Abstract
Male sexual dysfunctions (MSDs) often remain undiagnosed and untreated in Asia compared to Europe due to conservative cultural and religious beliefs, socioeconomic conditions, and lack of awareness. There is a tendency for the use of traditional medicines and noncompliance with and reduced access to modern healthcare. The present systematic review compared the incidence and factors of MSD in European and Asian populations. English language population/community-based original articles on MSDs published in MEDLINE from 2008 to 2018 were retrieved. A total of 5392 studies were retrieved, of which 50 (25 Asian and 25 European) were finally included in this review. The prevalence of erectile dysfunction (ED) (0%–95.0% vs. 0.9%–88.8%), low satisfaction (3.2%–37.6% vs. 4.1%–28.3%), and hypoactive sexual desire disorder (HSDD) (0.7%–81.4 vs. 0%–65.5%) was higher in Asian than in European men, whereas the prevalence of anorgasmia (0.4% vs. 3%–65%) was lower in Asian than in European men. Age was an independent positive factor of MSD. In European men over 60 years old, the prevalence of premature ejaculation (PE) decreased. The prevalence of MSD was higher in questionnaires than in interviews. The significant factors were age, single status, low socioeconomic status, poor general health, less physical activity, cardiovascular diseases, diabetes, obesity, lower urinary tract symptoms, prostatitis, anxiety, depression and alcohol, tobacco, and drug use. The prevalence of MSD differed slightly in Asian and European men. There is a need to conduct large studies on the various Asian populations for the effective management of MSD.
Keywords: sexual dysfunction, erectile dysfunction, premature ejaculation, Asian region, European region
Male sexual dysfunction (MSD) generally entails an alteration in at least one of the basic sexual functions (desire, erection, orgasm, and ejaculation). The most common MSD-related complaints are hypoactive sexual desire disorder (HSDD), erectile dysfunction (ED), anorgasmia or difficulties in reaching orgasm, and premature or delayed ejaculation (Wylie & Kenney, 2010). MSD may also involve pain during sexual activities and dissatisfaction with sexual life (Ni Lochlainn & Kenny, 2013).
Erectile dysfunction is a consistent or recurrent inability to attain and/or maintain penile erection sufficient for sexual activity (Mola, 2015). Ejaculation dysfunction involves anejaculation, retrograde ejaculation, premature ejaculation (PE), or delayed ejaculation (DE). Anejaculation and retrograde ejaculation (ejaculation back to the urinary bladder) are symptomatically similar due to the absence of fluid ejaculation during orgasm. In the former condition, semen is not produced at all, whereas in the latter condition, semen is produced but cannot be released during orgasm. Post-orgasm urine analysis reveals sperm in urine in the case of retrograde ejaculation (McMahon, 2014). PE is a spontaneous ejaculation that occurs sooner than desired, either before or after penetration. DE is an undue delay in ejaculation (Ralph & Wylie, 2005). Orgasmic dysfunction is defined by anorgasmia, reduced orgasmic sensation, or delayed orgasm during sexual activity (DeLamater & Karraker, 2009). Sexual desire disorder is characterized by a reduced desire (hypoactive desire) compared to normal levels, increased desire (hyperactive desire) than normal, or sexual aversion (fear, revulsion, or disgust for sexual activity) (Kafka, 2010; Montgomery, 2008).
The causes of MSD are physical, psychological, or a combination of both. MSD can occur due to several pathological conditions (diabetic neuropathy, hypertension, endocrine alterations, prostate cancer, urinary infections, urinary incontinence, degenerative and vascular diseases, and surgical damage to nerves and organs), psychological problems (relationship with partner, depression, and anxiety), and the use of psychoactive (antipsychotic) and antihypertensive drugs (Al-Turki, 2012; DeLamater & Karraker, 2009; Hassan et al., 2014; Hoekstra et al., 2012; Huhtaniemi, 2014; Justo et al., 2010; Mutagaywa et al., 2014; Wong et al., 2009a; Zhang et al., 2017). Lifestyle (smoking, substance abuse, overweight, and obesity) and sociodemographic factors (age, income, education, and employment status) may also be associated with MSD (Donnelly et al., 2018; Isha et al., 2016; Palacios-Ceña et al., 2012; Rao et al., 2015; Zhang et al., 2017).
Residents of European countries have access to sophisticated diagnostic and treatment options for their sexual problems. Discussing sex is a taboo in most Asian societies, and sexual dysfunctions are considered a part of the normal process of aging. Due to Asian men’s cultural and religious beliefs, socioeconomic conditions, lack of awareness, tendency for traditional medicines, and noncompliance with and reduced access to modern healthcare, they do not take sexual dysfunction as a serious disorder, and it commonly remains undiagnosed and untreated (Ho et al., 2011). The differences in genetic and environmental factors may also influence the risks of MSD in Asian and European populations differently. The differences in prevalence and associated factors of MSD between these regions are not being reported. This review is being performed to investigate the comparative incidence of and factors contributing to MSD in European and Asian populations. The prevalence of MSD among young men, defined as men under 60 years of age (<60 years), and elderly men, defined as men over 60 years of age (>60 years), of the two regions will also be compared.
Methods
Systematic Literature Search
The literature was searched on MEDLINE using the following keywords: “male sexual dysfunctions,” “erectile dysfunctions,” “ejaculation dysfunctions” and “orgasmic dysfunctions”. The search was not narrowed down to Asian and European regions to avoid missing potential studies, because many of the studies mention countries but do not mention the region.
Inclusion and Exclusion Criteria
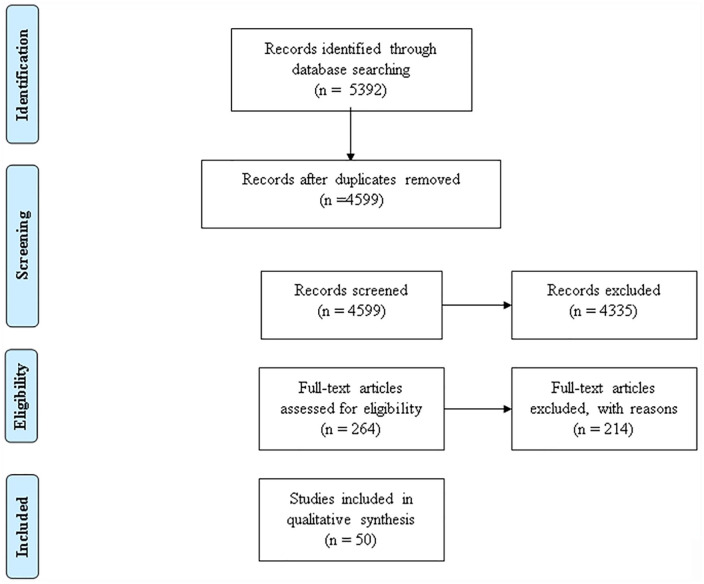
The criteria for eligibility of studies included that they be original quantitative population/community-based studies published from 2008 to 2018 in the English language. The 10 years duration is to represent a recent review of the epidemiology of MSD. In this regard, qualitative studies, reviews, conference abstracts and proceedings, case reports, reviews, and editorials were excluded. Furthermore, studies conducted in a population with specific morbidities and from other than Asian and European regions were also excluded (Figure 1).
Figure 1.
Flow diagram of study selection.
Data Extraction
The studies were carefully reviewed, and information was extracted about the first authors, study types, population characteristics, sampling durations, types of MSD, definitions of MSD, instruments and methods used to assess the prevalence of MSD, and associated factors. Men <60 years of age were categorized as young men and >60 years as elderly, in accordance with the criteria of the World Health Organization (WHO).
Results
Included Studies
The database search resulted in the identification of 5,392 studies. In total, 793 of these articles were duplicates, and 2,533 did not discuss the desired research topic. The remaining 2,066 articles were screened based on abstracts, and 1,802 studies were excluded based on their design as a specific cohort, review, or qualitative studies. The full texts of the 264 remaining studies were assessed, and, finally, 50 of those studies were included in this systematic review (Figure 1).
