Abstract
The majority of patients with chronic kidney disease (CKD) have elevated blood pressure (BP). In patients with CKD, hypertension is associated with increased risk for cardiovascular disease, progression of CKD, and all-cause mortality. New guidelines from the American College of Cardiology/American Heart Association (ACC/AHA) recommend new thresholds and targets for the diagnosis and treatment of hypertension in patients with and without CKD. A new aspect of the guidelines is the recommendation for measurement of out-of-office BP to confirm the diagnosis of hypertension and guide therapy. In this KDOQI (Kidney Disease Outcomes Quality Initiative) perspective, we review the recommendations for accurate BP measurement in the office, at home, and with ambulatory BP monitoring. Regardless of location, validated devices and appropriate cuff sizes should be used. In the clinic and at home, proper patient preparation and positioning are critical. Patients should receive information about the importance of BP measurement techniques and be encouraged to advocate for adherence to guideline recommendations. Implementing appropriate BP measurement in routine practice is feasible and should be incorporated in system-wide efforts to improve the care of patients with hypertension. Hypertension is the number 1 chronic disease risk factor in the world; BP measurements in the office, at home, and with ambulatory BP monitoring should adhere to recommendations from the AHA.
Introduction
The number of US adults with hypertension is now more than 100 million according to the new guidelines from the American College of Cardiology/American Heart Association (ACC/AHA).1 Of these individuals, more than 80 million qualify for treatment with antihypertensive medications.1 Hypertension is an especially important comorbid condition in patients with chronic kidney disease (CKD); 86% of participants in the Chronic Renal Insufficiency Cohort (CRIC) Study had hypertension at baseline.2 A key component for quality of care in adults with hypertension is measurement of blood pressure (BP).
In this KDOQI (Kidney Disease Outcomes Quality Initiative) perspective, we summarize recommendations for proper clinic/office, home, and ambulatory BP measurements and highlight areas that are especially pertinent in patients with CKD. A separate KDOQI commentary discussed the relevance of the 2017 ACC/AHA guidelines for management of BP in patients with CKD.3
Critical Aspects of BP Measurement Technique Office BP
Introduction of cuff-based sphygmomanometry by Riva-Rocci4 in 1896 provided the first practical method for estimation of systolic BP. Diastolic BP readings became feasible in 1905 when Korotkov5 described his auscultatory measurement method. These methods were disseminated rapidly and by 1918, all US insurance companies considered measurement of BP to be an essential part of their eligibility examination.6 The fact that BP varies dramatically from one reading to another was recognized and as early as 1904, Janeway7 focused attention on standardizing BP measurement methods to avoid errors in estimation. However, as is still the case, there was much variation in technique and minimal attention to quality control.8 By the mid-1960s, the relative importance of systematic errors such as digit preference demonstrated by a higher-than-expected proportion of patients with a given systolic BP (eg, 110, 120, and 138 mm Hg; Fig 1) and random (unpredictable) errors in BP measurement had been quantified.9,10 Based on this, BP guideline committees, professional societies, and government agencies repeatedly recommended specific approaches to improve the accuracy of measuring BP. This advice has been largely ignored by the practice community. A recent meta-analysis documents an average systolic BP in routine clinical practice close to 15 mm Hg higher than in research studies.11 However, in many of the studies, the order of routine and research BP measurements was not randomized and they were not obtained during the same visit.12,13 Landmark BP risk and treatment studies have devoted considerable attention to the accuracy of BP measurement. To take full advantage of these reports, accurate BP measurements should be an essential part of clinical practice.
Figure 1.
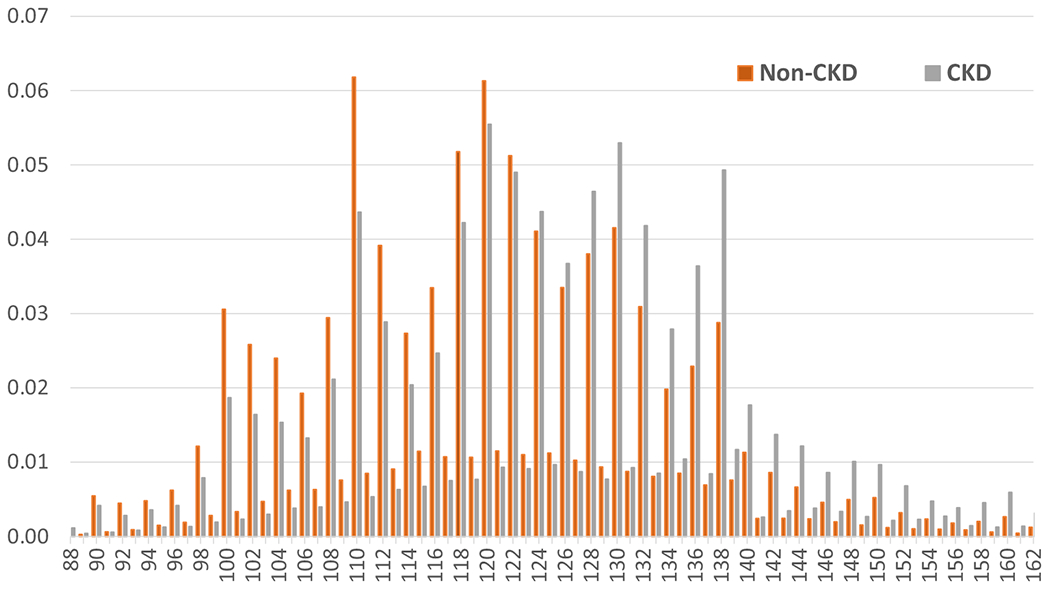
Proportion of systolic blood pressure readings from primary care visits by chronic kidney disease (CKD) status.
