Abstract
While disparities in depressive symptoms by race/ethnicity and gender have been documented, left unclear is how such status characteristics intersect to influence mental well-being, particularly across early life and among a diverse set of population subgroups. This study investigates how intra- and inter-individual trends in depressive symptoms unfold across a 30-year span (ages 12-42) and are structured by the intersection of race/ethnicity and gender among White, Black, Hispanic, and Asian American young adults (N=18,566). Analyses use data from the National Longitudinal Study of Adolescent to Adult Health, a nationally-representative study of adolescents who have been followed through their fourth decade of life. We draw on Waves I-IV and a representative subsample of the brand-new Wave V data. Growth curve models indicate depressive symptoms decreased across adolescence and young adulthood before increasing in the late twenties/early thirties. Racial/ethnic minorities reported more depressive symptoms than Whites. Women reported more depressive symptoms than men and experienced especially steep increases in their late 30s. Racial/ethnic-gender disparities remained stable with age, except for Hispanic-White disparities among women and Asian-White disparities among men, which narrowed with age. Overall, findings demonstrate dynamic inequalities across a longer period of the life span than was previously known, as well as heterogeneity in trajectories of poor mental health within and between racial/ethnic-gender groups. Results also suggest that Black and Asian American women experience the highest mental health risks and that interventions for reducing disparities in depressive symptoms should focus on adults in their late 20s/early 30s, particularly women of color.
Keywords: Intersectionality, Race/Ethnicity, Gender, Depressive Symptoms, Life Course
INTRODUCTION
The documented increases in levels of depressive symptoms among adolescents and young adults in recent years (e.g., [1–2]) constitute major economic, social, and health concerns. Indeed, recent estimates indicate that spending on Major Depression Disorder-related costs totaled $210.5 billion in 2010 [3]. Depressive symptoms are also linked to significant social and personal burdens, including poor health conditions such as cardiovascular disease, stroke, and anxiety [4–5]; limited achievement of socioeconomic resources such as educational attainment and labor market productivity and earnings [6,7]; and strained social and familial relationships [8]. Understanding trends and the nature of social inequalities in depressive symptoms is therefore critical to reducing disparities in mental and physical health and promoting the well-being of US society.
Existing scholarship documents the unequal distribution of depressive symptoms in the US, placing groups at varying levels of risk for social, physical health, and personal burdens. Women consistently report more depressive symptoms than men, while adolescents, young adults, and older adults tend to experience more depressive symptoms than their middle-aged adult counterparts [9–10]. Racial/ethnic differences in depressive symptoms are less clear, as prior research has produced inconsistent findings (e.g., [11]). However, more recent and accumulating evidence suggests that Blacks, Hispanics, and Asians experience more depressive symptoms than their white counterparts [12–14]. Furthermore, gender and racial/ethnic disparities in depressive symptoms across the life course are dynamic, as prior work suggests that such disparities tend to emerge in early adolescence and increase with age until early adulthood, after which disparities begin to narrow [12–13,15].
While some research has documented disparities in depressive symptoms by race/ethnicity and other studies have documented disparities by gender, less clear is whether and how race/ethnicity and gender may intersect to shape depressive symptoms, particularly across a substantial portion of the life course (i.e., from adolescence to the beginning of midlife). That is, prior research rarely considers how racial/ethnic inequality may be gendered or how gender inequality may be racialized. Instead, studies tend to treat social categories as independent of one another and assume they combine in an additive manner—meaning that health is considered a result of the (dis)advantages of one’s racial/ethnic group plus the (dis)advantages of one’s gender (e.g., [12]). Women of color, for example, would be posited to have the worst health due to the sum of disadvantages stemming from being a racial/ethnic minority and from being a woman. While these approaches lead to valuable information, they overlook the unique and simultaneous positions of power and disadvantage within which individuals may be situated. For example, African American men may hold a dominant position in the gender hierarchy, yet a subordinate position in the racial hierarchy. These positions may differentiate their lived experiences from black women and white men, and lead to distinct risk profiles for emotional well-being.
This possibility has led scholars to increasingly apply an intersectionality perspective to the study of health disparities. Intersectionality argues that systems of inequality such as racism and sexism intersect in multiplicative ways to mutually construct one another and produce unique social contexts in which privilege and oppression may be experienced simultaneously [16]. Such contexts may lead to differences in life chances and opportunities for healthy living for those within and across social groups [17–18]. Indeed, recent scholarship provides evidence suggesting that race/ethnicity and gender combine in multiplicative ways to influence health both directly—such that racial/ethnic inequalities tend to be larger among women compared to men [19–22]—and indirectly, such that the intersections of race and gender differentially shape the influence of social factors on health [23–25]. For example, a study using two datasets that collectively span adolescence, young adulthood, and midlife found evidence suggesting that racial differences in depression existed only among women [21].
Few studies, however, explicitly utilize an intersectional approach. A recent systematic review of the literature on intersectionality and depression identified only four studies that explicitly used an intersectionality perspective that was operationalized in the theoretical framing, study design, and analyses [22]. This review also found a handful of other studies that utilized approaches suggestive of intersectionality—yet, an implicit assumption of additivity remained in the studies’ framing and design. Assuming additivity among social categories may lead to over- or under-estimates of social disparities in health because such assumptions do not take into account the potential interdependence of social inequalities [16,18]. They also do not allow for considerations of heterogeneity that may exist within racial/ethnic and gender groups. Examining inter- and intra-group disparities is needed to discern the most vulnerable groups that may otherwise be overlooked in studies that rely solely on additive approaches. Such examinations may also help clarify inconsistent or contradictory findings of prior work on racial/ethnic disparities in mental health—including the documented advantages among Blacks compared to whites in terms of psychiatric disorders but disadvantages in terms of psychological distress (e.g., [26])—by providing insight into distinct patterns that exist among those positioned at varying locations in the social hierarchy.
