Abstract
Background
Preventing transmission of COVID-19 within prisons is both important and challenging. The confined conditions in prisons can encourage person-to-person spread with the potential for outbreaks occurring. Contact tracing is an important contributor to the longer-term management strategy for COVID-19 in prisons as well as in the community but is highly resource-intensive. This paper describes the approach to contact tracing taken by the Irish Prison Service (IPS).
Methods
The IPS National Infection Control Team, in collaboration with the National Quality Improvement (QI) team and Health Service Executive (HSE) in Ireland, implemented a programme to develop and train in-prison contact tracing teams (CTTs). CTTs were run by prison staff with experience of working with detainees, prison IT systems and CCTV. Protocols for undertaking contact tracing for both detainee and staff cases of COVID-19 were established.
Results
All prisons, and two support agencies, within the IPS now have fully functional in-prison CTTs. Every CTT has responded to at least one case COVID-19, undertaken contact tracing and instigated quarantine of contacts.
Conclusions
A partnership approach with development of prison-led CTTs can provide an effective mechanism for contact tracing of COVID-19 cases within the prison setting.
Keywords: Covid-19, Prison, Public Health, Contact Tracing
Introduction
Preventing the transmission of COVID-19 within prisons and other prescribed places of detention (PPDs) is an integral part of the public health response to the current pandemic.1 PPDs concentrate individuals who may be vulnerable to severe infection due to poor health profiles, and the confined conditions in which detainees live can encourage person-to-person spread, increasing the basic reproduction number (R0) above that seen in the general population.1,2,3 Furthermore, outbreaks of COVID-19 within these settings have the potential to overwhelm prison healthcare services and place additional burden on hospital critical care units in the community.
Guidance for how to prevent and control COVID-19 outbreaks within PPDs is commonly adapted from the guidance for the general public, with additional measures included to reflect the increased susceptibility of the population and likelihood of explosive outbreaks. Therefore, the approach to COVID-19 in PPDs often reflects the approach for the country as a whole. Social distancing measures adopted by many countries across the world are challenging to implement in prisons, where individuals are already deprived of their liberty. There have been various approaches to facilitate this such as implementing ‘restricted regimens’ within prisons and by enabling single cell accommodation through movement of people in prison to alternative accommodation, temporary or early release of detainees, and through increasing community disposals.4
As countries look to move forward and consider easing social distancing measures, alternative approaches will need to be explored in order to prevent a resurgence of cases. Contact tracing is an important contributor to the longer-term management strategy for COVID-19 both in the community and prisons. Contact tracing aims to rapidly identify secondary cases that may arise through transmission from known cases, allowing for intervening action to take place to interrupt further onward transmission. In a prison setting, this outbreak management tool has the potential to rapidly deploy sufficient resources and bring outbreaks to a close quickly. However, the resource implications of these activities in terms of personnel are significant.5
Successes in managing COVID-19 to date have been informed by international experiences, learning from countries where strategies and actions have already been established. In Ireland, contact tracing is central to the response strategy and is currently being implemented alongside social distancing measures.6 This approach has been extended to all prisons within Ireland, with the adoption of a broader case definition to provide further protection against prison-level outbreaks.
This paper describes the approach to contact tracing in the Irish Prison Service (IPS).
Methods
Aim of the programme
Within Ireland, contact tracing for cases of COVID-19 is primarily managed by the national public health agency, Public Health (PH). However, similar to many countries, the rapid increase in the number of cases has impacted on the capacity of PH to manage the volume of contact tracing required in all areas of the wider community. A Contact Management Programme (CMP) was established in prisons to enable contact tracing to operate at scale and to support the work being done by PH, with the National Quality Improvement (QI) team providing an education and training enabling function within the CMP. In response to the contact tracing requirements in prisons, the IPS National Infection Control Team (NICT), with the support of PH and the National QI team, commenced a programme to develop and train contact tracing teams (CTTs) within prisons. CTTs were intended to be prison-based and run by members of staff from within each prison. The aim of this programme was to enable the IPS to assist PH in the early identification of people that may have been exposed to COVID-19 and take action to prevent onward transmission.
Contact tracing teams
The NICT manager initially contacted all Governors within the IPS to outline the importance of contact tracing in the management of COVID-19 within prisons and the proposed programme for achieving this. Governors were then asked to suggest names of personnel within their prison staff who they considered would be interested in being invited to be part of a CTT.
