Abstract
Introduction:
The aims of this study were to investigate (1) whether demographic factors would be risk factors for severe proximal humerus fracture (PHF), (2) relationship of radiological parameters with bone mineral density (BMD), deltoid tuberosity index (DTI), or severe PHF, and (3) correlation between DTI and BMD.
Methods:
We conducted a cross-sectional study based on radiographs and medical records taken during admission or the visit to the orthopedic clinic. We reviewed consecutive 100 adult patients who were diagnosed with PHF in our hospital from March 2014 to December 2016. Three- and 4-part fractures were regarded as severe PHFs. Univariable and multivariable logistic regression analyses were performed to evaluate risk factors for severe PHF. Also, we investigated the correlation between BMD and DTI using the additional BMD data of the patients who underwent shoulder surgeries.
Results:
This study included 62 nonsevere PHFs and 38 severe PHFs. There were 30 male and 70 female patients with a mean age of 66.4 ± 16.4 years. Mean T score of BMD was −2.5 ± 0.9 at the time of injury. Logistic regression analyses showed that age (odds ratio: 1.044, range: 1.011-1.079, P = .009) and sex (odds ratio of females: 3.763, range: 1.236-11.459, P = .020) were related to severe PHF. The group satisfying the radiological parameter criteria had significantly higher rates of severe PHF. The correlation coefficient (r) between DTI and T score was 0.555 (P < .001).
Discussion and Conclusion:
Older age and female were the independent risk factors for severe PHF. Conversely, BMD and other medical comorbidities were not risk factors for severe PHF. Deltoid tuberosity index showed significantly high intraclass correlation coefficient and a strong correlation with the T score of BMD. Therefore, DTI may be useful for screening osteoporosis in PHF patients.
Level of Evidence:
Level IV, Cross-sectional study.
Keywords: risk factor, humerus fracture, bone mineral density, classification, deltoid tuberosity index
Introduction
With an increase in life expectancy, the incidence of osteoporotic fractures has also increased. Typical osteoporotic fractures are hip fractures, compression fractures of the thoracic and lumbar spines, and distal radius fractures.1 Fixation surgery for osteoporotic fractures tends to result in weak fixation of the screw and slow or uncertain fusion of the fractures. Therefore, more careful treatment and procedure selection are required for osteoporotic fractures than for fractures with normal bone density. Recently, proximal humerus fracture (PHF) has been recognized as a major osteoporotic fracture.2-5 Studies on the relationship with osteoporosis drugs6 and optimal treatment methods are actively conducted.7-10 Predicting and determining the severity of the fracture is important when selecting the treatment method and for prognosis prediction. Finding out whether demographic characteristics, bone mineral density (BMD), and local bone density measurements are related to the fracture severity may help in determining the optimal treatment of PHF.
Bone mineral density is commonly measured by dual-energy X-ray absorptiometry (DXA) and is widely used to represent the patient’s overall bone condition.11 Conversely, deltoid tuberosity index (DTI) is often used to measure the local bone density of PHF.12 Although such a local bone density measurement better reflects the osteoporosis of the proximal humerus, the relationship between local bone density and BMD remains unclear. Therefore, we performed this study to investigate (1) correlation between DTI and BMD, (2) whether demographic factors would be risk factors for severe PHF, and (3) relationship of radiological parameters with BMD, DTI, or severe PHF. We hypothesized that the DTI would be correlated with BMD and that old age, BMD, local bone density, and other demographic factors would be risk factors for severe PHF.
