Abstract
Aims
An increase in out-of-hospital cardiac arrest (OHCA) incidence has been reported in the very early phase of the COVID-19 epidemic, but a clear demonstration of a correlation between the increased incidence of OHCA and COVID-19 is missing so far. We aimed to verify whether there is an association between the OHCA difference compared with 2019 and the COVID-19 epidemic curve.
Methods and results
We included all the consecutive OHCAs which occurred in the Provinces of Lodi, Cremona, Pavia, and Mantova in the 2 months following the first documented case of COVID-19 in the Lombardia Region and compared them with those which occurred in the same time frame in 2019. The cumulative incidence of COVID-19 from 21 February to 20 April 2020 in the study territory was 956 COVID-19/100 000 inhabitants and the cumulative incidence of OHCA was 21 cases/100 000 inhabitants, with a 52% increase as compared with 2019 (490 OHCAs in 2020 vs. 321 in 2019). A strong and statistically significant correlation was found between the difference in cumulative incidence of OHCA between 2020 and 2019 per 100 000 inhabitants and the COVID-19 cumulative incidence per 100 000 inhabitants both for the overall territory (ρ 0.87, P < 0.001) and for each province separately (Lodi: ρ 0.98, P < 0.001; Cremona: ρ 0.98, P < 0.001; Pavia: ρ 0.87, P < 0.001; Mantova: ρ 0.81, P < 0.001).
Conclusion
The increase in OHCAs in 2020 is significantly correlated to the COVID-19 pandemic and is coupled with a reduction in short-term outcome. Government and local health authorities should seriously consider our results when planning healthcare strategies to face the epidemic, especially considering the expected recurrent outbreaks.
Keywords: Out-of-hospital cardiac arrest, COVID-19, SARS-CoV-2, Italy
Graphical Abstract
Graphical Abstract.
Introduction
A novel coronavirus, capable of human to-human transmission, emerged in China at the end of 20191 and was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).2 The resulting infection, called ‘Coronavirus disease 2019’ (COVID-19), has a wide spectrum of severity, from asymptomatic or pauci-symptomatic patients to patients with severe pneumonia and acute respiratory distress syndrome (ARDS) requiring mechanical ventilation.3 Northern Italy was one of the first regions outside China to be significantly affected by COVID-19.4 The first case of severe pneumonia due to SARS-CoV-2 without history of possible exposure abroad was diagnosed in Codogno, Province of Lodi, Lombardy Region on 20 February 2020. Since then, the number of infections has been rapidly increasing, with a mortality rate higher than that of China,5 and an increase in incidence of out-of-hospital cardiac arrest (OHCA) in the very early phase of the epidemic also being reported.6 However, the correlation between the increase in OHCAs observed in 2020 and the COVID-19 epidemic curve still remain unproved. Our aim was to assess whether the difference in the number of OHCAs between 2020 and 2019 was statistically correlated with the COVID-19 epidemic trend and to look for clinical pre-hospital elements supporting this evidence.
Methods
Study population
The Lombardia Cardiac Arrest Registry (Lombardia CARe: NCT03197142) is a multicentre longitudinal prospective registry that has been registering all the OHCAs from the Province of Pavia since January 2015 and additionally from the Provinces of Lodi, Cremona, and Mantua Pavia since January 2019. All the data are collected following Utstein 2014 recommendations.7 It was approved by the Ethical Committee of the Fondazione IRCSS Policlinico San Matteo (proc. 20140028219) and by all the others involved in the territory.
We considered all the OHCAs that occurred in these four provinces in the southern part of the Lombardy Region, in northern Italy, in the 2 months following the first documented case in the Lombardy Region (21 February 2020 to 20 April 2020) and those of the same time frame in 2019 (21 February 2019 to 21 April 2019, to account for the leap year). For the Province of Pavia, the mean value of OHCAs that occurred in the same time frame from 2015 to 2019 was also provided as historical reference. The daily new cases and the cumulative incidence of COVID-19, based on the confirmed cases announced by the National Department of Civil Defence/Protezione Civile Nazionale,8 were also computed.
All the Emergency Medical System (EMS) electronic records have been reanalysed and the number of patients with suspected COVID-19 (fever for at least 3 days before OHCA associated with cough and/or dyspnoea) or with a diagnostic pharyngeal swab (performed before OHCA or after death) have been computed. Moreover, among the patients with suspected or diagnosed COVID-19, eventual gastrointestinal symptoms (vomiting or diarrhoea for at least 3 days) were assessed.
All the ECGs acquired in the field after the return of spontaneous circulation (ROSC) were evaluated for OHCA patients in 2020, and the QTc value was calculated with Bazett’s formula. QTc was defined as prolonged if longer than 440 ms in males and 460 ms in females.9
We also counted the number of emergency calls received by the EMS dispatch centre and the resulting number of callouts for any pathology for both the 2020 and 2019 study periods. Among those, we counted, and compared with the previous year, those leading to a pre-hospital diagnosis of ST-segment elevation myocardial infarction (STEMI) according to the criteria recommended by the 2017 guidelines of the European Society of Cardiology.10
Data management
The data of the study are collected and managed using REDCap electronic data capture tools hosted at Fondazione IRCCS Policlinico San Matteo.11,12 REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies, providing (i) an intuitive interface for validated data capture; (ii) audit trails for tracking data manipulation and export procedures; (iii) automated export procedures for seamless data downloads to common statistical packages; and (iv) procedures for data integration and interoperability with external sources.