Detailed guidance for BP measurement has been provided in the 2017 ACC/AHA BP guideline, the 2018 European Society of Cardiology/European Society of Hypertension (ESH) guidelines, a 2019 National Heart, Lung, and Blood Institute Working Group report, and a 2019 AHA Scientific Statement.14–17 Key elements for success in office settings include proper preparation of the patient, use of a validated upper-arm BP measurement device, correct technique, and averaging of readings (Table 1). Unfortunately, most of the devices have not been validated in patients with CKD. Patients should be instructed to empty their bladder and avoid smoking, caffeine, and exercise for at least 30 minutes before measuring their BP. They should be seated comfortably with their back supported and feet on the ground for 3 to 5 minutes before the readings. The patient and observer should refrain from talking during the rest period and during BP measurement.
Table 1.
Technique for Accurate BP Measurement
| Key Steps | Specific Instructions |
|---|---|
| Step 1: Properly prepare the patient | 1. Have the patient relax, sitting in a chair (feet on floor, back supported) for >5 min. 2. The patient should avoid caffeine, exercise, and smoking for at least 30 min before measurement. 3. Ensure patient has emptied his/her bladder. 4. Neither the patient nor the observer should talk during the rest period or during the measurement. 5. Remove all clothing covering the location of cuff placement. 6. Measurements made while the patient is sitting or lying on an examining table do not fulfill these criteria. |
| Step 2: Use proper technique for BP measurements | 1. Use a BP measurement device that has been validated, and ensure that the device is calibrated periodically. 2. Support the patient’s arm (eg, resting on a desk). 3. Position the middle of the cuff on the patient’s upper arm at the level of the right atrium (the midpoint of the sternum). 4. Use the correct cuff size, such that the bladder encircles 80% of the arm, and note if a larger- or smaller-than-normal cuff size is used. 5. Either the stethoscope diaphragm or bell may be used for auscultatory readings. |
| Step 3: Take the proper measurements needed for diagnosis and treatment of elevated BP/hypertension | 1. At the first visit, record BP in both arms. Use the arm that gives the higher reading for subsequent readings. 2. Separate repeated measurements by 1-2 min. 3. For auscultatory determinations, use a palpated estimate of radial pulse obliteration pressure to estimate SBP. Inflate the cuff 20-30 mm Hg above this level for an auscultatory determination of the BP level. 4. For auscultatory readings, deflate the cuff pressure 2 mm Hg per second, and listen for Korotkoff sounds. |
| Step 4: Properly document the accurate BP readings | 1. Record SBP and DBP. If using the auscultatory technique, record SBP and DBP as onset of the first Korotkoff sound and disappearance of all Korotkoff sounds, respectively, using the nearest even number. 2. Note the time of most recent BP medication taken before measurements. |
| Step 5: Average the readings | Use an average of ≥2 readings obtained on ≥2 occasions to estimate the individual’s level of BP. |
| Step 6: Provide BP readings to patient | Provide patients the SBP/DBP readings both verbally and in writing. |
Abbreviations: BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Reproduced from Whelton et al14 with permission of Elsevier Science and Technology Journals; original content ©2018 by the American College of Cardiology Foundation and the American Heart Association, Inc.
A variety of BP measurement devices can be used, but oscillometric devices have become the clinical standard for BP measurement.14,17 This is due to environmental concerns about mercury toxicity, the need for frequent calibration with aneroid sphygmomanometers, errors due to auscultation and inappropriately rapid deflation of the cuff, and the greater convenience and cost savings associated with use of oscillometric devices. Oscillometric devices should be preprogrammed (when possible) to record repeated measurements at 1-minute intervals after the 5-minute rest period.
Whatever instrument is used, brachial artery BPs are preferred. In those for whom it is not feasible to measure BP in the brachial artery (eg, size of arm too large), radial artery pressures measured with a validated oscillometric wrist device are favored.17 The patient’s arm should be supported and clothing at the site of the cuff should be removed. Cuff size should be appropriate for the individual’s arm circumference, and the cuff should be positioned at heart level (midsternum). Guidelines recommend averaging 2 or more readings obtained on 2 or more occasions to obtain the best estimate of BP.14,15 Patients should be informed of their BP values.
Implementation of appropriate BP measurement protocols in routine clinical practice can be challenging due to time and space constraints. Results from the Systolic Blood Pressure Intervention Trial (SPRINT) indicate that unattended and attended automated office BP measurements result in similar BPs when the core recommendations for accurate BP measurement are followed.18,19 Therefore, it is possible for rooming staff to initiate BP measurement on a patient, leave to begin rooming another patient, and return to the first patient only to remove the BP cuff and record the BPs. Measuring clinic BP appropriately also reduces or even eliminates the need for repeat measurements to confirm low or high readings. These gains in efficiency increase the feasibility of appropriate BP measurement in the routine clinical setting. Additionally, increased use of home and ambulatory BP monitoring (ABPM) can also alleviate these constraints on time, space, and personnel.