Also missing from the literature is an investigation of the extent to which the intersecting consequences of social statuses on depressive symptoms vary with age, particularly among a diverse set of population subgroups. Prior evidence suggests that levels of depressive symptoms are dynamic across the life course, generally following a U-shaped curve. That is, depressive symptoms tend to be high in adolescence, decrease with age throughout the transition to adulthood and early adulthood, reach their lowest levels during midlife, and increase again in late life [27]. This patterning of depressive symptoms by age tends to be attributed to the roles and transitions individuals experience at different stages of the life course. For example, adolescence is a period filled with rapid changes across physical, emotional, developmental, and social domains—all of which may influence exposure to stressors and other mental health risks [28,29]. Early adulthood, however, is typically characterized by gains in status and forms of support that benefit mental health, such as completion of education, entry into the labor market, marriage and family formation, and increases in income [30,31]. The following stage of the life course, midlife, is generally accompanied by stabilization of statuses—that is, when careers are solidified and perhaps advancing, families are formed, and assets accumulate [30]. Lastly, individuals in late stages of life are likely to experience declining physical health and independence, loss of social networks, and exits from roles that perhaps once defined their identities. Such transitions embody mental health risks and have been linked to increases in depressive symptoms [30,32].
While a host of prior work has provided evidence supporting these age-related trends in depressive symptoms across adulthood (e.g., [12,15]), little work has explicitly examined how such trajectories may depend on unique positions in the social structure—namely at the intersection of racial/ethnic and gender hierarchies. Understanding how disparities in depressive symptoms at the intersection of race/ethnicity and gender change with age is crucial for several reasons. Importantly, life course theory posits that social factors and experiences accumulate throughout one’s life span and interact with one another to influence health and well-being [33]. The consequences of such factors and experiences vary by individuals’ roles, transitions, and contexts at a given time [34–35]. When paired with past scholarship documenting stark differences in the lived experiences of racial/ethnic-gender groups, it is likely that the age-patterning of depressive symptoms will vary across and within social categories.
For example, Blacks and Hispanics—particularly men—are more likely to be incarcerated [36]; be victims of police brutality [37]; live in poverty, be unemployed, have lower incomes for a given level of education [38]; and have markedly lower levels of wealth compared to their white and Asian American counterparts [39]. Women—particularly Black and Hispanic women—hold fewer positions of power and receive less pay than men who hold similar occupations [40]; are more likely to experience sexual assault and harassment [41]; and are more likely to be victims of intimate partner violence [42]. These distinct social realities of individuals at varying intersections of racial/ethnic and gender hierarchies have important implications for the development of mental health risks and, ultimately, the development of disparities in depressive symptom trajectories with age across and within social groups. In turn, disparities in mental health likely undergird the maintenance of broader patterns of social inequality, as the experience of depressive symptoms influences opportunities and abilities to attain social, economic, and political resources [6–8]. To our knowledge, no study has evaluated the extent to which race/ethnicity and gender intersect to differentially shape trajectories of depressive symptoms across early adulthood to the cusp of mid-life (e.g., ages 12-42), periods critical for shaping risks for poor health and well-being in later life.
The present study addresses these limitations of prior work by integrating intersectionality and life course perspectives to investigate changes in depressive symptoms with age among Americans across a 30-year period spanning adolescence to the cusp of mid-life. Longitudinal data have not been used to study disparities in age trends of depressive symptoms during this life stage, nor has research tested whether social statuses intersect to shape disparities in depressive symptoms. We use five waves of data from the National Longitudinal Study of Adolescent to Adult Health (Add Heath) to address two research questions critical to understanding disparities in depressive symptoms across a substantial portion of the life course: 1) to what extent do racial/ethnic inequalities in depressive symptoms vary by gender? 2) Do the intersections of race/ethnicity and gender result in widening, narrowing, or stable disparities in mental health from adolescence to the beginning of midlife (ages 12-42)? Examining how intra- and inter-individual trends in depressive symptoms unfold across the life course and are structured by the intersections of race/ethnicity and gender will shed light on the processes through which social factors differentially influence health and well-being throughout life.
METHODS
Data
Add Health is a nationally-representative, longitudinal study of US adolescents who have been followed through their fourth decade of life. Respondents were in grades 7-12 at baseline in 1994-1995 (Wave I), and follow-up data were collected in 1996 (Wave II), 2001-2002 (Wave III), and 2008-2009 (Wave IV). Response rates ranged from approximately 77%-88%. The study used a multistage, stratified, school-based, cluster sampling design. A stratified sample of 80 high schools was selected along with a feeder school in which an in-school questionnaire would be administered. Every student who attended each selected school on one day during the period of September 1994 to April 1995 was given the questionnaire. Using school rosters as the sampling frame, a gender- and grade-stratified random sample was selected, along with several oversamples (e.g., sibling pairs, race and ethnic groups including Cuban, Chinese, Puerto Rican, and African American adolescents who came from high socioeconomic backgrounds) for 90-minute in-home interviews, producing a sample size of 20,745 adolescents in Wave I when respondents were aged 12-20 [43–44].
We used data from Waves I-IV and a nationally representative subsample (n=3,872) of the newly-released Wave V data, which were collected in 2016-2017. While the Wave V follow-up interview in Add Health was fielded across three years (2016-2018), the first nationally representative sub-sample, Sample 1, was completed and its data released in fall 2017. Data for the entire Wave V cohort will be released in late 2019. Our analytic sample included respondents who participated in at least one wave of Add Health and who self-identified as non-Hispanic White, non-Hispanic Black, Hispanic, or non-Hispanic Asian American (N=18,566).