Characteristics of Included Studies
Table 1 presents the population/community-based studies reporting on MSD in Asian (n = 25) and European (n = 25) populations. The Asian studies covered the prevalence of MSD in eight countries: China (Chung et al., 2015; Hao et al., 2011; Huang et al., 2014; Kim et al., 2009; Liang et al., 2010; Tang et al., 2015; Wong et al., 2009a; Wong et al., 2009b; Zhang et al., 2013; 2016; 2017), India (Rao et al., 2015), Jordan (Ghalayini et al., 2010), Korea (Jeong et al., 2011; Kim & Jeon, 2013; Lee et al., 2013; Park et al., 2010), Malaysia (Khoo et al., 2008; Quek et al., 2008), Taiwan (Hwang et al., 2010; Liu et al., 2010), Thailand (Permpongkosol et al., 2008), and Turkey (Çayan et al., 2017; Kendirci et al., 2014; Serefoglu et al., 2011). The European studies were from 15 countries, namely Belgium (Hendrickx et al., 2016), Croatia (Carvalheira et al., 2014; Landripet & Stulhofer, 2015), Denmark (Andersen et al., 2008; Christensen et al., 2011), Finland (Jern et al., 2012; Kontula & Haavio-Mannila, 2009), France (Moreau et al., 2016), Germany (Beutel et al., 2018), Ireland (Donnelly et al., 2018), the Netherlands (Korfage et al., 2008), Norway (Traeen & Stigum, 2010), Poland (Jankowska et al., 2008), Portugal (Quinta Gomes & Nobre, 2014), the Republic of Moldova (Dumbraveanu et al., 2018), Spain (Castellanos-Torres et al., 2013; Ruiz-Muñoz et al., 2013), Sweden (Beckman et al., 2008; Holm et al., 2012), and the United Kingdom (Lee et al., 2016; Mitchell et al., 2016; Mitchell et al., 2013), while a further three studies were conducted on men from 10 particular countries: Belgium, Estonia, France, Germany, Hungary, Italy, Poland, Spain, Sweden, and the United Kingdom (Corona et al., 2010; Lee et al., 2013; Sand et al., 2008).
Table 1.
Sexual Dysfunctions in Asian and European Men.
| Author (Year) | Sampling Duration | Assessment Method | Cut-Off Score/Definition | Time Period | Condition/Dysfunction | Prevalence (%) | Associated Factors | ||
|---|---|---|---|---|---|---|---|---|---|
| Asia | |||||||||
| China |
Whole
Population |
Age Groups (Years) | Significant | Nonsignificant | |||||
| Kim et al. (2009) | SAQ | Erectile difficulties for 3 months | Year | ED | 12.2 | 25–59 years: 12.2 | NA | ||
| No interest in sex | Year | HSDD | 12.2 | 25–59 years: 12.2 | |||||
| Anxiety about sex | Year | Anxiety | 16.0 | 25–59 years: 16.0 | |||||
| Liang et al. (2009) | NS | SAQ | Ejaculation within in 1 min of penetration always or nearly always | 6 months | PE | 15.3 | 15–30 years: 9.2 31–40 years: 25.6 41–50 years: 11.2 51–60 years: 3.3 |
(-) Age (+) Pain (+) Urinary symptoms (+) Quality of life (-) IIEF-Score (+) Prostatitis |
|
| Wong, Leung, and Woo (2009a) | 2001–2003 | IAQ# | Impotent | NS | ED | 56.6 | ≥65 years: 56.6 | (+) Mod to severe LUTS (+) BMI (+) CVD (+) Hypertension (+) Diabetes (+) Stroke (+) β-blockers use (+) Thiazides (+) Clinical depression |
|
| Mildly impotent | Mild ED | 24.9 | ≥65 years: 24.9 | ||||||
| Moderately impotent | Mod ED | 19.8 | ≥65 years: 19.8 | ||||||
| Completely impotent | Severe ED | 11.9 | ≥65 years: 11.9 | ||||||
| Wong, Leung, and Woo (2009b) | NS | IAQ | 6 months | NS | ED | 88.3 | ≥65 years: 88.3 | (+) Age (+) Mod to severe LUTS (+) Depression (-) Physical activity |
|
| Mild ED | 77.0 | ≥65 years: 77.0 | |||||||
| Mod ED | 7.4 | ≥65 years: 7.4 | |||||||
| Severe ED | 4.0 | ≥65 years: 4.0 | |||||||
| Hao et al. (2011) | 2007 | SAQ# | Inability to sustain or achieve an erection sufficient for satisfactory intercourse | ED | 12.1 | ≤30 years: 11.1 31–40 years: 10.5 41–50 years: 12.1 51–60 years:17.2 |
(+) Age (+) Prostatitis symptoms |
||
| Mild ED | 62.3 | 15–60 years: 62.3 | |||||||
| Mod ED | 23.3 | 15–60 years: 23.3 | |||||||
| Sever ED | 14.4 | 15–60 years: 14.4 | |||||||
| ED | 40.5 | ≤30 years: 33.2p
31–40 years: 36.5p 41–50 years: 56 p 51–60 years:75.9p |
|||||||
| ED | 39.3 | ≤30 years: 34.9a
31–40 years: 32.5a 41–50 years: 41.8a 51–60 years: 61.1a |
|||||||
| SAQ; IIEF-5 | <22 | ED | 17.1 | ≤30 years: 16.0 31–40 years: 14.5 41–50 years: 15.4 51–60 years: 29.1 |
|||||
| Mild ED | 64.8 | 15–60 years: 64.8 | |||||||
| Mod ED | 20.5 | 15–60 years: 20.5 | |||||||
| Sever ED | 14.7 | 15–60 years: 14.7 | |||||||
| ED | 35.1 | ≤30 years: 28.3 p
31–40 years: 33.6 p 41–50 years: 44.0 p 51–60 years:70.0 p |
|||||||
| ED | 30.1 | ≤30 years: 20.1a
31–40 years: 25.6a 41–50 years: 30.0a 51–60 years: 53.7a |
|||||||
| Zhang et al. (2013) | 2007 | Interview# | Erectile problem | Year | ED | 4.3 | 30–39 years:1.0 40–49 years: 3.4 50–60 years: 9.8 |
(+) Age (+) Partner sought medical help (+) Nonliberal attitudes toward female sexual initiation (+) Nonliberal attitudes toward female sexual refusal (+) Dissatisfaction with marriage |
Age (for PE/DE) |
| Ejaculation dysfunction | PE/DE | 4.7 | 30–39 years:4.2 40–49 years: 4.4 50–60 years: 6.1 |
||||||
| Lack of sexual interest | HSDD | 11.1 | 30–39 years:7.0 40–49 years: 10.3 50–60 years: 17.2 |
||||||
| ≥1 MSD | 14.8 | 30–39 years:10.3 40–49 years: 14.0 50–60 years: 21.7 |
|||||||
| Huang et al. (2014) | 2008–2011 | SAQ; IIEF-5 | <22 | 6 months | ED | 49.9 | 40–51: 58.6 52–59 years: 60.1 60–64 years: 51.2 65–80 years: 39.6 |
(+) Age (+) Diabetes (+) Hypertension (+) BPH (+) PLS (+) FBG (+) TPSA (-) FSH |
BMI, WC, exercise, alcohol, tea, smoking, dyslipidemia, BP, HR, creatinine, TT, LH, PRL, E2, ALT, and TG |
| Chung et al. (2015) | 2001–2005 | Interview# | Impotent | NS | ED | 57.2 | ≥65 years: 57.2 | ||
| Mild ED | 24.7 | ≥65 years: 24.7 | |||||||
| Mod ED | 20.0 | ≥65 years: 20.0 | |||||||
| Severe ED | 12.5 | ≥65 years: 12.5 | (+) All causes mortality (CVD, respiratory and Cancer) | ||||||
| Tang et al. (2015) | 2007–2008 | SAQ; Chinese version IIEF-5 | <22 | NS | ED | 77.9 | 40–49 years: 55.3 50–59 years: 88.2 60–69 years: 91.8 |
(+) Age (+) Occupation (physical, semi-physical, or mental labor) (+) Educational level (+) Poor health status (+) Drug use (+) Smoking duration (+) Drinking frequency, (+) Genitourinary diseases |
AD, marriage age, and smoking frequency |
| 12–21 | Mild ED | 28.1 | 40–49 years: 35.0 50–59 years: 25.1 60–69 years: 23.6 |
||||||
| 8–11 | Mod ED | 10.3 | 40–49 years: 8.2 50–59 years: 13.0 60–69 years: 9.7 |
||||||
| 5–7 | Severe ED | 39.5 | 40–49 years: 12.2 50–59 years: 50.1 60–69 years: 58.4 |
||||||
| SAQ; Chinese version of ADAM | NS | NS | LOH | 80.8 | 40–49 years: 55.7 50–59 years: 91.5 60–69 years: 97.1 |
(+) Sever ED | |||
| SAQ; Chinese version of AMS | ≥ 27 | NS | LOH | 32.3 | 40–49 years: 9.5 50–59 years: 25.9 60–69 years: 63.7 |
||||
| Total testosterone | ≤9.13 nM | NS | AD | 14.0 | 40–49 years: 12.9 50–59 years: 15.0 60–69 years: 13.9 |
||||
| cFT | ≤0.169 nM | 43.7 | 40–49 years: 30.3 50–59 years: 43.1 60–69 years: 57.4 |