Statistical analysis
We present categorical variables as counts and percentage; we computed the difference in percentage between 2020 and 2019 together with its 95% confidence interval (CI) using a binomial regression model with identity link. We present continuous variables using the median and 25th–75th percentiles; we computed the difference in medians and 95% CI using quantile regression. We computed the Spearman R and its 95% CI to measure the strength of the correlation of difference in cumulative incidence in OHCAs between 2020 and 2019 per 100 000 inhabitants and COVID-19 cumulative incidence per 100 000 inhabitants for the entire series and for each province. To assess whether the 2020–2019 difference in incidence over time of OHCA paralleled that of COVID-19 in 2020, we used fractional polynomials within a generalized regression linear model to model the relationship of these two variables, and plotted the fitted and observed values. We assessed the interaction of the cumulative incidence of COVID-19 and OHCA difference and fitted the same models separately for each province. Given the risk of overfitting, these models are to be considered exploratory. Statistical analyses were performed with the MedCalc version 19.2 (MedCalc Software Ltd) and the Stata software (version 16, StataCorp, College Station, TX, USA). All tests were two-sided, and a P-value <0.05 was considered statistically significant.
EMS adaptation to the COVID-19 outbreak
During the COVID-19 outbreak, the number of BLS-D- and ALS-trained staffed vehicles increased by 40% (from 45 to 63) and by 29% (from 21 to 27), respectively. The EMS dispatchers and personnel were instructed to investigate for any possible symptoms related to COVID-19, both during the emergency call and at the patient’s side from the caller, the relatives, and the eventual bystanders. Moreover, EMS personnel had been instructed to wear personal protective equipment (PPE; face shield, N95 face mask, and isolation gown) before starting resuscitation in case of doubt or if diagnosed for COVID-19. No specific changes in BLS or ALS protocols were adopted during the COVID-19 epidemic. See the Supplementary material online for details of the EMS description.
Results
The cumulative incidence of COVID-19 from 21 February to 20 April 2020 in the territory of the study was 956 COVID-19/100 000 inhabitants (Lodi 1190; Cremona 1529; Pavia 667; Mantua 706) and the cumulative incidence of OHCA was 31.7 cases/100 000 inhabitants, with a 52% increase compared with 2019 (490 OHCA in 2020 vs. 321 in 2019).
The increase in OHCA cases per 100 000 inhabitants was confirmed in each province, even if with different magnitude, according to the start of the epidemic (Lodi: +169%; Cremona: +106%; Pavia: +31%; Mantua: +12%) (Table 1). Notably, when considering the Province of Pavia as the historical reference, the mean incidence of OHCAs per 100 000 in the study period from 2015 to 2019 was 21.5 cases (95% CI 18.2–24.7).
Table 1.
Relationship of COVID-19 per 100 000 inhabitants and OHCA difference between 2020 and 2019 cumulative incidences per 100 000 from days 1 to 60
| Description |
Model with fractional polynomials |
||||||
|---|---|---|---|---|---|---|---|
| Province | Cumulative incidence per 100 000 |
% increase | Cumulative incidence per 100 000 | Spearman’s ρ | 95% CI | P-value | |
| 2020 OHCA | 2019 OHCA | COVID-19 | |||||
| All* | 31.7 | 20.8 | +52% | 956 | 0.87 | 0.84–0.9 | <0.001 |
| Lodi | 38.7 | 14.4 | +169% | 1,190 | 0.98 | 0.97–0.99 | <0.001 |
| Cremona | 31.5 | 15.3 | +106% | 1,529 | 0.98 | 0.97–0.99 | <0.001 |
| Pavia | 34.1 | 26 | +31% | 667 | 0.88 | 0.8–0.92 | <0.001 |
| Mantova | 24.7 | 22.1 | +12% | 706 | 0.81 | 0.7–0.88 | <0.001 |
P for interaction with province <0.001.
Correlation between OHCA excess in 2020 and COVID-19
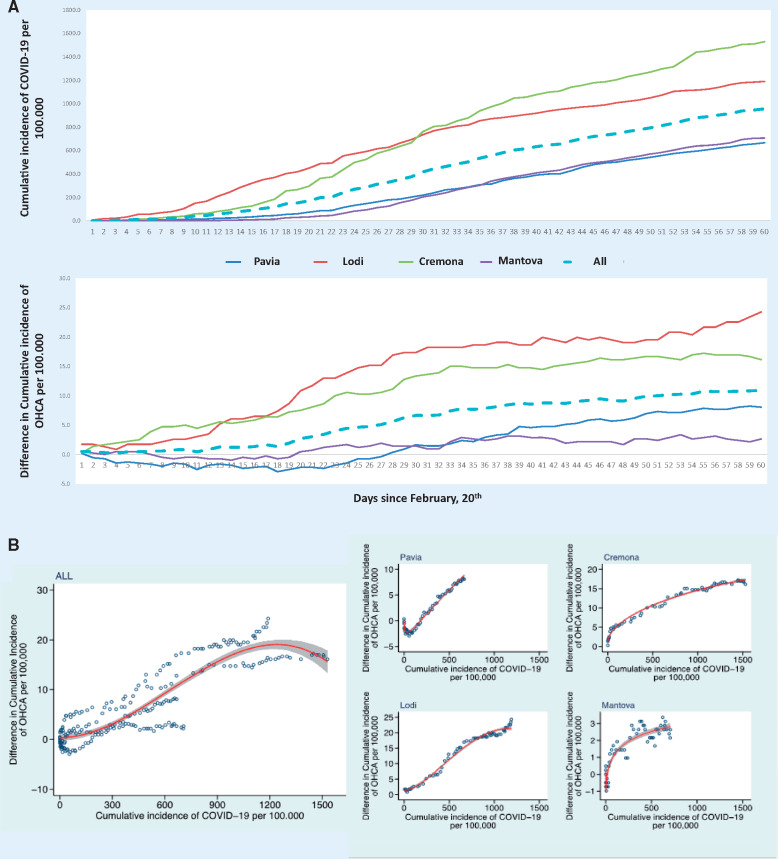
Statistical correlation
A strong and statistically significant correlation was found between the difference in cases of OHCA between 2020 and 2019 per 100 000 inhabitants and the trend of COVID-19 cumulative incidence per 100 000 inhabitants, both for the overall territory. In all cases, the association was strong, with a Spearman ρ >0.80 both for the entire case series and for each province (Table 1). Graphically, the overall association was best described by a polynomial including a square root followed by cubic transformation of the original variable. As a strong modifying effect by province of the relationship of the OHCA difference and COVID-19 cumulative incidence was present (P for interaction <0.001), we described each province separately; each had a different shape and slope of the corresponding curve (Figure 1).
