Abstract
Anxiety is a mental state characterized by an intense sense of tension, worry or apprehension, relative to something adverse that might happen in the future. Researchers differentiate aspects of anxiety into state and trait, respectively defined as a more transient reaction to an adverse situation, and as a more stable personality attribute in experiencing events. It is yet unclear whether brain structural and functional features may distinguish these aspects of anxiety. To study this, we assessed 42 healthy participants with the State-Trait Anxiety Inventory and then investigated with MRI to characterize structural grey matter covariance and resting-state functional connectivity (rs-FC). We found several differences in the structural–functional patterns across anxiety types: (1) trait anxiety was associated to both structural covariance of Default Mode Network (DMN), with an increase in dorsal nodes and a decrease in its ventral part, and to rs-FC of DMN within frontal regions; (2) state anxiety, instead, was widely related to rs-FC of Salience Network and of DMN, specifically in its ventral nodes, but not associated with any structural pattern. In conclusion, our study provides evidence of a neuroanatomical and functional distinction between state and trait anxiety. These neural features may be additional markers in future studies evaluating early diagnosis or treatment effects.
Subject terms: Psychology, Cognitive neuroscience, Emotion
Introduction
The human anxious psychophysiological response was first scientifically described by Sigmund Freud as a feeling of imminent and pressing danger that could be based on objective or moral risk1. A more contemporary definition2,3 considers anxiety as a mental state characterized by an intense sense of tension, worry or apprehension, relative to something adverse that might happen in the future. Anxiety can be an adaptive response driving coping behaviours to face possible dangers, but if excessive and unmotivated, can become dysfunctional, paving the way for developing anxiety disorders.
One core issue in the field has been to distinguish between anxiety as “state anxiety” defined as a temporary reaction to adverse events, and “trait anxiety”, a more stable personality feature4, defined as a constant individual difference related to a tendency to respond with concerns, troubles and worries to various situations. Trait anxiety is thought to belong to a list of characteristic traits of an individual’s personality5, and it can be associated with different psychopathological conditions and constant high arousal. Conversely, state anxiety is a more transient intense emotional state, associated with a temporary increased sympathetic nervous system activity5, but with no specific pathological conditions. Nonetheless, whether the two anxiety types are behaviourally correlated, or independent features, still remains unanswered. According to Spielberg’s6 early formulation, anxiety is a unidimensional construct including both state and trait anxiety, considered to be different sides of the same coin. In this theoretical frame, the anxious individual is characterized by a personality trait combined with a predisposition to an increased phasic anxiety level in dangerous or stressful situations. However, other authors suggested trait and state anxiety to be separate multidimensional constructs7,8.
With the aim of better understanding their neural correlates, these two anxiety types have been investigated in healthy populations, both jointly and as separate constructs, using a variety of neuroimaging techniques. Concerning structural grey matter (GM), trait anxiety is related to volume alterations in limbic regions, such as amygdala, parahippocampal gyrus, inferior temporal gyrus and inferior frontal cortex9 and abnormal cortical thickness in amygdala and cingulate regions10. At the functional level, trait anxiety impacts anterior cingulate cortex and medial prefrontal cortex activity during decision-making tasks11and mediates, in these regions, a compensatory response in cognitively demanding tasks12. As far as state anxiety is concerned, neuroimaging studies focusing on this aspect are lacking. Reported structural GM modification in state anxiety are missing and functional changes are mainly recognized as the result of anxious feelings induced during the MRI scanning13,14. Considering both anxiety types, the neural limbic system is thought to play a prominent role; in particular, amygdala activation is believed to be mediated by anxiety in unconscious emotional vigilance15. Indeed, the amygdala does not show a typical suppression in response to threat in state anxiety when the attentional focus is engaged in other tasks16, but people with high trait anxiety were found to be prone to distraction in the presence of emotional stimuli17. A clearer separation of anxiety types, and a better understanding of their neural bases, could be relevant for the clinical practice, especially if one considers that trait anxiety is a risk factor for mood and anxiety disorders18,19. Evidence exists of the fact that high trait anxiety individuals are vulnerable to develop stress-induced depression or anxiety disorders, because they display hyper-responsivity to stressful situations, increased passive coping responses to environmental challenges, alterations in cognitive functions, and lower social competitiveness18. Altogether, these factors facilitate the development of psychopathological disorders making the investigation of neural correlates of the two anxiety types of crucial importance.
Indeed, anxiety disorders are thought to be the outcome of limbic system disturbances20. Limbic regions such as amygdala and cingulate cortices are both functionally and structurally involved in anxiety disorders21,22, consequentially inducing an imbalance in the brain’s emotional centres20, which presumably drives the anxious symptomatology. Furthermore, anxiety disorders are frequently investigated as a matter of connectivity changes: several findings reported functional changes and highlighted an increased functioning of the cingulo-opercular network, also known as Salience Network (SN)23,24, and decreased functional connectivity (FC) in the Default Mode Network (DMN) while performing emotion regulation tasks25–27. In this framework, Sylvester et al., 2012, proposed a new functional network model of anxiety that considers the anxious behavioural phenomenon and anxiety disorders as a combination of disturbances in brain FC28–31. Authors suggested a characteristic FC pattern for anxiety, where an increased functioning in the SN12,32,33 is associated with a decrease in the regulation exploited by the DMN22,25,26,34–36. The stated dissociation between these two main large-scale functional networks is reported to be at the basis of trait anxiety and anxiety disorders, potentially useful in differentiating this diagnostic entity from other mental disorders. Even so, this model does not account for such connectivity disruptions to be present in state anxiety. Indeed, the functional networks dysfunction is presented only considering the personality anxious trait and the resulting pathological anxiety disorder, without elucidating what happens when the two types of anxiety are considered separately. Moreover, it is still not clear to which extent anxiety is represented by these changes in FC patterns and how these patterns are distinguished in the healthy population between the transient emotional state of anxiety and the more stable and premorbid trait anxiety37–39.
Taken together, all these studies support the idea that anxiety is a complex phenomenon where both structural and functional changes are taking place, but to the best of authors’ knowledge, none of these has tried to investigate trait and state anxiety simultaneously, both at brain structural and functional networking levels. Furthermore, the extent to which these changes happen, and how they interact with the two types of anxiety, is still not well defined. This creates a need for deepening the understanding of both anxiety types to picture a larger framework where state and trait anxiety are described both in terms of differences and communalities.
In this study, our aim is to characterize neural during rest while awake that can distinguish between trait and state anxiety, both at structural and functional brain levels. With our data-driven techniques we expected to find that the two anxiety types will be reflected differently at the neural level, in particular with trait anxiety impacting on structural GM and state anxiety resulting in perturbations of FC patterns. Particularly, trait anxiety, being a more stable individual difference encoded in the personality, should affect GM of fronto-temporal areas including the cingulate gyrus for their role in emotion processing and the top-down control of subcortical areas. Whereas, state anxiety, for its transient nature, should affect more the FC level, especially the SN, for its role in detecting potentially dangerous stimuli, and the DMN, for its function in emotion regulation, rumination and worry. Furthermore, we hypothesize that the functional dissociative pattern between DMN and SN described in Sylvester et al. 2012 applies to variations in trait and state anxiety in a healthy population.
