Abstract
As a result of the emergence of coronavirus disease 2019 (COVID-19) outbreak caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in the Chinese city of Wuhan, a situation of socio-economic crisis and profound psychological distress rapidly occurred worldwide. Various psychological problems and important consequences in terms of mental health including stress, anxiety, depression, frustration, uncertainty during COVID-19 outbreak emerged progressively. This work aimed to comprehensively review the current literature about the impact of COVID-19 infection on the mental health in the general population. The psychological impact of quarantine related to COVID-19 infection has been additionally documented together with the most relevant psychological reactions in the general population related to COVID-19 outbreak. The role of risk and protective factors against the potential to develop psychiatric disorders in vulnerable individuals has been addressed as well. The main implications of the present findings have been discussed.
Introduction
As a result of the emergence of coronavirus disease 2019 (COVID-19) outbreak caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in the Chinese city of Wuhan, a situation of socio-economic crisis and psychological distress rapidly occurred worldwide. Although social activities have been restricted in most countries, almost all not essential individual movements were prohibited due to quarantine, while the local hospitals received suddenly thousands of critically ill COVID-19 patients and were forced to implement their emergency protocols. In this context, the general population as well as most of the front-line healthcare workers became vulnerable to the emotional impact of COVID-19 infection1 due to both the pandemic and its consequences worldwide.2,3
Many psychological problems and important consequences in terms of mental health including stress, anxiety, depression, frustration, uncertainty during COVID-19 outbreak emerged progressively.4 Common psychological reactions related to the mass quarantine which was imposed in order to attenuate the COVID-19 spread are generalized fear and pervasive community anxiety which are typically associated with disease outbreaks, and increased with the escalation of new cases together with inadequate, anxiety-provoking information which was provided by media.5 The psychological reactions to COVID-19 pandemic may vary from a panic behavior or collective hysteria6 to pervasive feelings of hopelessness and desperation which are associated with negative outcomes including suicidal behavior.2 Importantly, other health measures may be compromised by abnormally elevated anxiety.7
As the general population became increasingly exposed, anxiety-provoking topics related to this emergence of the health and socio-economic crisis need to be rapidly identified to early detect dysfunctional processes and maladaptive lifestyle changes potentially leading to the onset of psychiatric conditions.8
Given this background, this work aimed to comprehensively review the current literature about the impact of the COVID-19 epidemic on the mental health in the general population.
The psychological impact of quarantine related to COVID-19 infection
The modern world in which all individuals are able to rapidly travel and communicate has been rarely forced to the current social isolation and restrictions which are linked to feelings of frustration and incertainty. This unprecedented situation related to COVID-19 outbreak is clearly demonstrating that individuals are largely and emotionally unpreparated to the detrimental effects of biological disasters that are directly showing how everyone may be frail and helpless.
Social distancing and important lockdown restrictions have been carried out first in China and later in most European countries where Italy and Spain experienced a tragic growth of the number of positive cases.9 Although government regulations are necessary to maintain social balance and guarantee the safety of all individuals, a direct strategy aimed to manage the psychosocial issues related to COVID-19 crisis and its consequences in the community is currently lacking.
The psychological outcomes for subjects who have been quarantined compared with those who did not, have been examined by both cross-sectional10–14 and longitudinal studies.15,16Table 1 summarized the most relevant information about the psychological impact of lockdown restrictions and quarantine included in these studies.
Table 1.