Take home figure.
(A) Over a period of 60 days from 20 February, the cumulative incidence of COVID-19 per 100 000 inhabitants in the four provinces and in the overall territory (dotted line) (upper part), and the trend of the difference of OHCA between 2020 and 2019 per 100 000 inhabitants in the four provinces and in the overall territory (dotted line) (bottom part). (B) The cumulative incidence of the difference in OHCA between 2020 and 2019 per 100 000 inhabitants as a function of the cumulative incidence of COVID-19 per 100 000 inhabitants, since 20 February 2020. Dots are the observed values. The red line is the function fitted using fractional polynomials. The shaded area is the 95% CI for the estimates.
Clinical findings
The comparison of the patient and OHCA characteristics between the two years is presented in Table 2. Of note, medical aetiology (94.9% vs. 89.4%; P = 0.006), home location (90.2% vs. 83.2%; P = 0.005), and unwitnessed OHCAs (53.5% vs. 45.8%; P = 0.037) were more frequent in 2020 compared with 2019; EMS arrival time was longer (15 min vs. 12 min; P < 0.001) and the outcome of patients with resuscitation attempted by EMS was worse in 2020 (pre-hospital ROSC 8.6% vs. 19.8%; P < 0.001 and survival at hospital discharge 5.1% vs. 9.5%; P = 0.06).
Table 2.
Comparison between patients’ and OHCAs’ characteristics in 2020 and 2019 period
| Variable | 2020 (n = 490) | 2019 (n = 321) | Difference (95% CI)* | P-value |
|---|---|---|---|---|
| Males, (%) | 321 (65.5) | 188 (58.6) | 6.9 (0.1–13.8) | 0.047 |
| Age, years (IQR) | 78 (67–84) | 79 (67–86) | –1 (–3.2 to 1.2) | 0.366 |
| EMS arrival time, min (IQR) | 15 (11–20) | 12 (9–15) | 3 (1.9–4.1) | <0.001 |
| Aetiology of arrest, n (%) | ||||
| Medical | 465 (94.9) | 287 (89.4) | 5.5 (95%CI, 1.6 to 9.4) | 0.006 |
| Trauma | 13 (2.6) | 28 (8.7) | –6.1 (–9.5 to –2.7) | <0.001 |
| Drowning | 0 (0) | 0 (0) | – | |
| Overdose | 1 (0.2) | 1 (0.3) | –0.1 (–0.8 to 0.6) | 0.77 |
| Electrocution | 0 (0) | 0 (0) | – | |
| Asphyxia (external causes) | 11 (2.3) | 5 (1.6) | 0.7 (–1.2 to 2.6) | 0.47 |
| OHCA location, n (%) | ||||
| Home | 442 (90.2) | 267 (83.2) | 7 (2.2–11.9) | 0.005 |
| Nursing residence | 21 (4.3) | 23 (7.2) | –2.9 (–6.2 to 0.5) | 0.09 |
| Workplace | 2 (0.4) | 0 (0) | –0.4 (–1 to 0.2) | 0.16 |
| Street | 17 (3.5) | 23 (7.2) | –3.7 (–6.9 to –0.4) | 0.026 |
| Public building | 3 (0.6) | 5 (1.5) | –0.9 (–2.5 to 0.6) | 0.22 |
| Sport | 0 (0) | 1 (0.3) | – | |
| Other | 5 (1) | 2 (0.6) | 0.4 (–0.8 to 1.6) | 0.5 |
| Witnessed status, n (%) | ||||
| Unwitnessed | 261 (53.3) | 147 (45.8) | 7.5 (0.5–14.5) | 0.037 |
| Bystander witnessed | 171 (34.9) | 143 (44.5) | –9.6 (–16.5 to –2.8) | 0.006 |
| Witnessed by EMS | 58 (11.8) | 31 (9.7) | 2.1 (–2.1 to 6.5) | 0.32 |
| Resuscitation attempted by EMS, n (%) | ||||
| Yes | 314 (64.1) | 222 (69.2) | –5.1 (–11.7 to 1.5) | 0.13 |
| No, dead on arrival | 148 (30.2) | 73 (22.7) | 7.5 (1.3–13.6) | 0.017 |
| No, considered futile | 28 (5.7) | 26 (8.1) | –2.4 (–6 to 1.2) | 0.2 |
| Bystander CPR, n (%)† | 89 (34.6) | 87 (45.3) | –10.7 (–19.8 to –1.5) | 0.02 |
| Presenting rhythm, n (%)‡ | ||||
| Shockable | 36 (11.5) | 37 (16.7) | –5.2 (–11.2 to 0.8) | 0.09 |
| Not shockable | 278 (88.5) | 185 (83.3) | 5.2 (–0.8 to 11.2) | 0.09 |
| ACLS initiated, n (%)‡ | 138 (43.9) | 138 (62.2) | –18.3 (–26.6 to –9.8) | <0.001 |
| Amiodarone administered, n (%)§ | 17 (12.3) | 16 (11.6) | 0.7 (–6.9 to 8.4) | 0.85 |
| Adrenaline administered, n (%)§ | 120 (89.5) | 119 (86.9) | 2.6 (–0.5 to 10.4) | 0.49 |
| Mechanical CPR, n (%)§ | 9 (6.5) | 23 (16.7) | –10.2 (–17.6 to –2.7) | 0.008 |
| Outcome, n (%)‡ | ||||
| Death in the field | 253 (80.6) | 156 (70.3) | 10.3 (2.9–17.7) | 0.007 |
| Transported with ongoing CPR | 34 (10.8) | 22 (9.9) | 0.9 (–4.3 to 6.1) | 0.73 |
| Transported with ROSC | 27 (8.6) | 44 (19.8) | –11.2 (–17.3 to –5.1) | <0.001 |
| Survived at hospital discharge, n (%)‡ | 16 (5.1) | 21 (9.5) | –4.4 (–8.9 to 0.2) | 0.06 |
EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; CPR, cardio-pulmonary resuscitation; ACLS, advanced cardiac life support (i.e. endotracheal intubation, administration of drugs, mechanical CPR); ROSC, return of spontaneous circulation.