Results
Gender differences in age and anxiety tests results were controlled across all participants and none of them proved to be relevant (Age (t(40) = 0.5301, p = 0.5989); STAI-Y1STATE (t(40) = 0.6900, p = 0.4942); STAI-Y2TRAIT (t(40) = 0.2093, p = 0.8353). The STAI-Y1STATE scores had a mean of 31 ± 4.9 and a range of 21–44; STAI-Y2TRAIT scores had a mean of 41.1 ± 9.7 with a range of 27–71. The STAI-Y1STATE scores did not significantly correlate with STAI-Y2TRAIT scores (r = 0.2516, p = 0.1080), while still showing a positive association.
Trait anxiety
Source-based morphometry
The multivariate SBM analysis was performed on 42 participants and returned 20 ICs. SBM results were then correlated with trait anxiety scores (STAI-Y2 TRAIT) using Pearson’s parametric correlation. The Sources are numbered in terms of relevance of anatomical structures in trait anxiety by means of previous evidence.
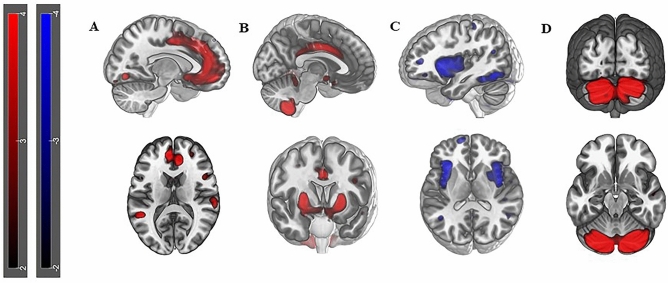
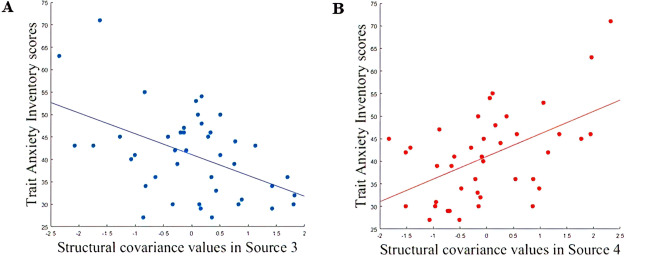
Four Sources resulted to be significantly correlated with trait anxiety (p values < 0.05): (1) positive correlation with STAI-Y2TRAIT scores in Source 1 including limbic structures as cingulate gyrus (Fig. 1A, Table 1, r = 0.3, p value = 0.04), Source 2 including temporal and frontal region (Fig. 1B, Table 1, r = 0.4, p value = 0.03) and Source 4 including portions of the cerebellum (Fig. 1D, Table 1, r = 0.5, p value = 0.0004); (2) negative correlation with STAI-Y2TRAIT scores in Source 3 including portions of the precuneus, the cuneus and of the middle temporal gyrus (Fig. 1C, Table 1, r = − 0.5, p value = 0.001). When the FDR correction is applied for testing the different 20 Sources, only Source 4 (p valueFDR = 0.0076) and Source 3 (p valueFDR = 0.0095) resulted to survive. Source 4 and 3 correlations, which are the most explicative in terms of statistic power and strength of correlation, are showed in Fig. 2. Specific details about significant Sources compositions and locations are described in Table 1.
Figure 1.
Surface reconstruction of Sources: A Reconstruction of Source 1 (r = 0.3, p value = 0.04) in the sagittal view exhibiting positive structural covariance in the anterior cingulate; B Reconstruction of Source 2 (r = 0.4, p value = 0.03) in sagittal and axial view showing positive structural covariance in limbic regions such as amygdala and cingulate gyrus; C Reconstruction of Source 3 (r = − 0.5, p value = 0.001) in the sagittal view, showing negative spatial pattern of covariance, in both hemispheres, mostly located in precuneus, cuneus and inferior frontal gyrus; D Source 4 (r = 0.5, p value = 0.0004) highlighting a strong positive structural covariance cerebellar involvement.
Table 1.
Demographic information of participants including age, gender, educational years and STAI-Y assessment.
| Participants | ||
|---|---|---|
| Gender (M/F) | 24/19 | |
| Mean | SD | |
| Age (years) | 23.8 | 2.19 |
| Education (years) | 15.4 | 11.17 |
| STAI-Y1 state anxiety | 31.0 | 11.45 |
| STAI-Y2 trait anxiety | 41.1 | 9.45 |
Figure 2.
A Correlation plot of Source 4 and STAI-Y2TRAIT scores (r = 0.5, p value = 0.0004; p valueFDR = 0.007). The caption is showing a positive correlation with the structural covariance network mainly localized in cerebellar areas. B Correlation plot of Source 3 and STAI-Y2TRAIT scores (r = − 0.5, p value = 0.001; p valueFDR = 0.009). The caption is showing a negative correlation with the structural covariance network mainly localized in precuneus, cuneus and middle temporal gyrus.
Functional connectivity analysis
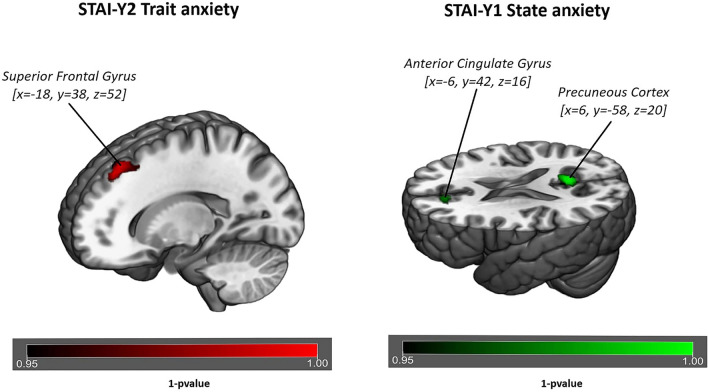
A significant correlation with trait anxiety (STAI-Y2 TRAIT), was detected in FC of the IC identified as the DMN40. Trait anxiety is shown to be associated with increase FC of the DMN in frontal regions such as superior-frontal gyrus and middle frontal gyrus (p value = 0.007, Fig. 3, Table 2). Conversely the SN is not showing any FC correlation with trait anxiety.
Figure 3.