||||||
| ADAM + cFT | NS | 37.9 | 40–49 years: 18.9 50–59 years: 38.1 60–69 years: 55.9 |
||||||
| AMS + cFT | NS | 15.4 | 40–49 years: 4.6 50–59 years: 6.9 60–69 years: 36.0 |
||||||
| Zhang et al. (2017) | 2010–2013 | IAQ; IIEF-5 | <22 | NS | ED | 40.6 | 40–49 years: 18.1 50–59 years: 23.6 60–69 years: 48.4 ≥70 years: 81.6 |
(+) Age (+) 30 cigarettes daily (+) Bad spouse relationship (+) Diabetes (+) BPH related LUTS (+) BMI: 30kg/m2 (+) Personal income (-) Zhuang & Muslim |
Marital status, waist-to-hip ratios, education levels, area of residence, CVD, cerebrovascular diseases, and alcohol |
| Zhang et al. (2015) | 2012 | SAQ# | No erection or could not maintain erection for 3 months | Year | ED | 5.0 | 18–29 years: 0.0 30–39 years: 0.8 40–49 years: 5.7 50–59 years: 8.7 >60 years: 16.7 |
(+) Age (+) Dissatisfied with marriage (+) HSDD (+) |
Employment, housing ownership, having children, length of marriage, and divorce |
| India | |||||||||
| Sathyanarayana Rao et al. (2015) | NS | IAQ; IIEF-5 | NS | NS | ED | 43.5 | >60 years: 43.5 | (+) Married (+) Unemployed (+) Hypertension (+) Diabetes |
Age, occupation, education, sociodemographic status, domicile, family structure, alcohol, and smoking |
| Mild ED | 10.5 | >60 years: 10.5 | |||||||
| Mild to Mod ED | 31.6 | >60 years: 31.6 | |||||||
| Mod ED | 36.8 | >60 years: 36.8 | |||||||
| Severe ED | 21.0 | >60 years: 21.0 | |||||||
| IAQ; PEDT | NS | PE | 10.9 | >60 years: 10.9 | |||||
| IAQ | NS | NS | Anorgasmia | 0.38 | >60 years: 0.38 | ||||
| IAQ | HSDD | 0.77 | >60 years: 0.77 | ||||||
| Jordon | |||||||||
| Ghalayini et al. (2010) | NS | IAQ; IIEF-5 | ≤20 | NS | ED | 49.9 | <29 years:24.7 30–39 years:41.4 40–49 years: 52.7 50–59 years:59.5 60–69 years: 72.3 >70 years: 89.2 |
(+) Age (+) BMI, (-) Educational level (+) Smoking (-) Household income (-) Physical activity (+) Medication (+) Diabetes mellitus (+) HTN (+) IHD |
|
| Mild ED | 25.0 | ≥18 years: 25.0 | |||||||
| Mod ED | 13.5 | ≥18 years: 13.5 | |||||||
| Severe ED | 11.4 | ≥18 years: 11.4 | |||||||
| Korea | |||||||||
| Park et al. (2010) | 2008 | SAQ | Self-diagnosed premature ejaculation | 3 months | PE | 27.5 | 20–29 years: 23.4 30–39 years: 24.6 40–49 years: 30.7 ≥50 years: 36.8 |
(+) Prostatitis (+) Hyperthyroidism (+) Psychological disturbances |
|
| Jeong et al. (2011) | 2003 | SAQ; Korean Version IIEF-5 | <18 | NS | ED | 48.8 | 45–54 years: 18.2 55–64: 26.2 65–74 years: 60.4 |
(+) Age (+) Past smoking (+) Depression |
Educational level, exercise, marital status, alcohol, BMI, and hypertension |
| Kim and Jeon (2013) | 2008–2009 | Interview# | Never satisfied | Low satisfaction | 3.2 | ≥60 years: 3.2 | (-) Frequency of sexual activity (-) Satisfaction in relationship with spouse (-) Cognitive function |
Age, education, income, diseases, health statues of self and spouse, ADL, IADL, cognitive function, length of cohabitation, depression, and importance of sex-life | |
| Not satisfied | 13 | ≥60 years: 13.0 | |||||||
| Less satisfied | 37.6 | ≥60 years: 37.6 | |||||||
| Lee et al. (2013) | 2010 | SAQ | NS | PE | 19.5 | 20–29 years: 10.7 30–39 years: 14.9 40–49 years: 19.3 50–59 years: 27.8 60–64 years: 41.8 |
(+) Age (+) Diabetes (+) Hypertension (+) Arthritis (+) Back pain (+) Thyroid disease (+) Spinal disease (+) Prostatic disease (+) ED (-) Satisfaction |
For IELT: Hypertension, back pain, thyroid disease, spinal disease, prostatic disease, and satisfaction | |
| SAQ; PEDT | ≤8 | PE | 11.3 | 20–64 years: 11.3 | |||||
| Stopwatch IELT | ≤2 min | PE | 16.6 | 20–29 years: 15.0 30–39 years: 13.2 40–49 years: 16.5 50–59 years: 16.6 60–64 years: 35.4 |
|||||
| Malaysia | |||||||||
| Khoo et al. (2008) | NS | IAQ; IIEF-5 | <22 | NS | ED | 74.5 | 50–59 years: 67.5 60–69 years: 90.8 >70 years: 95.0 |
(+) Age (-) Health status (+) Occupation (+) LUTS (+) Depression |
Ethnicity, educational level, |
| 17–21 | Mild ED | 32.8 | 50–59 years: 36.8 60–69 years: 30.3 >70 years: 30.0 |
||||||
| 12–16 | Mild to Mod ED | 17.7 | 50–59 years: 16.7 60–69 years: 5.0 >70 years: 28.9 |
||||||
| 8–11 | Mod ED | 5.1 | 50–59 years: 5.1 60–69 years: 5.0 >70 years: 6.6 |
||||||
| 1–7 | Severe ED | 14.5 | 50–59 years: 9.0 60–69 years: 55.0 >70 years: 25.0 |
||||||
| IAQ; ADAM | Yes to three questions | AD | 25.4 | 50–59 years: 18.3 60–69 years: 33.3 >70 years: 63.0 |
(+) BMI (+) Glucose |
||||
| Quek et al. (2008) | NS | SAQ; IIEF-5 | <21 | ED | 41.6 | 20–29 years: 6.3 30–39 years: 6.5 40–49 years: 22.9 50–59 years: 54.6 ≥60 years: 62.7 |
(+) Age (+) Diabetes (+) Hypertension (+) Nocturia |
Marital difficulties, anxiety, and depression, | |
| Overall SP | 50.0 | 20–29 years: 25.0 30–39 years: 29.7 40–49 years: 45.8 50–59 years: 75.3 ≥60 years: 88.2 |
|||||||
| IELT | ≤2 min | PE | 22.3 | 20–29 years: 16.7 30–39 years: 13.0 40–49 years: 9.4 50–59 years: 1.0 ≥60 years: 0 |
(+) Frequency of sex (+) Anxiety (-) Diabetes |
Age, marriage difficulties, hypertension, and depression | |||
| ED+PE | 14.0 | 20–29 years: 2.1 30–39 years: 10.1 40–49 years: 13.5 50–59 years: 19.6 ≥60 years: 25.5 |
|||||||
| Taiwan | |||||||||
| Hwang et al. (2010) | 2006 | Interview | NS | ED | 30–39 years: 1 40–49 years: 1 50–59 years: 3 60–69 years: 7 >70 years: 15 |
(+) Educational level (-) Income (-) Satisfaction |
|||
| IAQ; IIEF-5 | <22 | ED | 27 | 30–39 years: 17 40–49 years: 18 50–59 years: 31 60–69 years: 44 >70 years: 58 |
|||||
| Mild to Mod ED | 65 | 30–59 years: 65 | |||||||
| Mod ED | 28 | 30–59 years: 28 | |||||||
| Severe ED | 7 | 30–59 years: 7 | |||||||
| IAQ; EHS | ≤3 | ED | 23 | 30–39 years: 11 40–49 years: 18 50–59 years: 28 60–69 years: 46 >70 years: 67 |
|||||
| Liu et al. (2010) | 2007–2008 | IAQ; IIEF-5 | Problem with erection or score <22 | NS | ED | 54.3 | 40–49 years: 42.5 50–59 years: 47.9 60–69 years: 74.7 ≥70 years: 74.4 |
||
| NS | NS | HSDD | 52.3 | 40–49 years: 50.4 50–59 years: 48.1 60–69 years: 57.0 ≥70 years: 81.4 |
|||||
| Thailand | |||||||||
| Permpongkosol et al. (2008) | NS | Interview | NS | 6 months | ED | 42.2 | 40–49 years: 23.4 50–59 years: 47.8 60–70 years: 77.0 |
(+) Age (+) Unmarried (-) Education (-) Income (+) Duration of smoking (+) Smoking (+) Alcohol (+) Unemployment (+) Occupation (+) Diabetes (+) Hypertension (+) Heart disease (+) Peptic ulcer (+) Prostatitis |
Exercise and BMI |
| Mild ED | 17.5 | 40–49 years: 12.4 50–59 years: 21.2 60–70 years: 23.9 |
|||||||
| Mod ED | 13.1 | 40–49 years: 7.7 50–59 years: 16.9 60–70 years: 20.2 |
|||||||
| Severe ED | 11.6 | 40–49 years: 3.3 50–59 years: 9.7 60–70 years: 32.9 |
|||||||
| Turkey | |||||||||
| Serefoglu et al. (2011) | 2009 | IAQ; Turkish version of PEDT, AIPE, and PEP | >9, <31 | 6 months | PE | 25.0 | 20–29 years: 14.0 30–39 years: 15.5 40–49 years: 20.5 50–59 years: 22.0 60–69 years: 38.7 ≥70 years: 49.1 |