Home BP
Investigators have evaluated the utility of home BP measurements since the 1970s.20,21 Measurement of home BPs allows for identification of patients with white-coat and masked hypertension, the latter of which is more prevalent in patients with reduced kidney function,22,23 is associated with target-organ damage and adverse outcomes,22,24 and will be missed in the absence of out-of-office BP measurements. Additionally, measurement of home BP can be an effective method to overcome therapeutic inertia, improve medication adherence, and improve BP control, especially in combination with education and other strategies such as pharmacist or nurse case manager care.17 Newer devices allow for measurement of BP at night and telemonitoring with automatic transmission of BPs to providers.
As with clinic BP, the accuracy of home BPs depends on adherence to recommended guidelines.14–17 Patient training should provide information about hypertension, including the variable nature of BP and how to interpret BP readings. Guidelines recommend use of an upper-arm automated home BP monitor that has been validated and preferably has the capacity to store BP readings. Similar to clinic devices, nearly all of the validation studies for home BP monitors were conducted in the general population with normal kidney function. The important aspects of home BP measurement are similar to measurements in he clinic: empty bladder; avoidance of tobacco, alcohol, and exercise 30 minutes before BP measurement; proper positioning with feet on the floor, back straight and supported, and arm supported at heart level; at least 5 minutes of quiet rest before measurement; and use of an appropriate-sized cuff. Patients should measure their BP in the morning before taking antihypertensive medications and in the evening before dinner, with 2 readings at each time of day 1 minute apart. Patients do not need to measure home BPs daily but should obtain readings for 3 to 7 days a few weeks after initiating or changing medication and before clinic visits. Clinicians should adjust hypertension therapy based on the average of all readings over the 3- to 7-day monitoring period (minimum of 12 readings).17
Ambulatory BP
Proper technique for BP measurement is important not only for home- and office-based random measurements, but also for ABPM. Technical considerations include selection of a device validated for clinical accuracy and appropriate software that allows for analysis of the ABPM data. As with clinic and home devices, few devices have been validated for adults with CKD or kidney failure.25 Patients should receive explanations about the measurement device; selection of an appropriate arm, cuff, and bladder for their measurements; and instructions regarding completion of a diary to identify sleep and wake periods, as well as the timing of antihypertensive medication dosing.26
Many patients with CKD have comorbid conditions that complicate the use of ABPM devices (as well as clinic and home devices), including older age, obesity, arterial stiffness, and arrhythmias.17 In addition, hemodialysis patients may have restrictions on placement of the BP cuff due to access considerations.27 Finally, oscillometric diastolic BP readings may be less reliable in the presence of arterial stiffness.28,29
Software requirements, as recommended by the ESH, are shown in Box 1. The report generated by the software should include easily readable graphics for systolic and diastolic BP, mean BP, and pulse, with clearly demarcated daytime and nighttime intervals, summary statistics, and the ability to note current medications.30 Softwaregenerated reports that have been validated by comparison to expert interpretation are preferred to eliminate the potential for human variability in routine clinical settings.31 Other desirable ABPM software characteristics include the capacity to generate trend reports that allow for the comparison of ABPM measurements over time, research reports that allow for additional statistical analysis such as measurements of short-term BP variability, BP load parameters and the ambulatory arterial stiffness index, and the ability to store and export such data. Some ambulatory BP monitors have additional features that allow for measurement of arterial stiffness, position of the patient (standing or lying), and/or activity of the patient.
Box 1. ABPM Software Requirements.
Clinical report
Ambulatory blood pressure measurement analysis and report should be standardized independent of the monitor type
Standardized plot of all blood pressure measurements with daytime and nighttime windows and normal blood pressure bands demarcated
Average SBP, DBP, and heart rate to be displayed
Nocturnal blood pressure decline (%) for SBP and DBP
Summary statistics for time-weighted average SBP and DBP and heart rate for the 24-h period, daytime and nighttime, with SDs and number of valid blood pressure readings
Facility for showing error readings, if required
Optional requirements
Automated software-generated interpretative report indicating the normal or abnormal patterns and whether the requirements for a valid recording are fulfilled
Facility to plot heart rate and mean blood pressure
Trend report for comparing repeated ambulatory blood pressure measurement recordings
Ability to centrally host data
Research report
Data storage and raw data export capability for research analysis and audit
Parameters include variability measures (such as 24-h SD, 24-h weighted SD, average real variability, coefficient of variation), area under the curve calculations, blood pressure load parameters, rate-pressure product, trough and peak levels, smoothness index (the last 2 parameters requiring ABPM data before and during treatment to be available), custom-derived statistics, and ambulatory arterial stiffness index
Abbreviations: ABPM, ambulatory blood pressure monitoring; DBP, diastolic blood pressure; SBP, systolic blood pressure; SD, standard deviation.
Reproduced from O’Brien et al26 with permission of Wolters Kluwer Health, Inc; original content ©2013 Lippincott Williams & Wilkins.