Most relevant studies about the psychological impact of lockdown restrictions and quarantine due to global infections
| Author(s) | Study design | Sample | Main results | Limitations | Conclusions |
|---|---|---|---|---|---|
| Bai et al.10 | Cross-sectional | 338 staff members in a hospital in East Taiwan with potential contacts with SARS | Seventeen staff members (5%) reported an acute stress disorder. The experience of quarantine was the most relevant predictor of acute stress disorder. Participants manifested predominantly anxiety, irritability, insomnia, poorer concentration and performance, reluctance to work due to the contact with febrile patients. Sixty-six staff members (20%) felt stigmatized and rejected in their neighborhood. | (i) The preliminary nature of the findings; (ii) the moderate response rate; (iii) voluntary nature of the survey (selection bias); lack of validity in the absence of face-to-face interviews. | An integrated administrative and psychosocial response to the occupational and psychological challenges caused by outbreaks is needed |
| Liu et al.11 | Cross-sectional | 549 hospital staff | Overall, 9% had higher depressive symptoms 3 years after quarantine. Among subjects with higher depressive symptoms, nearly 60% had been quarantined while only 15% of the group with lower depressive symptoms had been imposed restrictions. | (i)the cross-sectionalnature of results; (ii) the absence of a true control group comparison; (iii) the use of CES-D to measure depression. | Hospital staff and subjects in quarantine due to infective outbreaks may be at elevated risk for depression, even over the long term. |
| Sprang and Silman12 | Cross-sectional | 398 adult respondents | The mean post-traumatic stress scores were four times higher in children who had been quarantined relative to those who were not quarantined. | (i) Responses are potentially flawed by recall bias and social desirability; (ii) respondents who completed the survey represent a self-selected group. | Pandemic disasters need specific response strategies to guarantee behavioral health needs of both children and families. |
| Taylor et al.13 | Cross-sectional | 2760 horse owners | Higher psychological distress during the outbreak was reported in >30% of horse owners quarantined for several weeks due to equine influenza outbreak relative to ∼10% of the Australian general population. | (i) Findings are difficult to be generalized as it was not possible to identify, bound or sample the target population accurately. | Younger subjects, individuals with no educational qualifications, and subjects the main income of which was linked to a horse-related industry were more vulnerable to psychological distress. |
| Wu et al.16 | Cross-sectional | Hospital employees even 3 years after this experience | Being quarantined resulted a predictor of PTS symptoms. Symptoms related to quarantine were reported in 28% of parents relative to 6% of those who were not quarantined. 9% among the Hospital staff reported higher depressive symptoms 3 years after quarantine. Among subjects with higher depressive symptoms, >50% had been quarantined than 15% of the group with lower depressive symptoms. | (i) No causal relation between risk perception and PTS symptoms may be established; (ii) PTS symptoms have been measured using the IES-R. | The psychological impact of stressful events linked to infectious disease outbreaks may be mediated by individual perceptions of these events. Altruism may help to protect healthcare workers against these negative impacts. |
| Reynolds et al.15 | Cross-sectional | 1912 adult individuals | Of individuals who have been quarantined as in close contact with those who potentially have SARS, 20% reported fear, 18% nervousness, 18% sadness and 10% guilt. Maladaptive psychological reactions such as avoidance behaviors (e.g. minimizing direct contact with patients and not reporting to work) may be really common even after quarantine. | (i) The response rate was 55%; (ii) younger persons were under-represented; (iii) Information were not collected on specific socioeconomic details. | Improvements in terms of compliance and reduced psychological distress may be performed by minimizing duration, revising requirements, and providing enhanced education/support. |
| Jeong et al.27 | Longitudinal prospective | 1656 South Korea residents isolated for 2-week due to having contact with MERS patients | Anxiety symptoms were present in 7.6%, and feelings of anger in 16.6% during the isolation period. At 4–6 months after release from isolation, anxiety symptoms were observed in 3.0. Feelings of anger were present in 6.4%. Risk factors for anxiety/anger at 4–6 months included symptoms related to MERS during isolation, inadequate supplies, social networking activities, history of psychiatric illnesses and financial loss. | (i) The inclusion of subjects with higher priority in the survey; (ii) the use of self-report (GAD-7 to assess anxiety and STAXI-2 to assess anger) measures. | Mental health problems might be prevented by providing mental health support to subjects with vulnerable mental health, and providing accurate information together with adequate supplies. |
| Wu et al.16 | Longitudinal prospective | 549 randomly selected hospital employees | Current alcohol abuse/ dependence symptom counts 3 years after the outbreak were associated with having been quarantined, or having worked in high-risk locations such as SARS wards. PTS and depression were also linked to increased alcohol abuse/dependence. After regression analyses, hyperarousal resulted associated with alcohol abuse/dependence. | (i) Information on the hospital employees’ pre-SARS alcohol use patterns was not available; (ii) alcohol abuse/dependence diagnoses were performed using a single instrument measuring levels of alcohol abuse/dependence. | Exposure to severe infectious disease may lead not only to PTSD but even to other psychiatric conditions such as alcohol abuse/dependence. |
MERS, Middle East Respiratory Syndrome; IES-R, Event Scale-Revised; PTS, post-traumatic stress; PTSD, post-traumatic stress disorder; SARS, severe acute respiratory syndrome; CED-S, Center for Epidemiologic Studies Depression Scale; GAD-7, General Anxiety Disorder-7; STAXI-2, State-Trait Anger Expression Inventory 2.