Methods
This study has been approved by the appropriate institutional review board (IRB number: ISPAIK 2016-10-020). All procedures performed in the study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Patients
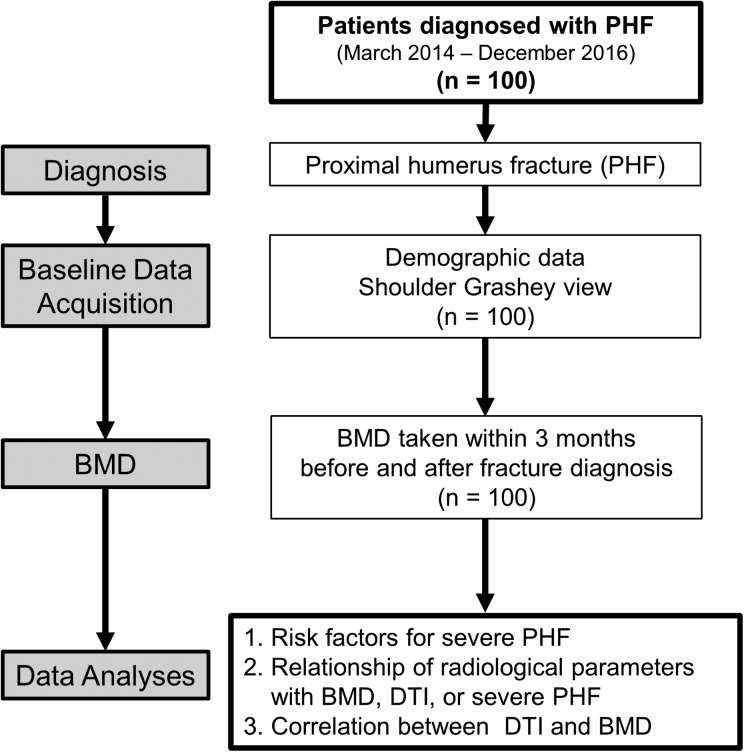
We conducted a cross-sectional study based on radiographs and medical records taken during admission or the visit to the orthopedic clinic. We reviewed consecutive 100 adult patients who were diagnosed with PHF in our hospital from March 2014 to December 2016. The exclusion criteria were (1) history of fracture at the same site, (2) history of operation near the fracture, (3) patients who did not have key information such as radiological or demographic data. Dual-energy X-ray absorptiometry was routinely taken in PHF patients who did not have DXA test within 3 months. Figure 1 shows the overall design of the current study.
Figure 1.
Overall design of the current study.
Demographic and Clinical Data Acquisition
We gained information about demographic items by examining the patient’s medical records included in this study: age, sex, weight, height, BMI, treatment for PHF, history of diseases and medications, and history of fractures. We gained BMD data (hip, spine, and total T scores) from DXA taken within 3 months before and after fracture diagnosis. Because of the wide variety of medical disease histories, the Charlson comorbidity index (CCI) and age-adjusted CCI were used to assess the degree of comorbidities comprehensively.13-15
Radiographic Analysis
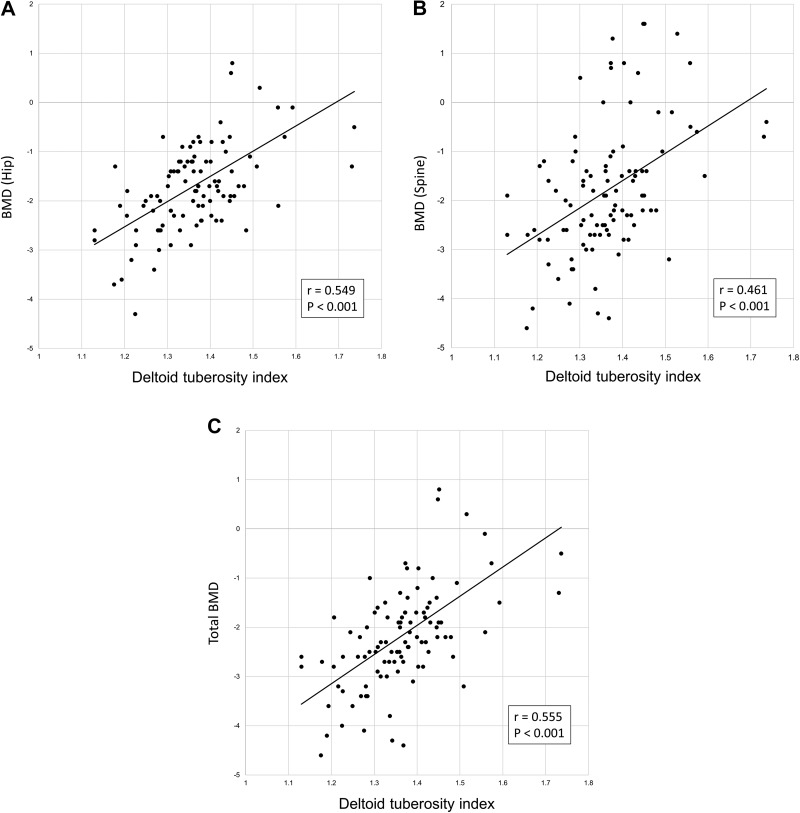
The Neer classification and Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association classification are used for PHF.16-18 We used the easy and widely used Neer classification, based on plain radiographs and additional computed tomography, in this study. The DTI and 5 parameters that showed the fracture pattern of PHF through a true anteroposterior view were evaluated. Three- and 4-part fractures, according to the Neer classification, were regarded as severe PHFs, and 1- and 2-part fractures were regarded as nonsevere PHFs. The DTI was measured in the upper end of the deltoid tuberosity where the outer cortical borders were parallel. The ratio of the outer cortical diameter to the inner cortical diameter was defined as the DTI value at the site (Figure 2).12
Figure 2.