Staff using ABPM devices should be trained in placement of the monitor, educating the patient about how the monitor works (including discomfort from cuff inflation), the importance of maintaining a diary, and choice of the appropriate BP cuff size and arm for placement of the cuff. BP measurements should be performed on a typical work day. BP readings should be obtained every 15 to 30 minutes during the day and typically every 30 minutes at night. Usually the nondominant arm is chosen to place the cuff, unless the dominant arm is found to provide significantly higher BP readings. Most ABPM devices provide at least 3 cuff sizes and, as with clinic and home BPs, the appropriate cuff should be used for ABPM measurements.32 If the patient’s arm circumference is greater than the largest available cuff, consideration should be given to placing the cuff on the wrist if the largest cuff has a bladder that is too small. Under these circumstances, the patient should be told to keep the forearm at heart level during their BP measurements and results should note the use of forearm readings, which are not equivalent to brachial BPs.33,34 There is some controversy regarding the editing of ABPM records for “outlier” values. At the present time, it is usually adequate to omit only physiologically impossible readings. In the presence of excessive outlier or artifact values, ABPM measurements should be repeated. An adequate recording should have a minimum of 70% of expected measurements after editing. The ESH guidelines also recommend a minimum of 20 daytime and 7 nighttime BP measurements.26
Use of Home BP Monitoring and ABPM
The current ACC/AHA guideline for the detection and treatment of hypertension recommends use of out-of-office BP measurement to confirm the diagnosis of hypertension and to monitor treatment.14 This recommendation is based on observational studies showing that out-of-office BPs are associated with adverse events. Ambulatory BPs are more strongly associated with cardiovascular disease events and mortality than clinic BPs.35–38 Home BP measurements also show a stronger association with cardiovascular events and mortality compared with office BP measurements.39,40 In a meta-analysis that included 8 observational studies with 17,698 participants, cardiovascular disease mortality was increased by 1.29-fold (95% confidence interval [CI], 1.02-1.64) for every 10–mm Hg greater home systolic BP and by 1.15-fold (95% CI, 0.91-1.46) for every 10–mm Hg greater clinic systolic BP.41 In patients with CKD, ambulatory and home BPs are stronger predictors of kidney failure, cardiovascular events, and all-cause mortality than clinic BPs.24,42–44
Use of out-of-office BP measurement is important because office BP may not be representative of patients’ home or ambulatory BP.45 Patients with CKD are at increased risk for masked hypertension, which is defined by elevated ambulatory BP with normal office BP.23 Patients with CKD and masked hypertension are at increased risk for target-organ damage, kidney failure, cardiovascular disease, and all-cause mortality.22,24 Additionally, lack of nocturnal dipping of BP is a strong predictor of cardiovascular disease events46 and is present in a significant number of patients with CKD.47 In patients with CKD, nondipping is an independent risk factor for a composite outcome of kidney failure or death.48 Given the increased prevalence of nondipping and elevated nighttime BP, ambulatory BP may be preferred over home BP for identifying masked hypertension in patients with CKD, especially those with more advanced CKD or severe proteinuria.
Currently, Medicare and most insurance companies do not provide financial coverage for ABPM in patients with established hypertension but provide coverage for its use to diagnose white-coat hypertension. This lack of coverage may soon change. The Centers for Medicare & Medicaid Services (CMS) recently proposed expansion of Medicare coverage for ABPM and may soon announce a decision regarding coverage for such monitoring for patients with established hypertension. ABPM provides information regarding nocturnal BP, but its disadvantages include the need for administrative oversight, limited availability, analysis of BP values, and lack of coverage by most insurance carriers.
In contrast, home BP monitoring can be completed independently by most patients and measurements can be obtained over extended periods (eg, several BP readings per day for several weeks or months). It is reasonable to use clinic BP as a screening tool, ABPM for diagnosis, and home BP for treatment monitoring and adjustment.16 However, treatment in all the landmark treatment trials to date has been based on clinic BPs. Of note, home and ambulatory BPs are not interchangeable; between 20% and 50% of patients will have discordant ambulatory and home BPs.49,50 Use of home BP measurements can: (1) improve patient engagement and medication adherence,14 (2) avoid issues of white-coat hypertension and help diagnose masked hypertension, and (3) reduce provider inertia for drug titration.51 Given the new recommendations will likely increase use of home BP monitoring, ongoing research is needed to better understand longitudinal changes in home BPs, how to best incorporate home BP monitoring into clinical practice, and how to implement measurements into the electronic medical record to reduce provider inertia for medication titration. Although some home BP monitors can be programmed for nocturnal BP readings, many devices do not have this capability. Some patients may be unduly worried about their level of BP, leading to excessive measurements and a cycle of anxiety. If patients are not taught proper techniques for home BP measurement, the readings will likely not provide accurate guidance for medication titration and treatment.
Observational studies and clinical trials have shown that clinicians often do not intensify antihypertensive drug therapy despite failure to meet the BP target. This has been termed provider inertia.52,53 For this reason, health systems, clinics, and providers should consider implementation of patient-centric tools that facilitate attainment of BP goals. Provider and web-based communication combined with care management has demonstrated success for attaining BP goals in studies of patients with hypertension.54,55 Increasingly, technology has begun to enable patients to upload self-measured home BP information to their medical record, a practice that may lead to eliminating the need for additional health personnel. Advances in electronic health records, capture of patientcentric data, and development of a learning health care system are emerging tools that may be used to implement BP monitoring without additional burden or delay in the practitioner’s workflow or use of additional resources.