Differences are expressed as rate difference or mean difference and 95% confidence intervals.
Among those in whom resuscitation was attempted by the EMS and excluding those witnessed by the EMS.
Among those in whom resuscitation was attempted by the EMS.
Among those in whom ACLS was initiated.
Among the 490 OHCA patients in 2020, 19 had a defined diagnosis of COVID-19 and 106 presented only suspected COVID-19 symptoms (fever for at least 3 days before OHCA associated with cough and/or dyspnoea). These 125 patients (25.5% of all OHCAs in 2020) represent 74% of the increase in OHCA in 2020, equally distributed in the four provinces (30 in Lodi, 32 in Cremona, 42 in Pavia, and 21 in Mantua). Moreover, among these 125 patients, gastrointestinal symptoms (vomiting or diarrhoea for at least 3 days) were also present in 9 (7.2%). The characteristics of these patients, as well as their comparison with unsuspected/undiagnosed patients, are presented in Table 3.
Table 3.
Characteristics of patients with OHCA suspected or diagnosed for COVID-19
| Variable | COVID-19 suspected or diagnosed (n = 125) | COVID-19 not suspected or diagnosed (n = 365) | Difference (95% CI)* | P-value |
|---|---|---|---|---|
| Symptoms suspected (fever associated with cough and/or dyspnoea) | 125 (100) | |||
| Defined diagnosis of COVID-19 | 19 (15.2) | |||
| Gastrointestinal symptoms | 9 (7.2) | |||
| Males, n (%) | 83 (66.4) | 238 (65.2) | 1.2 (–8.4 to 10.8) | 0.81 |
| Age, years (IQR) | 77 (70.2–83.7) | 78 (67–84) | –1 (–4 to 2) | 0.52 |
| EMS arrival time, min (IQR) | 16 (12–22.2) | 14 (11–19) | 2 (0.5–3.4) | 0.007 |
| Aetiology of arrest, n (%) | ||||
| Medical | 125 (100) | 340 (93.1) | – | |
| Trauma | 0 (0) | 13 (3.6) | – | |
| Drowning | 0 (0) | 0 (0) | – | |
| Overdose | 0 (0) | 1 (0.3) | – | |
| Electrocution | 0 (0) | 0 (0) | – | |
| Asphyxia (external causes) | 0 (0) | 11 (3) | – | |
| OHCA location, n (%) | ||||
| Home | 119 (95.2) | 323 (88.5) | 6.7 (1.7–11.7) | 0.008 |
| Nursing residence | 5 (4) | 16 (4.4) | –0.4 (–4.4 to 3.6) | 0.85 |
| Workplace | 0 (0) | 2 (0.5) | – | |
| Street | 1 (0.8) | 16 (4.4) | –3.6 (–6.2 to –1) | 0.007 |
| Public building | 0 (0) | 3 (0.8) | – | |
| Sport | 0 (0) | 0 (0) | – | |
| Other | 0 (0) | 5 (1.4) | – | |
| Witnessed status, n (%) | ||||
| Unwitnessed | 61 (48.8) | 200 (54.8) | –6 (–16.1 to 4.1) | 0.25 |
| Bystander witnessed | 39 (31.2) | 132 (36.2) | –5 (–14.5 to 4.5) | 0.31 |
| Witnessed by EMS | 25 (20) | 33 (9) | 11 (3.4–18.6) | 0.005 |
| Resuscitation attempted by EMS, n (%) | ||||
| Yes | 88 (70.4) | 226 (61.9) | 8.5 (–1 to 17.9) | 0.078 |
| No, dead on arrival | 27 (21.6) | 121 (33.1) | –11.5 (–20.2 to –2.9) | 0.009 |
| No, considered futile | 10 (8) | 18 (4.9) | 3.1 (–2.2 to 8.3) | 0.25 |
| Bystander CPR, n (%)† | 13 (20.6) | 76 (39.2) | –18.6 (–30.7 to –6.4) | 0.003 |
| Presenting rhythm, n (%)† | ||||
| Shockable | 8 (9.1) | 28 (12.4) | –3.3 (–10.7 to 4.1) | 0.38 |
| Not shockable | 80 (90.9) | 198 (87.6) | 3.3 (–4.1 to 10.7) | 0.38 |
| ACLS initiated, n (%)‡ | 32 (36.4) | 106 (46.9) | –10.5 (–22.5 to 1.4) | 0.08 |
| Amiodarone administered, n (%)§ | 3 (9.4) | 14 (13.2) | –3.8 (–15.8 to 8.1) | 0.53 |
| Adrenaline administered, n (%)§ | 28 (87.5) | 92 (90.2) | –2.7 (–15.5 to 10.1) | 0.68 |
| Mechanical CPR, n (%)§ | 2 (6.2) | 7 (6.6) | –0.4 (–10 to 9.3) | 0.94 |
| Outcome, n (%)‡ | ||||
| Death in the field | 70 (79.5) | 183 (81) | –1.5 (–11.3 to 8.4) | 0.77 |
| Transported with ongoing CPR | 11 (12.5) | 23 (10.2) | 2.3 (–5.6 to 10.3) | 0.57 |
| Transported with ROSC | 7 (8) | 20 (8.8) | –0.8 (–7.7 to 5.9) | 0.79 |
| Survived at hospital discharge, n (%)§ | 2 (2.3) | 14 (6.2) | –3.9 (–8.3 to 0.5) | 0.08 |
EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; CPR, cardio-pulmonary resuscitation; ACLS, advanced cardiac life support (i.e. endotracheal intubation, administration of drugs, mechanical CPR); ROSC, return of spontaneous circulation.