Deltoid tuberosity index.
The 5 radiographic parameters designed to represent the appearance of the PHF are as follows: calcar comminution, metaphyseal extension, medial hinge disruption, shaft displacement, and displacement of the greater tuberosity (GT). We determined that there is calcar comminution if there is at least one intermediate fragment in the medial curvature of the lower part of the anatomical neck, as suggested by Osterhoff et al.19 We checked whether the metaphyseal extension was less than 8 mm and the medial hinge disruption was more than 2 mm.20-22 We also measured whether the head-diaphysis contact was less than 50% (displacement of shaft) and the displacement of GT was 10 mm or more on the coronal plane.23
Statistical Analysis
First, we performed univariable and multivariable logistic regression analyses to determine which variables were independent risk factors. The model derived from the logistic regression analysis was tested using the Hosmer-Lemeshow test. Second, we performed χ2 test, Fisher exact test, and Student t test to investigate the difference in PHF severity, BMD, and the DTI between the groups that met the criteria for each radiological parameter and those that did not. Third, to determine the correlation between the DTI and BMD, correlation coefficients and P values between the DTI and T score (hip, spine, and total) were obtained through correlation analysis. Moreover, an untrained medical doctor was trained to measure the DTI, and then the intraclass correlation coefficient (ICC) was analyzed to assess the consistency of the measurements. All statistical analyses were performed using SPSS v.16.0 (SPSS Inc), and a P value of less than .05 was considered statistically significant.
Results
Demographic and Radiographic Analysis
A total of 100 PHF patients were included in this study. There were 30 men and 70 women, and the mean age was 66.4 ± 16.4 (19-91) years. There were 62 nonsevere PHFs (9 one-part and 53 two-part fractures) and 38 severe PHFs (27 three-part and 11 four-part fractures), according to the Neer classification. Table 1 summarizes the demographic data and radiographic analysis of all patients. Mean DTI was 1.38 ± 0.13 (1.13-1.74).
Table 1.
Demographic and Radiographic Analyses.
| Items | Outcome |
|---|---|
| Mean age (years) (±SD) | 66.4 ± 16.4 |
| Younger than 50 | 17 |
| 50-59 | 14 |
| 60-69 | 14 |
| 70-79 | 36 |
| 80 or older | 19 |
| Sex (M/F) | 30/70 |
| Mean BMI (±SD) | 23.2 ± 3.5 |
| Mean BMD (hip, ±SD) | −1.9 ± 0.9 |
| Mean BMD (spine, ±SD) | −2.3 ± 1.0 |
| Mean BMD (total, ±SD) | −2.5 ± 0.9 |
| Normal | 1 (2.6%) |
| Osteopenia | 17 (44.7%) |
| Osteoporosis | 20 (52.6%) |
| History of hip fractures | 9 |
| History of spine fractures | 5 |
| Charlson comorbidity index | 1.0 ± 1.3 |
| Age-adjusted CCI | 3.3 ± 2.2 |
| History of osteoporosis medication (%) | 10 |
| Mean DTI (±SD) | 1.38 ± 0.13 |
| Metaphyseal comminution | Present: 41 Absent: 59 |
| Metaphyseal extension (>8 mm) | Present: 41 Absent: 59 |
| Medial hinge disruption (>2 mm) | Present: 56 Absent: 44 |
| Displacement of shaft | Present: 21 Absent: 79 |
| Displacement of GT | Present: 44 Absent: 56 |
Abbreviations: BMI, bone mass index; CCI, Charlson comorbidity index; DTI, deltoid tuberosity index; F, female; GT, greater tuberosity; M, male; SD, standard deviation.