Patient Education Regarding Proper BP Measurement Technique
A common concern regarding the validity of applying SPRINT findings to routine clinical practice is that SPRINT BP measurements were “research protocol” measurements and therefore cannot be applied in the busy clinical practice. The major flaw with this argument is that standardization of techniques has been the norm in most of the landmark BP–cardiovascular disease risk and antihypertensive treatment trials. In the context of diagnosis and management of high BP, evidence-based medicine assumes BP measurements that mimic those conducted in these studies. Standardization is common in other clinical measurements. For instance, electrocardiogram leads need to be placed correctly for proper interpretation. If laboratory measurements were performed using nonstandardized techniques, patient care would suffer tremendously. Given this, it is hard to understand the common use and acceptance in routine clinical practice of BP measurements that are not standardized.
The obvious answer is that there are no financial incentives or penalties associated with incorrect office BP measurements. There are no Medicare pay-for-performance measures for correct office BP measurements. None of the national regulatory or professional standards agencies require certification of proficiency in office BP measurement, whereas there are national standards for appropriate measurement of analytes in clinical laboratories. This omission needs to be urgently corrected. A simple measure of adherence could be the presence of 3 BP readings at a single clinic visit.
Although clinicians, clinics, and insurance companies are stakeholders in correct office BP measurement, patients are the most important stakeholders. Incorrect office BP measurements can lead to overdiagnosis and overtreatment, leading to unnecessary use of and potential adverse effects from antihypertensive medications, as well as unnecessary office visits. Less frequently, incorrect measurements can lead to undertreatment of hypertension with consequent higher risk for stroke, heart attacks, heart failure, and death.
Current patient education materials do not provide adequate and simple instructions regarding BP measurement. This should be corrected. Furthermore, insurers such as Medicare should insist on documentation of BP measurement proficiency. Patients should ensure that their office BP measurements were performed correctly and postclinic patient surveys should include questions regarding specific aspects of their BP measurements. Finally, there has to be a major patient education campaign by societies such as the National Kidney Foundation and others on proper measurement of BP in the clinic. Informational posters that demonstrate proper BP measurement techniques could be displayed in office settings (eg, Fig 2). The AHA-American Medical Association Target: BP Initiative and the Million Hearts initiative from CMS are important steps in the right direction.
Figure 2.
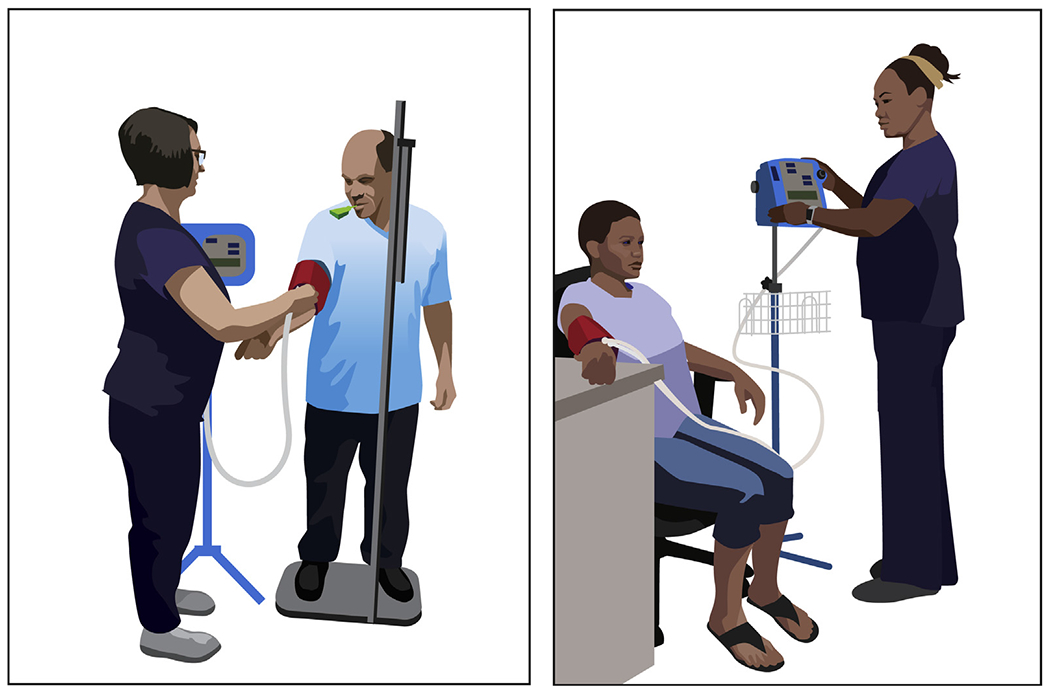
Improper (left) and proper (right) blood pressure measurement technique. Original image © Tom Mattix; reproduced with permission of the copyright holder.
Empowered knowledgeable patients who post on social media whether their clinic BP measurements were performed correctly may be the best advocates for accurate BP measurements in routine clinical practice.