Surface rendering of functional connectivity changes in the Default Mode Network related to trait anxiety (left of figure) and state anxiety (right of figure) respectively. Trait anxiety is shown to be correlated to functional connectivity of the Default Mode Network in the superior frontal gyrus (p value = 0.007) for p < 0.05 threshold corrected for multiple comparisons (TFCE) across voxels and p < 0.012 for Bonferroni correction across different components. State anxiety is shown to be correlated to functional connectivity of the Default Mode Network in the precuneus (p value = 0.003) and in anterior cingulate (p value = 0.0016) for p < 0.05 threshold corrected for multiple comparisons (TFCE) across voxels and p < 0.012 for Bonferroni correction across different components.
Table 2.
Anatomical labelling for statistically significant Sources correlated with trait anxiety.
| Source | p value | r-value | MNI peak coordinates | Anatomical labelling of the Harvard–Oxford atlas |
|---|---|---|---|---|
| Source 1 | 0.04 | 0.3 | [− 6, 34, 30]; [12, 41, 13] | Middle Frontal Gyrus |
| [− 50, − 39, 5] | Middle Temporal Gyrus | |||
| [− 3, 36, 24]; [9, 42, 1] | Anterior Cingulate | |||
| [− 3, 33, 27]; [9, 22, 29] | Cingulate gyrus | |||
| [− 50, − 46, 11]; [64, − 24, 11] | Superior Temporal Gyrus | |||
| Source 2 | 0.03 | 0.4 | [− 24, 3, 4]; [25, 2, 5] | Lentiform Nucleus |
| [59, − 37, − 11] | Middle Temporal Gyrus | |||
| [− 1, − 54, − 38]; [3, − 53, − 41] | Cerebellar Tonsil | |||
| [− 3, − 59, − 41]; [3, − 59, 41] | Inferior Semi-lunar Lobule | |||
| [− 27, − 62, 35]; [31, − 61, 36] | Precuneus | |||
| [0, − 1, 33]; [3, − 4, 32] | Cingulate Gyrus | |||
| [− 45, − 37, 39]; [34, − 61, 39] | Inferior Parietal Lobule | |||
| Source 3 | 0.001a | − 0.5 | [− 49, − 38, 28] | Inferior Parietal Lobule |
| [− 42, − 59, 15]; [15, − 61, 38] | Precuneus | |||
| [43, − 66, 25] | Middle Temporal Gyrus | |||
| [− 52, − 38, 31] | Supramarginal Gyrus | |||
| [53, − 17, 30] | Postcentral Gyrus | |||
| [− 16, − 11, 61]; [36,1,44] | Middle Frontal Gyrus | |||
| [− 16, − 71,10] | Cuneus | |||
| Source 4 | 0.0004a | 0.5 | [− 18, − 71, 10]; [16, − 81, − 19] | Declive |
| [− 13, − 80, − 23]; [16, − 80, − 23] | Uvula | |||
| [− 24, − 80, − 29]; [28, − 74, − 28] | Tuber | |||
| [24, − 74, − 27] | Pyramis | |||
| [− 24, − 85, − 18]; [25, − 75, − 14] | Fusiform Gyrus | |||
| [− 28, − 61, − 23]; [31, − 61, − 23] | Culmen | |||
| [− 28, − 75, − 37]; [13, − 71, − 37] | Inferior Semi-lunar Lobule |
The table is showing the strength of correlation (Pearson’s correlation coefficient), the MNI Coordinates of the peak, the anatomical name of the area. aSources surviving FDR correction for multiple comparison across 20 ICs.
State anxiety
Source-based morphometry analysis
The multivariate SBM analysis was performed on 42 participants and returned 20 ICs, as set in the analysis features. SBM results were then correlated with state anxiety scores (STAI-Y1 STATE) using Pearson’s parametric correlation. None of the 20 Sources returned by SBM were found to be significantly correlated with STAI-Y1 STATE (all p values > 0.05).
Functional connectivity analysis
Significant correlation with state anxiety, measured with STAI-Y1 STATE, was detected in FC of the ICs identified as DMN and SN40. State anxiety is shown to be associated with: (1) an increased FC of the DMN in posterior/ventral regions such as precuneus and posterior cingulate (p value = 0.003, Fig. 3, Table 2) and (2) an increased FC of the SN in temporal regions such as precentral gyrus, planum polare and Insula (p value = 0.007, Fig. 4, Table 3).
Figure 4.
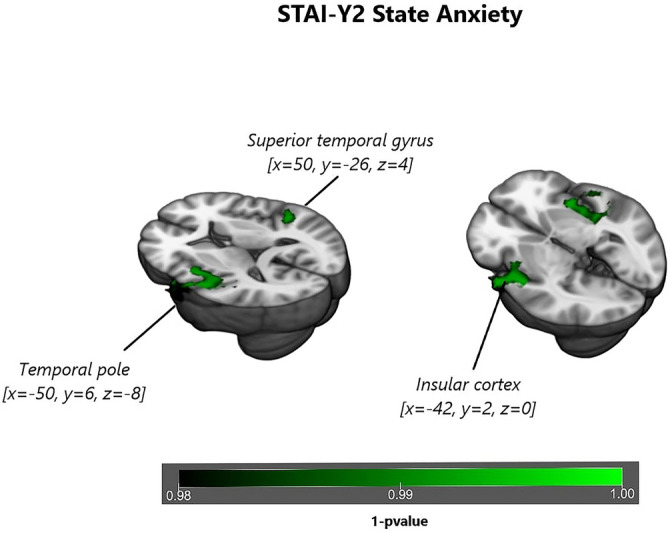
Surface rendering of functional connectivity changes in the Salience Network related to State anxiety. State anxiety is shown to be correlated to functional connectivity of the Default Mode Network in the temporal pole (p value = 0.007), superior temporal gyrus (p value = 0.006) and in insular cortex (p value = 0.008) for p < 0.05 threshold corrected for multiple comparisons (TFCE) across voxels and p < 0.012 for Bonferroni correction across different components.
Table 3.
Clusters of reliable voxels for changes in resting-state functional connectivity in the Default Mode Network associated respectively with Trait (upper rows) and State anxiety (lower rows).
| STAI-Y | p value | Cluster index | MNI peak coordinates | Anatomical labelling of the Harvard–Oxford atlas |
|---|---|---|---|---|
| Trait anxiety | 0.007 | 1 | [− 18, 38, 52] | Superior Frontal Gyrus, Frontal Pole, Middle Frontal Gyrus |
| 0.029 | 1 | [− 18, 22, 52] | Superior Frontal Gyrus, Middle Frontal Gyrus | |
| State anxiety | 0.003 | 2 | [6, − 58, 20] | Precuneous Cortex, Cingulate gyrus, posterior division, Supracalcarine Cortex |
| 0.035 | 2 | [10, − 46, 32] | Intracalcarine cortex, Cuneal Cortex | |
| 0.036 | 2 | [− 10, − 58, 16] | Cingulate Gyrus, posterior division, Precuneous Cortex | |
| 0.016 | 1 | [− 6, 42, 16] | Precuneous Cortex, Supracalcarine Cortex, Intracalcarine Cortex | |
| 0.026 | 1 | [− 6, 38, − 4] | Cingulate Gyrus, posterior division | |
| 0.03 | 1 | [− 2, 38, 4] | Paracingulate Gyrus, Cingulate gyrus, anterior division | |
| 0.035 | 1 | [− 2, 26, 12] | Cingulate Gyrus, anterior division, Paracingulate Gyrus, Frontal Medial Cortex |
MNI Coordinates of the peak, peak labelling and for p < 0.05 threshold corrected for multiple comparisons (TFCE) across voxels are reported for each cluster.