Risk Factors for Severe PHF
The univariable analysis showed differences in age and sex, but no difference in other major items such as CCI and DTI between severe and nonsevere PHF groups (Table 2). A multivariable logistic regression analysis was performed on variables with P values <.25. Multivariable regression analysis showed that age (odds ratio: 1.044, range 1.011-1.079, P = .009) and female sex (odds ratio of female: 3.763, range 1.236-11.459, P = .020) were independent risk factors for severe PHF. The same trend was also observed when the age variable was converted into a categorical variable and applied to the additional multivariable logistic regression analysis. Patients aged 70 to 79 years old and those older than 80 years had significantly higher odds ratios than those younger than 50 years (19.982 [1.419-281.284] and 24.639 [1.053-576.672], respectively). If age was considered a continuous variable, the probability of severe PHF increased by 1.044 times as age increased by one year. Moreover, the probability of severe PHF in women is 3.763 times higher than in men. The P value of the Hosmer-Lemeshow test for multivariable analysis was .708 showing that the model of multivariable analysis was appropriate.
Table 2.
Univariable and Multivariable Logistic Regression Analyses Evaluating Risk Factors for Severe Proximal Humerus Fracture.
| Variable | Univariable analysis | Multivariable logistic regression analysis | Odds ratio (95% CI) |
|---|---|---|---|
| Sex | 0.004 | 0.020a | 3.763 (1.236-11.459) |
| Age (continuous variable) | 0.001 | 0.009a | 1.044 (1.011-1.079) |
| Age (categorical variable) | 0.021 | ||
| Younger than 50 | 1 | ||
| 50-59 | 0.056 | 10.459 (0.946-115.616) | |
| 60-69 | 0.072 | 9.980 (0.816-122.115) | |
| 70-79 | 0.026a | 19.982 (1.419-281.284) | |
| 80 or older | 0.046a | 24.639 (1.053-576.672) | |
| History of hip fracture | 0.216 | 0.293 | NA |
| History of spine fracture | 0.632 | NA | |
| History of osteoporosis medication | 0.410 | NA | |
| BMI | 0.136 | 0.410 | NA |
| BMD (Hip) | 0.488 | NA | |
| BMD (Spine) | 0.714 | NA | |
| BMD (Total) | 0.480 | NA | |
| DTI (continuous variable) | 0.316 | NA | |
| DTI (categorical variable) - DTI < 1.4 - DTI ≥ 1.4 |
0.305 | NA | |
| CCI | 0.922 | NA | |
| Age-adjusted CCI | 0.073 | 0.284 | NA |
| Hosmer-Lemeshow test | P = .708 |
Abbreviations: BMD, bone mineral density; BMI, bone mass index; CCI, Charlson comorbidity index; CI, confidence interval; DTI, deltoid tuberosity index; NA, not applicable.
a Statistically significant.
Differences in BMD, DTI, and Fracture Severity According to the Radiographic Parameters
Table 3 summarizes the results of BMD, DTI, and fracture severity according to PHF-related radiographic parameters. There was no significant difference in BMD between the groups that met the parameter criteria and those that did not. Similarly, no difference in DTI between the groups was seen. On the other hand, all groups satisfying the criteria were found to have a significantly higher percentage of severe PHF (P < .001).
Table 3.
Comparison Between the Groups That Met the Parameter Criteria and Those That Did Not.
| Parameter | BMD | P value | DTI | P value | Severity | P value | |
|---|---|---|---|---|---|---|---|
| Severe | Nonsevere | ||||||
| Metaphyseal comminution | .267 | .561 | <.001a | ||||
| Yes | −2.74 ± 0.9 | 1.40 ± 0.14 | 26 | 15 | |||
| No | −2.40 ± 0.9 | 1.38 ± 0.13 | 12 | 47 | |||
| Metaphyseal extension (>8 mm) | .574 | .750 | <.001a | ||||
| Yes | −2.62 ± 1.0 | 1.38 ± 0.13 | 28 | 13 | |||
| No | −2.46 ± 0.8 | 1.39 ± 0.13 | 10 | 49 | |||
| Medial hinge disruption (>2 mm) | .169 | .660 | <.001a | ||||
| Yes | −2.68 ± 0.9 | 1.38 ± 0.14 | 32 | 5 | |||
| No | −2.23 ± 0.8 | 1.39 ± 0.11 | 6 | 57 | |||
| Displacement of shaft (Head-diaphysis contact <50%) | .494 | .054 | <.001a | ||||
| Yes | −2.33 ± 1.0 | 1.44 ± 0.16 | 16 | 10 | |||
| No | −2.59 ± 0.9 | 1.37 ± 0.12 | 22 | 18 | |||
| Displacement of GT (>10 mm) | .616 | .837 | <.001a | ||||
| Yes | −2.46 ± 0.8 | 1.38 ± 0.13 | 33 | 11 | |||
| No | −2.61 ± 1.0 | 1.39 ± 0.13 | 5 | 51 | |||
Abbreviations: BMD, bone mineral density; DTI, deltoid tuberosity index; GT, greater tuberosity.
a Statistically significant.