School and individual Wave I weights were used to adjust for school- and individual-level sampling probabilities, respectively. The combination of these weights ensured population estimates such that the sample was representative of the US school population in grades 7-12 in 1994-95 (Wave I) as they are followed into adulthood. Informed consent was obtained for all Add Health respondents who participated at each wave. Survey procedures were approved by the institutional review board at the University of North Carolina at Chapel Hill.
Measures
Dependent variable.
Depressive symptoms were measured at each wave and assessed with four items derived from the 20-item Center for Epidemiologic Studies-Depression Scale (CES-D): “you could not shake off the blues, even with help from your family and your friends”; “you were depressed”; “you were sad”; and “you felt happy” (α = .77, .77, .80, .81, and .82 across Wave I-V, respectively). Importantly, these items are invariant across race, ethnicity, and immigrant generation [45], making them ideal measures to contrast racial/ethnic groups. Respondents were asked how frequently they experienced each symptom in the past seven days, ranging from “never/rarely” (0) to “most of the time” (3). Responses were reverse coded when necessary and summed across the four items (range=0-12). The last item, “you felt happy”, was not asked in Wave III. We imputed values for this item as an average of Wave II and Wave IV responses. Respondents were excluded if they were missing on all four CES-D items (N=42 across all waves).
Independent variables.
Four binary variables indexed self-reported race/ethnicity: non-Hispanic White (yes=1); non-Hispanic Black (yes=1); Hispanic (yes=1); and non-Hispanic Asian American (1=yes). Non-Hispanic whites served as the reference group. Gender was measured by a dummy variable (0=men; 1=women) and age was measured in years (ages 12-42) and centered at 12.
All models controlled for whether the respondent was born outside the US (1=yes) and missing waves, defined as the number of waves in which a respondent was not interviewed, to account for differential rates of attrition or non-response across the longitudinal waves.
Analytic Strategy
To determine the extent to which racial/ethnic inequalities in depressive symptoms varied by gender, we estimated multilevel models within a mixed model framework. These models described disparities in the mean level of depressive symptoms according to the joint statuses of race/ethnicity and gender between ages 12 and 42. They adjusted for correlations and non-independence of observations due to repeated measures of the same individuals across multiple waves and clusters within the sample [46]. Model fit indices indicated a cubic age pattern best fit the data (Supplement Table 1). Linear, quadratic, and cubic age terms were included in each model. All models were stratified by gender and Chow tests—statistical tests of equality that compare parameters of different groups [47]—were used to determine whether the coefficients for race/ethnicity were statistically different for men and women. Chow tests provide information similar to an interaction term and are used in lieu of a three-way interaction so that results may be presented in a comprehensible manner [19,20,48].
Random coefficient growth curve models assessed whether and how disparities in depressive symptoms by the joint statuses of race/ethnicity and gender changed across ages 12-42. Growth curve models estimated person-specific intercepts (initial value) and slopes (rate of change) that described intra-individual variations in the relationship between age and depressive symptoms. Model fit indices suggested that fixed cubic, and random linear and quadratic slopes best fit the data (Supplement Table 1). Model fit did not improve when regressing covariates on quadratic or cubic slopes. Final models were stratified by gender, and all covariates were regressed on the intercepts and linear age slopes only.
RESULTS
Table 1 summarizes means and proportions of study variables at baseline by race/ethnicity and gender. Results indicated that women of all racial/ethnic groups reported more depressive symptoms than their same race, male counterparts. These differences were statistically significant at the .05 alpha level. Furthermore, results show a statistically significant difference in depressive symptoms by race/ethnicity within each gender group. Black and Hispanic women reported more symptoms than White women, and Black and Hispanic men reported more symptoms than White men. Both Asian American women and Asian American men reported comparable levels of depressive symptoms as their same gender, white counterparts at baseline. Taken together, Hispanic women reported the most depressive symptoms at baseline, followed by Black women, White and Asian American women, Black men, Hispanic men, and White and Asian American men.
Table. 1.
Weighted Means/Proportions, by Race/Ethnicity and Gender; Add Health, Wave I (N=18,544)
| WM | BM | HM | AM | WW | BW | HW | AW | Total | |
|---|---|---|---|---|---|---|---|---|---|
| Depressive Symptoms | 1.95 | 2.21* | 2.25* | 2.27 | 2.48† | 2.89*† | 2.94*† | 2.74† | 2.33 |
| Controls | |||||||||
| Age | 15.55 | 15.47 | 15.68 | 15.54 | 15.35† | 15.30† | 15.43† | 15.53 | 15.45 |
| Foreign born | .01 | .02 | .25* | .51* | .02 | .02 | .27* | .53* | .06 |
| Missing Waves | 1.52 | 1.79* | 1.69* | 1.67 | 1.32† | 1.43*† | 1.60* | 1.62* | 1.49 |
| N | 4888 | 1900 | 1607 | 706 | 5068 | 2133 | 1611 | 631 | 18,544 |
Note: WM, WW, BM, BW, HM, HW, AM, AW refer to White men, White women, Black men, Black women, Hispanic men, Hispanic women, Asian American men, and Asian American women, respectively.