Discussion
The aim of this study was to investigate the neural basis of the trait/state distinction of anxiety in a group of healthy volunteers. One hypothesis for this distinction is that the more stable and personality aspects (trait) are implemented in structural configurations, whereas the temporary aspects of anxiety (state) correlate with functional patterns of brain activity during awake rest with eyes closed. Our main findings support this view, as we found that, while the correlation of state and trait anxiety does not reach significance in our sample of participants, trait anxiety correlates with GM structural covariance of DMN and SN nodes and with the FC of the DMN, whereas state anxiety correlates with the FC of DMN and SN.
Therefore, our results will be discussed in terms of how the DMN and SN, both with reference to structure and function, are represented and contribute to the double construct of anxiety, e.g. trait and state. When referring to anxiety, the DMN and the SN can be seen as two sides of the same coin: one side is related to self-generated thoughts, rumination, mind-wandering as the more inner component of anxiety, whereas the other side is associated to salience processing, cognitive control as the behavioural modality of facing stimuli/stressors.
Starting from the DMN, we found that its structural GM nodes covary positively with trait anxiety in fronto-temporal regions (e.g. medial frontal cortex, medial/superior temporal cortex) and negatively in parietal one (e.g. precuneus, cuneus, inferior parietal lobule); conversely, state anxiety is not structurally related with any GM structures. Previous findings highlighted how fronto-temporal nodes of the DMN are involved in social cognition and emotion processing41,42. Additionally prefrontal cortex, while being related to anxiety, showed structural GM changes43 which are thought to indirectly mediate aberrant functioning of the amygdala circuitry44,45. Indeed, since frontal regions are key components of emotion regulation systems46, and considering trait anxiety as a stable and enduring characteristic of the individual, it is plausible that these structurally altered regions mediate improper connections with the amygdala circuitry, which are instead intact in the transient emotional state.
Furthermore, we reported that functionally the DMN was frontally associated with trait anxiety, while precuneus cortex was correlated with state anxiety. This functional dissociation appears to embrace the double role of DMN functional nodes, where (1) on one hand, the prefrontal cortex has a prominent role in regulating/supressing anxiety feelings and exploiting executive control47, (2) and on the other, the posterior cingulate/precuneal regions are involved in adapting behaviour to environmental changes and attentional control48,49. That could explain why if the individual is experiencing state anxiety the brain transiently changes functional connections serving attentional processing and generates maladaptive behaviour by means of making hyper-relevant emotional events. While in a reciprocal way, the functional network is durably disturbed in trait anxiety, since the structural nodes are altered and can no longer sub-serve efficiently functional connections within the emotion regulation system. The observed effect may be established due to GM density anomalies in specific regions (e.g. frontal DMN), which by modifying the statistical dependency of the GM hemodynamic response in that defined areas, potentially give rise to abnormal FC. Nevertheless, this relationship is not one to one and we cannot assume that for a defined structural change a related FC alteration will be observed in so far as: (1) FC per se does not always depend on structural correlates but can be influenced by it50,51; and (2) functional abnormalities, in this study, are also extended to other brain regions where, due to the transient nature of the state anxiety, there are no apparent structural abnormalities. Nevertheless, consequently, in trait anxiety, emotionally relevant stimuli are always treated as salient, and the absence of regulation makes this condition a risk factor for anxiety disorder18,19,52.
This framework easily connects to our results within the SN: anterior cingulate cortex was positively correlated with trait anxiety while considering its GM structure, whereas it was functionally positively associated with state anxiety. The SN, by detecting salient changes in the surrounding environment, broadly connects the cingulate cortex and the insula with the emotion relay node of the amygdala53, which was found to be functionally associated with state anxiety and structurally with trait anxiety54,55. For this reason, our findings expand experimentally the model proposed by Sylvester et al., by confirming the involvement of both DMN and SN in anxiety, but at the same time highlight how the double construct of anxiety is represented differently at the neural level in respect to which anxiety type is considered. We did not replicate the dissociative pattern between the two networks56, but we described how different nodes of the two networks are structurally and functionally connected in different fashions based on the type of anxiety. This may allow a potential improvement in the study of therapeutic intervention for anxiety disorders. Indeed, starting from the strong structural involvement of the DMN nodes in trait anxiety, we can better associate the “neuroticism” to the putative biomarker of excessive rumination57 characterized by a hyper-functioning of the frontal part of DMN, which disrupts FC with the amygdala. At the same time, we can better describe state anxiety as temporary anxious avoidance behaviour57, where attention circuits comprising the precuneus are disrupted in favour of SN hyper-connectivity.
In this picture, by combining behavioural exhibitions and neural correlates, it will be easier to recognise the perdurable condition of an anxious personality trait from transient worries, and establish suitable approaches to regulate it (e.g. with TMS, Cognitive-behavioural therapy or Mindfulness). According to this, a strategic improvement in anxiety regulation in high trait anxiety individuals could be achieved via pharmacological and/or neurostimulation methods (e.g. TMS, or tDCS, over nodes of SN/DMN) targeting the specific areas found in this study. Such treatments could be used in anxiety disorders, in a preventive way in subclinical populations, as well as for improving diagnostic procedures by including specific neuroimaging biomarkers. Finally, these findings may lead to the creation of new diagnostic tools and treatments based on neuroscientific findings aimed at ameliorating symptoms of anxiety disorders.
However, there are some limitations in this study, which can restrict the generalizability of our results. Firstly, our sample is relatively small, and even if recent findings demonstrate no agreement in finding a biomarker for anxiety with larger sample size in favour of a stronger cognitive hypothesis58, future studies could try to replicate our results using distinct and/or larger datasets. Moreover, while considering the two types of anxiety (e.g. trait and state), we used only one psychometric test to measure it. A more comprehensive analysis could include multiple assessments to introduce several levels of description of the anxious phenomena, to reduce potential biases inherent to particular tests. Furthermore, state anxiety was measured subsequently after the MRI scan, thus introducing some limitations in correlating the psychometric score with functional activity of the brain during the MRI. Further studies should address this issue by adding complementary information of state anxiety of the participant during scanning, for example, by measuring sympathetic response or arousal levels by means of galvanic skin response, heart rate, and respiratory rhythms.