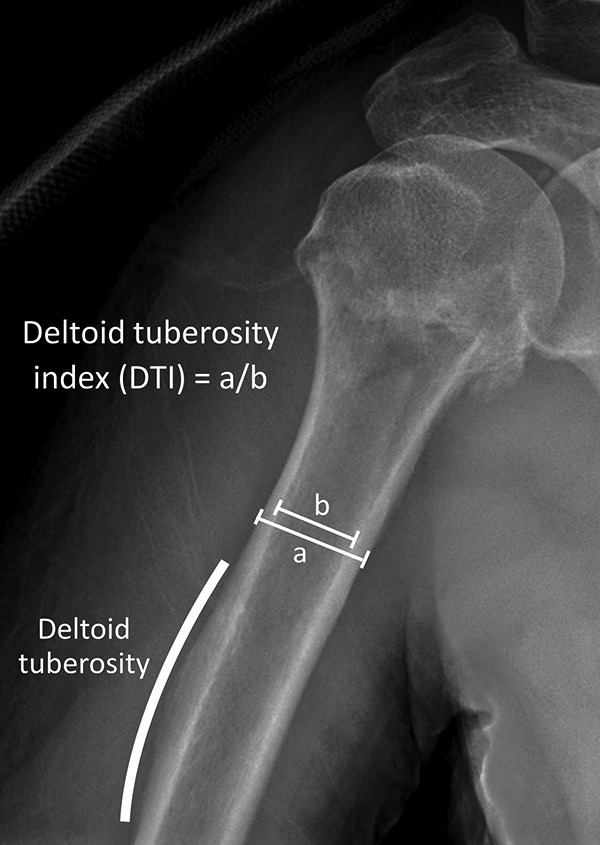
Correlation Between BMD and Local Bone Density Represented by the DTI
We analyzed the data from 100 patients. We conducted a correlation analysis to analyze the relationship between DTI and BMD (Figure 3). Deltoid tuberosity index was significantly correlated with the hip (r = 0.549, P < .001), spine (r = 0.461, P = .019), and total (r = 0.555, P < .001) T scores. Hip BMD and total BMD were correlated with DTI more than spine BMD. The ICC for the DTI measurements was 0.81 (0.74-0.86, P < .001), and the correlation coefficient was 0.69.
Figure 3.
Correlation between DTI and hip BMD (A) correlation between DTI and spine BMD (B) correlation between DTI and total BMD (C). BMD indicates bone mineral density; DTI, deltoid tuberosity index.
Discussion
The strong correlation between the DTI and BMD is likely to be applicable to clinical practice and may be useful to predict systemic osteoporosis. A low DTI and local osteoporosis should indicate systemic osteoporosis. Therefore, it is necessary to recommend BMD assessment to patients with low DTI and local osteoporosis. Several studies have shown that osteoporosis management has not been effectively implemented even after osteoporotic fractures.24,25 Thus, as proper management can prevent osteoporotic fractures, the DTI can help screen for osteoporosis.
In this study, independent risk factors of severe PHF were age (old age) and sex (female). The results showed that the probability of severe PHF increases by 1.044 times as age increases by one year and that the probability of severe PHF in women is 3.763 times higher than in men. Since the response to trauma would be slower and weaker in older age population,26 severe fractures may have occurred due to poor shock absorption. No clear cause has been identified to explain that women are a risk factor for PHF. However, the possible causes we suggest are as follows: (1) poor shock absorption, and (2) hormonal action. Further research is needed to determine the clear cause of this finding.
Conversely, our study’s hypothesis that BMD and local bone density would be risk factors for severe PHF was rejected. Bone mineral density and the DTI were not related to severity using the Neer classification. This finding is in contrast to the general concept that if the bone is weak, the fracture will be severe. Weak bones may act only as one of the multiple factors causing severe fractures. There is a possibility that the adaptation to trauma is a more important factor for severe fracture like that seen in an older woman.
