Abstract
Acyl coenzyme A binding protein (ACBP), also known as diazepam binding inhibitor (DBI) is a multifunctional protein with an intracellular action (as ACBP), as well as with an extracellular role (as DBI). The plasma levels of soluble ACBP/DBI are elevated in human obesity and reduced in anorexia nervosa. Accumulating evidence indicates that genetic or antibody-mediated neutralization of ACBP/DBI has anorexigenic effects, thus inhibiting food intake and inducing lipo-catabolic reactions in mice. A number of anorexiants have been withdrawn from clinical development because of their side effects including an increase in depression and suicide. For this reason, we investigated the psychiatric impact of ACBP/DBI in mouse models and patient cohorts. Intravenously (i.v.) injected ACBP/DBI protein conserved its orexigenic function when the protein was mutated to abolish acyl coenzyme A binding, but lost its appetite-stimulatory effect in mice bearing a mutation in the γ2 subunit of the γ-aminobutyric acid (GABA) A receptor (GABAAR). ACBP/DBI neutralization by intraperitoneal (i.p.) injection of a specific mAb blunted excessive food intake in starved and leptin-deficient mice, but not in ghrelin-treated animals. Neither i.v. nor i.p. injected anti-ACBP/DBI antibody affected the behavior of mice in the dark–light box and open-field test. In contrast, ACBP/DBI increased immobility in the forced swim test, while anti-ACBP/DBI antibody counteracted this sign of depression. In patients diagnosed with therapy-resistant bipolar disorder or schizophrenia, ACBP/DBI similarly correlated with body mass index (BMI), not with the psychiatric diagnosis. Patients with high levels of ACBP/DBI were at risk of dyslipidemia and this effect was independent from BMI, as indicated by multivariate analysis. In summary, it appears that ACBP/DBI neutralization has no negative impact on mood and that human depression is not associated with alterations in ACBP/DBI concentrations.
Subject terms: Endocrine system and metabolic diseases, Psychiatric disorders
Introduction
Acyl coenzyme A (CoA) binding protein (ACBP) has been identified as an ubiquitously expressed 86 amino acid polypeptide that binds medium-sized (C14–C22) acyl CoA chains in the cytoplasm of multiple (if not all) cell types1. In addition, this protein acts as an “endozepine” and displaces benzodiazepines such as tritium-labeled diazepam from its receptors, hence acting as diazepam binding inhibitor (DBI)1. There are two benzodiazepine receptors, the peripheral receptor, a mitochondrion-located translocator protein (TSPO), and a central receptor, which is the γ-aminobutyric acid (GABA) A receptor (GABAAR), the major inhibitory neurotransmitter receptor in the central nervous system. Full length ACBP/DBI displaces diazepam from both TSPO and GABAAR. In the central nervous system, ACBP/DBI produced by astrocytes and other cell types can be subjected to endoproteolytic cleavage to generate neuropeptides such as triakontatetraneuropeptide (residues 17–50) that acts as a selective ligand of TSPO and octadecaneuropeptide (residues 33–50) that acts as an allosteric modulator of GABAAR activity1.
Recently, we reported that ACBP/DBI plasma concentration is abnormally high in obese individuals, correlating with the fact that the periumbilical fat from obese persons expresses high levels of ACBP/DBI mRNA that diminish upon dietary intervention2. Similarly, in mice, obesity induced by a high-fat diet or a genetic deficiency of leptin results into increased expression of ACBP/DBI mRNA and protein in the liver and in adipose tissue, accompanied by an increase in circulating ACBP/DBI protein levels2. Conversely, anorexia nervosa is associated with a reduction in ACBP/DBI plasma level2,3. A prior study had shown that in patients with acute inflammatory disease, ACBP/DBI plasma levels increase, positively correlating with tumor necrosis factor-α (TNFα) levels4. Intriguingly, obesity is coupled to a state of chronic inflammation in which TNFα is elevated, contributing to the development of insulin-resistant (type-2) diabetes5,6. This points to a relationship between metabolic inflammation and the elevation of mediators such as ACBP/DBI and TNFα.
Experiments in mice revealed that intravenous (i.v.) injection of ACBP/DBI protein or transgenic expression of ACBP/DBI in the liver caused hyperphagy and weight gain. Conversely, neutralization of ACBP/DBI by an inducible whole-body knockout or intraperitoneal (i.p.) injection of neutralizing antibodies had anorexigenic effects, reducing food intake and lipo-anabolic reactions, while increasing lipo-catabolism (such as lipolysis and fatty acid oxidation), thus reducing weight gain in the context of a high-fat diet or leptin deficiency or enhancing weight loss upon a switch from a high-fat diet to a normal diet2. These findings, combined with the fact that ACBP/DBI, an evolutionarily ancient gene/protein, can stimulate sporulation in unicellular yeast species7,8 and in slime moldsan9, pharyngeal pumping in nematodes8, and mouse hook movement (the equivalent of mastication) in flies10 let us to postulate that ACBP/DBI is the elusive phylogenetically conserved appetite stimulator or “hunger factor”11,12.
Eating disorders such as anorexia nervosa and morbid obesity are metabolic diseases with a psychiatric component. Importantly, prototypic psychiatric diseases including treatment-resistant depression and severe schizophrenia are coupled to major derangements in appetite and body weight and often lead to a state of metabolic syndrome that negatively affects life expectancy13–15. Obviously, the GABAergic system composed by GABA and its receptors plays a major role in the central nervous system16,17 as well as in the regulation of metabolism18 and inflammation19.
Intrigued by these premises, we decided to investigate the possible impact of ACBP/DBI on psychiatric conditions. For this, we addressed the questions as to whether ACBP/DBI stimulates appetite through its binding to acyl CoA or an action on GABAAR and whether ACBP/DBI affects the behavior of mice upon its artificial elevation or neutralization in peripheral tissues. We also measured ACBP/DBI concentration in the plasma of psychiatric patients to understand its potential impact on mental vs. metabolic disease.