p < 0.05 for comparison of racial/ethnic group with gender
p < .05 for comparison of men and women within racial/ethnic groups
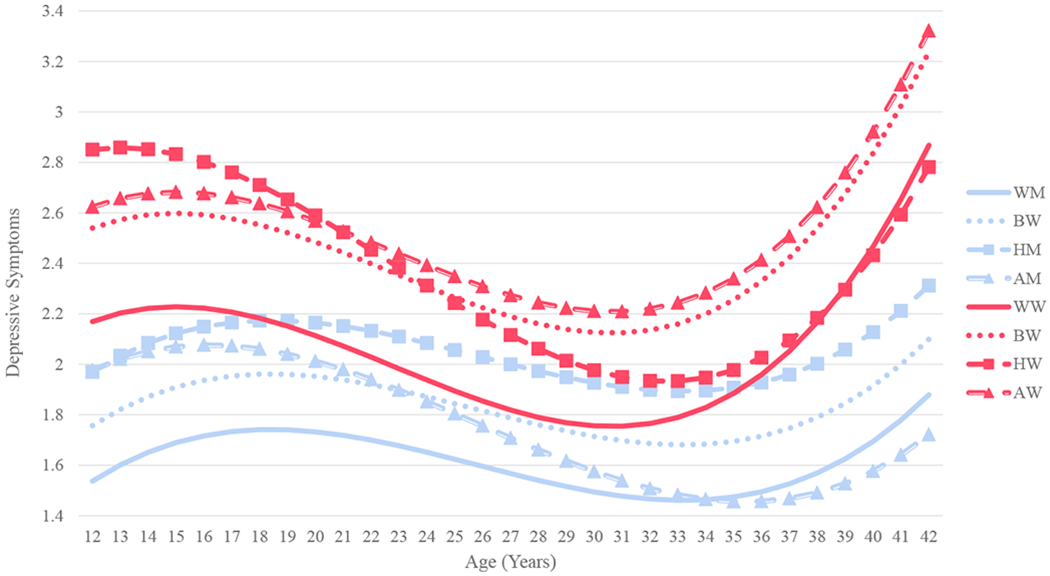
Estimates from multilevel models are presented in Table 2. Results from Model 1 indicated that within gender, all racial/ethnic minority groups reported more depressive symptoms than their White counterparts across ages 12-42. The statistically significant Chow test for the intercept suggested that White women reported more depressive symptoms than White men. When considered in tandem with the significant coefficients for race/ethnicity among men and women, all women regardless of race/ethnicity experienced higher average levels of depressive symptoms compared to their male counterparts. The non-significant Chow tests for the Black, Hispanic, and Asian American coefficients suggested the magnitude of racial/ethnic disparities was similar among men and women. These results are illustrated in Figure 1, which shows that Black, Hispanic, and Asian American women reported the highest average levels of depressive symptoms across ages 12-42.
Table. 2.
Multilevel Models of Racial/Ethnic-Gender Disparities in Depressive Symptoms (N=18,566)
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Fixed Effects a | Men | Women | bm≠w | Men | Women | m≠w |
| Constant | 1.461*** | 2.076*** | † | 1.537*** | 2.169*** | † |
| Race/Ethnicity (ref. White) | ||||||
| Black | .281*** | .415*** | .220** | .370*** | ||
| Hispanic | .323*** | .441*** | .433*** | .681*** | ||
| Asian American | .279** | .275* | .440*** | .455*** | ||
| Linear Slope (Age) | .092*** | .078*** | .071*** | .042* | ||
| Race/Ethnicity (ref. White) | ||||||
| Black | -- | -- | .007 | .007 | ||
| Hispanic | -- | -- | −.014 | −.026** | ||
| Asian American | -- | -- | −.020* | −.019 | ||
| Quadratic Slope (Age2) | −.009*** | −.011*** | −.007*** | −.008*** | ||
| Cubic Slope (Age3) | .0002*** | .0003*** | .0002*** | .0002*** | ||
| Random Effects | ||||||
| Level 1 Residual | 1.591*** | 1.843*** | 1.420*** | 1.678*** | ||
| Level 2 Age | -- | -- | .178*** | .217*** | ||
| Level 2 Age2 | -- | -- | .005*** | .006*** | ||
| Level 2 Intercept | 1.120*** | 1.373*** | 1.359*** | 2.006*** | ||
| −2 Log Likelihood | 20618552 | 24789356 | 20481940 | 24687062 | ||
| N | 9,113 | 9,453 | 9,113 | 9,453 | ||
All models control for nativity and number of waves missing
‘m≠w’ indicates Chow tests for differences between men and women
p < 0.05
p < 0.01
p < 0.001
indicates a statistically significant (p< 0.05) difference in coefficients for men and women
Figure 1.

Average Depressive Symptoms by Race/Ethnicity and Gender Across Ages 12-42 (N=18,566)
Model 2 displays results from growth curve models. The significant positive coefficients for race/ethnicity on the intercepts among both men and women indicated that racial/ethnic minorities reported more depressive symptoms at age 12 than their White counterparts. The significant Chow test for the intercept indicated that White men reported fewer depressive symptoms than White women. The non-significant Chow tests for the coefficients for race/ethnicity suggested that the magnitude of racial/ethnic inequalities in depressive symptoms at age 12 were similar by gender.
The significant positive coefficients for the linear slopes, coupled with the significant negative coefficients for the quadratic slopes and positive coefficients for the cubic slopes, indicated that depressive symptoms slightly increased in early adolescence until the late teens. Symptoms then decreased throughout the twenties and early thirties before increasing again at an exponential rate. The coefficients for Black and Hispanic on the linear age slopes among men and for Black and Asian American on the linear age slopes among women were not significant. Therefore, racial/ethnic disparities in depressive symptoms within gender remained stable among these groups across ages 12-42. Age-trajectories of depressive symptoms for each racial/ethnic-gender group are shown in Figure 2.
Figure 2.
Age Trajectories of Depressive Symptoms by Race/Ethnic-Gender Groups Across Ages 12-42 (N=18,566)
There were two groups for whom the stable inequality patterns described above did not apply: Hispanic women and Asian American men. The significant negative coefficients for Hispanic on the linear age slope among women and for Asian American on the linear age slope among men suggested that depressive symptoms among these groups increased less steeply in adolescence and declined more rapidly across early adulthood relative to their White counterparts. Disparities in depressive symptoms between Hispanic and White women and Asian American and White men therefore narrowed between ages 12 and 42. By the late twenties/early thirties, Black and Asian American women consistently experienced the most depressive symptoms out of all race/ethnic-gender groups.
