depression and/or anxiety
In this research, we found that yoga, singing, meditation-based programs, chatting with friends online, and attending online psychological lectures was associated with a lower risk of depression and/or anxiety. Similar results were found in previous studies on depression20,21 and anxiety.22,23 However, we found that singing helped relieve symptoms of depression and anxiety, but listening to music did not. This phenomenon could be explained in that compared to listening to music, singing is an active expression of emotions rather than passive acceptance. Previous studies indicated that singing alleviates depression and anxiety, improves health-related life quality, and generates a feeling of social support and well-being.24–26 Singing not only makes individuals feel excited, but also activates the brain cortex, limbic system, endocrine system, and nervous system.27
Why could these factors help to ease depression and/or anxiety? What common and differential effects did they have on depression and/or anxiety? Yoga, singing, and meditation encourages the use of diaphragmatic breathing, which influences some important physiological functions including deep and slow breathing. Specifically, breathing control in yoga, singing, and meditation is thought to recalibrate the automatic nervous system through a shift towards an advantage of the parasympathetic nervous system via vagal stimulation.28 Yoga and meditation also affect the hypothalamic-pituitary-adrenal responsiveness and contribute to adaptions in endocrine secretion of substances including cortisol and adrenocorticotropic hormones.29 Singing and chatting with friends online contribute to gaining a sense of connectivity and belonging. Besides, singing and online chatting were also found to help develop resilience among individuals, building coping skills and confidence.30 Chatting with friends online and attending online psychological lectures may reduce the estrangement and loneliness caused by isolation. And experienced experts or friends can share valuable suggestions on how to cope with depression and anxiety. Besides, online chatting and online psychological lectures require a small repertoire of uncertainty reduction, little interpersonal sophistication, and few politeness strategies.
These alleviating behaviors also function by different mechanisms. Yoga contributes to reduce subjective stress perception among healthy adults and reduce levels of plasma cortisol among individuals with depression.31 Singing can lead to a sense of well-being as demonstrated by positive self-esteem, positive emotions, declined aggression, and development of a sense of mutuality.32,33Meditation training allows one to rapidly notice and break away from ruminative and pessimistic thoughts (e.g. thinking repeatedly about the pandemic), and recognize when the emotion is starting to change.34
Behaviors associated with increased risk of depression and/or anxiety
Self-injury was described as “the deliberate injuring of body tissue without conscious suicidal intent”.35 The sudden outbreak of the epidemic actually acts as a stress. When facing this stress, some may choose self-injury to release the negative emotion. In fact, self-injury cannot relieve negative emotion, rather, it exacerbates this trend. Previous study showed that self-injury can cause significant psychological and physical harm to people. On the one hand, it causes extra negative stress, for example, an immediate decrease in a desired internal state or an increase in an aversive state.35 On the other hand, there is a possibility for people to conduct self-injury repeatedly after the first try. Most importantly, it leads to direct physical harm, which may develop into suicide attempts.36
The current study found that doing housework is associated with increased risk of depression and anxiety. Compared to physical activities (e.g. yoga, running and walking), housework tasks concentrate on the physiological costs (e.g. energy expenditure) rather than musculoskeletal load or physical relaxation. These energy costs are relevant as they lead to fatigue and may amplify the influences of housework.37 Garabiles' study found that fatigue has the highest strength in the depression network structure, and this is common among Asian populations.38 However, the relationship between housework and depression/anxiety should be considered in deeper layers. Against the Chinese cultural background, women usually spend more time on household activities than men, which could explain why we found a higher risk of depression/anxiety in women in this study.