Materials and methods
Mouse experiments
Eight- to ten-week-old male C57BL/6 mice, Wild-type (WT, Envigo, Gannat, France and Janvier, Le Genest-Saint-Islen, France), B6.Cg-Lepob/J ob/ob mice, S/B6.V-LEP+/Ob (JAX™ Mice Strain, Charles River Laboratory, Lentilly, France) or Gabrg2tm1Wul/J, containing the point mutation F77I in the gamma-aminobutyric acid (GABA) A receptor γ2 subunit20 (JAX™ Mice Strain, Charles River Laboratory, Lentilly, France) were bred and maintained according to the FELASA guidelines and local guidelines from the Animal Experimental Ethics Committee (#04447.02, #2315-2015101617138161v1, #8530-2017011216394941v2, #10862-2017080217568517v3, #25032, 19144-201805041255279v2, France).
Treatments
Mice were housed in a temperature-controlled environment with 12 h light/dark cycles and received normal diet and water ad libitum. Mice were subjected to 24 h starvation (Unfed), injected intraperitoneally or intravenously and cumulative food intake was analyzed. The mAb 7A antibody against ACBP/DBI or the isotype IgG2a control were used in vivo (5 µg/g body weight (BW), i.p, in total volume 200 μL) (Fred Hutch Antibody Technology, Seattle, WA, USA). Recombinant mouse ACBP/DBI (i.v., in total volume of 200 μL, 0.5 mg/kg BW) (recACBP/DBI, from Institute of Psychiatry and Neuroscience of Paris, France) or the vehicle control (phosphate-buffered saline) were used in vivo. Moreover, two mutant forms of mouse recombinant ACBP/DBI were used in which two conserved residues were substituted (Y29F and K33A), reducing the affinity of ACBP/DBI for the acyl-CoAs21. Recombinant mouse Ghrelin (purchased by Merk Millipore) was administered by i.p. injection at 10 µg/25 g BW.
Food intake analysis
Food intake was monitored as previously described2. In brief, food was removed 2 h prior to experimentation followed by individual housing and acclimatization in individual cages. Different treatments were administered and the accumulated food intake was monitored.
Light-to-dark transition test (D/LT)
Test based on the innate aversion of rodents to brightly illuminated areas and on their spontaneous exploratory behavior in response to the stressor that light represents22. The test apparatus consists of a dark, safe compartment and an illuminated, aversive one (43 × 43 cm chamber). The lit compartment was brightly illuminated with an 8 W fluorescent tube (1000 lx). Naive mice were placed individually in the testing chamber in the middle of the dark area facing away from the doorway to the light compartment. Mice were tested for 10 min, and four parameters were recorded: time spent in the lit compartment, the number of transitions between compartments, the speed of the mice and the distance spent in the lit compartment indices of anxiety-related behavior and exploratory activity. Behavior was scored using an infrared light beam activity monitor using actiMot2 Software (PhenoMaster Software, TSE) and it was statistically analyzed using Prism program.
Open-field test (OFT)
Test takes advantage of the aversion of rodents to brightly lit areas22. Each mouse is placed in the center of the OFT chamber (43 × 43 cm chamber) and allowed to explore for 30 min. Mice were monitored throughout each test session by infrared light beam activity monitor using actiMot2 Software (PhenoMaster Software, TSE). The overall motor activity was quantified as the total distance travelled (ambulation). Anxiety was quantified by measuring the time and distance spent in the center versus periphery of the open-field chamber. Behavior was scored using an infrared light beam activity monitor using actiMot2 Software (PhenoMaster Software, TSE) and it was statistically analyzed using Prism program.
Forced swim test (FST)
Test based on the observation that rodents, after initial escape-oriented movements, develop an immobile posture when placed in an inescapable stressful situation23. Each mouse is placed in a cylinder (height: 25 cm and diameter: 10 cm) filled with water (23–25 °C). Mice were tested for 5 min, and the time spent immobile (behavioral despair) was quantified.
ACBP/DBI detection in human plasma samples
Plasma ACBP/DBI levels were measured in two different cohorts of bipolar and schizophrenic patients, by means of the KA0532 ACBP (Human) ELISA kit. The subjects (n = 271) were participants of the FACE-BD and FACE-SZ studies13–15. Dyslipidaemia and type 2 diabetes were extracted from patient’s medical history. Hypertension was defined as systolic blood pressure ≥ 140 and/or diastolic blood pressure ≥ 90 mmHg. Abdominal obesity was defined as waist circumference ≥ 94 cm or 37 in. (male) or ≥80 cm or 31.5 in. (female). Metabolic syndrome was defined according to the International Diabetes Foundation definition24.
Statistical analysis
Data are reported as Box and whisker plots (mean, first and third quartiles, and maximum and minimum values). The number of independent data points (n) is indicated in the corresponding graphs or in the legends. For statistical analyses, p values were calculated by two-way ANOVA, one-way ANOVA with Tukey’s multiple comparisons test or two-tailed unpaired Student’s t test as indicated (Prism version 7, GraphPad Software). Differences were considered statistically significant when p values *(p < 0.05), **(p < 0.01), ***(p < 0.001), and n.s. = not significant (p > 0.05). For the analysis of human samples, means (±standard deviation or standard error of the mean) were compared with two-tailed unpaired Student’s t test and Pearson’s correlation coefficients with their 95% confidence interval were calculated. A generalized linear model was constructed to calculate odds ratios between ACBP/DBI (per 1 ng/mL increase) and categorical metabolic variables in a univariate model and in a multivariate model incorporating body mass index (BMI).