Other studies reported a higher prevalence of subjects with psychological symptoms,17 emotional disturbance,18 depression,19 stress,20 mood alterations and irritability, insomnia,21 post-traumatic stress symptoms,15 anger22 and emotional exhaustion5 among those who have been quarantined. Notably, fear, anger, anxiety and insomnia, confusion, grief and numbness have been identified as additional psychological responses to quarantine. Long-term behavioral changes like vigilant handwashing and avoidance of crowds as well as a delayed return to normality even after many months after the quarantine were also reported.23 Thus, the quarantine period seems to have important and dysfunctional psychological consequences on the individual’s mental health not only in the short-term but even in the long-term period.
COVID-19 infection on the mental health: which are the main psychological reactions in the general population?
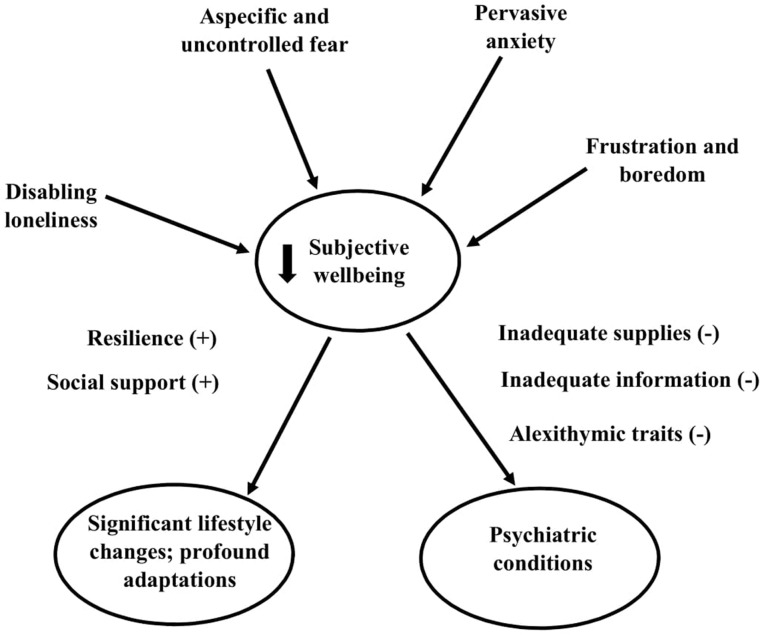
Existing evidence clearly showed the most relevant and profound psychological impact of the outbreaks on the general population.24–27Figure 1 summarized the most relevant psychological reactions in the general population related to COVID-19 infection. Although aspecific and uncontrolled fears related to infection, pervasive anxiety, frustration and boredom, loneliness have been hypothesized to impair subjective wellbeing and quality of life, resilience and enhanced social support are protective factors that may help with regard to lifestyle changes and re-adaptation mechanisms.24,25
Figure 1.
Summary of the most relevant psychological reactions in the general population related to COVID-19 infection.
Most relevant psychological reactions to COVID-19 infection
Aspecific and uncontrolled fears related to infection
This is commonly one of the most frequent psychological reaction to pandemics. Several existing studies demonstrated that those who have been exposed to the risk of infection may develop pervasive fears about their health, worries to infect others and fear infecting family members.10,23,27,28 Jeong et al.27 reported that these individuals are more vulnerable than others to manifest worries if they experienced physical symptoms potentially linked to the infection and fear that symptoms are directly associated to actively having the infection even several months after the exposure. Other studies reported that pregnant women and individuals with young children are the most at risk to develop the fear of becoming infected or transmitting the virus.29
Pervasive anxiety
Social isolation related to restrictions and lockdown measures are linked to feelings of uncertainty for the future, fear of new and unknown infective agents resulting in abnormally increased anxiety.25 Anxiety may be directly related to sensorial deprivation and pervasive loneliness, in this case first insomnia but later depression and post-traumatic stress occurred. In addition, anxiety is closely associated with fatigue and reduced performance in healthcare workers while boredom and loneliness are directly related to anger, frustration and sufferings linked to quarantine restrictions.26 Furthermore, additional tragic effects associated with pervasive anxiety in a pandemic period may include the perceived lower social support, separation from loved ones, loss of freedom, uncertainty and boredom.30
Frustration and boredom
Distress, boredom, social isolation and frustration are directly related to confinement, abnormally reduced social/physical contact with others, and loss of usual habits.15,19,20,23,28,29 As reported by Jeong et al.,27 frustration and pervasive loneliness seem to derive by the inhibition from daily activities, interruption of social necessities, not taking part in social networking activities. Unfortunately, in this context hopelessness together with other individual characteristics such as the experience of childhood maltreatment as well as extreme sensory processing patterns may significantly and independently predict suicidal behavior31,32 but even the unbearable anger related to the imposition of quarantine may lead to negative outcomes.