DISCUSSION
High levels of depressive symptoms are a significant public health concern, as they are linked to disability, disease burden, and quality of life [4, 49] as well as significant economic costs in the US [3]. Given these associations, it is imperative to identify groups who are at increased risk of depressive symptoms and to understand how such disparities change across adolescence and the beginning of midlife. While disparities in depressive symptoms along the individual statuses of race/ethnicity and gender have been documented, few studies have investigated how the intersections of race/ethnicity and gender structure inequalities in depressive symptoms, particularly across a substantial portion of the life course. Such examinations are needed to identify the most vulnerable populations. The present study addressed this gap by investigating the joint consequences of race/ethnicity and gender on age trajectories of depressive symptoms across a 30-year span from adolescence through the fourth decade of life in a nationally representative sample. Adolescence and young adulthood are critical life stages for the development of depression that set the trajectory for health and well-being for the rest of adulthood [29, 50].
Our first objective was to evaluate the extent to which race/ethnicity and gender intersected to shape depressive symptoms across ages 12-42. We found that women, regardless of race/ethnicity, reported more depressive symptoms than men. Black, Hispanic, and Asian American women experienced more depressive symptoms, on average, than any other population subgroup across ages 12-42. These findings are consistent with growing evidence that women of color bear disproportionate burdens of poor health and well-being compared to their white and male counterparts [12, 20, 21, 51]. While depressive symptoms increased among White women during their mid- to late-30s, depressive symptoms among Black and Asian American women increased at similar rates and at higher levels as they approached midlife (Figure 2).
Our second objective was to evaluate whether the intersections of race/ethnicity and gender resulted in widening, narrowing, or stable disparities in mental health from adolescence to the beginning of midlife. Growth curve models indicated that changes in depressive symptoms with age were dynamic. Depressive symptoms increased slightly through adolescence before declining in early adulthood and increasing again in the late thirties. Age trends in depressive symptoms were more dynamic for women than for men, who showed flatter patterns of change overall. For example, the decline in depressive symptoms during the early 20s was quite dramatic for women, especially Hispanic and White women (Figure 2). In fact, the rapid decreases in depressive symptoms among Hispanic women between the early 20s and late 30s resulted in levels of symptoms falling below those among Black and Asian American women and becoming comparable to those of Hispanic men. The decline of depressive symptoms among White women also resulted in levels of symptoms similar to those of Black and Hispanic men between the early 20s and late 30s. Furthermore, the increase in depressive symptoms in the late 30s was quite steep for women compared to men, with depressive symptoms among all women surpassing those of men by age 37 (Figure 2).
While racial/ethnic minorities experienced an initial disadvantage in depressive symptoms, the age-patterning of symptoms was similar across groups, suggesting stable racial/ethnic-gender disparities across adolescence and throughout young adulthood. Two exceptions were Hispanic women and Asian American men, for whom decreases in depressive symptoms in early adulthood were steeper relative to their same gender, White counterparts. Gaps between these groups therefore narrowed with age. Hispanic women and Asian American men reported levels of depressive symptoms comparable to their White counterparts by the mid-thirties.
Research using national samples has also found that Hispanics and Asian Americans experience a more rapid decline in depressive symptoms across early adulthood and midlife [12,15]. This study goes further to show that such declines are concentrated among specific race/ethnic-gender combinations. These results indicate that racial/ethnic differences in depressive symptoms across ages 12-42 are not equivalent across gender, as would be suggested by additive approaches to health inequalities. The more rapid decreases in depressive symptoms among Hispanic women and Asian American men are intriguing, as past research also suggests foreign-born adolescents experience an initial mental health advantage relative to their US-born counterparts [52]. Indeed, approximately 26% of Hispanics and 52% of Asian Americans in our analytic sample were born outside of the US. Evidence from more recent studies that draw on both quantitative and qualitative data, however, suggests a mental health disadvantage among foreign-born adolescents. Specifically, the stressors to which children of color are exposed (e.g., discrimination, social isolation) [53] may compound with the unique stressors faced by immigrant children (e.g., stereotypes of immigrant populations, acculturation processes, identity development in a new social context) [54,55] to increase depressive symptoms among Hispanic and Asian American young adults. The consequences of such stressors may dissipate with age, perhaps due to the development of more effective coping strategies or the attainment of socioeconomic resources.
For example, family support, which is argued to be particularly protective for Hispanic families [15, 56], may increase during the transition to adulthood as adolescents experience new roles such as spouse or parent that lead to the expansion of family networks. It is possible that the mental health benefits of extended family networks are concentrated among Hispanic women given racialized notions of masculinity. That is, hegemonic masculinity requires men to fulfill specific ideals and enact certain behaviors, such as being the financial provider of the household, displaying independence and strength, and being fearless [57,58]. The pressures that result from hegemonic masculinity, as well as the barriers experienced by Hispanic men to fulfill such notions of masculinity given their subordinate position in the social hierarchy, may incur additional stressors or mitigate the benefits of additional support networks on health [20, 57–59].
Moreover, Asian American adults, particularly men, have some of the highest education and income levels by early adulthood relative to other sociodemographic groups [60,61]. These resources may enhance opportunities for emotional well-being and mitigate the negative consequences of stressors [62]. Similarly, despite initial hardships associated with immigrating to America and acculturating into US schools, foreign-born Asian American adults typically achieve intergenerational mobility, attaining higher levels of education and income than their parents. This may provide an enhanced sense of well-being and accomplishment [63].
Asian American women may not receive the same mental health benefits from socioeconomic mobility as their male counterparts given their experiences at the intersection of gender and race. That is, prior work suggests that traditional cultural norms among Asian Americans translate into women having less decision-making power in the household, assuming housekeeping and multi-generational caretaking responsibilities, and being less likely to participate in extra-familial roles compared to Asian American men and White women [64–67]. Such roles and expectations may lead to increases in unique types of stressors that compromise mental health, especially as length of residence in the US increases. For example, prior research suggests that the acculturation and assimilation processes that first- and second-generation Asian immigrants experience may be accompanied by challenges to traditional patriarchal norms of one’s country of origin [64,68]. These challenges may result in increases in intergenerational conflict among parents and female children in particular regarding gender roles, leading to higher levels of depressive symptoms [69,70].