Results
Appetite stimulation by ACBP/DBI in mice through an action on GABAA receptors
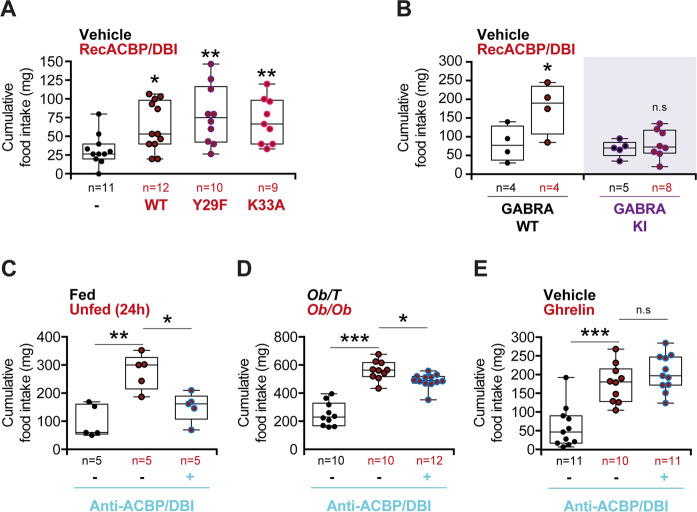
As indicated by its dual name, ACBP/DBI has two fundamentally distinct functions, as a protein that binds acyl coenzyme A (CoA) and as a protein that binds to GABAAR. The interaction with acyl-CoA is reduced by 3 orders of magnitude upon mutation of tyrosine residue 29 to phenylalanine, Y29F, or mutation of lysine residue 33 to alanine, K33A (Supplementary Fig. S1a)21,25. I.v. injection of such mutated Y29F or K33A ACBP/DBI recombinant proteins induced a similar hyperphagic response as did the WT protein (Fig. 1a), indicating that appetite stimulation by ACBP/DBI does not rely exclusively on the binding of acyl-CoA-related metabolites. The action of ACBP/DBI on GABAA receptor is lost in mice in which the γ2 subunit bears a point mutation substituting the phenylalanine residue 77 to isoleucine, F77I) (Supplementary Fig. S1b)20,26. Mice bearing this knockin (KI) mutation failed to mount a hyperphagic response upon injection of WT ACBP/DBI in conditions in which age- and sex-matched WT control mice did increase their food intake (Fig. 1b), indicating that ACBP/DBI indeed acts on GABAA receptors to stimulate appetite.
Fig. 1. Analysis of feeding behavior modulated by ACBP/DBI.
a Cumulative food intake was measured after 60 min in WT mice injected with recombinant ACBP/DBI (recACBP/DBI) protein, its mutant forms Y29F or K33A (i.v., 0.5 mg/kg BW) or a vehicle control (a), in GABRA WT or GABRA knock-in (KI) mice upon recACBP/DBI i.v. injection (b), in WT mice after 24 h of starvation (Unfed) (c), in obese Ob/Ob or lean Ob/T mice (d), and in WT mice after Ghrelin injection (i.p., 10 µg/25 g BW) (e), all of them either alone or in combination with the i.p injection of an antibody against ACBP/DBI (anti-ACBP/DBI, i.p., 5 µg/g BW). Quantitative results are reported as box and whisker plots (mean, first and third quartiles, and maximum and minimum values). For statistical analyses, p values were calculated by two-way ANOVA (b) or one-way ANOVA with Tukey’s multiple comparisons test (a, c–e). Differences were considered statistically significant when p values *(p < 0.05), **(p < 0.01), ***(p < 0.001) and n.s. not significant (p > 0.05).
Of note, i.p. injection of a neutralizing ACBP/DBI-specific monoclonal antibody (mAb) was able to inhibit food intake in mice that had been rendered hyperphagic (Supplementary Fig. S1c) by a 24-h starvation period (Fig. 1c). Similarly, anti-ACBP/DBI mAb reduced food intake in mice homozygous for the Lepob mutation (often referred to as ob/ob mice) that are rendered hyperphagic due to a mutation in the gene encoding for the appetite inhibitor leptin (Fig. 1d). In contrast, ACBP/DBI neutralization was unable to interfere with hyperphagy induced by ghrelin injection (Fig. 1e), indicating that anti-ACBP/DBI mAb has a specific rather than general effect on food intake. Thus, the possibility that anti-ACBP/DBI mAb would simply induce a general lethargy that compromises food intake can be excluded.
Effects of ACBP/DBI on the behavior of mice
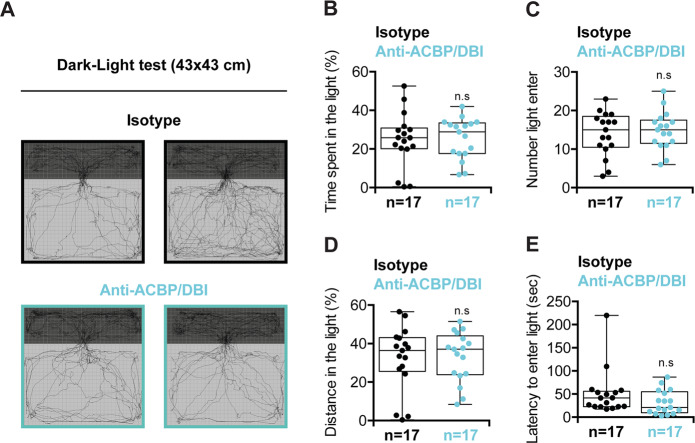
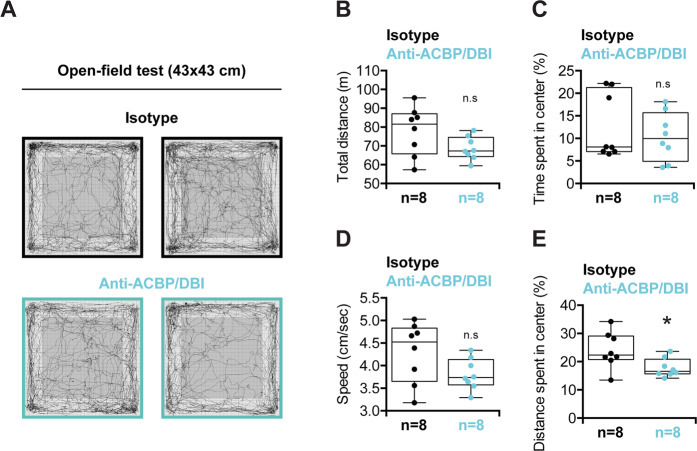
Pharmacological agents acting on GABAA receptors (which include anesthetics, barbiturates, benzodiazepines, and zolpidem) have major effects on human behavior16,27, and several appetite-inhibitory agents have been rejected or withdrawn by either the FDA or EMA (or both) due to an increase in depression and suicide28,29, prompting us to assess the behavioral effects of ACBP/DBI neutralization in mouse models. In the light–dark box test, which measures unconditioned anxiety and that accurately reflects the anxiolytic effects of benzodiazepines30,31, mice receiving the neutralizing anti-ACBP/DBI antibody exhibited a similar behavior as control mice injected with an isotype control antibody (Fig. 2). Similarly, ACBP/DBI injection had no impact on this behavioral test (Supplementary Fig. S2). The open-field test, which measures general locomotor activity levels, anxiety, and willingness to explore, is known to be sensitive to benzodiazepines32–34. ACBP/DBI neutralization had no major effects on the open-field test, except for a longer distance spent in the center of the box, suggesting a mild anxiolytic activity for the anti-ACBP/DBI antibody (Fig. 3). However, recombinant ACBP/DBI did not affect the open-field test (Supplementary Fig. S3).