Selection criteria for CTT members included:
Experience in the use of CCTV within the prison.
Ability to use the prison IT system, including use of Microsoft® Excel®.
Ability to use the IPS rostering/clocking system.
These prerequisites were essential to ensure that the CTTs had the expertise required to establish the movements of detainees and staff and therefore identify any potential contacts of cases.
Each CTT was made up of a minimum of four members of staff either side of the roster, which consisted of Security Chiefs, Assistant Chief Officers, Prison Officers, an Assistant Psychologist and clerical staff. The final membership of the CTT within each prison was determined locally, taking into account the skill sets of members.
Development and delivery of training
The NICT, PH and the National QI team jointly developed a contact tracing training package. This tripartite collaboration was crucial to ensuring that the required standard of contact tracing would be accomplished.
Training then occurred in two phases. The first phase involved delivery of a ‘Train-the-Trainer’ package for all members of the NICT, under the guidance of PH and the National QI team. Once trained, NICT members then delivered face-to-face training to the 158 staff across the IPS who had been selected to be members of a CTT. CTTs training consisted of the following:
(i) An overview of COVID-19 and modes of transmission.
(ii) A description of the contact tracing process.
(iii) An introduction to the interview scripts.
On completion of the training, all members of the CTTs were provided with contact tracing protocols, interview scripts for undertaking contact tracing of both staff and detainee cases and an Excel® template for collection of information regarding close and casual contacts of cases.
Process of contact tracing within prisons
Within the IPS, contact tracing is commenced for all confirmed and highly probable cases of COVID-19 amongst both detainees and prison staff (see Box 1 for case definitions).
Box 1.
Case definitions.
Confirmed case: An individual with laboratory confirmed COVID-19.
Highly probable case: An individual with either a cough, a fever of 38.0 °C or above or shortness of breath.
The process of contact tracing is summarized in Fig. 1. Once a case is identified by, or reported to, a member of prison staff, they immediately notify the CTT. The case is then interviewed by a member of the CTT to establish all close and casual contacts during the 48 hours prior to, and during the period since, symptom onset in the case (see Box 2 for definitions of contacts).
Fig. 1.
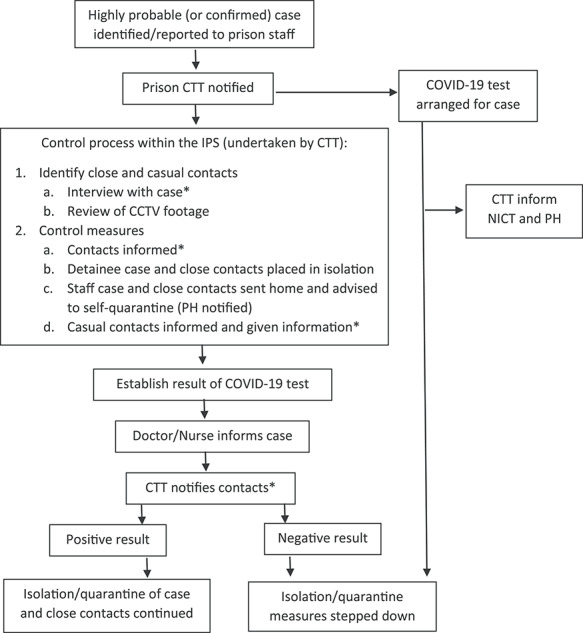
Outline of the contact tracing process within the IPS.
Box 2.
Definitions of close and casual contacts.
Contact tracing includes contact from 48 hours before symptom onset.
Close contact:
Any person who has shared a space with for longer than 2 hours with a case.
Any person who has had face-to face contact with a case for a total of 15 minutes over the period of a day.
Any person who has not worn appropriate PPE or had a breach of PPE when dealing with a case.
Casual contact:
Any person who has shared a closed space with a case for less than 2 hours.
Any person who has worn appropriate PPE and taken recommended infection control precautions and that has direct contact with a case or their body fluids.
Any person who has shared a closed space with a case for longer than 2 hours but, following a risk assessment, does not meet the definition of a close contact.
A member of the CTT also reviews any CCTV footage from within the prison, which contains footage of the case during the 48 before, and period since, symptom onset. This process is used to identify any additional contacts not reported during the interview with the case and to provide further details on the nature and proximity of contact events.
