Abstract
Introduction
Chronic lower back pain is a leading cause of disability in US adults. Opioid use continues to be controversial despite the Centers for Disease Control and Prevention guidance on chronic pain management to use nonpharmacologic and nonopioid pharmacologic interventions. The objectives of the study were to assess the impact of early physical therapy (PT) intervention on improving functionality and reducing opioid burden in patients with chronic lower back pain.
Methods
A single-center, retrospective chart review of patients receiving ≥6 PT visits and treated with either opioids first (OF) or PT first (PTF) therapy for chronic lower back pain were evaluated. Concomitant use of nonopioid and nonpharmacologic therapy was permitted. The Oswestry Disability Index (ODI), a survey measuring functionality, was recorded for PTF group. Pain scores and medication use including opioids were collected at treatment initiation and completion.
Results
One hundred and eighty patients were included in three groups: OF group (n = 60), PTF group (n = 60), and PTF + ODI group (n = 60). The PTF + ODI group had mean ODI reduction of 11.9% (P < .001). More OF patients were lost to follow up (68.3%) or failed PT (60%) compared to the PTF group, 38.3% and 3.3% (P < .001). Reduction in both opioid and nonopioid medications as well as pain scores were observed but not statistically significant.
Discussion
Early PT resulted in improved functionality, decreased pain, and reduced medication use upon PT completion. These findings suggest PT, along with nonopioid modalities, are a viable first-line option for the management of chronic lower back pain.
Keywords: physical therapy, chronic lower back pain, lower back pain, pain, opioids, Oswestry Disability Index
Introduction
About 10% to 20% of individuals with acute lower back pain will develop chronic lower back pain (CLBP). Chronic lower back pain was defined using National Institute of Neurological Disorders and Stroke1 definition of pain and disability persisting for more than 3 months. In the United States, CLBP is the third leading disease contributing to disability adjusted life years with a mean increase of 24% from 1990 to 2010.1-4 Lost work days from CLBP is approximately 149 million days per year accruing costs upwards of $100 billion to $200 billion annually.5 Chronic lower back pain is often managed by opioids but use as first-line therapy remains controversial. Not only are opioids associated with tolerance and risk of addiction, patients with CLBP have reduced progress in regaining functionality.6 Kidner et al6 found the work-return rate for very high opioid users (>120 mg/d of morphine equivalents) versus nonopioid users was 76% and 94%, respectively. Compared to other specialties, family practice, general practice, and internal medicine opioid prescription use per capita increased by 7.35% between 2007 to 2012.5,7 Despite recent improved prescribing habits, the repercussions in disability and patient harm are still evident as patients continue to struggle with addiction, substance use, chronic pain, and psychiatric comorbidities.8-10
In 2016, the Centers for Disease Control and Prevention (CDC)5 published guidelines to improve opioid prescribing habits and reduce opioid harm in individuals using opioids chronically. The CDC recommends using pharmacologic and nonpharmacologic strategies. The guidelines5 encourage caution when prescribing opioids by using the lowest effective dose, using immediate release formulations, developing treatment goals, and discussing risks as well as benefits with the patient. Furthermore, CLBP studies have shown exercise reduces pain and improves functionality but no specific type of exercise or therapy were recommended.11-16 Lastly, Gomes et al8 and Dunn et al9 showed opioid use for chronic pain was associated with increased overdose rates in patients using higher doses. A 2.5-fold higher risk of overdose (hazard ratio 2.33, confidence interval [CI] 1.26-4.32) was found when long-acting opioids were used compared to the immediate-release formulations.10 With significant dangers associated with opioid use, additional studies in CLBP to evaluate the benefit of specific nonpharmacologic interventions such as physical therapy (PT) and impact on medication use for pain management are needed. Benefits of improved functionality and decreased opioid use may theoretically provide improved outcomes in treatment of neurologic and psychiatric comorbidities. This study's objective was to assess the impact of early PT intervention on improving functionality and opioid burden reduction in patients with CLBP.