Mental health implication
Considering the unpredictable end of the COVID-19 pandemic, our results will provide some effective guidance for the general population who pay attention to psychological emotions or suffer from negative psychological emotions, and have some clinical and policy implications. Firstly, it is necessary for mental health authorities to identify high-risk groups based on basic characteristics. For example, this result corresponds to previous research that women were at higher risk of depression and/or anxiety.39 Secondly, we found that doing yoga and singing could help relieve depression and anxiety symptoms. Meditation could relieve depression symptoms but not anxiety symptoms. However, there is growing evidence to suggest that meditation has positive influences on anxiety symptoms.21,40,41 Our observations may be related to the short duration of the intervention with fewer opportunities for assessment of the effects of meditation. Thus, meditation may be effective given as online group meditation. Thirdly, self-injury and masturbation may be associated with increased risk of negative emotions. We can advise the general population how to deal with negative emotions correctly through a network-based mental health course. For example, by singing to release emotions. Yoga can be good physical exercise (e.g. improve cardiopulmonary function), and alleviate negative emotions at the same time. The results of this study played an important role in guiding online psychological intervention before and during the epidemic.42 We can identify high-risk groups through basic characteristics (e.g. gender, age, and education), and guide the general population for emotional self-management via behaviors to lower the depression/anxiety risks (e.g. do yoga, sing and meditation). In addition to self-management of disturbed emotions through positive coping behaviors, how to organize mental health care for those people who present psychiatric symptoms as a result of the COVID-19 pandemic is also very important. On the one hand, community-based and internet-based mental health services should be integrated into the national health system.42,43 On the other hand, mental health services should be provided post-COVID-19 to prevent possible psychiatric disorders.44
Limitations
This research has some limitations. Firstly, there was possible bias of the results caused by the sampling. The Snowball sampling strategy allowed for additional respondents, but it was likely that most of our respondents were individuals who paid attention to mental health and had negative emotions. Thus, the research was not entirely representative of the general population and possibly does not reflect the actual psychological state of the general population. Caution is warranted in generalizing the findings to the general population. In future, a random selection of the general population is needed. Secondly, different yoga forms (e.g. Hatha yoga, Yin yoga, Bikram yoga, Kundalini yoga) have different influences on physical and mental practices, but we did not distinguish between these in this study. Similar bias existed with meditation, where we only recorded whether the individuals meditated, not the details of the duration or frequency of meditation. Thirdly, Moccia's study found that depression and anxiety in the COVID-19 period may be mediated by temperamental and personality characteristics of the people. In other words, specific affective temperament (e.g. cyclothymic, depression, and anxious temperaments) and attachment features (e.g. need for approval) can predict the burden of mental health.45 But we did not collect information on temperamental and personality characteristics. Future studies should take temperament and personality characteristics into consideration.
Supplementary Material
ACKNOWLEDGEMENTS
This paper is supported by the 1·3·5 Project for Disciplines of Excellence—Clinical Research Incubation Project, West China Hospital, Sichuan University (Grant No. 2020HXFH041), and the Strategic Priority Research Program of the Chinese Academy of Sciences (Grant No. XDA23090502).
Contributor Information
Fenfen Ge, Mental Health Center of West China Hospital, Sichuan University, Chengdu 610041, China.
Mengtong Wan, Wuyuzhang Honors College, Sichuan University, Chengdu 610041, China.
Anni Zheng, National Laboratory of Pattern Recognition, Institute of Automation, Chinese Academy of Sciences, Beijing 100190, China.
Jun Zhang, Mental Health Center of West China Hospital and Disaster Medicine Center, Sichuan University, Chengdu 610041, China.
Author contributions
Jun Zhang conceived and designed the study. Fenfen Ge, Mengtong Wan, and Anni Zheng participated in the study design, data analysis, interpretation of findings, literature search, drafting, implementation, and approval of the final manuscript.
Conflict of interest statement
None declared.