Disabling loneliness
The final effect of social isolation is pervasive loneliness and boredom, which have potential dramatic effects on both physical and mental individual well-being. Pervasive loneliness may be significantly associated with increased depression and suicidal behavior.23 Unfortunately, the isolation is progressively enhanced by anxiety, panic or collective hysteria. Cognitive functions and decision making are firstly impaired by hyperarousal and anxiety and later by disabling feelings of loneliness. In addition, social isolation and loneliness are also associated with alcohol and drug abuse.14 Both frustration and pervasive loneliness seem to derive by the inhibition from daily activities, interruption of social necessities, inability to take part in social networking activities enhancing the risk of hopelessness and suicidal behavior in this specific context.33 Overall, it is well known that long periods of social isolation or quarantine for specific illnesses may have detrimental effects on mental well-being.34
Risk factors
Alexithymia
The risk of related quarantine distress may be also due to the presence of alexithymic traits which may reduce psychological resilience in some subgroups of individuals.35–37 Alexithymia may be literally defined as ‘no words for mood’ and was initially identified to describe cognitive and affective features in patients with psychosomatic disorders. Alexithymic individuals may show significantly higher levels of anxiety, depression and psychological distress than non-alexithymics. In summary, the alexithymia construct applied to major depressive disorder (MDD) subjects showed a significant correlation between alexithymia traits, MDD severity and increased risk of suicidal behavior.
Inadequate supplies
Importantly, feelings of frustration and incertainty tend to occur even in relation with inadequate basic supplies (e.g. food, water, clothes etc.) during the quarantine period which is a major source of worries, and anxiety/anger even after 4–6 months from quarantine.27 There are studies demonstrating that supplies provided by public health authorities in order to address the outbreak may be inappropriate or their release may be carried out too late to successfully address the needs. For instance, thermometers or masks may be received too late while water and food were only inconsistently distributed.23 DiGiovanni et al.20 reported that during the 2003 SARS outbreak in Toronto, the government was unable to meet needs for groceries and other routine supplies needed for daily living.
Inadequate information
Existing evidence20,23,29 suggest that the poor or inadequate information from public health authorities may be a significant stressor because it provides inappropriate guidelines concerning call for actions or leads to confusion about the purpose of quarantine or the importance of measures needed to interrupt the pandemic spread. Confusion may be directly related to different approaches, contradictory health messages, and poor coordination during the Toronto SARS epidemic as a result of the involvement of multiple jurisdictions and different levels of government.20 Braunack-Mayer et al.29 clearly referred to the perceived lack of transparency from health and government authorities concerning the severity of the outbreak. Finally, Reynolds et al.15 stated that post-traumatic stress symptoms may be related to perceived difficulties in interpreting quarantine protocols as well as the lack of clear rationale/guidelines.
Protective factors
Resilience
Psychological resilience may be generally defined as the ability to support or retrieve psychological well-being during or after addressing stressful disabling conditions. Although the interconnectedness increased dramatically over the past decades, similarly the vulnerability of billions of individuals across the world to existing or novel pathogens tragically increased without a corresponding enhancement in coping abilities.24 Historically, different indices have been adopted to measure resilience and individual ability to react to social, economic and political threats, including public health emergencies. Unfortunately, being less resilient to social threats, such as pandemics, may enhance the risk of developing psychiatric conditions.25 Notably, a general message of hope and social protection given by healthcare regulatory authorities and scientists not only about the risk of being infected but even about the existence of containment measurements that may be implemented in the hospitals and in the community as a whole may enhance resilience and individual abilities to successfully react to social threats.30
Social support
A higher and significant perception of social support is associated with a reduced likelihood to develop psychological distress and psychiatric conditions. Conversely, according to a recent online survey conducted in South Korea,30 most (72.0%) of the respondents reported they could get someone else’s support if they were isolated due to COVID-19, and 28.0% clearly reported they would not have social support. Adequate social support for the general population with regard to specific at risk populations (e.g. infected patients, quarantined individuals and medical professionals) should be provided by offering targeted, tailored messages according to the most reliable scientific evidence. Relevantly, a variety of mental health supporting strategies are required in pandemic areas in order to facilitate lifestyle changes and re-adaptation activities required after the occurrence of invalidating outbreaks.1,24
Preventive strategies
Specific preventive strategies at the community level such as (i) implementing effective communication and (ii) providing adequate psychological services should be carried out in order to attenuate the psychological and psychosocial impact of COVID-19 outbreak. Health education needs to be enhanced using online platforms, social fear related to COVID-19 needs to be correctly addressed while stigma and discrimination need to be recognized as major challenges able to reinforce the feelings of uncertainty in a period of social crisis. Hospitals protocols linked to the early and effective management of health emergency need to be implemented while healthcare professionals need to be supplied by adequate protective facilities.