Methods
This study, approved by the Scripps Institutional Review Board, was a single-institution, retrospective chart review conducted at Family Health Centers of San Diego (FHCSD), Department of Physical Therapy in collaboration with Scripps Mercy Hospital San Diego, Department of Pharmacy using FHCSD electronic health records between January 1, 2014 and August 14, 2018. This study was originally designed to evaluate reduction in opioid burden with early PT confirmed by temporal relationship when opiate(s) were used prior or after PT initiation. The opioids first (OF) group was identified by patients using opioids prior to PT initiation, and the PT first (PTF) group, referred to as early PT, were patients not using opioids at PT initiation. When the Oswestry Disability Index (ODI) survey for monitoring functional improvement began at FHCSD PT Department in September 2017, an additional group of PTF patients was added to evaluate functionality improvements with early PT without prior opioid use and redefined functionality based on ODI as the new primary objective.17
Patients were included if they were 18 years or older, completed ≥6 PT visits, diagnosed with CLBP for ≥3 months, and used either opioids or PT as first-line therapy at the beginning of the study. Concomitant, nonopioid pharmacologic and nonpharmacologic therapy was allowed. Patients were excluded if they concomitantly used opioids and physical therapy at the beginning of the study.
Variables collected included demographics, comorbidities (eg depression, musculoskeletal disorders, history of falls), and opioid use based on the statewide prescription drug monitoring program. Medications used were recorded at the initial PT evaluation and post PT treatment. Using the 1 to 10 numeric pain rating scale, pain scores at the initial PT evaluation and the last PT office visit were collected. Patient functionality was also collected at the initial PT evaluation and at the last PT visit using a validated, self-administered survey known as the ODI survey. This survey evaluates the patient's level of disability and assigns them to 1 of the 5 following categories: 0% to 20% minimal, 21% to 40% moderate, 41% to 60% severe, 61% to 80% crippled, and 81% to 100% immobile.17 Changes in ODI scores greater than 10% are considered clinically significant.17
The primary study outcome was functionality measured by a reduction in ODI scores among CLBP patients only using PT first. The secondary study outcomes compared CLBP patients using either PT first versus opioid treatment first. These outcomes were reduction in opioid burden, as evidence by decreased opioid and nonopioid medication use post-PT treatment, reduction in objective pain scores post-PT, number of patients failing PT and continuing or initiating opioids during study, and number of patients lost to follow up.
Descriptive statistics evaluated demographics and baseline characteristics. Wilcoxon signed rank reported a change in ODI. Continuous variables were expressed as a mean ± SD. Categorical variables were analyzed using Fisher's exact test. A P value <.05 was considered statistically significant for all outcomes, and a power level of 0.9 was calculated to detect a 1-point difference in the primary outcome for sample size. A multivariable logistic regression was used to determine associations between baseline medication use and change in functionality. Corresponding 95% CI was calculated using a significance level of 5% for logistic regression. Statistical analysis was performed using IBM SPSS®, version 23 (Armonk, NY).