Differences are expressed as rate difference or mean difference and 95% confidence intervals.
Among those in whom resuscitation was attempted by the EMS and excluding those witnessed by the EMS.
Among those in whom resuscitation was attempted by the EMS.
Among those in whom ACLS was initiated.
Out of the 27 patients transported with ROSC in 2020, a post-ROSC ECG was available and could be evaluated in 18 (67%), 6 of them with suspected or diagnosed COVID-19, with a median QTc value of 464 ms [interquartile range (IQR) 420–486]. Notably the QTc values was prolonged in 12 patients (4 of them with suspected or diagnosed COVID-19).
Finally, the number of emergency calls to the EMS dispatch centre and the resulting callouts increased by 94.1% (55 903 in 2020 and 28 794 in 2019) and by 20.3% (26 729 in 2020 and 22 212 in 2019) in 2020 compared with the same period in 2019. Among the overall emergency calls, those with a resulting diagnosis of STEMI were 43 in 2020 and 72 in 2019, with a reduction of 40.2%.
Discussion
Our study provides important insights into the impact of COVID-19 on OHCAs during the first 2 months of the epidemic from one of the first and most burdened areas worldwide. The main finding of our study is the strong and statistically significant correlation of the difference between the 2020 and 2019 OHCAs and the COVID-19 epidemic. Of note, the correlation was maintained even in the presence of a different phase of the epidemic, characterized by a more rapid rise at the beginning, towards a plateau in the latter part.
This aspect becomes even more evident when considering the different provinces separately, where specific shapes of the relationship were also shown when modelling using fractional polynomials. Interestingly, despite different shapes of the epidemic curve, the excess of OHCAs strictly followed the COVID-19 epidemic in all the phases of the epidemic in each province.
From our perspective, this latter finding, together with the high percentage of OHCA patients with suspected or diagnosed COVID-19, strongly supports the presence of a link between the infection and such a dramatic condition as that of cardiac arrest. Furthermore, considering only the Province of Pavia, from where we have collected OHCA data since January 2015, the number of OHCAs was quite stable in the same 2-month period from 2015 to 2019, so an impressive increase in OHCA as documented in 2020 would be unexplained except for the COVID pandemic with which it was in a strong statistical relationship. Different pathophysiological reasons may support this relationship, attributable both to infection- and pandemic-related issues.
Concerning infection-related issues, the first and more predictable reason is the occurrence of cardiac arrest due to respiratory failure caused by SARS-CoV-2, as it is the most feared life-threatening complication.13,14 There are at least two elements supporting this theory. The former is the presence of suspected symptoms or of a defined diagnosis of COVID-19 before the event in 125 patients, representing 74% of the increase in OHCAs in 2020. The latter is that hypoxia is one of the causes known to be associated to non-shockable presenting rhythm,15 being one of the ‘five Hs and Ts’. This, along with the 3-min increase in EMS arrival time,16 could explain the increase in non-shockable rhythm. However, questions arise as to why these patients developed respiratory failure at home. The rapid progression toward ARDS has been reported in single case reports describing a rapid worsening to respiratory failure, even in patients who were apparently stable a few hours earlier.17,18 This could have been fatal to some patients, not leaving them sufficient time to activate the emergency system. This phenomenon is truly alarming, especially considering that the age of the patients who suffered an OHCA during the epidemic is not particularly high and is similar to that in 2019. Moreover, in some cases, the severity of the clinical situation and the risk of its rapid progression could have been undervalued, with resulting at-home care attempts favoured by the impossibility of mass hospitalization, despite extraordinary efforts of the local and national government to immediately increase ICU beds and the capacity of general wards.19 Risk factors associated with the progression to ARDS have been identified in some populations,18,20 but they were retrieved from critically ill patients with already confirmed COVID-19 pneumonia and they may not be appropriate for discriminating patients at risk among those treated at home. However, respiratory failure cannot be the only explanation for the increase in OHCAs. It cannot be excluded that some patients experienced arrhythmic sudden cardiac death (SCD) related to this infection. A non-negligible percentage of patients affected by COVID-19 in fact experienced myocardial injury,21–23 and a series of mechanisms possibly leading to SCD have been proposed,24 including the effect of hydroxychloroquine and azithromycin, which were proposed as a treatment for COVID-19,25 on QT interval prolongation,26 with the consequent risk of ventricular arrhythmias. Additionally, the infection itself could have played a role in prolonging the QTc values, as the elevated level of some cytokines, particularly interleukin-6 (IL-6), can suppress IKr in heterologous cells and myocytes, resulting in prolonged repolarization, and IL-6 also markedly blunted the hERG/IKr channel mRNA and protein expression.27 Recent evidence highlighting that the QTc values might be at the upper limits or even prolonged in many patients with COVID-19, even before starting drugs potentially causing QTc prolongation, also seems to confirm this mechanism.28 Notably, in four out of six patients of our population with suspected or diagnosed COVID-19 and a post-ROSC ECG available, a prolonged QTc was found. However, we found that also in non-suspected or diagnosed COVID-19 patients, the percentage of those with a prolonged QTc was similar, possibly caused by myocardial ischaemia. Indeed, it has been known for >40 years that a prolongation of the QT interval is associated with a major increase in the risk for ventricular arrhythmias and SCD either after a myocardial infarction29 or in the general population.30,31
In addition, digestive symptoms (i.e. diarrhoea and vomiting) are present in a fair number of COVID-19 patients, especially in those with mild disease severity, with a delayed diagnosis and treated at home,32 and they were also experienced by 7% of the suspected or diagnosed COVID-19 patients in our cohort. All these conditions may favour hypokalaemia, which can drive powerful electrophysiological effects on the myocardial cells, promoting life-threatening ventricular arrhythmias.33 Moreover, recent data suggest that pulmonary embolism (PE) could be a complication in COVID-19 patients,34 and this could have been another cause of OHCA in our population, consistent with a non-shockable presenting rhythm.