Information relating to the case and all close and casual contacts is collected and recorded in an Excel® spreadsheet and saved securely on the prison IT system. This data comprises name of the case, date of symptom onset, the result of their COVID-19 test and symptom status of any close and casual contacts. This information is securely emailed to the NICT and PH. This data is collated centrally by PH in the Health Service Executive (HSE).
Management of contacts
All close contacts are considered ‘at risk’. Detainee close contact are placed in isolation within the prison, and staff close contacts are advised that they need to self-quarantine at home. The period of isolation/quarantine is dependent on the COVID-19 test result of the case. If the case returns a negative result, the close contacts are informed that they no longer need to be in isolation/quarantine, provided they are asymptomatic. If the case returns a positive result, the close contacts are informed that they need to remain in isolation/quarantine for 14 days from the date of contact with the case. During this period detainee close contacts receive daily clinical monitoring. Any staff close contacts are notified to PH and followed up by the community CMP. If close contacts develop symptoms consistent with COVID-19, they are then required to remain in isolation/quarantine, testing is arranged, and tracing of their contacts is also undertaken.
Casual contacts identified are provided with an information leaflet, which advises that they do not need to isolate/self-quarantine but that they should self-monitor for signs and symptoms of COVID-19.
Supporting resources
To support contact tracing, information leaflets about COVID-19 and contact tracing were developed for both detainees and prison staff, as well as posters for display around the prisons.
Flow charts for use within the IPS detailing the procedures for reporting cases, contact tracing and follow-up were jointly developed and agreed by the IPS, the National QI team and HSE. Scripts were created for use by the CTTs for each step of the contact tracing process: the initial interview with the case to establish contacts, the discussion with contacts regarding isolation/quarantine and symptoms and the follow-up discussion with contacts following the test result of the case. Leaflets for close contacts were developed to provide information about what activities are and are not permitted during isolation/quarantine; how to safeguard themselves and others, including those who may be at higher risk of complications from COVID-19; and what to do if they become symptomatic themselves.
Results
Contact tracing teams
All 12 prisons and the two support agencies, Operational Support Group (OSG) and Prison Service Escort Corp (PSEC), within the IPS now have fully functional in-prison CTTs. Every CTT has responded to at least one case of highly probable or confirmed COVID-19, undertaken contact tracing and instigated quarantine of contacts.
Detainee cases
Between 6 April (date of establishment of the first CTT) and 22 May 2020 (time of writing), there have been 66 highly probable cases of COVID-19 identified amongst prison detainees, all of which have subsequently tested negative for COVID-19. There have been no confirmed cases of COVID-19 amongst the detainee population in the IPS during this period.
A total of 84 close contacts (50 detainees, 9 staff and 25 externals) of detainee cases were identified and followed up by prison CTTs, resulting in a mean of 1.3 close contacts per detainee case.
Staff cases
Between 6 April and 22 May 2020, there have been 119 highly probable and 45 confirmed cases of COVID-19 identified amongst prison staff. This includes 13 historic cases, which predated the establishment of the CTT in every prison.
A total of 448 close contacts of staff cases were identified and followed up by prison CTTs, all of whom were prison staff members, resulting in a mean of 2.8 close contacts per staff case.
Discussion
Main finding of this study
We have described an approach to implementing contact tracing for cases of COVID-19 within prisons, with the aim of preventing and controlling outbreaks. By taking a collaborative approach, the prison service and the national public health agency in Ireland were able to achieve the rapid creation and deployment of in-prison CTTs in every estate within the IPS. Working to agreed contact tracing protocols, CTTs have undertaken contact tracing for 230 cases within the IPS to date.
What is already known on this topic
Contact tracing can be a highly effective approach to controlling the spread of COVID-19 and preventing outbreaks.3 However, this activity is highly labour intensive and can quickly place a strain on the resources of public health organizations.
What this study adds
To our knowledge, there has not been any scientific literature published on the subject of contact tracing for cases COVID-19 in PPDs. This case study provides an example of a partnership approach to contact tracing that could be adopted by other countries over the next few months as they look for alternatives to the highly restrictive social distancing measures currently in place across Europe and elsewhere.