From a methodological point of view, our functional analysis was based on static functional connectivity. This approach assumes that resting-state or intrinsic networks are stationary during data acquisition. However, evidence suggests that networks fluctuate, as studied in the emerging field of functional dynamic connectivity. Various analytical methods have been proposed to estimate dynamic properties of functional connectivity, including sliding-window, time–frequency, point-process, temporal graph analyses, as described in various reviews59. The comparison of dynamic metrics across these methods is still a matter of research60, making the interpretation of results from studies challenging. In future studies, these methods could be of interest to characterize temporal fluctuations of connectivity, particularly if anxiety fluctuations could be also monitored or manipulated independently61. By means of dynamic functional connectivity, one could improve knowledge about how brain networks interact and are activated in precise moments during scanning. In this framework, the functional correlation of precuneal regions with state anxiety could be better associated with the exact timing of the adapting behavioural response in the scanner and understood as a function of its coupling or anti-coupling with the dynamics of the SN. Concerning trait anxiety, the potentially disrupted regulation function of DMN frontal regions could be observed in relationships to dynamics of the anterior cingulate cortex (here structurally related to trait anxiety), which, as subpart of the SN, could have time-varying properties different from the whole SN. Therefore, dynamic functional connectivity could bring to further insights about how FC patterns of the DMN and SN are paired in association to the double anxiety construct.
Summarizing, in this original study we attempt to decouple the double anxiety construct62 and show, by comparing its structural and functional neural correlates, how trait and state anxiety are mapped differently in the healthy human brain. Further studies could corroborate these findings by directly measuring anxiety levels during scanning and looking at the synchronous dynamic changes in FC related to trait and state anxiety.
Materials and methods
Participants
Forty-two healthy participants took part in this study (19 females and 23 males, mean age = 23.8 years, sd = 4.4, age range 19–38 years). This study was approved by the “Ethics Committee on experiments involving human beings” of the University of Trento, and all research was performed in accordance with relevant guidelines and regulations. All participants signed a written informed consent, according to guidelines set by the Ethics Committee. The inclusion criteria to participate in this study were to be aged between 18 and 45 years; absence of a history of psychiatric or neurological disease, not currently on psychoactive medications and no contraindication to MRI environment (claustrophobia, ferromagnetic material in the body, etc.). A detailed description of demographical information of participants is listed in Table 4. Participants first underwent a structural and functional Magnetic Resonance Imaging (MRI) acquisition (details below) and then answered to the State-Trait Anxiety Inventory (STAI-Y)4 at the end of the neuroimaging session. The STAI-Y consists of 40 self-report items related to anxiety, for both state (STAI-Y1STATE) and trait (STAI-Y2TRAIT) components, adapted and standardized for the Italian population4,63. STAI-Y items are rated on a 4-point Likert scale. The range for each subtest (STAI-Y1STATE and STAI-Y2TRAIT) is 20–80, a higher score indicating greater anxiety. The behavioural data were analysed with MATLAB R2016b: we tested for any a-priori gender, STAI-Y1 STATE and STAI-Y2TRAIT differences and correlation between STAI-Y1 STATE and STAI-Y2TRAIT in our sample.
Table 4.
Clusters of reliable voxels for changes in resting-state functional connectivity in the Salience Network associated with State anxiety (lower row).
| STAI-Y | p value | Cluster index | MNI peak coordinates | Anatomical labelling of the Harvard–Oxford atlas |
|---|---|---|---|---|
| State anxiety | 0.007 | 3 | [− 50, 6, − 8] | Precentral Gyrus, Inferior Frontal Gyrus, pars opercularis, Central Opercular Cortex |
| 0.007 | 3 | [− 46, − 6, − 8] | Planum Polare, Heschl's Gyrus, Insular Cortex, Frontal Operculum Cortex | |
| 0.007 | 3 | [− 38, 6, 0] | Insular Cortex, Central Opercular Cortex | |
| 0.007 | 3 | [− 62, − 2, − 12] | Precentral Gyrus, Postcentral Gyrus, Central Opercular Cortex | |
| 0.008 | 3 | [− 54, − 18, 8] | Heschl's Gyrus, Planum Temporale, Central Opercular Cortex, Planum Polare | |
| 0.009 | 3 | [− 58, − 10, 24] | Postcentral Gyrus, Precentral Gyrus | |
| 0.006 | 2 | [50, − 26, 4] | Superior Temporal Gyrus, posterior division, Planum Temporale | |
| 0.007 | 2 | [38, − 18, − 8] | Insular Cortex, Heschl's Gyrus, Planum Polare | |
| 0.007 | 2 | [38, 10, − 4] | Insular Cortex | |
| 0.009 | 2 | [38, − 6, 0] | Insular Cortex | |
| 0.013 | 2 | [50, − 10, 4] | Planum Polare, Heschl's Gyrus, Superior Temporal Gyrus | |
| 0.013 | 2 | [58, − 2, − 4] | Superior Temporal Gyrus, anterior division, Planum Polare, Heschl's Gyrus | |
| 0.048 | 1 | [− 42, − 14, 40] | Precentral Gyrus, Postcentral Gyrus |
MNI Coordinates of the peak, peak labelling and for p < 0.05 threshold corrected for multiple comparisons (TFCE) across voxels are reported for each cluster.
Image acquisition
Imaging data were acquired using a 4 T Bruker MedSpec Biospin MR scanner with a birdcage transmit and 8-channel receive head radiofrequency coil. For the resting-state functional connectivity (rs-fMRI) acquisition participants were instructed to lay still, with their eyes closed and to think of nothing in particular. The scanning duration of the rs-fMRI was approximately 8 min (215 volumes). Rs-fMRI images were acquired with a single shot T2*-weighted gradient-recalled echo-planar imaging (EPI) sequence (TR = 2,200 ms, voxel resolution = 3 × 3 × 3 mm3, TE = 33 ms, FA = 75°, FOV = 192 × 192 mm2; slice gap, 0.4 mm).
Moreover, a structural T1- weighted anatomical scan was acquired (MP-RAGE; 1 × 1 × 1 mm3; FOV, 256 × 224 mm2; 176 slices; GRAPPA acquisition with an acceleration factor of 2; TR, 2,700 ms; TE, 4.18 ms; inversion time (TI), 1,020 ms; 7° flip angle).
