We report a COVID-19 case with the longest ECMO before lung transplantation. It is also the first reported case with severe intracardiac thrombus complication of the SARS-CoV-2 infection.
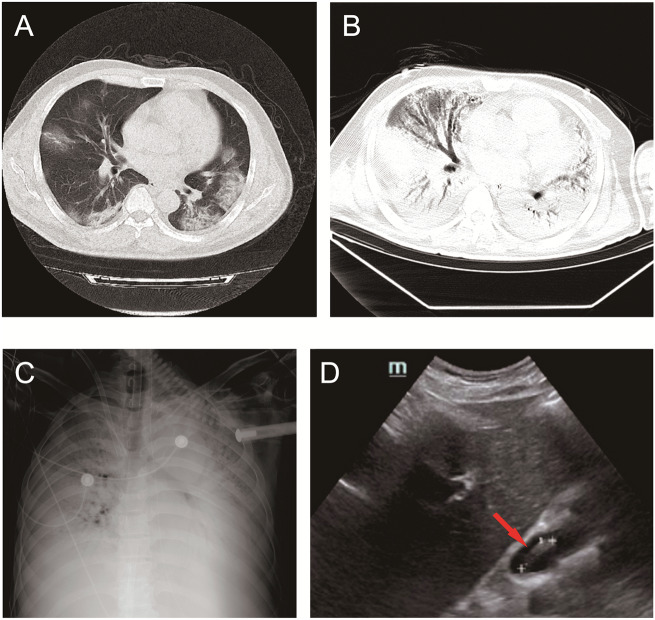
A 53-year-old previously healthy Chinese man presented with muscle soreness, dry cough, and fever for 5 days. Computed tomography (CT) confirmed diffuse ground-glass infiltrates of both lungs (Panel A). Nucleic acid test was positive for COVID-19 infection. His condition rapidly deteriorated in spite of prompt antivirus, anti-inflammatory, immunoenhancer, glucocorticoid, and supportive therapies. Soon he produced more purulent secretions, and developed acute respiratory distress syndrome, metabolic acidosis, septic shock, and multiple organ failure. He was intubated, and extracorporeal membrane oxygenation (ECMO, V-V mode) was started. A subsequent CT indicated large-sized heterogeneous high-density shadows with incomplete expansion in both lungs, and pleural effusion (Panel B). X-ray displayed a typical ‘white lung’ sign, without a clear border of the heart and mediastinum (Panel C).
On day 34 after ECMO was initiated, an echocardiogram revealed a mobile, linear, and large-sized (3.3 × 0.6 cm) echogenic mass in the right atrium, attached to the tip of the ECMO catheter (Panel D). The right ventricular outflow tract (RVOT) became widened, pulmonary artery pressure was significantly increased, and left ventricular diastolic function was markedly decreased. Anticoagulation therapy was started immediately, and adjusted based on frequently monitored clotting function (Supplementary material online, Figure 1). Ten days later, thrombus was no longer detected throughout the heart or large vessels. After three transfusions of serum from COVID-19 survivors, his nucleic acid test was finally negative. Eventually, he received a lung transplantation after 72 days with ECMO. At present (1 month after transplantation), the patient is recovering well with inpatient rehabilitation.
This is by far the longest ECMO use reported in a COVID-19 case before lung transplantation. It highlights the possible beneficial effect of serum from a COVID-19-recovered patient in rescuing critically ill cases. The intracardiac thrombus complication of the SARS-CoV-2 infection has not been reported before, but our finding is in accord with increasingly reported higher thrombotic risk in COVID-19 patients. The coagulation risk/events in COVID-19 patients requiring haemodynamic support devices need to be considered and monitored carefully.
We are grateful for the dedicated involvement of Dr Fuxiang Li from the Intensive Care Department in General Hospital of the West Theater Command of the People’s Liberation Army.
The study was supported by the National Natural Science Foundation of China (no. 81670304).
Supplementary material is available at European Heart Journal online.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.