Results
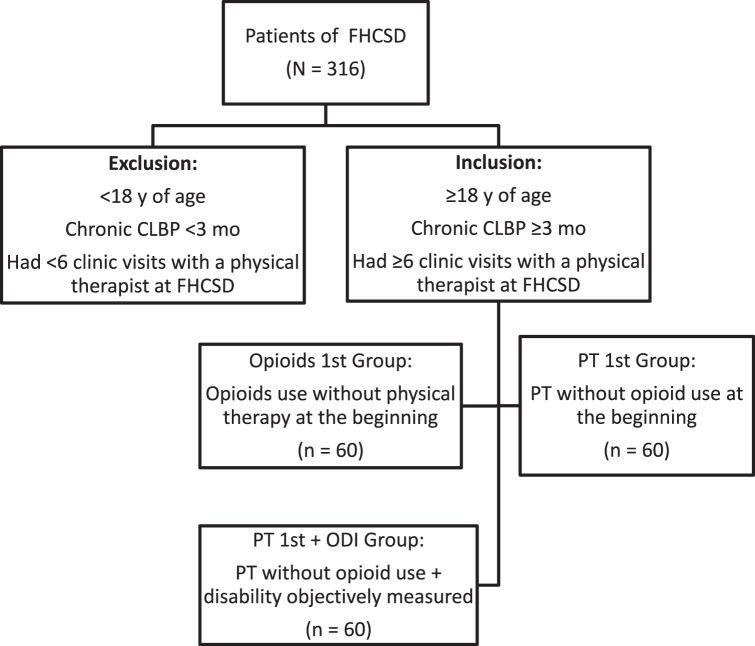
Of the 316 eligible patients, 180 (57%) met inclusion criteria (Figure). A total of 60 patients (33.3%) used opioids as a first-line therapy, 60 (33.3%) used PT as a first-line therapy, and 60 (33.3%) used PT first-line and reported ODI scores. The FHSCD Department of PT began using ODI for functionality in September 2017 and, therefore, only 60 of the 120 PTF group had documented ODI scores. In this study, most patients with CLBP included were female, who were predominately Hispanic followed by white (non-Hispanic) then black. More patients in the OF group compared to both PTF groups had a history of depression 53% versus 30.8% (P = .11), substance use disorder 30% versus 20% (P < .001), a fall within the past year 45% versus 15.8% (P < .001), and on average had more falls 1.1 ± 1.6 versus 0.3 ± 0.6 (P < .001; Table 1).
FIGURE.
Patient selection of the chronic lower back pain (CLBP) study conducted at Family Health Centers of San Diego (FHCSD; ODI = Oswestry Disability Index; PT = physical therapy)
TABLE 1.
Patient demographics of the presented studya
|
Patient Characteristic |
OF Group (n = 60) |
PTF Group (n = 60) |
PTF + ODI (n = 60) |
P
Valueb |
| Average age, mean ± SD | 53.4 ± 12.2 | 46.1 ± 14.9 | 43.3 ± 14.1 | .0041 |
| Sex | ||||
| Female, No. | 41 | 34 | 38 | .419 |
| Race | ||||
| White (non-Hispanic) | 15 (25) | 13 (22) | 17 (28) | NS |
| Hispanic | 20 (33) | 31 (52) | 28 (47) | NS |
| Asian | 3 (5) | 3 (5) | 2 (3) | NS |
| Black | 16 (27) | 11 (18) | 10 (17) | NS |
| Other | 6 (10) | 2 (3) | 3 (5) | NS |
| Depression | 32 (53) | 17 (28) | 20 (33) | .11 |
| Anxiety | 15 (25) | 7 (12) | 14 (23) | .131 |
| Substance use disorder history | 18 (30) | 20 (33) | 4 (7) | <.001 |
| Other mental health disorders | 18 (30) | 10 (17) | 11 (18) | .157 |
| History of falls | 27 (45) | 8 (13) | 11 (18) | <.001 |
| Average No. of falls, mean ± SDc | 1.1 ± 1.6 | 0.2 ± 0.5 | 0.3 ± 0.6 | <.001 |
| Musculoskeletal disorders | 46 (77) | 37 (62) | 13 (22) | <.001 |
NS = not significant; ODI = Oswestry Disability Index; OF = opioids first group; PTF = physical therapy first group.
Unless otherwise noted, data presented in No. (%) format.
P values for demographics compares OF group to total of PTF and PTF + ODI group.
Falls averaged over total number of falls for the specified group.