Scientific community should provide appropriate information to attenuate the impact of anxiety, frustration, and all the negative emotions which represent important barriers to the correct management of social crisis and psychological consequences related to pandemic. Unmet needs should be rapidly identified by medical staff who need to communicate frequently and in a timely manner with most of patients to understand the risk to develop new symptoms or worsen a preexisting psychological distress. Furthermore, telephones helplines, Internet access, active social networks, dedicated blogs and forums should be implemented in order to reduce social isolation and loneliness as well as allow to specific populations (e.g. infected subjects in hospitals or quarantine settings) the successful communication with their loved ones.
Marginalized populations such as elderly individuals or those with psychological problems should be able to actively consult with clinical psychotherapists to rapidly detect warning signs. Finally, telemedicine should be really implemented especially in areas where mental health services are poorly represented or severely impaired by the rapid spread of pandemic and lockdown restrictions. Importantly, symptoms related to initial psychological crisis together with the need to perform effective interventions using personalization and monitoring of adverse drug reactions related to psychoactive medications should be detected by psychiatrists.24
Conclusion
Implementing community-based strategies to support resilience and psychologically vulnerable individuals during the COVID-19 crisis is fundamental for any community.38 The psychological impact of fear and anxiety induced by the rapid spread of pandemic needs to be clearly recognized as a public health priority for both authorities and policy makers who should rapidly adopt clear behavioral strategies to reduce the burden of disease and the dramatic mental health consequences of this outbreak.
Funding
This work was developed within the framework of the DINOGMI Department of Excellence of MIUR 2018-2022 (law 232/2016).
Conflict of interest: None declared.
References
- 1. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel Coronavirus outbreak is urgently needed. Lancet Psychiatry 2020; 7:228–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thakur V, Jain A.. COVID 2019-suicides: a global psychological pandemic. Brain Behavior Immun 2020; S0889-1591:30643–7. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 3. Zhai Y, Du X.. Loss and grief amidst COVID-19: a path to adaptation and resilience. Brain Behavior Immun 2020; S0889-1591:30632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Duan L, Zhu G.. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 2020; 7:300–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Maunder R, Hunter J, Vicent L, Bennett J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003; 168:1245–51. [PMC free article] [PubMed] [Google Scholar]
- 6. Barbisch D, Koenig KL, Shih FY.. Is there a case for quarantine? Perspectives from to Ebola. Disaster Med Public Health Prep 2015; 9:547–53. [DOI] [PubMed] [Google Scholar]
- 7. Rubin GJ, Wessely S.. Coronavirus: the psychological effects of quarantining a city. BMJ Opinion 2020; 368:m313. [DOI] [PubMed] [Google Scholar]
- 8. Sa L. How much “Thinking” about COVID-19 is clinically dysfunctional? Brain Behavior Immun 2020; S0889-1591:30682–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. https://covid19.who.int/ (18 May 2020, date last accessed).