The approach taken in Ireland demonstrates that prison-based CTTs, run by prison staff, are ideally placed for undertaking contact tracing within prisons. Prison staff are experienced in working with detainees and fellow staff members. They are physically located within prisons and therefore have the ability to rapidly respond to notifications, complete interviews with cases and implement isolation/quarantine of the case and contacts. The ability to conduct contact tracing without delay, starting on the day that a case is identified, avoids missing opportunities to prevent further onward transmission from potentially infected contacts.
Furthermore, prison staff selected for CTTs in the IPS were experienced at accessing and interpreting prison CCTV. This means they are able to use this information to enhance intelligence gathered through interview and establish whether there are any additional contacts not previously discovered. An additional benefit of prison staff specifically undertaking this activity is that their familiarity with detainees and staff enables them to identify individuals by sight on the CCTV footage.
The combination of contact tracing interviews with CCTV footage has also provided an opportunity to identify ‘hotspots’ within prisons where advised social distancing is not being observed. CTTs have been able to use this information to help inform activities aimed at improving adherence to social distancing advice.
Limitations of this study
The epidemiology of COVID-19 in both the detainee and staff populations within the IPS is reflective of the number of cases of the disease within Ireland, and this may limit the applicability of this case study to other countries where the incidence may be different.7 Furthermore, the absence of any confirmed cases of COVID-19 amongst detainees in the IPS means that it is not possible to draw any conclusions about the effectiveness of this contact tracing approach in preventing transmission or outbreaks within the prison estate in Ireland.
The number of prisons and size of the prison population within the IPS is smaller than many countries. It is possible that larger prison services may find it challenging to adopt the approach taken in Ireland. However, this approach was designed with the aim of enabling prisons to take a key role in the contact tracing process and therefore has the ability to be scaled up.
Contact tracing of cases in prisons is only part of the IPS’s response to the COVID-19 pandemic. Every country is likely to need to implement a range of measures to prevent and control outbreaks of COVID-19 in PPDs.
Conclusions
A partnership approach involving community public health expertise, QI input and support and prison resources can provide an effective mechanism for contact tracing of COVID-19 cases within the vulnerable prison setting. As countries look to explore alternatives to stringent social distancing measures, in-prison CTTs offer a potential solution to the significant resource burden of implementing contact tracing in prisons and other PPDs.
Funding
No funding was received for this study.
Conflicts of interest
No conflicts of interest to declare.
Acknowledgements
The authors would like to thank Elaine Dunne (IPS), Liam Philips (IPS), Philip Kennedy (IPS), Padraic Carty (IPS), Tom Malone (IPS), Mark Farrelly (IPS), Darren McDonnell (IPS), Dr Mary Browne (HSE), Lisa Toland (HSE), Lorraine Murphy (HSE) and Dr Philip Crowley (HSE).
Mattea Clarke, Specialist Registrar in Public Health
John Devlin, Executive Clinical Lead
Emmett Conroy, Infection Prevention & Control Manager
Enda Kelly, National Operational Nurse Manager
Sunita Sturup-Toft, Public Health Specialist
References
- 1. Kinner SA, Young JTK, Southalan L et al. . Prisons and custodial settings are part of a comprehensive response to COVID-19. Lancet Public Health 2020;5:e188–e189. 10.1016/S2468-2667(20)30058-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kinner SA, Young JT. Understanding and improving the health of people who experience incarceration: an overview and synthesis. Epidemiol Rev 2018;40(1):4–11. 10.1093/epirev/mxx018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. Prisons and Health 2014. http://www.euro.who.int/__data/assets/pdf_file/0005/249188/Prisons-and-Health.pdf?ua=1 (27 May 2020, date last accessed).
- 4. Ministry of Justice , Public Health England, and Her Majesty’s Prison and Probation Service. COVID-19 population management strategy for prisons https://www.gov.uk/government/publications/covid-19-population-management-strategy-for-prisons(22 May 2020, date last accessed).
- 5. Kissler SM, Tedijanto C, Goldstein E et al. . Projecting the transmission dynamics of SARS-CoV-1 through the postpandemic period. Science> 2020; 22;368(6493):860–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Department of Health Ireland's response to COVID-19 (Coronavirus) https://www.gov.ie/en/publication/a02c5a-what-is-happening/#Irelands-response-to-confirmed-cases(21 April 2020, date last accessed).
- 7. World Health Organization Coronavirus disease (COVID-2019) situation reports: Situation report – 117, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (16 May 2020, date last accessed).