Overall, this study documented unique mental health disadvantages among Black and Asian American women throughout adolescence, young adulthood, and the beginning of midlife. These patterns would have been overlooked in studies focusing only on racial/ethnic or gender disparities. In the context of past scholarship on institutional-level inequality [62], our findings provide evidence that the unequal distribution of life course disadvantage by race/ethnicity and gender takes a toll on the psychological well-being of Blacks, Hispanics, and Asian Americans, particularly women, across adolescence, early adulthood, and into middle adulthood. This unequal distribution of disadvantage is likely a result, in large part, of the reproduction of socioeconomic inequality across generations and the gendered forms of racism that disproportionately affect women of color across the life course [17–18, 20]. It is therefore important for future research to more explicitly consider how heterogeneity in lived experiences is linked to disparate mental health risks among individuals positioned at unique locations in the social structure.
Limitations
This study is not without limitations. Sample size constraints prevented our ability to explicitly assess how sources of heterogeneity among Hispanic and Asian American populations (e.g., by country of origin, ethnicity, and skin color) play a role in shaping age trajectories of depressive symptoms [71,72]. For example, prior research suggests that foreign-born groups exhibit better health in adulthood than their US-born counterparts [73], though this advantage tends to diminish with time spent in the US and with each new generation [52]. Given global differences in understandings of, and interactions with, racialized social structures and systems of inequality, it is likely that the mental health consequences of race and gender also vary by nativity and generational status. This possibility should be evaluated in future studies.
Additionally, depressive symptoms are one measure of emotional well-being. Other indicators of mental health may have different relationships with race/ethnicity and gender. Moreover, race/ethnicity and gender, while important social categories, are only two of several meaningful status characteristics in the US. Other statuses, such as socioeconomic position, sexual orientation, and (dis)ability, may also significantly influence mental health. When possible, future research should consider how multiple indicators of mental health are differentially distributed across an array of intersecting social statuses.
Despite these limitations, this is the first national study to document unique age trends in depressive symptoms within an innovative developmental framework that covers crucial stages of the life course over 30 years from adolescence to the beginning of midlife. Findings demonstrate dynamic inequalities across a longer period of the life span than was previously known, as well as heterogeneity in trajectories of poor mental health within and between racial/ethnic-gender groups. Results allow us to identify the most appropriate ages to target for intervention, as well as the population groups most at risk between ages 12 and 42. Indeed, the majority of research and policy attention regarding mental health disparities has focused on adolescents/young adults and women [12–13, 15]. Our results indicate that the focus on women is well justified, as their changes in depressive symptoms are the most dynamic. Women experience higher levels of depressive symptoms in adolescence, steep downward swings in early adulthood, and very steep upward increases after age 35 as they approach midlife. Although less steep, males also experience upward swings in depressive symptoms in their late 30s. Thus, primary interventions for reducing disparities in depressive symptoms should not only focus on adolescents, but also on adults in their late 20s/early 30s. These young adult ages precede the second rise in depressive symptoms as young adults approach midlife (to levels documented in adolescence) as well as the period in which disparities may solidify for the remainder of adulthood.
CONCLUSION
This study paints a troubling picture for the future mental well-being of women of color, who experienced the most depressive symptoms across adolescence and young adulthood. These stages of the life course are critical for shaping the nature of trajectories of socioeconomic achievement and health [29]. Without intervention, women of color may expect to continue experiencing poor mental health and, consequently, additional socioeconomic and health disadvantages that reinforce existing inequalities. Reducing the burden of depressive symptoms, particularly among women of color, will be critical for addressing broader disparities in mental and physical health and promoting the well-being of US society.
Supplementary Material
Acknowledgments
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth).
Note: Use of this acknowledgment requires no further permission from the persons named
Footnotes
Conflict of Interest: The authors declare they have no conflict of interest.
COMPLIANCE WITH ETHICAL STANDARDS
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
REFERENCES
- 1.Child Trends Databank (CTD). Child Trends of the National Health Interview Survey. Young Adult Depression. 2015. https://www.childtrends.org/?indicators=young-adult-depression Accessed August 2019.