The PTF group showed improved functionality with a mean ODI decrease of 11.9% (P < .001), with 61.7% having an ODI reduction greater than 10% (Table 2). Subjective pain scores decreased similarly among all groups and were not statistically different between groups (Table 2). A higher portion of patients in the OF group were lost to follow up (68.3%) compared with the PTF group (38.3%; P = .026). Only 3.3% of patients in the PTF group failed PT and required opioids versus 60% of patients in the OF group, who failed PT and continued to require opioids (P < .001; Table 2). Both opioid and nonopioid medications decreased among each group (Table 2). The most common opioids used at baseline were hydrocodone-acetaminophen (n = 34) followed by tramadol (n = 37; Table 2). The most common nonopioid medications used at baseline were nonsteroidal anti-inflammatory drugs (NSAIDs; n = 115), acetaminophen (n = 67), and muscle relaxants (n = 59). Total number of opioids used in the OF group decreased by 48.3%, while nonopioid medication use decreased by 29.9% in the OF group and 42.8% in the PTF group (Table 2). Gabapentin was used by more OF patients at baseline (n = 24 vs n = 9, P < .001) and was the only non-opioid medication that showed increased use between both groups at PT completion. Multivariable logistic regression showed baseline NSAIDs (P = .004; CI 2.3-94.6; odds ratio 14.8) and acetaminophen use (P = .005; CI 2.1-64.8; odds ratio 11.72) was associated with a greater than 10% change in ODI when controlled for chest pain, sex, and initial ODI score.
TABLE 2.
Details of the study outcomesa
|
Primary Outcome |
PTF + ODI |
|||||
| Functionality Scores |
Pre-PT |
Post-PT |
P
Value |
|||
| Mean ± SD Oswestry score, % | 39.8 ± 19.8 | 27.9 ± 26.3 | <.001 | |||
| >10% change in Oswestry score, No. (%)b | 37 (61.7) | … | … | |||
|
Secondary Outcomes |
OF |
PTF |
PTF + ODI |
P
Valuec |
||
| Pain scores, mean ± SDd | ||||||
| Pre-PT pain score | 9.2 ± 1.0 | 8.5 ± 1.0 | 5.41 ± 2.1 | NS | ||
| Post-PT pain score | 4.7 ± 2.9 | 3.7 ± 1.0 | 2 ± 2.5 | NS | ||
| PT completion, n | ||||||
| Failed PT and used opioids | 36 | 3 | 1 | .0001 | ||
| Lost to follow up with PT | 41 | 28 | 18 | .026 | ||
|
OF |
PTF |
PTF + ODI |
||||
|
Medication Usage, No. (%) |
Pre-PT |
Post-PT |
Pre-PT |
Post-PT |
Pre-PT |
Post-PT |
| Total opioids | 91 (100) | 47 (100) | … | 3 (100) | … | 1 (100) |
| Morphine | 2 (2.2) | 2 (4.3) | … | 1 (33.3) | … | 0 |
| Codeine | 8 (8.8) | 0 | … | 0 | … | 0 |
| Oxycodone | 8 (8.8) | 9 (19.1) | … | 1 (33.3) | … | 1 (100) |
| Hydrocodone | 34 (37.4) | 16 (34) | … | 0 | … | 0 |
| Buprenorphine | 2 (2.2) | 0 | … | 0 | … | 0 |
| Tramadol | 37 (40.6) | 20 (42.6) | … | 1 (33.3) | … | 0 |
| Total nonopioids | 127 (100) | 93 (100) | 85 (100) | 36 (100) | 67 (100) | 54 (100) |
| NSAIDs | 50 (39.4) | 33 (35.5) | 43 (50.6) | 10 (27.8) | 22 (32.8) | 22 (40.7) |
| Acetaminophen | 25 (19.7) | 13 (13.9) | 22 (25.9) | 6 (16.7) | 20 (29.9) | 16 (29.6) |
| Muscle relaxant | 23 (18.1) | 18 (19.4) | 14 (16.4) | 8 (22.2) | 22 (32.8) | 10 (18.5) |
| Gabapentin | 24 (18.9) | 25 (26.9) | 6 (7.1) | 10 (27.8) | 3 (4.5) | 5 (9.3) |
| Unspecified | 5 (3.9) | 4 (4.3) | 0 | 2 (5.5) | 0 | 1 (1.9) |
NS = not significant; NSAIDs = nonsteroidal anti-inflammatory drugs; ODI = Oswestry Disability Index; OF = opioids first group; PT = physical therapy; PTF = physical therapy first group.