Fig. 2. Dark–light test.
a Examples of trajectories during the test by untreated (isotype) (upper panels) or anti-ACBP/DBI-treated mice (lower panels). b Percentage of time spent in the light (%), c number of accesses to light, d percentage of distance travelled in the light, and e latency to enter light in seconds were measured for 10 min. Quantitative results are reported as Box and whisker plots (mean, first and third quartiles, and maximum and minimum values) (n = 17). Symbols indicate statistical (Student’s t test) comparisons with isotype control (n.s not significant).
Fig. 3. Open-field test.
a Examples of trajectories during the test by untreated (isotype) (upper panels) or anti-ACBP/DBI-treated mice (lower panels). b Total distance, c percentage of time spent in center (%), d speed, and e percentage of distance spent in center were measured during 30 min. Quantitative results are reported as Box and whisker plots (mean, first and third quartiles, and maximum and minimum values) (n = 8). Symbols indicate statistical (Student’s t test) comparisons with isotype control (n.s not significant and *p < 0.05).
Next, we took advantage of the Porsolt forced swim test (also called “behavioral despair test”) (Supplementary Fig. S4a), which is used to detect a depression-like behavior, reflected by a premature switch from swimming to immobile floating23. Benzodiazepines are well known to enhance the immobile behavior in this test in a dose-dependent fashion35,36. Of note, the anti-ACBP/DBI antibody reduced the immobile behavior of mice (Fig. 4a), while injection of recombinant ACBP/DBI protein enhanced the floating behavior (Fig. 4b), in line with the interpretation that ACBP/DBI neutralization has an antidepressant effect. Of note, the effects of ACBP/DBI on depression were lost when the protein was mutated to suppress its acyl CoA binding ability (Supplementary Fig. S4b).
Fig. 4. Immobility time in the forced swim test.
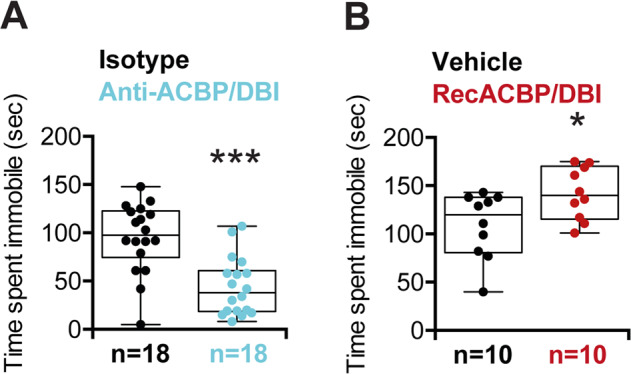
Time spent immobile in seconds after anti-ACBP/DBI (n = 18) (b) or recACBP/DBI (n = 10) (c) treatments were measured for 5 min. Quantitative results are reported as Box and whisker plots (mean, first and third quartiles, and maximum and minimum values). Symbols indicate statistical (Student’s t test) comparisons with controls (*p < 0.05 and ***p < 0.001).
Plasma ACBP/DBI levels in patients diagnosed with severe depression or schizophrenia
In the next step, we measured the circulating ACBP/DBI concentration in patients with bipolar disorder or schizophrenia. No difference in the plasma ACBP/DBI levels was detectable between depressive and schizophrenic patients (Fig. 5a, Supplementary Fig. S5a). In both groups, ACBP/DBI levels similarly correlated with the BMI, body weight or waist circumference (Supplementary Fig. S5d), as previously described for a series of patients with eating disorders including anorexia nervosa and morbid obesity2. ACBP/DBI concentrations did not correlate with subsequent weight variations, meaning that there were no significant variations in ACBP/DBI concentration between patients with minor weight oscillations (by <5), significant weight loss (≥5%) or weight gain (≥5%) within the 6 months following the ACBP/DBI measurement (Fig. 5b, Supplementary Fig. S5b).
Fig. 5. No impact of pychiatric disease or weight evolution on the correlation between ACBP/DBI plasma concentration and body mass index.
Scatter plot with regression line between ACBP/DBI (ng/mL) and body mass index (kg/m2) in bipolar and schizophrenic patients (a) and patients who lose weight (≥5%), gain weight (≥5%), or remain stable (variations < 5%) (b). Pearson’s correlation coefficient (R) and their p value are shown on top of each panel.
Nonetheless, patients with metabolic syndrome tended to exhibit a higher ACBP/DBI concentration than patients without metabolic syndrome (p = 0.097) (Fig. 6a, Supplementary Fig. S5c). However, multivariate analysis indicated that ACBP/DBI was not associated with metabolic syndrome, independently of BMI. In contrast, variations in ACBP/DBI plasma levels were associated with dyslipidemia (p = 0.003) (but not with diabetes nor arterial hypertension), and this association was independent of BMI (p = 0.055) (Fig. 6b, c).
Fig. 6. Impact of metabolic syndrome on ACBP/DBI levels.
No impact of pychiatric disease or weight evolution on the correlation between ACBP/DBI plasma concentration and body mass index. Scatter plot with regression line between ACBP/DBI (ng/mL) and body mass index (kg/m2) in patients with or without metabolic syndrome. Pearson’s correlation coefficient (R) and their p value are shown on top of each panel. Forest plots representing odds ratios for the association between ACBP/DBI (per 1ng/mL increase) and obesity, abdominal obesity, dyslipidemia, hypertension, type 2 diabetes, and metabolic syndrome in univariate analysis (b) and after adjustment for body mass index (c).