- 2.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics,2016;138(6):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiat. 2015;76(2);155–162. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC. The costs of depression. Psychiat Clin N AM. 2012;35(1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA.2011;306(11):1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fletcher JM. Adolescent depression and educational attainment: results using sibling fixed effects. Health Econ. 2010;19(7):855–871. [DOI] [PubMed] [Google Scholar]
- 7.Fletcher JM. Adolescent depression and adult labor market outcomes. South Econ J. 2013;80(1):26–49. [Google Scholar]
- 8.Lépine JP, Briley M. The increasing burden of depression. Neuropsych Dis Treat. 2011;7(Suppl 1):3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mirowsky J, Ross CE. Social causes of psychological distress, 2nd edition New York, NY: Routledge; 2017. [Google Scholar]
- 10.Sutin AR, Terracciano A, Milaneschi Y, An Y, Ferrucci L, Zonderman AB. The trajectory of depressive symptoms across the adult life span. JAMA Psychiat, 2013;70(8):803–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bratter JL, Eschbach K. Race/ethnic differences in nonspecific psychological distress: evidence from the National Health Interview Survey.” Soc Sci Quarter. 2005;86(3):620–644. [Google Scholar]
- 12.Adkins D, Wang V, Dupre M, van den Oord E, Elder G. Structure and Stress: Trajectories of Depressive Symptoms across Adolescence and Young Adulthood. Soc Forces. 2009;88(1):31–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown JS, Meadows SO, Elder Jr GH. Race-ethnic inequality and psychological distress: Depressive symptoms from adolescence to young adulthood. Dev Psych. 2007;43(6):1295–1311. [DOI] [PubMed] [Google Scholar]
- 14.McLeod JD, Owens TJ. Psychological well-being in the early life course: Variations by socioeconomic status, gender, and race/ethnicity. Soc Psych Quart. 2004;67(3):257–278. [Google Scholar]
- 15.Walsemann KM, Gee GC, Geronimus AT. Ethnic differences in trajectories of depressive symptoms: Disadvantage in family background, high school experiences, and adult characteristics. J Health Soc Behav, 2009;50(1):82–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collins PH. Intersectionality’s definitional dilemmas. Ann Rev Soc. 2015;41:1–20. [Google Scholar]
- 17.Bowleg L The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Pub Health, 2012;102(7):1267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rao D, Andrasik MP, Lipira L. HIV stigma among black women in the United States: Intersectionality, support, resilience. Am J Pub Health. 2018;108(4):446–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown TH, Richardson LJ, Hargrove TW, Thomas CS. Using multiple hierarchy stratification and life course approaches to understand health inequalities: The intersecting consequences of race, gender, SES, and age. J Health Soc Behav. 2016;57(2):200–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hargrove TH. Intersecting social inequalities and body mass index trajectories from adolescence to early adulthood. J Health Soc Behav. 2018;59(1):56–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenfield S Triple jeopardy? Mental health at the intersection of gender, race, and class. Soc Sci & Med. 2012;74(11):1791–801. [DOI] [PubMed] [Google Scholar]
- 22.Patil PA, Porche MV, Shippen NA, Dallenbach NT, Fortuna LR. Which girls, which boys? The intersectional risk for depression by race and ethnicity, and gender in the US. Clin Psych Rev. 2018;66:51–68. [DOI] [PubMed] [Google Scholar]
- 23.Assari S Social determinants of depression: The intersections of race, gender, and socioeconomic status. Brain Sci. 2017;7(12):156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Assari S, Lankarani MM. Association between stressful life events and depression; intersection of race and gender. J Racial Ethn Heath Disparities. 2016;3(2):349–356. [DOI] [PubMed] [Google Scholar]
- 25.Mair CA. Social ties and depression: An intersectional examination of Black and White community-dwelling older adults. J Applied Ger. 2010;29(6):667–96. [Google Scholar]
- 26.Barnes DM, Bates LM. Do racial patterns in psychological distress shed light on the Black-White depression paradox? A systematic review. Soc Psychiatry Psychiatr Epidemiol. 2017;52(8):913–928. [DOI] [PubMed] [Google Scholar]
- 27.Clarke P, Marshall V, House J, Lantz P. The social structuring of mental health over the adult life course: advancing theory in the sociology of aging. Soc Forces. 2011;89(4):1287–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crockett LJ. Cultural, historical, and subcultural contexts of adolescence: Implications for health and development In Schulenberg J, Maggs JL, Hurrelmann K (eds) Health Risks and Developmental Transitions During Adolescence. Cambridge University Press; 1997:23–53. [Google Scholar]
- 29.Harris KM. An integrative approach to health. Demography. 2010;47(1):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mirowsky J, Ross CE. Age and depression. J Health Social Behav. 1992;33(3):187–205. [PubMed] [Google Scholar]
- 31.Mirowsky J. Age and the gender gap in depression. J Health Social Behav. 1996;37(4):362–80. [PubMed] [Google Scholar]
- 32.Yang Y, George LK. Functional disability, disability transitions, and depressive symptoms in late life. J Aging Health. 2005;17(3):263–92. [DOI] [PubMed] [Google Scholar]
- 33.Elder GH, Johnson MK, Crosnoe R. Emergence and development of life course theory” In Mortimer JT, Shanahan MJ (eds) Handbook of the Life Course. New York, NY: Kluwer; 2003:3–22. [Google Scholar]
- 34.Clarke P, Wheaton B. Mapping social context on mental health trajectories through adulthood. Adv Life Course Res, 2005:9:269–301. [Google Scholar]
- 35.Ferraro KF Life course lens on aging and health In: Shanahan MJ, Mortimer JT, Johnson MK (eds) Handbook of the Life Course. Springer, Cham: 2016:389–406. [Google Scholar]
- 36.Western B, Pettit B. Incarceration & social inequality. Daedalus. 2010;139(3):8–19. [DOI] [PubMed] [Google Scholar]
- 37.Edwards F, Esposito MH, Lee H. Risk of police-involved death by race/ethnicity and place, United States, 2012–2018. Am J Pub Health. 2018;108(9):1241–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Current Population Survey (CPS), U.S. Department of Commerce, Census Bureau. Annual Social and Economic Supplement, 1996 through 2015.