A previous study by Spross et al compared DTI with local BMD measured on the peripheral quantitative computed tomography (pQCT). It reported that DTI was strongly correlated with local BMD measured by pQCT (r = 0.90; 0.63-0.90; P < .001).12 On the other hand, we compared DTI with BMD of hip and spine for assessing the possibility of using DTI as a screening test for general osteoporosis. Also, we applied DTI and BMD to the factor analyses and compared them with several radiologic parameters. In short, a comprehensive analysis of PHF and osteoporosis was performed. These points are the advantages of this study. Handa et al evaluated the correlation between 3 methods for proximal humerus on a plain radiograph and BMD. Although they reported the strong correlations, they did not analyze the factor analyses.27 Mazzucchelli et al reported that valgus impaction was significantly correlated with high DTI (≥1.4, P = .047). They included only several fracture types to the main analyses.28
Although our results indicate that BMD and DTI are not significant risk factors for severity, great care should be taken when severe osteoporosis is involved during open reduction and internal fixation for PHF. If osteoporosis is severe, despite the 2-part fracture, fracture fixation is often weak and unstable, which can lead to severe complications such as fixation failure and nonunion. It is often necessary to supplement with autologous bone graft or allograft due to severe trabecular bone loss.9 In such cases, osteoporosis medication is also recommended. There has been a debate about whether fracture patients may take bisphosphonate. However, recent articles suggest that taking bisphosphonate after fracture does not significantly affect fracture healing.6,29 Although there has been a debate on whether the anabolic agent such as teriparatide enhances fracture healing,30,31 the most recent studies suggesting that anabolic agents enhance fracture healing have been reported.32-34 Therefore, anabolic agents should be considered to patients with severe osteoporosis who are more likely to develop nonunion.
In recent years, elderly patients with severe PHF tend to undergo reverse total shoulder arthroplasty (rTSA). Although rTSA is sometimes problematic in that there is no additional treatment option available for reoperation in the event of failure, many good results have been reported with the development of instruments and techniques.35,36 The most significant advantage of rTSA in PHF is that it can solve all the problems of the patient in one operation. In addition, immediate shoulder rehabilitation can be performed after rTSA surgery, which will continue to be a promising treatment option. The pattern and severity of the PHF should be properly analyzed using Neer classification and various parameters. Reverse total shoulder arthroplasty should be actively considered for elderly patients with severe PHF and osteoporosis.
We defined 3- or 4-part fracture as severe PHF. There were no articles that provided clear reasons and criteria for diagnosing a severe PHF. We reviewed various articles and found that many of the articles mentioning severe PHF were based on the Neer classification.37-40 Many 1- or 2-part fractures were treated conservatively. Even with surgical treatment, fixation is easy and robust. Conversely, 3- and 4-part fractures are mainly treated surgically. Arthroplasty is also considered in the elderly because stable fixation is often difficult. Therefore, all authors agreed that 3- and 4-part fractures should be considered as severe fractures. Considering the result that BMD and the DTI were not related to the severity by Neer classification, whether Neer classification truly reflects fracture severity is debatable.
Our study has several limitations. First, this was a retrospective cross-sectional study. Thus, prospective parameter selection was not possible, and the data types were limited. A further prospective study is needed. Second, the sample size of our study was not large. Nevertheless, we derived statistically significant risk factors and correlation between DTI and BMD. Third, this study did not figure out the causes of the results. Further studies are needed to investigate the causes. Ultimately, big data or multicenter studies are required to conduct studies with a large number of patients on the relationship between PHF and osteoporosis.
Conclusion
Age (older age) and sex (female) were the independent risk factors for severe PHF. Conversely, BMD and other medical comorbidities were not risk factors for severe PHF. Five radiologic parameters (metaphyseal comminution, metaphyseal extension, medial hinge disruption, displacement of shaft, and displacement of GT) were strongly correlated with severe PHF. In the main analysis, DTI was significantly correlated with the T score of BMD, and the ICC of DTI was significantly high. Therefore, DTI may be useful for screening osteoporosis in PHF patients.
Footnotes
Authors’ Note: Dong Min Kim is now not affiliated with Department of Orthopedic Surgery, Kangnam Korea Hospital, Seoul, South Korea.