Altogether, these results suggest that ACBP/DBI levels are well correlated with BMI, irrespective of their psychiatric diagnosis, do not predict later changes in BMI, yet are associated with dyslipidemia.
Discussion
ACBP/DBI is a phylogenetically ancient protein that stimulates appetite and lipo-anabolism in animals, ranging from nematodes and insects to rodents8,12. It is also elevated in human obesity but reduced in anorexia nervosa2. For this reason, neutralization of ACBP/DBI by suitable antibodies might constitute a valid strategy for combating obesity and its co-morbidities12,37,38. Given the fact that several anorexigenic drugs have been withdrawn from the clinics due to their psychiatric side effects27,28, we evaluated the behavioral effect of ACBP/DBI and ACBP/DBI neutralizing antibodies in rodent models and attempted to establish a correlation between mental disease and circulating ACBP/DBI concentrations in psychiatric patients.
Mouse experiments detailed in this paper revealed that the orexigenic effect of systemically (i.v.) injected ACBP/DBI protein did not rely on its interaction with acyl-CoA but apparently involved an action on GABAAR, alerting about the possibility that ACBP/DBI might indeed affect GABA-regulated mood control. However, at odds with this possibility, neither the systemic (i.v.) injection of ACBP/DBI nor the systemic (i.p.) administration of a neutralizing ACBP/DBI antibody did affect the behavior of mice in the light–dark test and in the open-field tests. In contrast, ACBP/DBI injection caused a “depression-like” behavior in the forced swim test, meaning that the mice ceased active swimming and switched toward passive floating earlier than sham-injected mice. Conversely, neutralization of ACBP/DBI resulted into an “antidepressant” effect, prolonging the active combat of mice for survival. The effects of ACBP/DBI on depression depend on its acyl CoA binding ability, while induction of hyperphagy by ACBP/DBI did not require acyl CoA binding. These discrepant findings underscore that (some of) the metabolic and mood-modulating effect of ACBP/DBI can be uncoupled from each other.
Mice that are constitutively knockout for ACBP/DBI (meaning that the gene is even expressed during embryogenesis) exhibit a stereotyped self-grooming behavior, reduced social interest, but normal social recognition39, pointing to a minor behavioral phenotype. In contrast, we have not noted any evident changes in mouse behavior after the inducible knockout of ACBP/DBI in adult mice2, suggesting that these effects might be linked to neurodevelopment. Intracerebroventricular administration of recombinant ACBP/DBI or that of ACBP/DBI-derived neuropeptides induces proconflict behavior40, stimulates anxiety41, and reduces food intake42, causing a loss in bodyweight in long-term experiments43. When microinjected into the swallowing pattern generator located in the nucleus tractus solitarius, the octadecaneuropeptide derived from ACBP/DBI inhibits the swallowing reflex42. Of note, the anorexigenic effects of octadecaneuropetide do not depend on an action on TSPO or GABAAR but rather on a G protein coupled receptor44,45. Thus, the central (i.c.v.) injection of ACBP/DBI causes GABAAR-independent anorexigenic effects that are diametrically opposed to the GABAAR-dependent orexigenic effects observed after its peripheral (i.v.) administration2. Of note, it appears plausible that i.v. administered ACBP/DBI mediates its effects through an action on peripheral metabolism, causing a hypoglycemic response that then activates orexigenic neurons in the hypothalamus. Indeed, artificial maintenance of glucose concentrations by a glucose clamp prevents the activation of such orexigenic neurons as well as the hyperphagic response of mice2.
Obviously, it will be interesting to investigate the impact of ACBP/DBI on the expression of its receptors (in particular GABAAR subunits and the mitochondrial TSPO protein), the expression level of other neuroendocrine factors, as well as bioenergetic parameters in multiple different peripheral and central nervous tissue to understand the full range of its physiological effects. Thus a single-cell multi-omics approach (including but not limited to transcriptomics, proteomics and metabolomics) should be envisaged in the future to explore the effects of ACBP/DBI in further detail.
In line with the idea that the peripheral pool of ACBP/DBI has little impact on mental operations, we did not observe any difference between schizophrenic and bipolar patients with respect to their plasma ACBP/DBI concentrations, which however strongly correlated with BMI in both groups. The levels of ACBP/DBI concentrations measured at diagnosis did not allow predicting the subsequent trajectory of BMI (gain, loss, or stability) and rather correlated with the actual state of the BMI. However, a high ACBP/DBI plasma concentration constitutes a risk factor for dyslipidemia, independently from BMI, as indicated by multivariate analysis. This result strongly pleads in favor of a role of ACBP/DBI in metabolism that is more important than its putative role in mental disease.
As a final note, it appears important that ACBP/DBI neutralization, which might constitute a novel treatment for obesity and its comorbidities such as type-2 diabetes and non-alcoholic steatohepatitis, has no unwarranted (depression- or anxiety-inducing) effects on mice. This preclinical finding may facilitate the development of a novel type of antiobesity medication that targets ACBP/DBI or its interaction with peripheral GABAAR.
Supplementary information
Acknowledgements
The authors thank Maxime Perez for establishing contacts among dispersed investigators. The authors thank the CRC Core Facilities for the technical support. G.K. is supported by the Ligue contre le Cancer (équipe labellisée); Agence National de la Recherche (ANR)—Projets blancs; ANR under the frame of E-Rare-2, the ERA-Net for Research on Rare Diseases; AMMICa US23/CNRS UMS3655; Association pour la recherche sur le cancer (ARC); Association “Le Cancer du Sein, Parlons-en!”; Cancéropôle Ile-de-France; Chancelerie des universités de Paris (Legs Poix), Fondation pour la Recherche Médicale (FRM); a donation by Elior; European Research Area Network on Cardiovascular Diseases (ERA-CVD, MINOTAUR); Gustave Roussy Odyssea, the European Union Horizon 2020 Project Oncobiome; Fondation Carrefour; High-end Foreign Expert Program in China (GDW20171100085), Institut National du Cancer (INCa); Inserm (HTE); Institut Universitaire de France; LeDucq Foundation; the LabEx Immuno-Oncology (ANR-18-IDEX-0001); the RHU Torino Lumière; the Seerave Foundation; the SIRIC Stratified Oncology Cell DNA Repair and Tumor Immune Elimination (SOCRATE); and the SIRIC Cancer Research and Personalized Medicine (CARPEM). J.M.B-S.P. is supported by a Ramon y Cajal contract funded by the Spanish Government.