Last, but not least, considering the pandemic-related issues, another possible reason for the increase of OHCAs could reside in the increased deterioration at home, with electrical or mechanical complications of time-dependent cardiovascular disease that normally would have been treated earlier. This hypothesis is fully supported by our evidence of a 40.2% reduction in 2020 of the number of patients transported for STEMI, despite an increase in the number of all emergency calls managed by the EMS dispatch centre, which is absolutely in line with other experiences from northern Italy, Spain, and the USA,35–37 and it leads to the conclusion that a considerable number of patients experienced a myocardial infarction at home, exposing themselves to an increased risk of SCD.38 The two possible explanations for this issue could be the fear of being infected in the hospital or the desire to not further burden the health system, both resulting in non-activation of the emergency system. This brings about the need for specific information campaigns addressed at the population explaining the importance both of the quarantine and of early activation of the EMS in the case of effective need.
We also observed that the characteristics of OHCAs during the outbreak are different compared with those of a normal period. We highlighted an increase in medical aetiology over other types of aetiologies, and this further reinforces the hypothesis that the increase in the incidence of OHCAs is probably related to the direct (i.e. respiratory failure at home, SCD due to SARS-CoV-2 myocardial involvement or treatment) or indirect (i.e. lack of EMS activation in the case of time-dependent pathologies) effect of the COVID-19 epidemic. Moreover, consistently with the lockdown that was adopted in Italy,39 there was an increase in the OHCAs that occurred at home coupled, however, with a decrease in bystander-witnessed OHCAs. This is probably the result of social distancing and, in some cases, of quarantine isolation, enforcing living in different rooms or in a different house from the rest of the family. A decrease of the bystander CPR rate was also observed, and it is probably due to the issue of the fear of infection. Furthermore, a 3-min median increase in EMS arrival time was observed, reasonably affecting the percentage of non-shockable presenting rhythm.16 This delay was probably due both to the very high volume of rescues managed by EMS and to the time needed to put on PPE by EMS personnel. As a matter of fact, the EMS arrival time was longer for suspected/diagnosed COVID-19 patients than for the others. All the above aspects have led to a dramatic increase of OHCAs and, regretably, of people both dead on arrival, without any attempt of resuscitation by EMS, and dead in the field after a resuscitation attempt, highlighting COVID-19 as a disease that kills at home. This may also favour an underestimation of COVID-19 lethality, since the official statistics refer only to hospitalized patients,40 excluding those who died at home.
We believe that our evidence could be very useful to other countries, in order to optimize the treatment of COVID-19 patients and organize the emergency medical response, especially considering that SARS-CoV-2 will definitely not be defeated in a few months and recurrent outbreaks are expected already in the coming months.41
Our study has some limitations. The first consists of the relatively short period of time analysed. However, although we have analysed only the first 60 days since the start of the epidemic, our results are already impressive and highlight the close relationship between the increase in OHCAs in 2020 and the COVID-19 epidemic. Moreover, in these 60 days, the epidemic curve has reached a plateau and, nevertheless, the relationship was maintained. The second relies on the impossibility of having the certainty of the causative diagnosis of cardiac arrest for each patient, as is typical for OHCA registries. However, we believe that the statistically strong correlation, supported by clinical elements such as the evidence that more than three-quarters of the ‘extra’ patients were highly suspected of or diagnosed with COVID-19, the reduction of 40.2% of the patients with a pre-hospital diagnosis of STEMI, and the changes in the characteristics of OHCAs, can be reasonably sufficient for confirming the direct or indirect role of COVID-19 in the observed increase in the incidence of OHCA. The third limitation could be the lack of information either about home therapy at the moment of OHCA or about the previous medical history or comorbidities of the patients. Lastly, post-ROSC ECG was available only in 18 out 27 patients who achieved ROSC. This is because either the ECG was not performed by the EMS personnel or it was recorded but not transmitted to the dispatch centre or, even if transmitted, the file was unavailable due to technical issue.
Summarizing, the COVID-19 epidemic trend is associated with the difference between 2020 and 2019 OHCAs and is coupled with a reduction in the short-term outcome. Government and local health authorities should seriously consider our results when planning healthcare strategies to deal with the epidemic, not neglecting the pre-hospital issue of the emergency, especially considering the expected recurrent outbreaks.
Supplementary Material
Acknowledgements
We would like to thank all the Lombardia CARe researchers and all the EMS personnel. Lombardia CARe is a partner of the ESCAPE-NET consortium. E.B., E.C. and S.S. are member of the European Resuscitation Council (ERC) Research-net.