The data files are stored by Asan Medical Center, Seoul, South Korea, on a server dedicated to research and with security according to South Korean national rules. The data are available on request by the author, but restrictions apply to the availability of these data according to South Korean law and are therefore not publicly available. All procedures performed in the study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards (IRB number ISPAIK 2016-10-020). Formal consent is not required for this type of study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Asan Institute for Life Sciences, Asan Medical Center, Seoul, Korea (No. 2019OM-0118). No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ORCID iD: Kyoung Hwan Koh, MD, PhD  https://orcid.org/0000-0002-6181-9621
https://orcid.org/0000-0002-6181-9621
References
- 1. Meltzer M, Lessig HJ, Siegel JA. Bone mineral density and fracture in postmenopausal women. Calcif Tissue Int. 1989;45(3):142–145. [DOI] [PubMed] [Google Scholar]
- 2. Yoo JH, Moon SH, Ha YC, et al. Osteoporotic fracture: 2015 position statement of the Korean society for bone and mineral research. J Bone Metab. 2015;22(4):175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Launonen AP, Lepola V, Saranko A, Flinkkila T, Laitinen M, Mattila VM. Epidemiology of proximal humerus fractures. Arch Osteoporos. 2015;10:209. [DOI] [PubMed] [Google Scholar]
- 4. Sakuma M, Endo N, Oinuma T, et al. Incidence and outcome of osteoporotic fractures in 2004 in Sado City, Niigata Prefecture, Japan. J Bone Miner Metab. 2008;26(4):373–378. [DOI] [PubMed] [Google Scholar]
- 5. Schuit SC, van der Klift M, Weel AE, et al. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam study. Bone. 2004;34(1):195–202. [DOI] [PubMed] [Google Scholar]
- 6. Seo JB, Yoo JS, Ryu JW, Yu KW. Influence of early bisphosphonate administration for fracture healing in patients with osteoporotic proximal humerus fractures. Clin Orthop Surg. 2016;8(4):437–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen H, Zhou Q, Liu J. Combination of locking plate and anti-osteoporosis drug for the treatment of senior osteoporotic proximal humeral fractures. Pak J Pharm Sci. 2017;30(3(special)):1129–1132. [PubMed] [Google Scholar]
- 8. Schumaier A, Grawe B. Proximal humerus fractures: evaluation and management in the elderly patient. Geriatr Orthop Surg Rehabil. 2018;9:2151458517750516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stone MA, Namdari S. Surgical considerations in the treatment of osteoporotic proximal humerus fractures. Orthop Clin North Am. 2019;50(2):223–231. [DOI] [PubMed] [Google Scholar]
- 10. Jae-Kwang Y, Min-Kyu S, Chi-Woon H. Internal fixation with a locking T-plate for proximal humeral fractures in patients aged 65 years and older. Clin Shoulder Elbow. 2017;20(4):217–221. [Google Scholar]
- 11. Lorente Ramos RM, Azpeitia Arman J, Arevalo Galeano N, Munoz Hernandez A, Garcia Gomez JM, Gredilla Molinero J. Dual energy X-ray absorptimetry: fundamentals, methodology, and clinical applications. Radiologia. 2012;54(5):410–423. [DOI] [PubMed] [Google Scholar]
- 12. Spross C, Kaestle N, Benninger E, et al. Deltoid tuberosity index: a simple radiographic tool to assess local bone quality in proximal Humerus fractures. Clin Orthop Relat Res. 2015;473(9):3038–3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 14. Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–682. [DOI] [PubMed] [Google Scholar]
- 15. Huang YQ, Gou R, Diao YS, et al. Charlson comorbidity index helps predict the risk of mortality for patients with type 2 diabetic nephropathy. J Zhejiang Univ Sci B. 2014;15(1):58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium—2018. J Orthop Trauma. 2018;32(suppl 1):S1–S170. [DOI] [PubMed] [Google Scholar]
- 17. Kristiansen B, Andersen UL, Olsen CA, Varmarken JE. The Neer classification of fractures of the proximal humerus. an assessment of interobserver variation. Skeletal Radiol. 1988;17(6):420–422. [DOI] [PubMed] [Google Scholar]
- 18. Neer CS., II Displaced proximal humeral fractures. I. classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–1089. [PubMed] [Google Scholar]
- 19. Osterhoff G, Hoch A, Wanner GA, Simmen HP, Werner CM. Calcar comminution as prognostic factor of clinical outcome after locking plate fixation of proximal humeral fractures. Injury. 2012;43(10):1651–1656. [DOI] [PubMed] [Google Scholar]