N = 60 for the following groups: PTF + ODI, OF, PTF, and PTF + ODI.
P value for mean Oswestry score compares only PTF + ODI group prior to and after PT completion. A greater than 10% change in ODI indicates a significant difference within 90% confidence interval.
P values for PT completion outcomes compares OF group to total of PTF and PTF + ODI group.
Pain score based on numeric scale from 1 to 10. Pain scores compared between all 3 groups without significance.
Discussion
To our knowledge, this is the first assessment of early PT intervention for pain, functionality, and opioid use in the management of CLBP. Our results suggest early PT significantly improves functionality of patients with CLBP. Functional improvements included areas assessed in the ODI: pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling. Improvements in these areas are also areas targeted in improving various psychiatric comorbidities such as depression. Results showed early PT in CLBP provided similar reductions in pain compared to patients using opioids with PT. These findings are consistent with one large, systematic review16 showing no benefit in chronic pain control between opioids versus alternative nonopioid medications. Krebs et al18 demonstrated similar reduction in pain between opioids and nonopioid medications, but nonopioids provided sustained reductions in pain relief as opposed to opioids. These results also support CDC recommendations to use nonpharmacologic and nonopioid medications as first-line treatments for chronic pain. Although no significant difference between groups emerged in pain reduction, the positive trend suggests PT with nonopioids provided comparable pain relief to PT with opioids.
Fritz et al19 found an increased risk of long-term opioid use with primary care versus physical therapy visits following a new consultation for lower back pain. Although infrequently used, PT incorporates nonpharmacologic pain management strategies including exercises, spinal manipulation, and education to improve CLBP.19-21 Several studies19,22,23 suggest early use of PT are associated with lower CLBP-related costs and reduced use of MRI, spinal injections, and opioid use. While this study did not focuse on the CLBP-related costs and use of other services, PT did reduce the use of nonopioid and opioid medications. Interestingly, most patients in the OF group who failed PT and continued opioid medications still received a benefit in pain reduction and decreased number of medications used for pain relief. Therefore, patients currently using opioids for CLBP may still benefit from PT. Increasing PT referral and use may improve pain and function in CLBP in addition to mitigating opioid use to reduce overdose potential.19,22,24,25
Our study also highlighted patients in the opioid group had more comorbidities compared with PT group including depression and patient falls. Depression is a common comorbidity in patients with CLBP, which is associated with higher opioid use and rates of substance use disorder.19,26-30 Studies have shown individuals with CLBP and psychological conditions do not respond to opioid treatment and have an increased risk of long-term use or misuse.19,31 Our results suggest that patients with CLBP complicated by depression are more likely to be prescribed opioids and have a higher risk for substance use. It should be noted that depression rates with this group may have led to high failure rates and increased loss to follow up compared to PTF group.
Lastly, falls are also a common health concern contributing to patient morbidity and mortality in CLBP and opioid use, especially in elderly (>65 years of age) who have a 4 to 5 times higher likelihood of falling while taking opioids versus NSAIDs.32 In our study, a significantly higher number of falls in patients taking opioids was seen, which emphasizes the need for more cautious prescribing in patients with CLBP as they are already limited in their mobility due to pain. The decision to prescribe opioids in elderly with CLBP should be avoided if possible.