FACEGroups members List of FondaMental Advanced Center of Expertise (FACE-BD) collaborators
FACE-BD Clinical Coordinating Center (Fondation FondaMental); B. Etain, C. Henry, E. Olié, M. Leboyer, E. Haffen and PM Llorca; FACE-BD Data Coordinating Center (Fondation FondaMental); V. Barteau, S. Bensalem, O. Godin, H. Laouamri, and K. Souryis; FACE-BD Clinical Sites and Principal Collaborators in France; AP-HP, DHU PePSY, Pôle de Psychiatrie et d’Addictologie des Hôpitaux Universitaires H Mondor, Créteil; S. Hotier, A. Pelletier, N. Drancourt, JP. Sanchez, E. Saliou, C. Hebbache, J. Petrucci, L. Willaume and E. Bourdin; AP-HP, GH Saint-Louis–Lariboisière–Fernand Widal, Pôle Neurosciences, Paris; F. Bellivier, M. Carminati, B. Etain, J. Maruani, E. Marlinge, J. Meheust and S. Yeim; Hôpital C. Perrens, Centre Expert Trouble Bipolaire, Service de Psychiatrie Adulte, Pôle 3-4-7, Bordeaux; B. Antoniol, A. Desage, S. Gard, A. Jutant, K. Mbailara, I. Minois, and L. Zanouy; Département d’Urgence et Post Urgence Psychiatrique, CHRU Montpellier, Montpellier; C. Abettan, L. Bardin, A. Cazals, P. Courtet, B. Deffinis, D. Ducasse, M. Gachet, A. Henrion, E. Martinerie, F. Molière, B. Noisette, E. Olié and G. Tarquini; Pôle de Psychiatrie, addictologie et pédopsychiatrie, Hôpital Sainte Marguerite, Marseille; R. Belzeaux, N. Correard, F. Groppi, A. Lefrere, L. Lescalier., E. Moreau, J. Pastol, M. Rebattu, B. Roux and N. Viglianese; Service de Psychiatrie et Psychologie Clinique, CHU de Nancy, Hôpitaux de Brabois, Vandoeuvre Les Nancy; R. Cohen, Raymond Schwan, J.P. Kahn, M. Milazzo, and O. Wajsbrot-Elgrabli; Service Universitaire de Psychiatrie, CHU de Grenoble et des Alpes, Grenoble; T. Bougerol, B. Fredembach, A. Suisse, B. Halili, Z. Gaoua, and M. Polosan; Centre Hospitalier de Versailles, Service Universitaire de Psychiatrie d’adultes, Le Chesnay; A.M. Galliot, I. Grévin, A.S. Cannavo, N. Kayser, C. Passerieux, and P. Roux; Service de Psychiatrie, Centre Hospitalier Princesse Grace, Monaco; V. Aubin, I. Cussac, M.A Dupont, J. Loftus, and I. Medecin; AHPH, Departement de Psychiatrie, Hopital Louis Mourier, Colombes, France; C. Dubertret, N. Mazer, C. Portalier.
List of FondaMental Advanced Center of Expertise (FACE-SZ) collaborators
FACE-SZ Clinical Coordinating Center (Fondation FondaMental); F. Berna, E. Haffen, M. Leboyer, PM Llorca and F. Schürhoff; FACE-SZ Data Coordinating Center (Fondation FondaMental); V. Barteau, S. Bensalem, O. Godin, H. Laouamri and K. Souryis; FACE-SZ Clinical Sites and Principal Collaborators in France; AP-HP, INSERM U955, Translational Psychiatry Team, DHU Pe-PSY, Centre Expert Schizophrénie, Pôle de Psychiatrie et d’Addictologie des Hôpitaux Universitaires Henri Mondor, Paris Est University, 40 rue de Mesly, 94000 Créteil, France: N. Coulon, M. Leboyer, I. Offerlin-Meyer, B. Pignon, F. Schürhoff and A. Szöke; Department of Adult Psychiatry, Charles Perrens Hospital, F-33076 Bordeaux, France; Laboratory of Nutrition and Integrative Neurobiology (UMR INRA 1286), University of Bordeaux, France: B. Aouizerate; Department of Adult Psychiatry, Charles Perrens Hospital, F-33076 Bordeaux; University of Bordeaux, CNRS UMR 5287-INCIA, Bordeaux, France: A. Deloge, D. Misdrahi and E. Vilà; CHU Clermont-Ferrand, Department of Psychiatry (service de psychatrie B), University of Clermont Auvergne, Clermont-Ferrand, France: O. Blanc, I. Chéreau, H. Denizot, RM. Honciuc, D. Lacelle, PM. Llorca and S. Pires; AP-HP, Department of Psychiatry, Louis Mourier Hospital, Colombes, Inserm UMR1266, Institute of Psychiatry and Neurosciences of Paris, University Paris Descartes, Université Paris Diderot, Sorbonne Paris Cité, Faculté de médecine, France: C. Dubertret, J. Mallet, and C. Portalier; Psychosocial Rehabilitation Reference Center, Alpes Isère Hospital, Grenoble, France: J. Dubreucq, C. Fluttaz, F. Gabayet and C. Roman; University Claude Bernard Lyon 1, Le Vinatier Hospital Pole Est BP 300 39 - 95 bd Pinel - 69678 Bron Cedex, France: G. Chesnoy-Servanin, T. D’Amato, JM. Dorey, R. Rey and A. Vehier; Department of Psychiatry (AP-HM), Sainte-Marguerite University Hospital, Marseille, France: C. Lançon, C. Faget, E. Metairie, P. Peri and F. Vaillant; AP-HM, la Conception Hospital, Aix-Marseille Univ, School of medicine - La Timone Medical Campus, EA 3279: CEReSS - Health Service Research: L. Boyer and G. Fond; Strasbourg University Hospital, University of Strasbourg, INSERM U1114, Federation of Translational Psychiatry, Strasbourg, France: F. Berna, P. Vidailhet and A. Zinetti-Bertschy; University Department of Adult Psychiatry, La Colombiere Hospital, CHU Montpellier, University of Montpellier 1, Inserm 1061, Montpellier, France: D. Capdevielle and H. Yazbek; Department of Adult Psychiatry, Versailles Hospital, Le Chesnay, France; HandiRESP and Quality of Life Center, 27 Boulevard Jean Moulin, 13005 Marseille, France Laboratory, EA4047, UFR Health Sciences Simone Veil, Université de Versailles Saint-Quentin-En-Yvelines, Montigny-le-Bretonneux, France: S. Esselin, M. Jarroir, C. Passerieux, and M. Urbach.