(-) Sexual function | |
| Kendirci et al. (2014) | 2010 | IAQ; IIEF-5, IPSS, and MSHQ-4 | ≤25, ≥1, ≤12 | NS | MPD | 24.4 | 40–49 years: 9.1 50–59 years: 27.1 60–69 years: 56.7 ≥70 years: 76.6 |
(-) Income (+) BMI (+) Dyslipidemia (+) Hypertension, (+) Diabetes mellitus (+) CVD |
Residence area and testosterone deficiency |
| Cayan et al. (2017) | NS | IAQ; IIEF-5 | <26 | NS | ED | 33 | 40–49 years: 17.0 50–59 years: 35.5 60–69 years: 68.8 ≥70 years: 82.9 |
(-) Educational level (+) Retired (+) Urban residence (+) Income (+) Vascular disorder (mod-severe ED) (+) CP or BPE (mod-severe ED) (+) Diabetes (mod-severe ED) (+) Hypertension (mod-severe ED) (+) Atherosclerosis (mod-severe ED) (+) CAD (mod-severe ED) (+) Dyslipidemia (mod-severe ED) (+) CP (+) BPH |
Unemployment and BMI |
| Mild ED | 25.6 | 40–49 years: 2.5 50–59 years: 10.5 60–69 years: 38.5 ≥70 years: 28.1 |
|||||||
| Mod ED | 5.5 | 40–49 years: 0.29 50–59 years: 1.6 60–69 years: 8.1 ≥70 years: 26.0 |
|||||||
| Severe ED | 1.9 | 40–49 years: 0.1 50–59 years: 0.5 60–69 years: 0.8 ≥70 years: 14.9 |
|||||||
| EUROPE | |||||||||
| Belgium | |||||||||
| Hendrickx et al. (2016) | 2011–2012 | SAQ; SFS | ≥3 | 6 months | ED | 8.3 | 14–34 years:0.9 35–49 years:3.0 50–64 years: 11.0 65–80 years: 41.3 |
(+) Age (ED, HSDD) (-) Satisfaction |
Age (PE/DE) |
| Early orgasm | 6 months | PE | 9.2 | 14–34 years: 9.3 35–49 years: 10.7 50–64 years: 9.8 65–80 years: 2.7 |
|||||
| Delayed orgasm | 6 months | DE | 1.4 | 14–34 years: 1.3 35–49 years: 2.1 50–64 years: 1.8 65–80 years: 10.7 |
|||||
| Orgasm without ejaculation |
6 months | RE | 0.6 | 14–34 years: 0 35–49 years: 0 50–64 years: 1.8 65–80 years: 1.4 |
|||||
| Lack of spontaneous sexual desire | 6 months | HSDD | 13 | 14–34 years: 1.8 35–49 years: 2.1 50–64 years: 7.3 65–80 years: 5.3 |
|||||
| Sexual aversion | 6 months | Sexual aversion | 0.6 | 14–34 years: 0.9 35–49 years: 0.9 50–64 years: 0 65–80 years: 0 |
|||||
| Croatia | |||||||||
| Carvalheira et al. (2014) | NS | SAQ; NATSAL 2000 | Lack of sexual interest for at least 2 months with personal distress | Year | HSDD | 14.4 | 18–29 years: 3.3 30–39 years: 5.7 40–49 years: 3.4 50–59 years: 1.8 >60 years: 0.2 |
(+) Croatian and Norwegian (+) Asexuality (+) Higher depression (-) Self-confidence of erection (+) Duration of relationship (+) Negative perception of attractiveness of partner (+) Partner hurts feelings (+) Masturbation frequency (+) Pornography use (+) Perception of increased age (+) Bad health perception |
Tiredness, professional stress, perception of
sexual life boring and partner sexually passive, poor
communication and relationship with partner, sexual abuse,
medication, physical violent partner, partner does not want
sex, not sexually attracted to partner, not sexually
attractive, did not have sex for long, and pornography use |
| Decrease sexual interest | 6 months | HSDD | 18–29 years: 22 30–39 years: 26.2 40–49 years: 27.5 50–59 years: 29.9 >60 years: 22.9 |
||||||
| Landripet and Stulhofer (2015) | 2011 | SAQ; GSSAB | Difficulties with achieving and maintaining erection for 2 months | Year | ED | 14.2–28.3 | 18–40 years: 14.2–28.3 | (+) Pornography use (Croatian) (-) Education (Croatian 2) |
Age and education |
| SAQ; IIEF-5 | <22 | 30.8 | 18–40 years: 30.8b | ||||||
| SAQ; GSSAB | Reduced sexual desire for 2 months | Year | HSDD | 16.3–37.4 | 18–40 years: 16.3–37.4 | (+) Age (Croatian & Portuguese) (-) Education (Croatian) |
Age (Norwegian) and pornography use | ||
| Reduced sexual desire for 3 months | Year | 12.8 | 18–40 years: 12.8b | ||||||
| SAQ; GSSAB | Inability to climax for 2 months | Year | DE | 6.2–19.9 | 18–40 years: 6.2–19.9 | Age, pornography use, and education | |||
| Difficulties in reaching orgasm | 6 months | 9.3 | 18–40 years: 9.3b | ||||||
| Denmark | |||||||||
| Andersen et al. (2008) | 2004 | SAQ | Experiencing “all the time,” “almost all the time,” or
“quite often,” inadequate to obtain or maintain erection during intercourse |
6 months | ED | 10.1 8.2c 10.8d 17.4e |
20–45 years: 5.5 20–45 years: 4.6c 20–45 years: 5.2d 20–45 years: 12.7e 50–75 years: 18.4 50–75 years: 17.1c 50–75 years: 18.3d 50–75 years: 23.1e |
(+) Age (+) BMI≥30 (20–45 years) (+) Smoking (20–45 years) |
50–75 years: Age and BMI |
| Ejaculation come too fast “all the time,” “almost all the time,” or “quite often” | 6 months | PE | 22.3 22.0c 21.7d 27.0e |
20–45 years: 23.7 20–45 years: 23.4c 20–45 years: 23.1d 20–45 years: 28.6e 50–75 years: 19.6 50–75 years: 17.6 50–75 years: 19.8 50–75 years: 25 |
(-) Age | BMI | |||
| Ejaculation come too fast “all the time,” “almost all the time,” or “quite often” | 6 months | DE | 4.6 4.3c 4.5d 6.1e |
20–45 years: 2.5 20–45 years: 3.0c 20–45 years: 1.1d 20–45 years: 4.8e 50–75 years: 8.4 50–75 years: 7.6 50–75 years: 9.1 50–75 years: 7.7 |
(+) Age | BMI | |||
| Frequency of sexual desire “rarely” or “never” | 6 months | HSDD | 4.3 3.7c 5.4d 3.5e |
20–45 years:3.3 20–45 years: 3.2c 20–45 years: 3.7d 20–45 years: 1.6e 50–75 years: 6.2 50–75 years: 4.7 50–75 years: 7.6 50–75 years: 5.8 |
BMI | ||||
| Christensen et al. (2011a) | 2005 | SAQ | Erectile difficulties | NS | ED | 5 | <50 years: 1 50–59 years: 5 ≥60 years: 16 |
(-) Employment (ED) (+) Difficulties paying bills last year (sexual dysfunction & Dyspareunia) (-) Income (Dyspareunia) (+) Unmarried (PE) |
Place of residence, education level, Income, difficulties paying bills last year, employment, marital status, place of residence, education level, income, difficulties paying bills last year, marital status, and unmarried |
| Any sexual dysfunction | Sexual dysfunction | 11 | <20 years: 2 20–59 years: 10 ≥60 years: 20 |
||||||
| Anorgasmia | 2 | 20–30 years: 23 ≥70 years: 65 |
|||||||
| Sex painful | 0.1 | <20 years: 18 ≥70 years: 3 |
|||||||
| Europe* | |||||||||
| Sand et al. (2008) | 2001 | Interview | No or short-term erection | NS | ED | 16 | 20–29 years: 8 30–39 years: 11 40–49 years: 15 50–59 years: 22 60–69 years: 30 70–75 years: 37 |
(-) Sexual satisfaction (-) Health satisfaction |
Constructs of masculinity |
| Corona et al. (2010) | NS | SAQ; EMAS-SFQ-14 | NS | NS | ED | 30.5 | 40–49 years: 5.2 50–59 years: 18.8 60–69 years: 35.9 ≥70 years: 55.5 |
(+) Age () (+) Country of residence (+) Smoking (+) Unemployment (+) Partner’s poor health (-) Sexual satisfaction (+) Depression (+) LUTS (+) CVD (+) Diabetes (+) Obesity |
|
| Mod ED | 17.3 | 40–49 years: 4.5 50–59 years: 14.1 60–69 years: 23.0 ≥70 years: 29 |
|||||||
| Severe ED | 13.2 | 40–49 years: 0.6 50–59 years: 4.8 60–69 years: 15.0 ≥70 years: 35.0 |
|||||||
| Rarely to < half time | Orgasmic disorder | 12.1 | 40–49 years: 6.6 50–59 years: 8.9 60–69 years: 15 ≥70 years: 18.7 |
(+) Depression (+) LUTS |
|||||