We acknowledge the limitations of this study as it was a retrospective, single-center study with a majority female population and may not be generalizable to all CLBP populations. In contrast, retrospective design may be reflective of clinical practice and prescribing patterns of primary care setting in patients with CLBP. Additionally, baseline characteristics in the OF group included older patients with more musculoskeletal disorders, falls, and mental health disorders representing a sicker group, which may be prone to worse outcomes. Medication usage was based on availability of information provided by the electronic medical record, which limited our ability to determine when medications were initiated or discontinued as well as quantities and doses prescribed outside of FHCSD. Moreover, we were unable to assess the use of illicit substances, nonprescription opioids, or additional nonpharmacologic treatments. Groups were not matched and, thus, may include additional unidentified confounders. Overall, the population size is small, and additional patients would add to the robustness of these results. It should be noted that ODI is a patient-assessed survey and may exhibit response bias based on patient willingness to report accurately. Only the total ODI score was available, and assessment of the individual components from the survey were not possible. The ODI scale was also implemented in September 2017, leading to the low number of patients included in this group as well as this scale is not used in the OF group. Lastly, numeric pain scores were not consistently monitored for trends among patients in all groups.
Conclusion
Initial CLBP treatment with early PT leads to a significant improvement in functionality, reduced pain scores, and reduced medication burden for both treatment groups. The OF treatment revealed no difference in pain reduction compared to PT first, but this outcome was not evaluated in functional improvement. Although PT improves functionality, it is uncertain if PT is functionally beneficial compared to opioids as this was not compared. These findings suggest that PT interventions should be considered a first-line, nonpharmacologic treatment option for CLBP along with nonopioid pharmacologic agents. Multiple risks and limited efficacy restrict our ability to recommend opioids as a safe, initial treatment option for CLBP.
References
- 1.Bethesda (MD): National Institute of Neurological Disorders and Stroke; Low back pain fact sheet. [Internet] [updated 2020 Apr 27; cited 2017 Sept 10] Available from: https://www https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Low-Back-Pain-Fact-Sheet. [Google Scholar]
- 2.Maher CG. Effective physical treatment for chronic low back pain. Orthop Clin North Am. 2004;35(1):57–64. doi: 10.1016/S0030-5898(03)00088-9. DOI: 10.1016/S0030-5898(03)00088-9 PubMed PMID: 15062718. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. doi: 10.1001/jama.2013.13805. DOI: 10.1001/jama.2013.13805 PubMed PMID: 23842577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–8. doi: 10.1001/archinternmed.2008.543. DOI: 10.1001/archinternmed.2008.543 PubMed PMID: 19204216 PubMed Central PMCID: PMC4339077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain — United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. doi: 10.15585/mmwr.rr6501e1. DOI: 10.15585/mmwr.rr6501e1 PubMed PMID: 26987082. [DOI] [PubMed] [Google Scholar]