Competing interests
G.K. and J.M.B.-S.P. filed a patent application dealing with targeting the ACBP/DBI system in anorexia, obesity, and co-morbidities. G.K. filed additional patent applications dealing with caloric restriction mimetics (autophagy inducers) for the treatment of aging, age-related diseases, cancer, obesity, and co-morbidities. G.K. is a scientific co-founder of Samsara Therapeutics and Therafast Bio.
Footnotes
Edited by G.M. Fimia
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Adrien Joseph, Stéphanie Moriceau
The members of consortium group are listed below the Acknowledgements section
Contributor Information
José M. Bravo-San Pedro, Email: josemabr@ucm.es
Guido Kroemer, Email: kroemer@orange.fr.
Supplementary information
Supplementary Information accompanies this paper at (10.1038/s41419-020-2716-5).
References
- 1.Tonon, M.-C. et al. Endozepines and their receptors: structure, functions and pathophysiological significance. Pharmacol. Ther.208, 107386 (2020). [DOI] [PubMed] [Google Scholar]
- 2.Bravo-San Pedro, J. M. et al. Acyl-CoA-binding protein is a lipogenic factor that triggers food intake and obesity. Cell Metab.30, 1171 (2019). [DOI] [PubMed] [Google Scholar]
- 3.Conti, E. et al. Reduced fasting plasma levels of diazepam-binding inhibitor in adolescents with anorexia nervosa. Int. J. Eat. Disord.46, 626–629 (2013). [DOI] [PubMed] [Google Scholar]
- 4.Clavier, T. et al. Increased plasma levels of endozepines, endogenous ligands of benzodiazepine receptors, during systemic inflammation: a prospective observational study. Crit. Care Lond. Engl.18, 633 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dandona, P. et al. Tumor necrosis factor-alpha in sera of obese patients: fall with weight loss. J. Clin. Endocrinol. Metab.83, 2907–2910 (1998). [DOI] [PubMed] [Google Scholar]
- 6.Hotamisligil, G. S. Inflammation, metaflammation and immunometabolic disorders. Nature542, 177–185 (2017). [DOI] [PubMed] [Google Scholar]
- 7.Manjithaya, R., Anjard, C., Loomis, W. F. & Subramani, S. Unconventional secretion of Pichia pastoris Acb1 is dependent on GRASP protein, peroxisomal functions, and autophagosome formation. J. Cell Biol.188, 537–546 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charmpilas, N. et al. Acyl-CoA-binding protein (ACBP): a phylogenetically conserved appetite stimulator. Cell Death Dis.11, 7 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anjard, C. & Loomis, W. F. Peptide signaling during terminal differentiation of Dictyostelium. Proc. Natl Acad. Sci. USA102, 7607–7611 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ryuda, M. et al. Identification of a novel gene, anorexia, regulating feeding activity via insulin signaling in Drosophila melanogaster. J. Biol. Chem.286, 38417–38426 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bravo-San Pedro, J. M., Sica, V. & Kroemer, G. The elusive ‘hunger protein’: an appetite-stimulatory factor that is overabundant in human obesity. Mol. Cell. Oncol.6, e1667193 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pedro, J. M. B.-S., Sica, V., Madeo, F. & Kroemer, G. Acyl-CoA-binding protein (ACBP): the elusive ‘hunger factor’ linking autophagy to food intake. Cell Stress3, 312–318 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henry, C. et al. Outcomes for bipolar patients assessed in the French expert center network: A 2-year follow-up observational study (FondaMental Advanced Centers of Expertise for Bipolar Disorder [FACE-BD]). Bipolar Disord. 19, 651–660 (2017). [DOI] [PubMed]
- 14.Godin, O. et al. Metabolic syndrome, abdominal obesity and hyperuricemia in schizophrenia: Results from the FACE-SZ cohort. Schizophr. Res.168, 388–394 (2015). [DOI] [PubMed] [Google Scholar]
- 15.Godin, O. et al. Metabolic syndrome and illness severity predict relapse at 1-year follow-up in schizophrenia: the FACE-SZ cohort. J. Clin. Psychiatry79, 17m12007 (2018). [DOI] [PubMed]
- 16.Rudolph, U. & Möhler, H. GABAA receptor subtypes: therapeutic potential in Down syndrome, affective disorders, schizophrenia, and autism. Annu. Rev. Pharmacol. Toxicol.54, 483–507 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Setiawan, E. et al. Role of translocator protein density, a marker of neuroinflammation, in the brain during major depressive episodes. JAMA Psychiatry72, 268–275 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marino, R. A. M. et al. Control of food approach and eating by a GABAergic projection from lateral hypothalamus to dorsal pons. Proc. Natl Acad. Sci. USA10.1073/pnas.1909340117 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhandage, A. K. et al. GABA regulates release of inflammatory cytokines from peripheral blood mononuclear cells and CD4+ T cells and is immunosuppressive in type 1 diabetes. EBioMedicine30, 283–294 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wulff, P. et al. From synapse to behavior: rapid modulation of defined neuronal types with engineered GABAA receptors. Nat. Neurosci.10, 923–929 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kragelund, B. B. et al. Conserved residues and their role in the structure, function, and stability of acyl-coenzyme A binding protein. Biochemistry38, 2386–2394 (1999). [DOI] [PubMed] [Google Scholar]