| Rarely or never reach orgasm | Anorgasmia | 6.6 | 40–49 years: 3.0 50–59 years: 5.0 60–69 years: 8.0 ≥70 years: 11.0 |
||||||
| Reach orgasm < half time | Reach orgasm <Half time | 5.6 | 40–49 years: 4.0 50–59 years: 4.0 60–69 years: 7.3 ≥70 years: 10.1 |
||||||
| Dissatisfied with sexual life | Low satisfaction | 27.4 | 40–49 years: 23.2 50–59 years: 25.0 60–69 years: 27.2 ≥70 years: 28.3 |
(+) Age (+) Depression |
|||||
| Lee et al. (2013) | NS | SAQ; EMAS-SFQ | Sometimes—never able to get and keep erection | Year | ED | 50.3 | ≥60 years: 50.3 ≥60 years: 41.9f ≥60 years: 61.1g ≥60 years: 77.4h |
(+) Pre-frailty (+) Frailty |
|
| Finland | |||||||||
| Kontula et al. (2009) | 1992&1999 | SAQ | Erectile difficulties quite often | Year | ED | 14 | 45–54 years: 8 55–64 years: 16 65–74 years: 30 |
||
| Not satisfied with sexual life | Low satisfaction | 20 | 45–54 years: 18 55–64 years: 21 65–74 years: 23 |
||||||
| Lack of own sexual desire caused problems very or
quite often in last year |
HSDD | 15 | 45–54 years: 13 55–64 years: 12 65–74 years: 30 |
(-) Good health (+) Low sexual self-esteem (-) Good sexual functioning (-) Sexually skillful partner (-) Considering sexual life important (+) Unsatisfied with sex (-) Finding pornography arousing |
Age, duration of relationship, education, exercise frequency, BMI, stress symptoms, duration of the present relationship, preferring more frequent intercourse (or satisfaction with the frequency of it), partner seldom coming too quickly, and regarding sex without love to be wrong | ||||
| Jern et al. (2012) | 2005–2006 | SAQ; IIEF-5 | <22 | ED | 15.2 | 18–48 years: 15.2 | (+) Age (+) ED at first intercourse (+) Anxiety (+) Depression |
||
| 17–21 | Mild ED | 13.2 | 18–48 years: 13.2 | ||||||
| 12–16 | Mild to Mod ED | 1.6 | 18–48 years: 1.6 | ||||||
| 8–11 | Mod Ed | 0.4 | 18–48 years: 0.4 | ||||||
| 5–7 | Severe ED | 0 | 18–48 years: 0.0 | ||||||
| France | |||||||||
| Moreau et al. (2016) | 2010 | Interview | Problem in maintaining erection often to rarely | Year | ED | 16 | 15–24 years: 16 | (+) Sexual satisfaction when ED or PE hindering
intercourse or >1dysfunctions (+) Unintended pregnancy (>1 dysfunctions when hindering sexual intercourse |
Forced sex, STIs, and ever unintended pregnancy |
| Premature ejaculation often to rarely | PE | 52 | 15–24 years: 52 | ||||||
| Difficulty in reaching orgasm often to rarely | DE | 17 | 15–24 years: 17 | ||||||
| Pain during sex often to rarely | Sex painful | 13 | 15–24 years: 13 | ||||||
| Low sexual desire often to rarely | HSDD | 28 | 15–24 years: 28 | ||||||
| No pleasure in sex often to rarely | Sex not pleasurable | 26 | 15–24 years: 26 | ||||||
| Sexual dysfunction at least one | Sexual dysfunction | 17 | 15–24 years:17 | ||||||
| Sexual dysfunction >1 | 6 | 15–24 years: 6 | |||||||
| Germany | |||||||||
| Beutel et al. (2018) | 2005 | IAQ | No feeling of sexual desire | Month | HSDD | 8.4 | 18–30 years: 0.0 31–40 years: 0.6 41–50 years: 0.5 51–60 years: 4.4 61–70 years: 14.9 ≥70 years: 47.4 |
(+) Age (+) Sampling year |
Cohabiting (2005) |
| 5.8 | 18–30 years: 0.0i
31–40 years: 0.0i 41–50 years: 0.0i 51–60 years: 1.8i 61–70 years: 9.8i ≥70 years: 37.9i |
||||||||
| 14.0 | 18–30 years: 0.0j
31–40 years: 2.1j 41–50 years: 1.9j 51–60 years: 14.0j 61–70 years: 36.8j ≥70 years: 61.5j |
||||||||
| 2016 | 13.2 | 18–30 years: 2.8 31–40 years: 4.8 41–50 years: 4.2 51–60 years: 7.7 61–70 years: 19.8 ≥70 years: 50.0 |
|||||||
| 8.9 | 18–30 years: 0.0i
31–40 years: 1.7i 41–50 years: 1.7i 51–60 years: 4.1i 61–70 years: 13.9i ≥70 years: 38.5i |
||||||||
| 19.1 | 18–30 years: 4.2j
31–40 years: 11.5j 41–50 years: 8.5j 51–60 years: 14.5j 61–70 years: 31.1j ≥70 years: 65.5j |
||||||||
| Ireland | |||||||||
| Donnelly et al. (2018) | NS | SAQ; EPIC-26 | Very poor to no erection | NS | ED | 24.6 | 40–59 years: 9.4 60–69 years: 17.5 70–79 years: 32.6 ≥80 years: 60.8 |
(+) Age (+) BMI (+) Deprived (+) Poor general health (-) Physical activity |
Area of residence |
| No or poor ability to reach orgasm | NS | Orgasmic disorder | 22.9 | 40–59 years: 8.9 60–69 years: 15.5 70–79 years: 30.7 ≥80 years: 64.2 |
|||||
| Big sexual problems | NS | SP | 19.5 | 40–59 years: 10.1 60–69 years: 15.7 70–79 years: 25.1 ≥80 years: 65.3 |
|||||
| Netherlands | |||||||||
| Korfage et al. (2008) | 2003–2004 | SAQ; Dutch module SAc | Problems with getting or maintaining erections | NS | ED | 19.1 | 58–61 years: 12.0 62–64 years: 14.6 65–67 years: 18.4 68–70 years: 21.9 71–78 years: 26.3 |
(+) Age | |
| Almost no sexual desire | HSDD | 48.0 | 58–61 years: 40.8 62–64 years: 41.4 65–67 years: 46.1 68–70 years: 51.6 71–78 years: 57.7 |
||||||
| Very dissatisfied | Low satisfaction | 20.2 | 58–61 years: 13.3 62–64 years: 20.5 65–67 years: 18.8 68–70 years: 22.5 71–78 years: 23.2 |
||||||
| Norway | |||||||||
| Traeen and Stigum (2010) | 2008 | Interview | Problem of erection manifested | Year | ED | 10.0 | 18–29 years: 5.0 30–39 years: 5.0 40–49 years: 7.0 50–59 years: 11.0 60–67 years: 33.3 |
||
| Problem of erection manifested | Year | ED | 9.0 | 18–29 years: 5.0 30–39 years: 3.0 40–49 years: 4.0 50–59 years: 9.0 |
|||||
| NS | PE | 31 | 18–29 years: 24.0 30–39 years: 23.0 40–49 years: 19.0 50–59 years: 24.0 60–67 years: 28.0 |
||||||
| NS | PE | 38 | 18–29 years: 28.0 30–39 years: 22.0 40–49 years: 30.0 50–59 years: 33.0 |
||||||
| NS | DE | 8 | 18–29 years: 10.0 30–39 years: 8.0 40–49 years: 8.0 50–59 years: 7.0 60–67 years: 11 |
||||||
| NS | DE | 6 | 18–29 years: 9.0 30–39 years: 7.0 40–49 years: 11.0 50–59 years: 16.0 |
||||||
| Orgasmic problem | Orgasmic disorder | 6 | 18–29 years: 5.0 30–39 years: 5.0 40–49 years:6.0 50–59 years: 5.0 60–67 years: 14 |
||||||
| Orgasmic problem | Orgasmic disorder | 3 | 18–29 years: 6.0 30–39 years: 4.0 40–49 years: 8.0 50–59 years: 13.0 |
||||||
| Reduced sexual desire | HSDD | 16 | 18–29 years: 15.0 30–39 years: 19.0 40–49 years: 13.0 50–59 years: 13.0 60–67 years: 26 |
||||||
| Reduced sexual desire | HSDD | 11 | 18–29 years: 12.0 30–39 years: 13.0 40–49 years: 14.0 50–59 years: 19.0 |
||||||
| Poland | |||||||||
| Jankowaska et al. (2008) | NS | Polish version of AMS scale | ≥6 | Sexual problems | 32–45 years: 69.9 46–55 years: 96.6 56–65 years: 100 66–79 years: 100 |
(+) Age (-) Educational level |
|||
| 6–7 | Mild | 32–45 years: 22.8 46–55 years: 14.9 56–65 years: 2.5 66–79 years: 0 |
|||||||
| 8–10 | Mod | 32–45 years: 28.7 46–55 years: 32.4 56–65 years: 12.3 66–79 years: 5.0 |
|||||||
| ≥11 | Severe | 32–45 years: 18.4 46–55 years: 49.3 56–65 years: 85.2 66–79 years: 95.0 |
|||||||
| Portugal | |||||||||
| Gomes et al. (2013) | 2008–2010 | SAQ; Portuguese version of IIEF | Sometimes to always erection difficulties | NS | ED | 21.1 | 18–70 years: 21.1 | (+) Age (ED, HSD & DE) (-) Educational level (DE) |