Image pre-processing
Off-line quality assurance (QA) was performed, before and after pre-processing steps, to check for the quality of data and to detect gross distortion or artefacts; after this step no image was discarded. QA prior to pre-processing included visual inspection of the acquired images, tSNR and standard deviation maps inspection; whereas after pre-processing, motion parameters and power spectra of the rs-fMRI time series were examined together with co-registration and normalization steps to ensure the correct progress of data analysis. Structural T1-weigthed images were pre-processed with SPM12 software (https://www.fil.ion.ucl.ac.uk/spm/soiware) through the Computational Anatomy Toolbox 12 (CAT12) (https://www.neuro.uni-jena.de/cat/). During this process, for structural images, the origin was set to reorient the image, then the T1-weighted images were segmented in GM, white matter (WM) and cerebro-spinal fluid (CSF). As in Ashburner and Friston64, alignment and normalization to MNI space were performed with smoothing application of full width at half maximum of Gaussian smoothing kernel [8, 8, 8]. Resting-state data were analysed with FMRIB Software Library (FSL65). Images Pre-processing steps include: (1) reorientation of the volumes and head motion correction performed with the rigid body transformation default settings and motion outliers regression; (2) slice timing correction; (3) brain extraction for both EPI motion corrected sequence and T1-weighted image; (4) spatial smoothing using a 6 mm full-width half maximum Gaussian kernel (twice the voxel size of the images66); (5) temporal high-pass linear filtering (100 s cut-off); (6) and finally co-registration and normalization to standard MNI template with final resampling of the functional image to 4 mm.
Source-based morphometry
Source Based Morphometry (SBM) is a multivariate whole-brain approach based on Independent Component Analysis (ICA)67. ICA application to MRI images can recognize maximally spatially independent sources in order to reveal pattern of covariation between participants that characterize T1 anatomical images. This provides information of GM structural covariance among participants. SBM was performed using the GIFT software (https://trendscenter.org/software/gift/). The software was set to detect 20 Independent Components (ICs) by default as the best option for low model order studies67–70 Infomax algorithm was chosen to compute the analysis, and the ICASSO (https://research.ics.aalto.fi/ica/icasso/) was chosen to investigate the reliability of ICA. Both RandInit and Bootstrap modes were selected in ICASSO analysis setup, and ICA was run 100 times with a minimum cluster size set up to 80. The main goal of SBM is to find a numerical vector that displays the GM volume of each component for each participant. Once the analysis has been run, SBM creates a matrix where columns refer to the sources and rows refer to participants. This matrix indicates how a specific IC is expressed in each subject. A parametric correlation test was then used to test for correlations in all subjects between each subject’s matrix and STAI-Y1STATE and STAI-Y2TRAIT anxiety scores. All results are reported both at p < 0.05 uncorrected and then at p < 0.05 FDR corrected71,72 for multiple comparison across the 20 ICs.
Resting-state functional connectivity analysis
The pre-processed resting-state fMRI data was then analysed using Multivariate Exploratory Linear Optimized Decomposition into Independent Components 3.0 (MELODIC). The multiple 4D data sets were decomposed into their distinct spatial and temporal source components using ICA, which is the same methodology used by SBM in terms of detecting maximally independent cortical networks of GM variations. As the aim of the analysis was to detect group association of resting-state FC changes associated with anxiety, we did not assume consistent temporal responses within subjects. Therefore, the ICA group analysis was temporarily concatenated (FSL65). The ICs number was manually set to 2073 as low-order model analysis. In order to separate noise components from the underlying resting-state networks, ICs were tested for their correlation (threshold of r-value > 0.2) to labelled networks40. Subsequently, 8 ICs out of 20 were identified as noise (r-value < 0.2) and were discarded from the analysis (Table S1). As a final step in the network identification, ICs was visually inspected by expert users to detect consistency between ICs matching with template networks (high correlation values)40,74 resemble well-known functional networks (see Supplementary materials). Subsequently, we performed a dual regression to investigate group differences in resting-state networks related to STAI-Y. To do so, based on our a-priori hypotheses, a one sample t-test, randomised with permutation testing, was performed on 2 ICs (see Supplementary materials, Figure S1) respectively belonging to the DMN (r-value = 0.57) and SN40(r-value = 0.40) to detect correlations in state and trait anxiety, measured with the State-Trait Anxiety Inventory (STAI-Y), demeaned across subjects before the testing as the main covariate of interest. Finally, statistical correlations were tested using non-parametric permutation testing, with threshold-free cluster enhancement (TFCE). This was done to depict specific FC patterns correlated to the two anxiety types. Resting-state FC results are reported at p value = 0.012, for p < 0.05 threshold corrected for TFCE multiple comparisons across voxels, and p < 0.012 threshold with Bonferroni correction for multiple comparisons across the 2 IC for the 2 scores of STAI-Y1STATE and STAI-Y2TRAIT.
Supplementary information
Acknowledgements
This study was partially fund by the Dipartimento di Eccellenza project, 232 law of 2016.
Author contributions
N.D.P. and A.M. designed the study, N.D.P. and A.M. collected the data, F.S. and A.M. analysed the data, all the authors interpreted the data, F.S. and N.D.P. wrote the original draft, and all the authors edited and reviewed the manuscript.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
is available for this paper at 10.1038/s41598-020-68008-z.
References
- 1.Freud S. The problem of anxiety. New York: W. W. Norton & Co.; 1936. [Google Scholar]
- 2.Hopwood CJ, Thomas KM, Markon KE, Wright AGC, Krueger RF. DSM-5 personality traits and DSM-IV personality disorders. J. Abnorm. Psychol. 2012;121:424–432. doi: 10.1037/a0026656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grillon C. Models and mechanisms of anxiety: evidence from startle studies. Psychopharmacology. 2008;199:421–437. doi: 10.1007/s00213-007-1019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the state-trait anxiety inventory. Palo Alto: Consulting Psychologists Press; 1983. [Google Scholar]
- 5.Spielberger, C. D. Conceptual and methodological issues in research on anxiety. Anxiety: Current Trends in Theory and Research on Anxiety (1972).