- 10. Bai Y, Lin C-C, Lin C-Y, Chen J-Y, Chue C-M, Chou P.. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv 2004; 55:1055–7. [DOI] [PubMed] [Google Scholar]
- 11. Liu X, Kakade M, Fuller CJ, Fan B, Fang Y, Kong J, et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry 2012; 53:15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sprang G, Silman M.. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep 2013; 7:105–10. [DOI] [PubMed] [Google Scholar]
- 13. Taylor MR, Agho KE, Stevens GJ, Raphael B.. Factors influencing psychological distress during a disease epidemic: data from Australia’s first outbreak of equine influenza. BMC Public Health 2008; 8:347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry 2009; 54:302–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, Styra R.. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect 2008; 136:997–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wu P, Liu X, Fang Y, Fan B, Fuller CJ, Guan Z, et al. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol Alcohol 2008; 43:706–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mihashi M, Otsubo Y, Yinjuan X, Nagatomi K, Hoshiko M, Ishitake T.. Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychol 2009; 28:91–100. [DOI] [PubMed] [Google Scholar]
- 18. Yoon MK, Kim SY, Ko HS, Lee MS.. System effectiveness of detection, brief intervention and refer to treatment for the people with post-traumatic emotional distress by MERS: a case report of community-based proactive intervention in South Korea. Int J Ment Health Syst 2016; 10:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R.. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis 2004; 10:1206–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. DiGiovanni C, Conley J, Chiu D, Zaborski J.. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur Bioterror 2004; 2:265–72. [DOI] [PubMed] [Google Scholar]
- 21. Lee S, Chan LY, Chau AM, Kwok KP, Kleinman A.. The experience of SARS-related stigma at Amoy Gardens. Soc Sci Med 2005; 61:2038–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Marjanovic Z, Greenglass ER, Coffey S.. The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: an online questionnaire survey. Int J Nurs Stud 2007; 44:991–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cava MA, Fay KE, Beanlands HJ, McCay EA, Wignall R.. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs 2005; 22:398–406. [DOI] [PubMed] [Google Scholar]
- 24. Wang J, Wang JX, Yang GS.. The Psychological Impact of COVID-19 on Chinese Individuals. Yonsei Med J 2020; 61:438–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Khan S, Siddique R, Li H, Ali A, Shereen MA, Bashir N, et al. Impact of coronavirus outbreak on psychological health. J Glob Health 2020; 10:010331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A.. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry 2020; 66:317–320. [DOI] [PubMed] [Google Scholar]
- 27. Jeong H, Yim HW, Song Y-J, Ki M, Min JA, Cho J, et al. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health 2016; 38:e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Desclaux A, Badji D, Ndione AG, Sow K.. Accepted monitoring or endured quarantine? Ebola contacts’ perceptions in Senegal. Soc Sci Med 2017; 178:38–45. [DOI] [PubMed] [Google Scholar]
- 29. Braunack-Mayer A, Tooher R, Collins JE, Street JM, Marshall H.. Understanding the school community’s response to school closures during the H1N1 2009 influenza pandemic. BMC Public Health 2013; 13:344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lee M, You M.. Psychological and behavioral responses in South Korea during the early stages of coronavirus disease 2019 (COVID-19). Int J Environ Res Public Health 2020; 17:2977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pompili M, Innamorati M, Lamis DA, Erbuto D, Venturini P, Ricci F, et al. The associations among childhood maltreatment, “male depression” and suicide risk in psychiatric patients. Psychiatry Res 2014; 220:571–578. [DOI] [PubMed] [Google Scholar]
- 32. Engel-Yeger B, Muzio C, Rinosi G, Solano P, Geoffroy PA, Pompili M, et al. Extreme sensory processing patterns and their relation with clinical conditions among individuals with major affective disorders. Psychiatry Res 2016; 236:112–8. [DOI] [PubMed] [Google Scholar]
- 33. Orsolini L, Latini R, Pompili M, Serafini G, Volpe U, Vellante F, et al. Understanding the complex of suicide in depression: from research to clinics. Psychiatry Investig 2020; 17:207–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stickley A, Koyanagi A.. Loneliness, common mental disorders and suicidal behavior: findings from a general population survey. J Affect Disord 2016; 197:81–7. [DOI] [PubMed] [Google Scholar]
- 35. De Berardis D, Fornaro M, Valchera A, Rapini G, Di Natale S, De Lauretis I, et al. Alexithymia, resilience, somatic sensations and their relationships with suicide ideation in drug naïve patients with first-episode major depression: an exploratory study in the “real world” everyday clinical practice. Early Interv Psychiatry 2020; 14:336–42. [DOI] [PubMed] [Google Scholar]
- 36. De Berardis D, Vellante F, Fornaro M, Anastasia A, Olivieri L, Rapini G, et al. Alexithymia, suicide ideation, affective temperaments and homocysteine levels in drug naïve patients with post-traumatic stress disorder: an exploratory study in the everyday ‘real world’ clinical practice. Int J Psychiatry Clin Pract 2020; 24:83–7. [DOI] [PubMed] [Google Scholar]
- 37. De Berardis D, Fornaro M, Orsolini L, Valchera A, Carano A, Vellante F, et al. Alexithymia and suicide risk in psychiatric disorders: a mini-review. Front Psychiatry 2017; 8:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Amerio A, Bianchi D, Santi F, Costantini L, Odone A, Signorelli C, et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Biomed 2020; 91:83–8. [DOI] [PMC free article] [PubMed] [Google Scholar]