Age (PE), length of current relationship, educational level (ED, HSD, PE), and marital status |
| Sometimes and about half of the time erection difficulties | NS | Mild ED | 10.9 | 18–24 years: 11 25–34 years: 7 35–44 years: 12 45–54 years: 23 ≥55 years: 39 |
|||||
| Most times and almost always erection difficulties | Mod to severe ED | 10.2 | 18–24 years: 2 25–34 years: 1 35–44 years: 6 45–54 years: 12 ≥55 years: 21 |
||||||
| Sometimes to always rapid ejaculation | PE | 45.2 | 18–70 years: 45.2 | ||||||
| Sometimes and about half of the time rapid ejaculation | Mild PE | 22.5 | 18–24 years: 40 25–34 years: 45 35–44 years: 43 45–54 years: 48 ≥55 years: 49 |
||||||
| Most times and almost always rapid ejaculation | Mod to severe PE | 23.1 | 18–24 years: 23 25–34 years: 28 35–44 years: 23 45–54 years: 20 ≥55 years: 22 |
||||||
| Sometimes to always orgasmic difficulties | DE | 17.5 | 18–70 years: 17.5 | ||||||
| Sometimes and about half of the time orgasmic difficulties | Mild DE | 9.4 | 18–24 years: 12 25–34 years: 9 35–44 years: 11 45–54 years: 17 ≥55 years: 30 |
||||||
| Most times and almost always orgasmic difficulties | Mod to severe DE | 8.2 | 18–24 years: 8 25–34 years: 4 35–44 years: 8 45–54 years: 3 ≥55 years: 14 |
||||||
| Sometimes to always low sexual desire | HSDD | 17.2 | 18–70 years: 17.2 | ||||||
| Sometimes and about half of the time low sexual desire | Mild low HSDD | 14.3 | 18–24 years: 11 25–34 years: 4 35–44 years: 8 45–54 years: 17 ≥55 years: 34 |
||||||
| Most times and almost always low sexual desire | Mod to severe HSDD | 2.9 | 18–24 years: 2 25–34 years: 1 35–44 years: 1 45–54 years: 1 ≥55 years: 7 |
||||||
| Republic of Moldova | |||||||||
| Dumbraveanu et al. (2018) | 2015–2016 | IAQ; IIEF-5 | NS | NS | ED | 47.1 | 18–29 years: 17.2 30–39 years: 26.9 40–49 years: 52.0 50–64 years: 72.5 ≥65 years: 88.8 |
(+) Age (+) Nocturia (+) LUTS |
|
| Mild ED | 22.0 | 18–29 years: 11.9 30–39 years: 17.3 40–49 years: 30.2 50–64 years: 28.9 ≥65 years: 18.7 |
|||||||
| Mild to Mod ED | 12.4 | 18–29 years: 3.0 30–39 years: 5.8 40–49 years: 14.0 50–64 years: 22.0 ≥65 years: 21.5 |
|||||||
| Mod ED | 7.6 | 18–29 years: 1.4 30–39 years: 2.7 40–49 years: 5.5 50–64 years: 15.7 ≥65 years: 17.8 |
|||||||
| Severe ED | 5.1 | 18–29 years: 0.7 30–39 years: 1.2 40–49 years: 2.2 50–64 years: 5.9 ≥65 years: 30.8 |
|||||||
| Spain | |||||||||
| Castellanos-Torres et al. (2013) | 2009 | Interview | Feelings after sexual relations | Year | Low satisfaction | 8.7 | 16–29 years: 5.3 30–44 years: 5.0 45–64 years: 4.7 ≥65 years: 6.9 |
(-) Collaborate economically in supporting family (-) Good health (+) Manual working class (+) Desire low frequency of sex |
Age, caring for children, take time to look after oneself, and share in doing domestics tasks |
| Riuz-Munoz et al. (2013) | 2009 | Interview | Dissatisfaction with sexual life | All time | Low satisfaction | 10.1 | 16–24 years: 12.3 25–34 years: 9.8 35–44 years: 9.2 |
(-) Parity (All time) (-) Regular partner (year) (+) From under-developed country (year) |
Age, education, developed country (year), and casual partner age (year) |
| Dissatisfaction with sexual intercourse | Year | Low satisfaction | 5.1 | 16–24 years: 6.6 25–34 years: 5.3 35–44 years: 4.1 |
|||||
| Sweden | |||||||||
| Beckman et al. (2008) | 1976–77; 2000–01 | Interview | NS | NS | ED | 12.0 | 70 years: 12.0 | (-) Sampling year (ED) | Sampling year (PE) |
| 1976–1977 | 18.1 | 70 years: 18.1 | |||||||
| 2000–2001 | 8.3 | 70 years: 8.3 | |||||||
| 1976–77 & 2000–2001 | Interview | Premature ejaculation | NS | PE | 3.7 | 70 years: 3.7 | |||
| 1976–1977 | 3.6 | 70 years: 3.6 | |||||||
| 2000–2001 | 3.8 | 70 years: 3.8 | |||||||
| 1976–77; 2000–01 | Interview | Low/no satisfaction | Low satisfaction | 6.0 | 70 years: 6.0 | ||||
| Spetz Holm et al. (2012) | 2010 | SAQ; Modified Swedish translated ADAM | Less strong erection | ED | 16.6 | 35 years: 12.5 45 years: 19.5 |
(+) Age | Age (HSDD) and BT (ED) | |
| Decrease in libido | HSDD | 21.2 | 35 years: 18.3 45 years: 23.0 |
||||||
| United Kingdom | |||||||||
| Mitchell et al. (2013) | 2010–2012 | SAQ | Trouble getting and keeping an erection | ED | 12.9 | 16–24 years: 7.6 24–34 years: 7.9 35–44 years: 7.9 45–54 years: 13.4 55–64 years: 23.5 65–74 years: 30.0 |
(+) Age | ||
| Low sexual function | Low sexual function | 16–24 years: 14.1 24–34 years: 16.6 35–44 years: 21.2 45–54 years: 18.4 55–64 years: 27.8 65–74 years: 27.0 |
(+) Age (+) Unemployment (+) Depression (+) Poor health (-) Living with partner (+) Isolated (+) Unhappy to partner (+) Cannot talk about sex with a partner (+) Regret and distress at first time sex and past month (+) Same sex partner in last 5 years (+) Paying for sex in past year (+) Nonvolitional sex (+) STIs |
Deprived area of residence | |||||
| Anyone or more of sexual problems | SP | 41.6 | 16–24 years: 36.2 24–34 years: 39.7 35–44 years: 40.3 45–54 years: 40.1 55–64 years: 48.1 65–74 years: 53.5 |
(+) Age | |||||
| Any two or more of sexual problems | SP | 13.8 | 16–24 years: 13.6 24–34 years: 14.9 35–44 years: 13.9 45–54 years: 11.7 55–64 years: 15.7 65–74 years: 13.0 |
Age | |||||
| Reached climax too quickly | PE | 14.9 | 16–24 years: 16.5 24–34 years: 19.1 35–44 years: 15.8 45–54 years: 13.6 55–64 years: 10.0 65–74 years: 10.8 |
(-) Age | |||||
| Difficulty in reaching climax | DE | 9.2 | 16–24 years: 9.2 24–34 years: 9.8 35–44 years: 8.3 45–54 years: 7.9 55–64 years: 10.6 65–74 years: 10.4 |
Age | |||||
| Lacked interest in sex | HSSD | 14.9 | 16–24 years: 11.5 24–34 years: 14.5 35–44 years: 17.2 45–54 years: 15.3 55–64 years: 16.0 65–74 years: 13.6 |
Age | |||||
| Physical pain in sex | Sex painful | 1.8 | 16–24 years: 1.8 24–34 years: 1.7 35–44 years: 1.8 45–54 years: 2.0 55–64 years: 1.9 65–74 years: 1.0 |
Age | |||||
| Felt anxious during sex | Anxiety | 5.4 | 16–24 years: 5.7 24–34 years: 6.3 35–44 years: 5.8 45–54 years: 4.4 55–64 years: 5.5 65–74 years: 3.8 |
Age | |||||
| Lack enjoyment in sex | Sex not pleasurable | 4.8 | 16–24 years: 5.4 24–34 years: 6.7 35–44 years: 5.0 45–54 years: 3.3 55–64 years: 4.6 65–74 years: 1.8 |
Age | |||||
| Lee et al. (2016) | 2012–2013 | SAQ; ELSA SRA-Q | Erectile difficulties | ED | 39.2 | 50–59 years: 15.5 60–69 years: 35.5 70–79 years: 66.1 80–89 years: 88.3 |
(+) Age (ED & DE) (+) High BP (ED) (+) Arthritis (ED & HSDD) (+) CVD (ED) (+) Diabetes (ED) (+) Asthma (ED) (+) Poor health (ED, DE & HSDD) (+) dissatisfaction with overall sex life (+) Depression (ED) |
Age (satisfaction), High BP (DE & HSDD), arthritis (DE & HSDD), CVD (HSDD), and poor health (HSDD) | |
| Compared with previous year decreased level of sexual drive/desire | HSDD | 32.3 | 50–59 years: 24.2 60–69 years: 30.1 70–79 years: 42.6 80–89 years: 49.1 |
||||||