Reference
- 1. Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi:10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- 2. Lee DT, Wing YK, Leung HCet al. Factors associated with psychosis among patients with severe acute respiratory syndrome: a case-control study. Clin Infect Dis. 2004;39:1247–49.. doi:10.1086/424016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Huang JZ, Han MF, Luo TD, et al. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:E001. [DOI] [PubMed] [Google Scholar]
- 4. Qiu J, Shen B, Zhao Met al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry. 2020;33:e100213. doi:10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Horton R. Offline: 2019-nCoV–“A desperate plea”. Lancet North Am Ed. 2020;395:400. doi:10.1016/S0140-6736(20)30299-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Van Bortel T, Basnayake A, Wurie F, et al. Psychosocial effects of an Ebola outbreak at individual, community and international levels. Bull World Health Organ. 2016;94:210–14.. doi:10.2471/BLT.15.158543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leung GM, Lam TH, Ho LMet al. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health. 2003;57:857–63.. doi:10.1136/jech.57.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–9.. doi:10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 - Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.. doi:10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fine TH, Contractor AA, Tamburrino M, et al. Validation of the telephone-administered PHQ-9 against the in-person administered SCID-I major depression module. J Affect Disord. 2013;150:1001–7.. doi:10.1016/j.jad.2013.05.029. [DOI] [PubMed] [Google Scholar]
- 11. Blenkiron P, Goldsmith L. Patient-reported outcome measures in community mental health teams: pragmatic evaluation of PHQ-9, GAD-7 and SWEMWBS. BJPsych Bull. 2019;43:221–7.. doi:10.1192/bjb.2019.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zeng Q-Z, He Y-L, Liu H, et al. Reliability and validity of Chinese version of the Generalized Anxiety Disorder 7-item (GAD-7) scale in screening anxiety disorders in outpatients from traditional Chinese internal department. Chinese Mental Health J. 2013;27:163–8. [Google Scholar]
- 13. Wang W, Bian Q, Zhao Yet al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36:539–44.. doi:10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 14. Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder - The GAD-7. Arch Intern Med. 2006;166:1092–7.. doi:10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 15. Kroenke K, Spitzer RL, Williams JBW, et al. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–25.. doi:10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 16. Horton M, Perry AE. Screening for depression in primary care: a Rasch analysis of the PHQ-9. BJPsych Bull. 2016;40:237–43.. doi:10.1192/pb.bp.114.050294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Andreas JB, Brunborg GS. Depressive symptomatology among norwegian adolescent boys and girls: The Patient Health Questionnaire-9 (PHQ-9) psychometric properties and correlates. Front Psychol. 2017;8:887. doi:10.3389/fpsyg.2017.00887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tiirikainen K, Haravuori H, Ranta K, et al. Psychometric properties of the 7-item Generalized Anxiety Disorder Scale (GAD-7) in a large representative sample of Finnish adolescents. Psychiatry Res. 2019;272:30–5.. doi:10.1016/j.psychres.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 19. Huang Y, Wang Y, Wang Het al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6:211–24.. doi:10.1016/S2215-0366(18)30511-X. [DOI] [PubMed] [Google Scholar]
- 20. Cramer H, Lauche R, Langhorst J, et al. Yoga for depression: a systematic review and meta-analysis. Depress Anxiety. 2013;30:1068–83. [DOI] [PubMed] [Google Scholar]
- 21. Carpena MX, Tavares PS, Menezes CB. The effect of a six-week focused meditation training on depression and anxiety symptoms in Brazilian university students with 6 and 12 months of follow-up. J Affect Disord. 2019;246:401–7.. doi:10.1016/j.jad.2018.12.126. [DOI] [PubMed] [Google Scholar]
- 22. Kang S. Disembodiment in online social interaction: impact of online chat on social support and psychosocial well-being. Cyberpsychol Behav. 2007;10:475–7.. doi:10.1089/cpb.2006.9929. [DOI] [PubMed] [Google Scholar]
- 23. Li AW, Goldsmith CA. The effects of yoga on anxiety and stress. Altern Med Rev. 2012;17:21–35. [PubMed] [Google Scholar]