Systems Design Approaches for Optimal Assessment and Management of Hypertension
Management of patients with hypertension is amenable to a systems design approach. Many studies have demonstrated that multifaceted team-based interventions are effective at improving BP control rates.14 However, only a few of these investigations have included improvement of BP measurement techniques as a component of their interventions. The Kaiser Permanente Northern California hypertension program included a registry, reports on control rates, dissemination of effective strategies to medical centers, development of an evidence-based practice guideline, and standardized training of medical assistants combined with BP competency assessments.56 The Kaiser Permanente Northern California program led to an improvement in hypertension control from 44% in 2001 to 80% in 2009.56
In a more recent study, investigators at Johns Hopkins University attempted to reduce racial disparities in hypertension care with a multilevel system quality improvement intervention that included standardization of clinical BP measurement.57,58 The BP measurement bundle included use of an automated device (Omron HEM-907XL), didactic and hands-on training for office staff, and weekly site visits to assess adherence. The protocol called for a 3-minute rest period followed by 3 BP readings at intervals of 30 seconds. Despite challenges that included overcoming workflow and time management issues, clinics successfully implemented the new protocol in 72% of encounters. Providers were less likely to recheck BPs after the intervention than before (8% vs 24%).57,58
Investigators in Canada evaluated automated office BP measurement compared to routine manual office BP in the CAMBO cluster-randomized trial.59,60 The automated protocol called for 5 readings taken every 2 minutes with the patient alone in the room. No specific instructions were provided concerning other important aspects such as positioning, appropriate cuff size, or arm support. After 2 years, BP was significantly reduced in the clinics using automated measurements (−14.3/−4.0 mm Hg) compared with those using the routine approach (−8.0/−1.5 mm Hg). Additionally, the difference in systolic BP compared to awake ambulatory BP was smaller using the automated protocol versus the manual approach (−1.8 vs −7.3 mm Hg).59
These studies demonstrate the feasibility of implementing BP measurement protocols in routine clinical practice, as well as some of the potential benefits that result, including greater adherence to the methods used in landmark risk and treatment studies, reduced need for rechecking of BPs, and lower BPs. However, no studies have compared implementation of proper versus routine BP measurement technique on important outcomes such as hypertension incidence, BP control rates, number of antihypertensive medications prescribed, and cost. Convincing studies of this type could have a profoundly positive impact on the accu racy of BP measurements in routine clinical practice.
Conclusion
Proper BP measurement technique has been a cornerstone of both the observational studies that have established hypertension as one of the leading risk factors for chronic disease and the clinical trials that have demonstrated the benefits of treating elevated BP. Regardless of whether BP is measured in the clinic, at home, or with ABPM, proper technique is critically important to ensure as accurate an assessment as possible given the inherent variability of BP. Several issues can complicate the measurement of BP in patients with CKD, including an increased likelihood of arrhythmias, arterial stiffness,61 and masked hypertension. Accurate BP measurement is particularly important in high cardiovascular disease settings such as those that prevail in patients with CKD.
Acknowledgments
Support: There was no monetary or nonmonetary support for the preparation of the manuscript. Dr Drawz was supported by grant R01HL136679 from the National Heart, Lung, and Blood Institute.
Financial Disclosure: Dr Beddhu reports research grants/funding from NIH, VA, Boeringher Ingelheim, and Bayer, as well as consultant fees from Reata and Bayer. The other authors declare that they have no relevant financial interests.
Footnotes
Other Disclosures: Dr Rocco is Chair of KDOQI. Dr Kramer is KDOQI Vice Chair for Controversies and Commentaries and President of the National Kidney Foundation.
Publisher's Disclaimer: Disclaimer: The opinions expressed here are those of the authors and not necessarily those of the American Medical Association.
Contributor Information
Paul E. Drawz, Division of Renal Diseases & Hypertension, University of Minnesota, Minneapolis, MN
Srinivasan Beddhu, Medical Service Veterans Affairs Salt Lake City Health Care System, Division of Nephrology & Hypertension, University of Utah School of Medicine, Salt Lake City, UT.
Holly J. Kramer, Division of Nephrology and Hypertension, Department of Public Health Sciences and Medicine, Loyola University Chicago, Maywood
Michael Rakotz, American Medical Association, Chicago, IL.