- 20. Laux CJ, Grubhofer F, Werner CML, Simmen HP, Osterhoff G. Current concepts in locking plate fixation of proximal humerus fractures. J Orthop Surg Res. 2017;12(1):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42(11):1283–1288. [DOI] [PubMed] [Google Scholar]
- 22. Spross C, Zeledon R, Zdravkovic V, Jost B. How bone quality may influence intraoperative and early postoperative problems after angular stable open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2017;26(9):1566–1572. [DOI] [PubMed] [Google Scholar]
- 23. Gracitelli MEC, Dotta TAG, Assuncao JH, et al. Intraobserver and interobserver agreement in the classification and treatment of proximal humeral fractures. J Shoulder Elbow Surg. 2017;26(6):1097–1102. [DOI] [PubMed] [Google Scholar]
- 24. Kiebzak GM, Beinart GA, Perser K, Ambrose CG, Siff SJ, Heggeness MH. Undertreatment of osteoporosis in men with hip fracture. Arch Int Med. 2002;162(19):2217–2222. [DOI] [PubMed] [Google Scholar]
- 25. Lagari VS, Al-Yatama F, Rodriguez G, Berger HR, Levis S. Under-recognition of fractures as osteoporosis indicators. Geriatrics (Basel). 2019;4(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ahn HC, Seo JY, Chung JB, et al. Clinical review in geriatric trauma patients. J Korean Soc Emerg Med. 2002;13(1):49–54. [Google Scholar]
- 27. Handa A, Uchiyama Y, Shinpuku E, Watanabe M. Comparison of three plain radiography methods for evaluating proximal humerus bone strength in women. J Orthop Sci. 2019;24(2):243–249. [DOI] [PubMed] [Google Scholar]
- 28. Mazzucchelli RA, Jenny K, Zdravkovic V, Erhardt JB, Jost B, Spross C. The influence of local bone quality on fracture pattern in proximal humerus fractures. Injury. 2018;49(2):359–363. [DOI] [PubMed] [Google Scholar]
- 29. Duckworth AD, McQueen MM, Tuck CE, et al. Effect of alendronic acid on fracture healing: a multicenter randomized placebo-controlled trial. J Bone Miner Res. 2019;34(6):1025–1032. [DOI] [PubMed] [Google Scholar]
- 30. Bhandari M, Jin L, See K, et al. Does teriparatide improve femoral neck fracture healing: results from a randomized placebo-controlled trial. Clin Orthop Relat Res. 2016;474(5):1234–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shi Z, Zhou H, Pan B, et al. Effectiveness of teriparatide on fracture healing: a systematic review and meta-analysis. PLoS One. 2016;11(12):e0168691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Khan AZ, Rames RD, Miller AN. Clinical management of osteoporotic fractures. Curr Osteoporos Rep. 2018;16(3):299–311. [DOI] [PubMed] [Google Scholar]
- 33. Min HK, Ahn JH, Ha KY, et al. Effects of anti-osteoporosis medications on radiological and clinical results after acute osteoporotic spinal fractures: a retrospective analysis of prospectively designed study. Osteoporos Int. 2019;30(11):2249–2256. [DOI] [PubMed] [Google Scholar]
- 34. Shin WC, Moon NH, Jang JH, Seo HU, Suh KT. A retrospective bicenter comparative study of surgical outcomes of atypical femoral fracture: potential effect of teriparatide on fracture healing and callus formation. Bone. 2019;128:115033. [DOI] [PubMed] [Google Scholar]
- 35. Longo UG, Petrillo S, Berton A, Denaro V. Reverse total shoulder arthroplasty for the management of fractures of the proximal humerus: a systematic review. Musculoskelet Surg. 2016;100(2):83–91. [DOI] [PubMed] [Google Scholar]
- 36. Dillon MT, Prentice HA, Burfeind WE, Chan PH, Navarro RA. The increasing role of reverse total shoulder arthroplasty in the treatment of proximal humerus fractures. Injury. 2019;50(3):676–680. [DOI] [PubMed] [Google Scholar]
- 37. Andres-Cano P, Galan A, Arenas J, Del Aguila B, Guerado E. Results of uncemented hemiarthroplasty as primary treatment of severe proximal humerus fractures in the elderly. Eur J Orthop Surg Traumatol. 2015;25(2):273–280. [DOI] [PubMed] [Google Scholar]
- 38. Miyazaki AN, Fregoneze M, Santos PD, et al. Results of open reduction and internal fixation of severe fractures of the proximal humerus in elderly patients. Rev Bras Ortop. 2014;49(1):25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wang X, Shao J, Yang X, Li H, Liu F, Bi B. Treatment of severe displaced proximal humeral fractures with titanium elastic nails in older children [in Chinese]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28(3):345–348. [PubMed] [Google Scholar]
- 40. Zhao B, Ran X, Zhang MH, Jiang DM, He C. Self-made Kirschner wire hook for the treatment of severe displaced proximal humeral fractures in children [in Chinese]. Zhongguo Gu Shang. 2014;27(7):579–582. [PubMed] [Google Scholar]