Lombardia CARe researchers: Sara Compagnoni, Rosa Fracchia, Antonio Cuzzoli, Andrea Pagliosa, Guido Matiz, Alessandra Russo, Andrea Lorenzo Vecchi, Cecilia Fantoni, Cristian Fava, Cinzia Franzosi, Claudio Vimercati, Dario Franchi, Enrico Storti, Erika Taravelli, Fulvio Giovenzana, Giovanni Buetto, Guido Garzena, Giorgio Antonio Iotti, Guido Francesco Villa, Marco Botteri, Salvatore Ivan Caico, Irene Raimondi Cominesi, Livio Carnevale, Matteo Caresani, Mario Luppi, Maurizio Migliori, Paola Centineo, Paola Genoni, Roberta Bertona, Roberto De Ponti, Riccardo Osti, Stefano Buratti, Gian Battista Danzi, Arianna Marioni, Antonella De Pirro, Simone Molinari, Vito Sgromo, Valeria Musella, Martina Paglino, Francesco Mojoli, Bruno Lusona, Michele Pagani, and Moreno Curti.
Funding
The Lombardia CARe Registry is partially supported by Fondazione Banca del Monte di Lombardia.
Conflict of interest: none declared.
Contributor Information
Lombardia CARe researchers:
Sara Compagnoni, Rosa Fracchia, Antonio Cuzzoli, Andrea Pagliosa, Guido Matiz, Alessandra Russo, Andrea Lorenzo Vecchi, Cecilia Fantoni, Cristian Fava, Cinzia Franzosi, Claudio Vimercati, Dario Franchi, Enrico Storti, Erika Taravelli, Fulvio Giovenzana, Giovanni Buetto, Guido Garzena, Giorgio Antonio Iotti, Guido Francesco Villa, Marco Botteri, Salvatore Ivan Caico, Irene Raimondi Cominesi, Livio Carnevale, Matteo Caresani, Mario Luppi, Maurizio Migliori, Paola Centineo, Paola Genoni, Roberta Bertona, Roberto De Ponti, Riccardo Osti, Stefano Buratti, Gian Battista Danzi, Arianna Marioni, Antonella De Pirro, Simone Molinari, Vito Sgromo, Valeria Musella, Martina Paglino, Francesco Mojoli, Bruno Lusona, Michele Pagani, and Moreno Curti
References
- 1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W.. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fauci AS, Lane HC, Redfield RR.. Covid-19—navigating the uncharted. N Engl J Med 2020;382:1268–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS.. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Livingston E, Bucher K.. Coronavirus disease 2019 (COVID-19) in Italy. JAMA 2020;doi: 10.1001/jama.2020.4344. [DOI] [PubMed] [Google Scholar]
- 5. Onder G, Rezza G, Brusaferro S.. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020;doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 6. Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Bua D, Rizzi U, Bussi D.. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Italy. N Engl J Med 2020;doi: 10.1056/NEJMc2010418. [Google Scholar]
- 7. Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, Bossaert LL, Brett SJ, Chamberlain D, De Caen AR, Deakin CD, Finn JC, Gräsner JT, Hazinski MF, Iwami T, Koster RW, Lim SH, Ma MHM, McNally BF, Morley PT, Morrison LJ, Monsieurs KG, Montgomery W, Nichol G, Okada K, Ong MEH, Travers AH, Nolan JP, Aikin RP, Böttiger BW, Callaway CW, Castren MK, Eisenberg MS, Kleinman ME, Kloeck DA, Kloeck WG, Mancini ME, Neumar RW, Ornato JP, Paiva EF, Peberdy MA, Soar J, Rea T, Sierra AF, Stanton D, Zideman DA.. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein Resuscitation Registry Templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, Interamerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 2015;132:1286–1300. [DOI] [PubMed] [Google Scholar]
- 8.Protezione Civile National Department Repository. http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1.
- 9. Corrado D, Pelliccia A, Bjørnstad HH, Vanhees L, Biffi A, Borjesson M, Panhuyzen-Goedkoop N, Deligiannis A, Solberg E, Dugmore D, Mellwig KP, Assanelli D, Delise P, Van-Buuren F, Anastasakis A, Heidbuchel H, Hoffmann E, Fagard R, Priori SG, Basso C, Arbustini E, Blomstrom-Lundqvist C, McKenna WJ, Thiene G.. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol: Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J 2005;26:516–524. [DOI] [PubMed] [Google Scholar]
- 10. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P, Baumbach A, Bugiardini R, Coman IM, Delgado V, Fitzsimons D, Gaemperli O, Gershlick AH, Gielen S, Harjola VP, Katus HA, Knuuti J, Kolh P, Leclercq C, Lip GYH, Morais J, Neskovic AN, Neumann FJ, Niessner A, Piepoli MF, Richter DJ, Shlyakhto E, Simpson IA, Steg PG, Terkelsen CJ, Thygesen K, Windecker S, Zamorano JL, Zeymer U, Chettibi M, Hayrapetyan HG, Metzler B, Ibrahimov F, Sujayeva V, Beauloye C, Dizdarevic-Hudic L, Karamfiloff K, Skoric B, Antoniades L, Tousek P, Terkelsen CJ, Shaheen SM, Marandi T, Niemel€a M, Kedev S, Gilard M, Aladashvili A, Elsaesser A, Kanakakis IG, Merkely B, Gudnason T, Iakobishvili Z, Bolognese L, Berkinbayev S, Bajraktari G, Beishenkulov M, Zake I, Lamin H Ben, Gustiene O, Pereira B, Xuereb RG, Ztot S, Juliebø V, Legutko J, Timoteo AT, Tatu-Chiţoiu G, Yakovlev A, Bertelli L, Nedeljkovic M, Studencan M, Bunc M, de Castro AMG, Petursson P, Jeger R, Mourali MS, Yildirir A, Parkhomenko A, Gale CP.. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2018;39:119–177.28886621 [Google Scholar]
- 11. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN.. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG.. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maclaren G, Fisher D, Brodie D.. Preparing for the most critically ill patients with COVID-19: the potential role of extracorporeal membrane oxygenation. JAMA 2020;323:1245–1246. [DOI] [PubMed] [Google Scholar]
- 14. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B.. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Teodorescu C, Reinier K, Dervan C, Uy-Evanado A, Samara M, Mariani R, Gunson K, Jui J, Chugh SS.. Factors associated with pulseless electric activity versus ventricular fibrillation: the Oregon Sudden Unexpected Death Study. Circulation 2010;122:2116–2122. [DOI] [PubMed] [Google Scholar]