Michael V. Rocco, Section on Nephrology, Wake Forest School of Medicine, Winston-Salem, NC
Paul K. Whelton, Department of Epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA
References
- 1.Muntner P, Carey RM, Gidding S, et al. Potential U.S. population impact of the 2017 ACC/AHA high blood pressure guideline. J Am Coll Cardiol. 2018;71(2):109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muntner P, Anderson A, Charleston J, et al. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2010;55(3):441–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kramer HJ, Townsend RR, Griffin K, et al. KDOQI US Commentary on the 2017 ACC/AHA Hypertension Guideline. Am J Kidney Dis. 2019;73(4):437–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riva-Rocci S Un nuovo sfigmomanometro. Gazz Medi Torino. 1896;50:981–996. [Google Scholar]
- 5.Korotkoff NC. To the question of methods of determining the blood pressure. Rep Imp Military Acad. 1905;11:365–36 . [Google Scholar]
- 6.Brown AE. The Association of Life Insurance Medical Directors of America 100 years of progress. J Insur Med. 1989;21(3):156–163. [Google Scholar]
- 7.Janeway TC. The Clinical Study of Blood-Pressure. New York, NY: D Appleton & Co; 1994. [Google Scholar]
- 8.O’Brien E, Fitzgerald D. The history of blood pressure measurement. J Hum Hypertens. 1994;8(2):73–84. [PubMed] [Google Scholar]
- 9.Armitage P, Fox W, Rose GA, Tinker CM. The variability of measurements of casual blood pressure. II. Survey experience. Clin Sci. 1966;30(2):337–344. [PubMed] [Google Scholar]
- 10.Armitage P, Rose GA. The variability of measurements of casual blood pressure. I. A laboratory study. Clin Sci. 1966;30(2): 325–335. [PubMed] [Google Scholar]
- 11.Roerecke M, Kaczorowski J, Myers MG. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension: a systematic review and meta-analysis. JAMA Intern Med. 2019;179(3):351–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drawz PE, Ix JH. BP measurement in clinical practice: time to SPRINT to guideline-recommended protocols. J Am Soc Nephrol. 2018;29(2):383–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drawz P Clinical implications of different blood pressure measurement techniques. Curr Hypertens Rep. 2017;19(7):54. [DOI] [PubMed] [Google Scholar]
- 14.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):2199–2269. [DOI] [PubMed] [Google Scholar]
- 15.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. [DOI] [PubMed] [Google Scholar]
- 16.Muntner P, Einhorn PT, Cushman WC, et al. Blood pressure assessment in adults in clinical practice and clinic-based research: JACC Scientific Expert Panel. J Am Coll Cardiol. 2019;73(3):317–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muntner P, Shimbo D, Carey RM, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension. 2019;73(5):e35–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson KC, Whelton PK, Cushman WC, et al. Blood pressure measurement in SPRINT (Systolic Blood Pressure Intervention Trial). Hypertension. 2018;71(5):848–85 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kollias A, Stambolliu E, Kyriakoulis KG, Gravvani A, Stergiou GS. Unattended versus attended automated office blood pressure: systematic review and meta-analysis of studies using the same methodology for both methods. J Clin Hypertens (Greenwich). 2019;21(2):148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson AL, Taylor DW, Sackett DL, Dunnett CW, Shimizu AG. Self-recording of blood pressure in the management of hypertension. Can Med Assoc J. 1978;119(9):1034–1039. [PMC free article] [PubMed] [Google Scholar]
- 21.Julius S, Ellis CN, Pascual AV, et al. Home blood pressure determination. Value in borderline (“labile”) hypertension. JAMA. 1974;229(6):663–666. [PubMed] [Google Scholar]
- 22.Drawz PE, Alper AB, Anderson AH, et al. Masked hypertension and elevated nighttime blood pressure in CKD: prevalence and association with target organ damage. Clin J Am Soc Nephrol. 2016;11(4):642–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Drawz PE, Brown R, De Nicola L, et al. Variations in 24-hour BP profiles in cohorts of patients with kidney disease around the world: the I-DARE Study. Clin J Am Soc Nephrol. 2018;13(9):1348–1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Minutolo R, Gabbai FB, Agarwal R, et al. Assessment of achieved clinic and ambulatory blood pressure recordings and outcomes during treatment in hypertensive patients with CKD: a multicenter prospective cohort study. Am J Kidney Dis. 2014;64(5):744–752. [DOI] [PubMed] [Google Scholar]
- 25.Peixoto AJ, Gray TA, Crowley ST. Validation of the SpaceLabs 90207 ambulatory blood pressure device for hemodialysis patients. Blood Press Monit. 1999;4(5):217–221. [PubMed] [Google Scholar]
- 26.O’Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31(9):1731–1768. [DOI] [PubMed] [Google Scholar]
- 27.Clark CE, Campbell JL, Evans PH, Millward A. Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic review. J Hum Hypertens. 2006;20(12):923–931. [DOI] [PubMed] [Google Scholar]
- 28.Thompson AM, Eguchi K, Reznik ME, Shah SS, Pickering TG. Validation of an oscillometric home blood pressure monitor in an end-stage renal disease population and the effect of arterial stiffness on its accuracy. Blood Press Monit. 2007;12(4):227–232. [DOI] [PubMed] [Google Scholar]
- 29.Fagugli RM, Vecchi L, Valente F, Santirosi P, Laviola MM. Comparison between oscillometric and auscultatory methods of ambulatory blood pressure measurement in hemodialysis patients. Clin Nephrol. 2002;57(4):283–288. [DOI] [PubMed] [Google Scholar]
- 30.Stergiou GS, Palatini P, Asmar R, et al. Blood pressure monitoring: theory and practice. European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardio-vascular Variability Teaching Course Proceedings. Blood Press Monit. 2018;23(1):1–8. [DOI] [PubMed] [Google Scholar]