- 6.Vagg PR, Spielberger CD, O’Hearn TP. Is the state-trait anxiety inventory multidimensional? Personal. Individ. Differ. 1980;1:207–214. [Google Scholar]
- 7.Endler NS, Kocovski NL. State and trait anxiety revisited. J. Anxiety Disord. 2001;15:231–245. doi: 10.1016/s0887-6185(01)00060-3. [DOI] [PubMed] [Google Scholar]
- 8.Endler NS, Parker JDA, Bagby RM, Cox BJ. Multidimensionality of State and Trait Anxiety: factor structure of the Endler multidimensional Anxiety Scales. J. Pers. Soc. Psychol. 1991;60:919–926. doi: 10.1037//0022-3514.60.6.919. [DOI] [PubMed] [Google Scholar]
- 9.Hu Y, Dolcos S. Trait anxiety mediates the link between inferior frontal cortex volume and negative affective bias in healthy adults. Soc. Cogn. Affect. Neurosci. 2017;12:775–782. doi: 10.1093/scan/nsx008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Potvin O, et al. Gray matter characteristics associated with trait anxiety in older adults are moderated by depression. Int. Psychogeriatr. 2015;27:1813–1824. doi: 10.1017/S1041610215000836. [DOI] [PubMed] [Google Scholar]
- 11.Paulus MP, Feinstein JS, Simmons A, Stein MB. Anterior cingulate activation in high trait anxious subjects is related to altered error processing during decision making. Biol. Psychiatry. 2004;55:1179–1187. doi: 10.1016/j.biopsych.2004.02.023. [DOI] [PubMed] [Google Scholar]
- 12.Basten U, Stelzel C, Fiebach CJ. Trait anxiety modulates the neural efficiency of inhibitory control. J. Cogn. Neurosci. 2011;23:3132–3145. doi: 10.1162/jocn_a_00003. [DOI] [PubMed] [Google Scholar]
- 13.Mataix-Cols D, et al. Neural correlates of anxiety associated with obsessive-compulsive symptom dimensions in normal volunteers. Biol. Psychiatry. 2003;53:482–493. doi: 10.1016/s0006-3223(02)01504-4. [DOI] [PubMed] [Google Scholar]
- 14.Satpute AB, Mumford JA, Naliboff BD, Poldrack RA. Human anterior and posterior hippocampus respond distinctly to state and trait anxiety. Emotion. 2012;12:58–68. doi: 10.1037/a0026517. [DOI] [PubMed] [Google Scholar]
- 15.Etkin A, et al. Individual differences in trait anxiety predict basolateral amygdala response only to unconsciously processed fearful faces. Neuron. 2004;44:1043–1055. doi: 10.1016/j.neuron.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Bishop SJ. State anxiety modulation of the amygdala response to unattended threat-related stimuli. J. Neurosci. 2004;24:10364–10368. doi: 10.1523/JNEUROSCI.2550-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Derryberry D, Reed MA. Anxiety-related attentional biases and their regulation by attentional control. J. Abnorm. Psychol. 2002;111:225–236. doi: 10.1037//0021-843x.111.2.225. [DOI] [PubMed] [Google Scholar]
- 18.Weger M, Sandi C. High anxiety trait: a vulnerable phenotype for stress-induced depression. Neurosci. Biobehav. Rev. 2018;87:27–37. doi: 10.1016/j.neubiorev.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 19.McNally RJ. Anxiety sensitivity and panic disorder. Biol. Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- 20.Martin E, Ressler K, Binder E, Nemeroff C. The neurobiology of anxiety disorders: brain imaging, genetics, and psychoneuroendocrinology. Psychiatr. Clin. N. Am. 2013;32(3):549–575. doi: 10.1016/j.psc.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Madonna D, Delvecchio G, Soares JC, Brambilla P. Structural and functional neuroimaging studies in generalized anxiety disorder: a systematic review. Braz. J. Psychiatry. 2019;41:336–362. doi: 10.1590/1516-4446-2018-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hahn A, et al. Reduced resting-state functional connectivity between amygdala and orbitofrontal cortex in social anxiety disorder. Neuroimage. 2011;56:881–889. doi: 10.1016/j.neuroimage.2011.02.064. [DOI] [PubMed] [Google Scholar]
- 23.Hajcak G, McDonald N, Simons RF. Anxiety and error-related brain activity. Biol. Psychol. 2003;64:77–90. doi: 10.1016/s0301-0511(03)00103-0. [DOI] [PubMed] [Google Scholar]
- 24.Paulus MP, Stein MB. An insular view of anxiety. Biol. Psychiatry. 2006;60:383–387. doi: 10.1016/j.biopsych.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 25.Simmons A, et al. Anxiety vulnerability is associated with altered anterior cingulate response to an affective appraisal task. NeuroReport. 2008;19:1033–1037. doi: 10.1097/WNR.0b013e328305b722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krug MK, Carter CS. Adding fear to conflict: a general purpose cognitive control network is modulated by trait anxiety. Cogn. Affect. Behav. Neurosci. 2010;10:357–371. doi: 10.3758/CABN.10.3.357. [DOI] [PubMed] [Google Scholar]
- 27.Klumpp H, et al. Trait anxiety modulates anterior cingulate activation to threat interference. Depress. Anxiety. 2011;28:194–201. doi: 10.1002/da.20802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bishop SJ. Trait anxiety and impoverished prefrontal control of attention. Nat. Neurosci. 2009;12:92–98. doi: 10.1038/nn.2242. [DOI] [PubMed] [Google Scholar]
- 29.Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: attentional control theory. Emotion. 2007;7:336–353. doi: 10.1037/1528-3542.7.2.336. [DOI] [PubMed] [Google Scholar]
- 30.Shackman AJ, et al. The integration of negative affect, pain and cognitive control in the cingulate cortex. Nat. Rev. Neurosci. 2011;12:154–167. doi: 10.1038/nrn2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jakupcak Prevalence and psychological correlates of complicated. J. Trauma Stress. 2007;20:251–262. doi: 10.1002/jts.20223. [DOI] [PubMed] [Google Scholar]
- 32.Etkin A, Prater KE, Schatzberg AF, Menon V, Greicius MD. Disrupted amygdalar subregion functional connectivity and evidence of a compensatory network in generalized anxiety disorder. Arch. Gen. Psychiatry. 2009;66:1361–1372. doi: 10.1001/archgenpsychiatry.2009.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liao W, et al. Selective aberrant functional connectivity of resting state networks in social anxiety disorder. Neuroimage. 2010;52:1549–1558. doi: 10.1016/j.neuroimage.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 34.Kim MJ, Gee DG, Loucks RA, Davis FC, Whalen PJ. Anxiety dissociates dorsal and ventral medial prefrontal cortex functional connectivity with the amygdala at rest. Cereb. Cortex. 2011;21:1667–1673. doi: 10.1093/cercor/bhq237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Campbell-Sills L, et al. Functioning of neural systems supporting emotion regulation in anxiety-prone individuals. Neuroimage. 2011;54:689–696. doi: 10.1016/j.neuroimage.2010.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andreescu C, et al. The default mode network in late-life anxious depression. Am. J. Geriatr. Psychiatry. 2011;19:980–983. doi: 10.1097/JGP.0b013e318227f4f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Watson D. Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. J. Abnorm. Psychol. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- 38.Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. J. Abnorm. Psychol. 1994;103:103–116. [PubMed] [Google Scholar]