- 6.Kidner CL, Mayer TG, Gatchel RJ. Higher opioid doses predict poorer functional outcome in patients with chronic disabling occupational musculoskeletal disorders. J Bone Joint Surg Am. 2009;91(4):919–27. doi: 10.2106/JBJS.H.00286. DOI: 10.2106/JBJS.H.00286 PubMed PMID: 19339577 PubMed Central PMCID: PMC2665041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levy B, Paulozzi L, Mack KA, Jones CM. Trends in opioid analgesic–prescribing rates by specialty, U.S., 2007–2012. Am J Prev Med. 2015;49(3):409–13. doi: 10.1016/j.amepre.2015.02.020. DOI: 10.1016/j.amepre.2015.02.020 PubMed PMID: 25896191 PubMed Central PMCID: PMC6034509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171(7):686–91. doi: 10.1001/archinternmed.2011.117. DOI: 10.1001/archinternmed.2011.117 PubMed PMID: 21482846. [DOI] [PubMed] [Google Scholar]
- 9.Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. doi: 10.1059/0003-4819-152-2-201001190-00006. DOI: 10.7326/0003-4819-152-2-201001190-00006 PubMed PMID: 20083827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller M, Barber CW, Leatherman S, Fonda J, Hermos JA, Cho K, et al. Prescription opioid duration of action and the risk of unintentional overdose among patients receiving opioid therapy. JAMA Intern Med. 2015;175(4):608–15. doi: 10.1001/jamainternmed.2014.8071. DOI: 10.1001/jamainternmed.2014.8071 PubMed PMID: 25686208. [DOI] [PubMed] [Google Scholar]
- 11.Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians Clinical Practice Guideline. Ann Intern Med. 2007;147(7):492–504. doi: 10.7326/0003-4819-147-7-200710020-00007. DOI: 10.7326/0003-4819-147-7-200710020-00007 PubMed PMID: 17909210. [DOI] [PubMed] [Google Scholar]
- 12.Maher CG. Effective physical treatment for chronic low back pain. Orthop Clin North Am. 2004;35(1):57–64. doi: 10.1016/S0030-5898(03)00088-9. DOI: 10.1016/S0030-5898(03)00088-9 PubMed PMID: 15062718. [DOI] [PubMed] [Google Scholar]
- 13.O'Connell NE, Cook CE, Wand BM, Ward SP. Clinical guidelines for low back pain: a critical review of consensus and inconsistencies across three major guidelines. Best Pract Res Clin Rheumatol. 2016;30(6):968–80. doi: 10.1016/j.berh.2017.05.001. DOI: 10.1016/j.berh.2017.05.001 PubMed PMID: 29103554. [DOI] [PubMed] [Google Scholar]
- 14.Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–30. doi: 10.7326/M16-2367. DOI: 10.7326/M16-2367 PubMed PMID: 28192789. [DOI] [PubMed] [Google Scholar]
- 15.van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes BW, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J. 2011;20(1):19–39. doi: 10.1007/s00586-010-1518-3. DOI: 10.1007/s00586-010-1518-3 PubMed PMID: 20640863 PubMed Central PMCID: PMC3036018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain. A systematic review of randomized controlled trials of the most common interventions. Spine (Phila Pa 1976) 1997;22(18):2128–56. doi: 10.1097/00007632-199709150-00012. DOI: 10.1097/00007632-199709150-00012 PubMed PMID: 9322325. [DOI] [PubMed] [Google Scholar]
- 17.Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–3. PubMed PMID: 6450426. [PubMed] [Google Scholar]
- 18.Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain. JAMA. 2018;319(9):872–82. doi: 10.1001/jama.2018.0899. DOI: 10.1001/jama.2018.0899 PubMed PMID: 29509867 PubMed Central PMCID: PMC5885909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fritz JM, King JB, McAdams-Marx C. Associations between early care decisions and the risk for long-term opioid use for patients with low back pain with a new physician consultation and initiation of opioid therapy. Clin J Pain. 2018;34(6):552–8. doi: 10.1097/AJP.0000000000000571. DOI: 10.1097/AJP.0000000000000571 PubMed PMID: 29135698. [DOI] [PubMed] [Google Scholar]
- 20.Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer R, et al. Noninvasive treatments for low back pain. Rockville (MD): Agency for Healthcare Research and Quality (US);; 2016. [PubMed] [Google Scholar]
- 21.Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017;166(7):493–505. doi: 10.7326/M16-2459. DOI: 10.7326/M16-2459 PubMed PMID: 28192793. [DOI] [PubMed] [Google Scholar]