- 31.McGowan N, Atkins N, O’Brien E, Padfield P. Computerized reporting improves the clinical use of ambulatory blood pressure measurement. Blood Press Monit. 2010;15(3):115–123. [DOI] [PubMed] [Google Scholar]
- 32.O’Brien E Review: a century of confusion; which bladder for accurate blood pressure measurement? J Hum Hypertens. 1996;10(9):565–572. [PubMed] [Google Scholar]
- 33.Pierin AM, Alavarce DC, Gusmao JL, Halpern A, Mion D Jr. Blood pressure measurement in obese patients: comparison between upper arm and forearm measurements. Blood Press Monit. 2004;9(3):101–105. [DOI] [PubMed] [Google Scholar]
- 34.O’Brien E What to do when faced with an unmeasurable ambulatory blood pressure? J Hypertens. 2011;29(3):451–453. [DOI] [PubMed] [Google Scholar]
- 35.Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA. 1999;282(6):539–546. [DOI] [PubMed] [Google Scholar]
- 36.Shen J, Li ZM, He LZ, Deng RS, Liu JG, Shen YS. Comparison of ambulatory blood pressure and clinic blood pressure in relation to cardiovascular diseases in diabetic patients. Medicine (Baltimore). 2017;96(33):e780 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Banegas JR, Ruilope LM, de la Sierra A, et al. Relationship between clinic and ambulatory blood-pressure measurements and mortality. N Engl J Med. 2018;378(16):1509–1520. [DOI] [PubMed] [Google Scholar]
- 38.Gabbai FB, Rahman M, Hu B, et al. Relationship between ambulatory BP and clinical outcomes in patients with hypertensive CKD. Clin J Am Soc Nephrol. 2012;7(11):1770–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16(7):971–975. [DOI] [PubMed] [Google Scholar]
- 40.Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111(14):1777–1783. [DOI] [PubMed] [Google Scholar]
- 41.Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens. 2012;30(3):449–456. [DOI] [PubMed] [Google Scholar]
- 42.Agarwal R, Andersen MJ. Blood pressure recordings within and outside the clinic and cardiovascular events in chronic kidney disease. Am J Nephrol. 2006;26(5):503–510. [DOI] [PubMed] [Google Scholar]
- 43.Agarwal R, Andersen MJ. Prognostic importance of clinic and home blood pressure recordings in patients with chronic kidney disease. Kidney Int. 2006;69(2):406–411. [DOI] [PubMed] [Google Scholar]
- 44.Minutolo R, Agarwal R, Borrelli S, et al. Prognostic role of ambulatory blood pressure measurement in patients with non-dialysis chronic kidney disease. Arch Intern Med. 2011; 171(12):1090–1098. [DOI] [PubMed] [Google Scholar]
- 45.Drawz PE, Pajewski NM, Bates JT, et al. Effect of intensive versus standard clinic-based hypertension management on ambulatory blood pressure: results from the SPRINT (Systolic Blood Pressure Intervention Trial) Ambulatory Blood Pressure Study. Hypertension. 2017;69(1):42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hermida RC, Ayala DE, Mojon A, Fernandez JR. Sleep-time blood pressure and the prognostic value of isolated-office and masked hypertension. Am J Hypertens. 2012;25(3):297–305. [DOI] [PubMed] [Google Scholar]
- 47.Pogue V, Rahman M, Lipkowitz M, et al. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension. 2009;53(1):20–27. [DOI] [PubMed] [Google Scholar]
- 48.Agarwal R, Andersen MJ. Prognostic importance of ambulatory blood pressure recordings in patients with chronic kidney disease. Kidney Int. 2006;69(7):1175–1180. [DOI] [PubMed] [Google Scholar]
- 49.Gazzola K, Cammenga M, van der Hoeven NV, van Montfrans GA, van den Born BJH. Prevalence and reproducibility of differences between home and ambulatory blood pressure and their relation with hypertensive organ damage. J Hum Hypertens. 2017;31(9):555–560. [DOI] [PubMed] [Google Scholar]
- 50.Stergiou GS, Skeva II, Baibas NM, Kalkana CB, Roussias LG, Mountokalakis TD. Diagnosis of hypertension using home or ambulatory blood pressure monitoring: comparison with the conventional strategy based on repeated clinic blood pressure measurements. J Hypertens. 2000;18(12):1745–1751. [DOI] [PubMed] [Google Scholar]
- 51.Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004;329(7458):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D. Call to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. J Cardiovasc Nurs. 2008;23(4):299–323. [DOI] [PubMed] [Google Scholar]
- 53.Pickering TG, White WB; American Society of Hypertension Writing Group. ASH Position Paper: home and ambulatory blood pressure monitoring. When and how to use self (home) and ambulatory blood pressure monitoring. J Clin Hypertens (Greenwich). 2008;10(1):850–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299(24):2857–2867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159(3):185–194. [DOI] [PubMed] [Google Scholar]
- 56.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310(7):699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cooper LA, Marsteller JA, Noronha GJ, et al. A multi-level system quality improvement intervention to reduce racial disparities in hypertension care and control: study protocol. Implement Sci. 2013;8:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Boonyasai RT, Carson KA, Marsteller JA, et al. A bundled quality improvement program to standardize clinical blood pressure measurement in primary care. J Clin Hypertens (Greenwich). 2018;20(2):324–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Conventional versus automated measurement of blood pressure in the office (CAMBO) trial. Fam Pract. 2012;29(4):376–382. [DOI] [PubMed] [Google Scholar]
- 60.Myers MG, Godwin M, Dawes M, et al. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension: randomised parallel design controlled trial. BMJ. 2011;342:d286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cavallini MC, Roman MJ, Blank SG, Pini R, Pickering TG, Devereux RB. Association of the auscultatory gap with vascular disease in hypertensive patients. Ann Intern Med. 1996; 124(10):877–883. [DOI] [PubMed] [Google Scholar]