| Difficulty achieving orgasm | DE | 15.6 | 50–59 years: 8.3 60–69 years: 14.9 70–79 years: 33.2 80–89 years: 52.2 |
||||||
| Dissatisfied with overall sexual life | Low satisfaction | 19.9 | 50–59 years: 18.7 60–69 years: 22.5 70–79 years: 20.2 80–89 years: 19.2 |
||||||
| Mitchell et al. (2016) | 2010–2012 | SAQ | Difficulty getting and keeping an erection | ED | 7.8 | 16–21 years: 7.8 | NA | ||
| Anyone of sexual problems | SP | 33.8 | 16–21 years: 33.8 | ||||||
| Reached climax too quickly | PE | 13.2 | 16–21 years: 13.2 | ||||||
| Difficulty in reaching climax | DE | 8.3 | 16–21 years: 8.3 | ||||||
| Lacked interest in sex | HSDD | 10.5 | 16–21 years: 10.5 | ||||||
| Physical pain in sex | Sex painful | 1.9 | 16–21 years: 1.9 | ||||||
| Felt anxious during sex | Anxiety | 4.8 | 16–21 years: 4.8 | ||||||
| Lack enjoyment in sex | Sex not pleasurable | 5.4 | 16–21 years: 5.4 | ||||||
Note. AD = androgen deficiency; ADAM = Androgen Deficiency Assessment Module; AIPE = Arabic Index of Premature Ejaculation; AMS = The Aging Male’s Symptoms Scale; BMSFI = Brief Manual of Sexual Function Inventory; cFT = circulating free testosterone; ED = erectile dysfunction; EMAS SFQ = European Male Aging Study Sexual Function Questionnaire; ELSA SRA-Q = European Longitudinal Study of Aging Sexual Function Assessment Questionnaire; EPIC = The Expanded Prostate Cancer Index Composite; DE = delayed ejaculation; DSM-IV = Manual of Mental Disorder-IV; GDS-15 = 15-Item Geriatric Depression Scale; HSDD = hypoactive sexual desire disorder; IIEF-5 = 5-Items International Index of Erectile Dysfunction; IIEF-EF = International Index of Erectile Dysfunction – erectile function section; IELT = intravaginal ejaculation latency time; IPSS = International Prostate Symptom Score; ISSM = International Society for Sexual Medicine; LOH = late onset hypogonadism; Mod = moderate; MPD = male pelvic dysfunction; MSHQ-4 = Male Sexual Health Questionnaire; NATSAL 2000 = The National Survey of Sexual Attitudes and Lifestyles 2000; NS = not stated; PE = premature ejaculation; PEDT = Premature Ejaculation Diagnosis Tool; PEP = Premature Ejaculation Profile; SAc = sexual activity; SDI-2 = Sexual Desire Inventory 2; SFS = sexual function screener; SI = sexual inactivity; and SP = sexual problem.
Single question.
With prostate like symptoms.
Study two.
BMI: <25.
BMI: 25–29.9.
BMI: ≥30.
Robust.
Prefrail.
Frail.
Partnered.
Single.
Chronic prostatitis.
The most investigated MSDs included ED, various types of ED, ejaculation dysfunctions (PE and DE), and HSDD in both the Asian and European studies. A total of 19 Asian studies presented the prevalence of ED (Çayan et al., 2017; Chung et al., 2015; Ghalayini et al., 2010; Hao et al., 2011; Huang et al., 2014; Hwang et al., 2010; Jeong et al., 2011; Khoo et al., 2008; Kim et al., 2009; Liu et al., 2010; Permpongkosol et al., 2008; Quek et al., 2008; Rao et al., 2015; Tang et al., 2015; Wong et al., 2009a; 2009b; 2016; Zhang et al., 2013, 2017), including eight studies that also presented different types of ED (Çayan et al., 2017; Chung et al., 2015; Khoo et al., 2008; Permpongkosol et al., 2008; Rao et al., 2015; Tang et al., 2015; Wong et al., 2009a; 2009b). A total of seven Asian studies covered ejaculation dysfunction (Lee et al., 2013; Liang et al., 2010; Park et al., 2010; Quek et al., 2008; Rao et al., 2015; Serefoglu et al., 2011; Zhang et al., 2013), while four studies discussed HSDD (Kim et al., 2009; Liu et al., 2010; Rao et al., 2015; Zhang et al., 2013). Twenty studies investigated the prevalence of ED in European populations (Andersen et al., 2008; Beckman et al., 2008; Christensen et al., 2011; Corona et al., 2010; Donnelly et al., 2018; Dumbraveanu et al., 2018; Hendrickx et al., 2016; Jern et al., 2012; Holm et al., 2012; Kontula & Haavio-Mannila, 2009; Korfage et al., 2008; Landripet & Stulhofer, 2015; 2013, 2016; Mitchell et al., 2013; 2016; Moreau et al., 2016; Quinta Gomes & Nobre, 2014; Sand et al., 2008; Traeen & Stigum, 2010), and four of them also discussed the various types of ED (Corona et al., 2010; Dumbraveanu et al., 2018; Jern et al., 2012; Quinta Gomes & Nobre, 2014). A total of eight studies investigated ejaculation dysfunction (Andersen et al., 2008; Beckman et al., 2008; Hendrickx et al., 2016; Holm et al., 2012; Lee et al., 2016; Mitchell et al., 2013, 2016; Moreau et al., 2016; Quinta Gomes & Nobre, 2014; Traeen & Stigum, 2010), and 13 studies discussed HSDD (Andersen et al., 2008; Beutel et al., 2018; Carvalheira et al., 2014; Hendrickx et al., 2016; Korfage et al., 2008; Landripet & Stulhofer, 2015; Lee et al., 2016; Mitchell et al., 2013, 2016; Moreau et al., 2016; Quinta Gomes & Nobre, 2014; Traeen & Stigum, 2010). In the Asian and European populations, there were 23 and 24 studies, respectively, that discussed at least one associated factor of MSD (Table 1).
Prevalence of Sexual Dysfunctions
Erectile Dysfunction
Table 1 presents that the prevalence of ED was 0% to 95.0% of Asian men. The prevalence of ED was 0% to 88.2% and 7% to 95.0% for men <60 years (Çayan et al., 2017; Ghalayini et al., 2010; Hao et al., 2011; Huang et al., 2014; Hwang et al., 2010; Jeong et al., 2011; Khoo et al., 2008; Kim et al., 2009; Liu et al., 2010; Permpongkosol et al., 2008; Quek et al., 2008; Tang et al., 2015; Zhang et al., 2013, 2016, 2017) and >60 years (Çayan et al., 2017; Chung et al., 2015; Ghalayini et al., 2010; Huang et al., 2014; Hwang et al., 2010; Jeong et al., 2011; Khoo et al., 2008; Liu et al., 2010; Permpongkosol et al., 2008; Quek et al., 2008; Rao et al., 2015; Tang et al., 2015; Wong et al., 2009a; Zhang et al., 2016; 2017), respectively. The prevalence of ED in Asian men <60 years was lowest for 18–29 years (0%–6.3%) (Hwang et al., 2010; Quek et al., 2008; Zhang et al., 2016), followed by 30–39 years (0.8%–41.4%) (Ghalayini et al., 2010; Hwang et al., 2010; Quek et al., 2008; Zhang et al., 2013, 2016), 40–49 years (1%–55.3%) (Çayan et al., 2017; Ghalayini et al., 2010; Hwang et al., 2010; Liu et al., 2010; Permpongkosol et al., 2008; Quek et al., 2008; Tang et al., 2015; Zhang et al., 2016; Zhang et al., 2013, 2017) and 50–59 years (3%–88.2%) (Çayan et al., 2017; Ghalayini et al., 2010; Huang et al., 2014; Hwang et al., 2010; Khoo et al., 2008; Liu et al., 2010; Permpongkosol et al., 2008; Quek et al., 2008; Tang et al., 2015; Zhang et al., 2016, 2017). The prevalence of ED was 7% to 91.8%, and 15% to 95% for men 60–69 years (Çayan et al., 2017; Ghalayini et al., 2010; Huang et al., 2014; Hwang et al., 2010; Khoo et al., 2008; Liu et al., 2010; Tang et al., 2015; Zhang et al., 2017) and ≥70 years (Çayan et al., 2017; Ghalayini et al., 2010; Hwang et al., 2010; Khoo et al., 2008; Liu et al., 2010; Zhang et al., 2017), respectively.