- 39.Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV. J. Abnorm. Psychol. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- 40.Thomas Yeo BT, et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J. Neurophysiol. 2011;106:1125–1165. doi: 10.1152/jn.00338.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang, S., Taren, A. A. & Smith, D. V. Functional parcellation of the default mode network: a large-scale meta-analysis. bioRxiv 225375 (2018). 10.1101/225375. [DOI] [PMC free article] [PubMed]
- 42.Saxe R, Moran JM, Scholz J, Gabrieli J. Overlapping and non-overlapping brain regions for theory of mind and self reflection in individual subjects. Soc. Cogn. Affect. Neurosci. 2006;1:229–234. doi: 10.1093/scan/nsl034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spampinato MV, Wood JN, De Simone V, Grafman J. (2009) Neural correlates of anxiety in healthy volunteers: a voxel-based morphometry study. J. Neuropsychiatr. Clin. Neurosci. 2009;21:199–205. doi: 10.1176/jnp.2009.21.2.199. [DOI] [PubMed] [Google Scholar]
- 44.Castagna PJ. Structure related to function: prefrontal surface area has an indirect effect on the relationship between amygdala volume and trait neuroticism. Brain Struct. Funct. 2019;224:3309–3320. doi: 10.1007/s00429-019-01974-x. [DOI] [PubMed] [Google Scholar]
- 45.Baxter MG, Murray EA. The amygdala and reward. Nat. Rev. Neurosci. 2002;3:563–573. doi: 10.1038/nrn875. [DOI] [PubMed] [Google Scholar]
- 46.Davidson RJ. Anxiety and affective style: role of prefrontal cortex and amygdala. Biol. Psychiatry. 2002;51:68–80. doi: 10.1016/s0006-3223(01)01328-2. [DOI] [PubMed] [Google Scholar]
- 47.De Pisapia N, Barchiesi G, Jovicich J, Cattaneo L. The role of medial prefrontal cortex in processing emotional self-referential information: a combined TMS/fMRI study. Brain Imaging Behav. 2018 doi: 10.1007/s11682-018-9867-3. [DOI] [PubMed] [Google Scholar]
- 48.Pearson JM, Heilbronner SR, Barack DL, Hayden BY, Platt ML. Posterior cingulate cortex: adapting behavior to a changing world. Trends Cogn. Sci. 2011;15:143–151. doi: 10.1016/j.tics.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cavanna AE, Trimble MR. The precuneus: a review of its functional anatomy and behavioural correlates. Brain. 2006;129:564–583. doi: 10.1093/brain/awl004. [DOI] [PubMed] [Google Scholar]
- 50.Batista-García-Ramó K, Fernández-Verdecia CI. What we know about the brain structure-function relationship. Behav. Sci. (Basel) 2018;8:39. doi: 10.3390/bs8040039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Messé A, Rudrauf D, Benali H, Marrelec G. Relating structure and function in the human brain: relative contributions of anatomy, stationary dynamics, and non-stationarities. PLoS Comput. Biol. 2014;10:e1003530. doi: 10.1371/journal.pcbi.1003530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cisler JM, Olatunji BO, Feldner MT, Forsyth JP. Emotion regulation and the anxiety disorders: an integrative review. J. Psychopathol. Behav. Assess. 2010;32:68–82. doi: 10.1007/s10862-009-9161-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Menon V. Salience network. Brain mapping: an encyclopedic reference. Amsterdam: Elsevier; 2015. [Google Scholar]
- 54.Baur V, Hänggi J, Langer N, Jäncke L. Resting-state functional and structural connectivity within an insula-amygdala route specifically index state and trait anxiety. Biol. Psychiatry. 2013;73:85–92. doi: 10.1016/j.biopsych.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 55.Seeley WW, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J. Neurosci. 2007;27:2349–2356. doi: 10.1523/JNEUROSCI.5587-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sylvester CM, et al. Functional network dysfunction in anxiety and anxiety disorders. Trends Neurosci. 2012;35:527–535. doi: 10.1016/j.tins.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Williams LM. Precision psychiatry: a neural circuit taxonomy for depression and anxiety. Lancet Psychiatry. 2016;3:472–480. doi: 10.1016/S2215-0366(15)00579-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Boeke EA, Holmes AJ, Phelps EA. Toward robust anxiety biomarkers: a machine learning approach in a large-scale sample. Biol. Psychiatry Cogn. Neurosci. Neuroimaging. 2019 doi: 10.1016/j.bpsc.2019.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Keilholz SD. The neural basis of time-varying resting-state functional connectivity. Brain Connect. 2014;4:769–779. doi: 10.1089/brain.2014.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen JE, Rubinov M, Chang C. Methods and considerations for dynamic analysis of fMRI data. Neuroimaging Clin. N. Am. 2018;27:547–560. doi: 10.1016/j.nic.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cohen JR. The behavioral and cognitive relevance of time-varying, dynamic changes in functional connectivity. Neuroimage. 2018;180:515–525. doi: 10.1016/j.neuroimage.2017.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Takagi Y, et al. A common brain network among state, trait, and pathological anxiety from whole-brain functional connectivity. Neuroimage. 2018;172:506–516. doi: 10.1016/j.neuroimage.2018.01.080. [DOI] [PubMed] [Google Scholar]
- 63.Pedrabissi L, Santinello M. Manuale dell’adattamento italiano dello STAI forma Y. Firenze: Organizzazioni Speciali; 1989. [Google Scholar]
- 64.Ashburner J, Friston KJ. Voxel-based morphometry: the methods. Neuroimage. 2000;11:805–821. doi: 10.1006/nimg.2000.0582. [DOI] [PubMed] [Google Scholar]
- 65.Jenkinson M, Beckmann CF, Behrens TEJ, Woolrich MW, Smith SM. Review FSL. Neuroimage. 2012;62:782–790. doi: 10.1016/j.neuroimage.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 66.Friston KJ, et al. Analysis of fMRI tim-series revesited-again. NeuroImage. 1995;2:173–181. doi: 10.1006/nimg.1995.1023. [DOI] [PubMed] [Google Scholar]
- 67.Xu L, Groth KM, Pearlson G, Schretlen DJ, Vince D. NIH Public Access. 2009;30:711–724. doi: 10.1002/hbm.20540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Segall JM, et al. Correspondence between structure and function in the human brain at rest. Front. Neuroinform. 2012;6:1–17. doi: 10.3389/fninf.2012.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pappaianni E, et al. Three shades of grey: detecting brain abnormalities in children with autism using source-, voxel- and surface-based morphometry. Eur. J. Neurosci. 2018;47:690–700. doi: 10.1111/ejn.13704. [DOI] [PubMed] [Google Scholar]
- 70.Sorella S, et al. Testing the expanded continuum hypothesis of schizophrenia and bipolar disorder. Neural and psychological evidence for shared and distinct mechanisms. NeuroImage Clin. 2019;23:101854. doi: 10.1016/j.nicl.2019.101854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann. Stat. 2001;29:1165–1188. [Google Scholar]
- 72.Benjamini, Y. & Hochberg, Y. Benjamini-1995.pdf. J. R. Stat. Soc. B57, 289–300 (1995).
- 73.Elseoud AA, et al. Group-ICA model order highlights patterns of functional brain connectivity. Front. Syst. Neurosci. 2011;5:1–18. doi: 10.3389/fnsys.2011.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Damoiseaux JS, et al. Consistent resting-state networks across healthy subjects. Proc. Natl. Acad. Sci. U.S.A. 2006;103:13848–13853. doi: 10.1073/pnas.0601417103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.