- 22.Jeffrey Kao M-C, Minh LC, Huang GY, Mitra R, Smuck M. Trends in ambulatory physician opioid prescription in the United States, 1997-2009. PM R. 2014;6(7):575–82.e4. doi: 10.1016/j.pmrj.2013.12.015. DOI: 10.1016/j.pmrj.2013.12.015 PubMed PMID: 24412267. [DOI] [PubMed] [Google Scholar]
- 23.Fritz JM, Childs JD, Wainner RS, Flynn TW. Primary care referral of patients with low back pain to physical therapy. Spine (Phila Pa 1976) 2012;37(25):2114–21. doi: 10.1097/BRS.0b013e31825d32f5. DOI: 10.1097/BRS.0b013e31825d32f5 PubMed PMID: 22614792. [DOI] [PubMed] [Google Scholar]
- 24.Ballentyne JC. Avoiding opioid analgesics for treatment of chronic low back pain. JAMA Intern Med. 2016;315(22):2459–60. doi: 10.1001/jama.2016.6753. DOI: 10.1001/jama.2016.6753 PubMed PMID: 27299620. [DOI] [PubMed] [Google Scholar]
- 25.Fritz JM, Kim J, Thackeray A, Dorius J. Use of physical therapy for low back pain by medicaid enrollees. Phys Ther. 2015;95(12):1668–79. doi: 10.2522/ptj.20150037. DOI: 10.2522/ptj.20150037 PubMed PMID: 26316532. [DOI] [PubMed] [Google Scholar]
- 26.Deyo RA, Smith DHM, Johnson ES, Donovan M, Tillotson CJ, Yang X, et al. Opioids for back pain patients: primary care prescribing patterns and use of services. J Am Board Fam Med. 2011;24(6):717–27. doi: 10.3122/jabfm.2011.06.100232. DOI: 10.3122/jabfm.2011.06.100232 PubMed PMID: 22086815 PubMed Central PMCID: PMC3855548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seal KH, Shi Y, Cohen G, Cohen BE, Maguen S, Krebs EE, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307(9):940–7. doi: 10.1001/jama.2012.234. DOI: 10.1001/jama.2012.234 PubMed PMID: 22396516. [DOI] [PubMed] [Google Scholar]
- 28.Zheng P, Kao M-C, Karayannis NV, Smuck M. Stagnant physical therapy referral rates alongside rising opioid prescription rates in patients with low back pain in the United States 1997–2010. Spine (Phila Pa 1976) 2017;42(9):670–4. doi: 10.1097/BRS.0000000000001875. DOI: 10.1097/BRS.0000000000001875 PubMed PMID: 28441685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Braden JB, Sullivan MD, Ray GT, Saunders K, Merrill J, Silverberg MJ, et al. Trends in long-term opioid therapy for noncancer pain among persons with a history of depression. Gen Hosp Psychiatry. 2009;31(6):564–70. doi: 10.1016/j.genhosppsych.2009.07.003. DOI: 10.1016/j.genhosppsych.2009.07.003 PubMed PMID: 19892215 PubMed Central PMCID: PMC2774904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kobus AM, Smith DH, Morasco BJ, Johnson ES, Yang X, Petrik AF, et al. Correlates of higher-dose opioid medication use for low back pain in primary care. J Pain. 2012;13(11):1131–8. doi: 10.1016/j.jpain.2012.09.003. DOI: 10.1016/j.jpain.2012.09.003 PubMed PMID: 23117108 PubMed Central PMCID: PMC3641146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wasan AD, Michna E, Edwards RR, Katz JN, Nedeljkovic SS, Dolman AJ, et al. Psychiatric comorbidity is associated prospectively with diminished opioid analgesia and increased opioid misuse in patients with chronic low back pain. Anesthesiology. 2015;123(4):861–72. doi: 10.1097/ALN.0000000000000768. DOI: 10.1097/ALN.0000000000000768 PubMed PMID: 26375824 PubMed Central PMCID: PMC4573512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krebs EE, Paudel M, Taylor BC, Bauer DC, Fink HA, Lane NE, et al. Association of opioids with falls, fractures, and physical performance among older men with persistent musculoskeletal pain. J Gen Intern Med. 2016;31(5):463–9. doi: 10.1007/s11606-015-3579-9. DOI: 10.1007/s11606-015-3579-9 PubMed PMID: 26754689 PubMed Central PMCID: PMC4835377. [DOI] [PMC free article] [PubMed] [Google Scholar]