- 22.Fregeac, J. et al. Loss of the neurodevelopmental disease-associated gene miR-146a impairs neural progenitor differentiation and causes learning and memory deficits. Mol. Autism11, 22 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krishnan, V. & Nestler, E. J. Animal models of depression: molecular perspectives. Curr. Top. Behav. Neurosci.7, 121–147 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alberti, K. G. M. M., Zimmet, P. & Shaw, J. IDF Epidemiology Task Force Consensus Group The metabolic syndrome-a new worldwide definition. Lancet366, 1059–1062 (2005). [DOI] [PubMed] [Google Scholar]
- 25.Larsen, M. K., Tuck, S., Faergeman, N. J. & Knudsen, J. MAA-1, a novel acyl-CoA-binding protein involved in endosomal vesicle transport in Caenorhabditis elegans. Mol. Biol. Cell17, 4318–4329 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dumitru, I., Neitz, A., Alfonso, J. & Monyer, H. Diazepam binding inhibitor promotes stem cell expansion controlling environment-dependent neurogenesis. Neuron94, 125–137.e5 (2017). [DOI] [PubMed] [Google Scholar]
- 27.Rudolph, U. & Knoflach, F. Beyond classical benzodiazepines: novel therapeutic potential of GABAA receptor subtypes. Nat. Rev. Drug Discov.10, 685–697 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Srivastava, G. & Apovian, C. M. Current pharmacotherapy for obesity. Nat. Rev. Endocrinol.14, 12–24 (2018). [DOI] [PubMed] [Google Scholar]
- 29.Galaj, E. & Xi, Z.-X. Potential of cannabinoid receptor ligands as treatment for substance use disorders. CNS Drugs33, 1001–1030 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Belzung, C., Misslin, R., Vogel, E., Dodd, R. H. & Chapouthier, G. Anxiogenic effects of methyl-beta-carboline-3-carboxylate in a light/dark choice situation. Pharmacol. Biochem. Behav.28, 29–33 (1987). [DOI] [PubMed] [Google Scholar]
- 31.Ennaceur, A. Tests of unconditioned anxiety—pitfalls and disappointments. Physiol. Behav.135, 55–71 (2014). [DOI] [PubMed] [Google Scholar]
- 32.Engel, O. et al. Imepitoin shows benzodiazepine-like effects in models of anxiety. Front. Pharm.9, 1225 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Silva, M. T. & Calil, H. M. Screening hallucinogenic drugs: systematic study of three behavioral tests. Psychopharmacologia42, 163–171 (1975). [DOI] [PubMed] [Google Scholar]
- 34.Stanford, S. C. The Open Field Test: reinventing the wheel. J. Psychopharmacol.21, 134–135 (2007). [DOI] [PubMed] [Google Scholar]
- 35.Nagatani, T., Yamamoto, T., Sugihara, T. & Ueki, S. The effect of agonists at the GABA-benzodiazepine receptor complex on the duration of immobility of mice in the forced swimming test. Eur. J. Pharmacol.142, 17–22 (1987). [DOI] [PubMed] [Google Scholar]
- 36.Van der Meersch-Mougeot, V. et al. Benzodiazepines reverse the anti-immobility effect of antidepressants in the forced swimming test in mice. Neuropharmacology32, 439–446 (1993). [DOI] [PubMed] [Google Scholar]
- 37.Sica, V., Martins, I., Motiño, O., Bravo-San Pedro, J. M. & Kroemer, G. Antibody-mediated neutralization of ACBP/DBI has anorexigenic and lipolytic effects. Adipocyte9, 116–119 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kobayashi, H., Maeda, M., Hayata, T. & Kawashima, Y. Clinical study of combination chemotherapy with CDDP, ADM and CPM for ovarian cancer. Nihon Gan Chiryo Gakkai Shi23, 829–836 (1988). [PubMed] [Google Scholar]
- 39.Ujjainwala, A. L., Courtney, C. D., Rhoads, S. G., Rhodes, J. S. & Christian, C. A. Genetic loss of diazepam binding inhibitor in mice impairs social interest. Genes Brain Behav.17, e12442 (2018). [DOI] [PubMed] [Google Scholar]
- 40.Guidotti, A. et al. Isolation, characterization, and purification to homogeneity of an endogenous polypeptide with agonistic action on benzodiazepine receptors. Proc. Natl Acad. Sci. USA80, 3531–3535 (1983). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.De Mateos-Verchere, J. G., Leprince, J., Tonon, M. C., Vaudry, H. & Costentin, J. The octadecaneuropeptide ODN induces anxiety in rodents: possible involvement of a shorter biologically active fragment. Peptides19, 841–848 (1998). [DOI] [PubMed] [Google Scholar]
- 42.Cavaillon, J. M. & Haeffner-Cavaillon, N. The role of serum in interleukin 1 production by human monocytes activated by endotoxins and their polysaccharide moieties. Immunol. Lett.10, 35–41 (1985). [DOI] [PubMed] [Google Scholar]
- 43.de Mateos-Verchere, J. G., Leprince, J., Tonon, M. C., Vaudry, H. & Costentin, J. The octadecaneuropeptide [diazepam-binding inhibitor (33-50)] exerts potent anorexigenic effects in rodents. Eur. J. Pharmacol. 414, 225–231 (2001). [DOI] [PubMed]
- 44.do Rego, J.-C. et al. Pharmacological characterization of the receptor mediating the anorexigenic action of the octadecaneuropeptide: evidence for an endozepinergic tone regulating food intake. Neuropsychopharmacology32, 1641–1648 (2007). [DOI] [PubMed] [Google Scholar]
- 45.Matsuda, K. et al. Effect of the diazepam-binding inhibitor-derived peptide, octadecaneuropeptide, on food intake in goldfish. Neuroscience150, 425–432 (2007). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.