- 16. Waalewijn RA, Nijpels MA, Tijssen JG, Koster RW.. Prevention of deterioration of ventricular fibrillation by basic life support during out-of-hospital cardiac arrest. Resuscitation 2002;54:31–36. [DOI] [PubMed] [Google Scholar]
- 17. Goh KJ, Choong MC, Cheong EH, Kalimuddin S, Duu Wen S, Phua GC, Chan KS, Haja Mohideen S.. Rapid Progression to acute respiratory distress syndrome: review of current understanding of critical illness from COVID-19 infection. Ann Acad Med Singapore 2020;49:1–9. [PubMed] [Google Scholar]
- 18. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y.. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020;doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Grasselli G, Pesenti A, Cecconi M.. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020;doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 20. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y.. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020;8:475–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C.. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z.. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, Jain SS, Burkhoff D, Kumaraiah D, Rabbani LR, Schwartz A, Uriel N.. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation 2020;141:1648–1655. [DOI] [PubMed] [Google Scholar]
- 24. Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C.. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol 2020;31:1003–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gautret P, Lagier J-C, Parola P, Hoang VT, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Dupont HT, Honoré S, Colson P, Chabrière E, La Scola B, Rolain J-M, Brouqui P, Raoult D.. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020;doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 26. Chang D, Saleh M, Gabriels J, Ismail H, Goldner B, Willner J, Beldner S, Mitra R, John R, Epstein LM.. Inpatient use of ambulatory telemetry monitors for COVID-19 patients treated with hydroxychloroquine and/or azithromycin. J Am Coll Cardiol 2020;doi: 10.1016/j.jacc.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Aromolaran AS, Srivastava U, Alí A, Chahine M, Lazaro D, El-Sherif N, Capecchi PL, Laghi-Pasini F, Lazzerini PE, Boutjdir M.. Interleukin-6 inhibition of hERG underlies risk for acquired long QT in cardiac and systemic inflammation. PLoS One 2018;13:e0208321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Saleh M, Gabriels J, Chang D, Kim BS, Mansoor A, Mahmood E, Makker P, Ismail H, Goldner B, Willner J, Beldner S, Mitra R, John R, Chinitz J, Skipitaris N, Mountantonakis S, Epstein LM.. The effect of chloroquine, hydroxychloroquine and azithromycin on the corrected QT interval in patients with SARS-CoV-2 infection. Circ Arrhythmia Electrophysiol 2020;doi: 10.1161/CIRCEP.120.008662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Schwartz PJ, Wolf S.. QT interval prolongation as predictor of sudden death in patients with myocardial infarction. Circulation 1978;57:1074–1077. [DOI] [PubMed] [Google Scholar]
- 30. Algra A, Tijssen JGP, Roelandt JRTC, Pool J, Lubsen J.. QTc prolongation measured by standard 12-lead electrocardiography is an independent risk factor for sudden death due to cardiac arrest. Circulation 1991;83:1888–1894. [DOI] [PubMed] [Google Scholar]
- 31. Wellens HJJ, Schwartz PJ, Lindemans FW, Buxton AE, Goldberger JJ, Hohnloser SH, Huikuri H V., Kääb S, La Rovere MT, Malik M, Myerburg RJ, Simoons ML, Swedberg K, Tijssen J, Voors AA, Wilde AA.. Risk stratification for sudden cardiac death: current status and challenges for the future. Eur Heart J 2014;35:1642–1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Han C, Duan C, Zhang S, Spiegel B, Shi H, Wang W, Zhang L, Lin R, Liu J, Ding Z, Hou X.. Digestive symptoms in COVID-19 patients with mild disease severity. Am J Gastroenterol 2020;doi: 10.14309/ajg.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lazzerini PE, Boutjdir M, Capecchi PL.. COVID-19, arrhythmic risk and inflammation: mind the gap! Circulation 2020;doi: 10.1161/CIRCULATIONAHA.120.047293. [DOI] [PubMed] [Google Scholar]
- 34. Poissy J, Goutay J, Caplan M, Parmentier E, Duburcq T, Lassalle F, Jeanpierre E, Rauch A, Labreuche J, Susen S.. Pulmonary embolism in COVID-19 patients: awareness of an increased prevalence. Circulation 2020;doi: 10.1161/CIRCULATIONAHA.120.047430. [DOI] [PubMed] [Google Scholar]
- 35. De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omedè P, Pennone M, Patti G, Mancone M, De Ferrari GM.. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med 2020;doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, Martín-Moreiras J, Ramón Rumoroso J, López-Palop R, Serrador A, Cequier Á, Romaguera R, Cruz I, de Prado AP, Moreno R.. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC Interv Cardiol 2020;2:82–89. [Google Scholar]
- 37. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP, Henry TD.. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Grines C, Patel A, Zijlstra F, Weaver WD, Granger C, Simes RJ.. Primary coronary angioplasty compared with intravenous thrombolytic therapy for acute myocardial infarction: six-month follow up and analysis of individual patient data from randomized trials. Am Heart J. 2003;145:47–57. [DOI] [PubMed] [Google Scholar]
- 39. Parmet WE, Sinha MS.. Covid-19—the law and limits of quarantine. N Engl J Med 2020;382:E281–E283. [DOI] [PubMed] [Google Scholar]
- 40. Giulia F. Characteristics of COVID-19 patients dying in Italy. Report based on available data on March 20th, 2020https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_20_marzo_eng.pdf
- 41. Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M.. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 2020;368:860–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.