- 39.Brown TH. Diverging fortunes: Racial/ethnic inequality in wealth trajectories in middle and late life. Race and Soc Prob. 2016;8(1):29–41. [Google Scholar]
- 40.Read JN, Gorman BK. Gender and health inequality. Ann Rev Soc., 2010;11(36):371–86. [Google Scholar]
- 41.Holland KJ, Cortina LM. Sexual harassment: Undermining the wellbeing of working women In Handbook on well-being of working women (pp. 83–101). Springer, Dordrecht: 2016. [Google Scholar]
- 42.Petrosky E, Blair JM, Betz CJ, Fowler KA, Jack SP, Lyons BH. Racial and ethnic differences in homicides of adult women and the role of intimate partner violence—United States, 2003-2014. MMWR-Morbid Mort W, 2017;66(28):741–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Harris KM, Halpern CT, Whitsel EA, Hussey JM, Killeya-Jones LA, Tabor J, Dean SC. Cohort profile: The National Longitudinal Study of Adolescent to Adult Health (Add Health). Int Journ Epi. 2019. 10.1093/ije/dyz115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harris KM, Halpern CT, Hussey J, Whitsel EA, Killeya-Jones L, Tabor J, Elder G, Hewitt J, Shanahan M, Williams R, Siegler I. Social, behavioral, and genetic linkages from adolescence into adulthood. Am J Pub Health. 2013;103(S1):S25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perreira KM, Deeb-Sossa N, Harris KM, Bollen K. What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation. Soc Forces. 2005;83(4):1567–601. [Google Scholar]
- 46.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 47.Chow GC. Tests of equality between sets of coefficients in two linear regressions. Econometrica: J Econ Society. 1960;28(3):591–605. [Google Scholar]
- 48.Landry B, editor. Race, gender and class: Theory and methods of analysis. Routledge; 2007. [Google Scholar]
- 49.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ et al. Global burden of disease attributable to mental and substance use disorders: Findings from the global burden of disease study 2010. Lancet. 2013;382(9904):1575–86. [DOI] [PubMed] [Google Scholar]
- 50.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet 2012;379(9820):1056–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Seaton EK, Caldwell CH, Sellers RM, Jackson JS. An intersectional approach for understanding perceived discrimination and psychological well-being among African American and Caribbean Black youth. Dev Psych. 2010;6(5):1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Harker K Immigrant generation, assimilation, and adolescent psychological well-being. Soc Forces 2001;79(3):969–1004. [Google Scholar]
- 53.Pachter LM, Bernstein BA, Szalacha LA, Coll CG. Perceived racism and discrimination in children and youths: An exploratory study. Health Soc Work, 2010;35(1):61–9. [DOI] [PubMed] [Google Scholar]
- 54.Lui PP. Intergenerational cultural conflict, mental health, and educational outcomes among Asian and Latino/a Americans: Qualitative and meta-analytic review. Psychol Bulletin. 2015;141(2):404. [DOI] [PubMed] [Google Scholar]
- 55.Rogers-Sirin L, Ryce P, Sirin SR. Acculturation, acculturative stress, and cultural mismatch and their influences on immigrant children and adolescents’ well-being In: Dimitrova R, Bender M, van de Vijver F. (eds) Global Perspectives on Well-being in Immigrant Families. New York, NY: Springer; 2014:11–30. [Google Scholar]
- 56.Landale NS, Oropesa RS, Bradatan C. Hispanic families in the United States: Family structure and process in an era of family change In: Tienda M, Mitchell F, eds. Hispanics and the Future of America. Washington, DC: National Academies Press, 2006:138–178. [Google Scholar]
- 57.Courtenay WH. Engendering health: A social constructionist examination of men’s health beliefs and behaviors. Psych Men & Masculin. 2000;1(1):4. [Google Scholar]
- 58.Griffith DM. An intersectional approach to men’s health. J Men’s Health. 2012;9(2):106–12. [Google Scholar]
- 59.Pyke KD. Class-based masculinities: The interdependence of gender, class, and interpersonal power. Gender & Society. 1996;10(5):527–49. [Google Scholar]
- 60.Fontenot K, Semega J, Kollar M. Income and poverty in the United States: 2017 Current Population Reports. U.S. Government Printing Office, Washington, DC: 2018:60–263. [Google Scholar]
- 61.U.S. Census Bureau, Current Population Survey, 2017. Annual Social and Economic Supplement. https://www.census.gov/data/tables/2017/demo/education-attainment/cps-detailed-tables.html Accessed 19 Nov 2018.
- 62.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(S):S28–40. [DOI] [PubMed] [Google Scholar]
- 63.Chen P Assimilation of Immigrants and Their Adult Children: College Education, Cohabitation, and Work. El Paso, TX: LFB Scholarly Publishing LLC; 2011. [Google Scholar]
- 64.Pyke KD, Johnson DL. Asian American women and Racialized femininities: “Doing” gender across cultural worlds. Gender & Society. 2003;17(1):33–53. [Google Scholar]
- 65.Kibria N Family tightrope: The changing lives of Vietnamese Americans. Princeton University Press; 1995. [Google Scholar]
- 66.Alumkal AW. Preserving patriarchy: assimilation, gender norms, and second-generation Korean American evangelicals. Qual Soc. 1999;22(2):127–40. [Google Scholar]
- 67.Sodowsky GR, Kwan KL, Pannu R. Ethnic identity of Asians in the United States In: Ponterotto JG, Casas JM, Suzuki LA, Alexander CM, editors. Handbook of multicultural counseling. Thousand Oaks, CA: Sage; 1995. pp.123–154. [Google Scholar]
- 68.Chung RH. Gender, ethnicity, and acculturation in intergenerational conflict of Asian American college students. Cultural Divers Ethn Minor Psych. 2001;7(4):376. [DOI] [PubMed] [Google Scholar]
- 69.Tsai-Chae AH, Nagata DK. Asian values and perceptions of intergenerational family conflict among Asian American students. Cultural Divers Ethn Minor Psych. 2008;14(3):205. [DOI] [PubMed] [Google Scholar]
- 70.Greenberger E, Chen C. Perceived family relationships and depressed mood in early and late adolescence: A comparison of European and Asian Americans. Devel Psych. 1996;32(4):707. [Google Scholar]
- 71.Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. Am Journ Pub Health. 2007;97(1):68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chu JP, Sue S. Asian American mental health: What we know and what we don’t know. Online ReadPsychol Culture 2011;3(1):4. [Google Scholar]
- 73.Dey AN, Lucas JW. Physical and mental health characteristics of US-and foreign-born adults, United States, 1998-2003 Advance Data from Vital and Health Statistics. National Center for Health Statistics; Hyattsville, MD: 2006. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