- 24. Lord VM, Cave P, Hume VJ, et al. Singing teaching as a therapy for chronic respiratory disease–a randomised controlled trial and qualitative evaluation. BMC Pulm Med. 2010;10:41. doi:10.1186/1471-2466-10-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lord VM, Hume VJ, Kelly JLet al. Singing classes for chronic obstructive pulmonary disease: a randomized controlled trial. BMC Pulm Med. 2012;12:69. doi:10.1186/1471-2466-12-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liu H, Song M, Zhai ZHet al. Group singing improves depression and life quality in patients with stable COPD: a randomized community-based trial in China. Qual Life Res. 2019;28:725–35.. doi: 10.1007/s11136-018-2063-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kang J, Scholp A, Jiang JJ. A review of the physiological effects and mechanisms of singing. J Voice. 2018;32:390–5.. doi: 10.1016/j.jvoice.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 28. Brown RP, Gerbarg PL. Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression. Part II–clinical applications and guidelines. J Altern Complement Med. 2005;11:711–7.. doi:10.1089/acm.2005.11.711. [DOI] [PubMed] [Google Scholar]
- 29. Anderson E, Shivakumar G. Effects of exercise and physical activity on anxiety. Front Psychiatry. 2013;4:27. doi:10.3389/fpsyt.2013.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fancourt D, Warran K, Finn Set al. Psychosocial singing interventions for the mental health and well-being of family carers of patients with cancer: results from a longitudinal controlled study. BMJ Open. 2019;9:e026995. doi:10.1136/bmjopen-2018-026995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wang F, Szabo A. Effects of yoga on stress among healthy adults: A systematic review. Altern Ther Health Med. 2020. [PubMed] [Google Scholar]
- 32. Götell E, Brown S, Ekman SL. The influence of caregiver singing and background music on vocally expressed emotions and moods in dementia care: a qualitative analysis. Int J Nurs Stud. 2009;46:422–30.. doi:10.1016/j.ijnurstu.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 33. Dassa A, Amir D. The role of singing familiar songs in encouraging conversation among people with middle to late stage Alzheimer's disease. J Music Ther. 2014;51:131–53.. doi:10.1093/jmt/thu007. [DOI] [PubMed] [Google Scholar]
- 34. Hilt LM, Pollak SD. Getting out of rumination: Comparison of three brief interventions in a sample of youth. J Abnorm Child Psychol. 2012;40:1157–65.. doi:10.1007/s10802-012-9638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nock MK, Prinstein MJ, Sterba SK. Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. J Abnorm Psychol. 2009;118:816–27.. doi:10.1037/a0016948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Muehlenkamp JJ, Gutierrez PM. Risk for suicide attempts among adolescents who engage in non-suicidal self-injury. Arch Suicide Res. 2007;11:69–82.. doi: 10.1080/13811110600992902. [DOI] [PubMed] [Google Scholar]
- 37. Habib RR, Fathallah FA, Messing K. Full-time homemakers: workers who cannot “go home and relax”. Int J Occup Saf Ergon. 2010;16:113–28.. doi:10.1080/10803548.2010.11076833. [DOI] [PubMed] [Google Scholar]
- 38. Garabiles MR, Lao CK, Xiong Yet al. Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: A network approach. J Affect Disord. 2019;250:85–93.. doi:10.1016/j.jad.2019.02.062. [DOI] [PubMed] [Google Scholar]
- 39. Lim GY, Tam WW, Lu Yet al. Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci Rep. 2018;8:2861. doi:10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Saeed SA, Antonacci DJ, Bloch RM. Exercise, yoga, and meditation for depressive and anxiety disorders. Am Fam Physician. 2010;81:981–6. [PubMed] [Google Scholar]
- 41. Saeed SA, Cunningham K, Bloch RM. Depression and anxiety disorders: Benefits of exercise, yoga, and meditation. Am Fam Physician. 2019;99:620–7. [PubMed] [Google Scholar]
- 42. Zhang J, Wu W, Zhao Xet al. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precis Clin Med. 2020;3:3–8.. doi:10.1093/pcmedi/pbaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sani G, Janiri D, Di Nicola Met al. Mental health during and after the COVID-19 emergency in Italy. Psychiatry Clin Neurosci. 2020;74:372. doi:10.1111/pcn.13004. [DOI] [PubMed] [Google Scholar]
- 44. Landi F, Gremese E, Bernabei R, et al. Post-COVID-19 global health strategies: the need for an interdisciplinary approach. Aging Clin Exp Res. 2020. doi:10.1007/s40520-020-01616-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Moccia L, Janiri D, Pepe Met al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun. 2020. doi:10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.