The overall prevalence of ED in European men was 0.9% to 88.8%. European men <60 years had a prevalence of 0.9% to 52% (Andersen et al., 2008; Christensen et al., 2011; Corona et al., 2010; Dumbraveanu et al., 2018; Hendrickx et al., 2016; Holm et al., 2012; Jern et al., 2012; Kontula & Haavio-Mannila, 2009; Korfage et al., 2008; Landripet & Stulhofer, 2015; Lee et al., 2016; Mitchell et al., 2013, 2016; Moreau et al., 2016; Quinta Gomes & Nobre, 2014; Sand et al., 2008; Traeen & Stigum, 2010), while men >60 years had a prevalence of 8.3% to 88.8% (Andersen et al., 2008; Beckman et al., 2008; Christensen et al., 2011; Corona et al., 2010; Donnelly et al., 2018; Dumbraveanu et al., 2018; Hendrickx et al., 2016; Jern et al., 2012; Kontula & Haavio-Mannila, 2009; Korfage et al., 2008; Landripet & Stulhofer, 2015; Lee et al., 2013; Mitchell et al., 2013; Moreau et al., 2016; Quinta Gomes & Nobre, 2014; Sand et al., 2008; Holm et al., 2012; Traeen & Stigum, 2010). The age groups showed that the European men <60 years in the age group 18–29 years had a prevalence of ED ranging from 5% to 17.2% (Dumbraveanu et al., 2018; Sand et al., 2008; Traeen & Stigum, 2010), which became 3% to 26.9% for 30–39 years (Dumbraveanu et al., 2018; Sand et al., 2008; Traeen & Stigum, 2010) and 4% to 52% in men 40–49 years (Corona et al., 2010; Dumbraveanu et al., 2018; Holm et al., 2012; Sand et al., 2008; Traeen & Stigum, 2010). European men 50–59 years had a prevalence that varied from 5% to 22% (Christensen et al., 2011; Corona et al., 2010; Lee et al., 2016; Sand et al., 2008; Traeen & Stigum, 2010), followed by 60–69 years (14.6%–35.9%) (Corona et al., 2010; Donnelly et al., 2018; Korfage et al., 2008; Lee et al., 2016; Sand et al., 2008; Traeen & Stigum, 2010), ≥70 years (8.3%–66.1%) (Beckman et al., 2008; Corona et al., 2010; Donnelly et al., 2018; Korfage et al., 2008; Lee et al., 2016; Sand et al., 2008), and ≥80 years (60.8%–88.3%) (Donnelly et al., 2018; Lee et al., 2016) (Table 1).
Mild Erectile Dysfunction
According to Table 1, the overall prevalence of mild ED was 2.5% to 77% in Asian men. The prevalence of mild ED ranged from 2.5% to 36.8% and 10.5% to 77% in men <60 years (Çayan et al., 2017; Ghalayini et al., 2010; Hao et al., 2011; Khoo et al., 2008; Permpongkosol et al., 2008; Tang et al., 2015) and >60 years (Çayan et al., 2017; Chung et al., 2015; Khoo et al., 2008; Permpongkosol et al., 2008; Rao et al., 2015; Tang et al., 2015; Wong et al., 2009a; 2009b), respectively. The prevalence of mild ED for Asian men <60 years was lowest in the age group 40–49 years (2.5%–35%) (Çayan et al., 2017; Permpongkosol et al., 2008; Tang et al., 2015), followed by 50–59 years (10.5%–36.8%) (Çayan et al., 2017; Khoo et al., 2008; Permpongkosol et al., 2008; Tang et al., 2015). The prevalence of mild ED was 23.6% to 38.5% and 28.1% to 30.0% for men 60–69 years (Çayan et al., 2017; Khoo et al., 2008; Permpongkosol et al., 2008; Tang et al., 2015) and ≥70 years (Çayan et al., 2017; Khoo et al., 2008), respectively.
The overall prevalence of mild ED for European men was 7% to 39%. European men <60 years had a prevalence of 7% to 39% (Dumbraveanu et al., 2018; Jern et al., 2012; Quinta Gomes & Nobre, 2014), while men >60 years had a prevalence of 18.7% (Dumbraveanu et al., 2018). The age groups showed that European men <60 years in the age group 18–29 years had a prevalence of mild ED ranged from 11% to 11.9% (Dumbraveanu et al., 2018; Quinta Gomes & Nobre, 2014), which became 17.3% for 30–39 years (Dumbraveanu et al., 2018) and 30.2% in men 40–49 years (Dumbraveanu et al., 2018) (Table 1).
Mild to Moderate Erectile Dysfunction
For Asian men, the overall prevalence of mild to moderate ED was 5% to 31.6%. The prevalence of mild to moderate ED was 16.7% and 5% to 31.6% in men <60 years (Hwang et al., 2010; Khoo et al., 2008) and >60 years (Hwang et al., 2010; Khoo et al., 2008; Rao et al., 2015), respectively. The prevalence of mild to moderate ED for Asian men <60 years was lowest (16.7%) in 50–59 years (Khoo et al., 2008). The prevalence of mild to moderate ED was 5% and 28.9% for men 60–69 years (Khoo et al., 2008) and ≥70 years (Khoo et al., 2008), respectively (Table 1).
The overall prevalence of mild to moderate ED for European men was 1.6% to 22%. European men <60 years had a prevalence of 1.6% to 22% (Dumbraveanu et al., 2018; Jern et al., 2012), while men >60 years had a prevalence of 21.5% (Dumbraveanu et al., 2018). The age groups showed that European men <60 years in the age group 18–29 years had a prevalence of mild to moderate ED of 3%, which increased to 5.8% for 30–39 years and 14% in men 40–49 years (Dumbraveanu et al., 2018) (Table 1).
Moderate Erectile Dysfunction
For Asian men, the overall prevalence of moderate ED was 0.3% to 36.8%. The prevalence of moderate ED was 0.3% to 16.9% and 5% to 36.8% in men <60 years (Çayan et al., 2017; Ghalayini et al., 2010; Hao et al., 2011; Hwang et al., 2010; Khoo et al., 2008; Permpongkosol et al., 2008; Tang et al., 2015) and >60 years (Çayan et al., 2017; Chung et al., 2015; Khoo et al., 2008; Permpongkosol et al., 2008; Rao et al., 2015; Tang et al., 2015; Wong et al., 2009a; 2009b), respectively. The prevalence of moderate ED for Asian men <60 years was lowest (0.29%–8.2%) for men 40–49 years (Çayan et al., 2017; Permpongkosol et al., 2008; Tang et al., 2015), followed by 1.6% to 16.9% in 50–59 years (Çayan et al., 2017; Khoo et al., 2008; Permpongkosol et al., 2008; Tang et al., 2015). The prevalence of moderate ED was 5% to 9.7%, and 6.6% to 26% for men 60–69 years (Çayan et al., 2017; Khoo et al., 2008; Permpongkosol et al., 2008; Tang et al., 2015) and ≥70 years (Çayan et al., 2017; Khoo et al., 2008), respectively (Table 1).
The overall prevalence of moderate ED for European men was 0.4% to 29%. European men <60 years had a prevalence of 0.4% to 14.1% (Corona et al., 2010; Dumbraveanu et al., 2018; Jern et al., 2012), while men >60 years had a prevalence of 17.8% to 29% (Corona et al., 2010; Dumbraveanu et al., 2018). The age groups showed that European men <60 years in the age group 18–29 years had a prevalence of moderate ED of 1.4% (Dumbraveanu et al., 2018), which increased to 2.7% in 30–39 years (Dumbraveanu et al., 2018), 4.5% to 5.5% in 40–49 years (Corona et al., 2010; Dumbraveanu et al., 2018), and 14.1% for men 50–59 years (Corona et al., 2010) (Table 1). The prevalence of moderate ED was 23% and 29% for men 60–69 years and ≥70 years, respectively (Corona et al., 2010).
Severe Erectile Dysfunction
For Asian men, the overall prevalence of severe ED was 0.1% to 58.4%. The prevalence of severe ED was 0.1% to 50.1% and 0.8% to 58.4% in men <60 years (Çayan et al., 2017; Ghalayini et al., 2010; Hao et al., 2011; Hwang et al., 2010; Khoo et al., 2008; Permpongkosol et al., 2008; Tang et al., 2015) and >60 years (Çayan et al., 2017; Chung et al., 2015; Khoo et al., 2008; Permpongkosol et al., 2008; Rao et al., 2015; Tang et al., 2015; Wong et al., 2009a; 2009b), respectively. The prevalence of severe ED for Asian men <60 years was lowest (0.1% to 12.2%) in 40–49 years (Çayan et al., 2017; Permpongkosol et al., 2008; Tang et al., 2015) and increased to 0.5% to 50.1% in 50–59 years (Çayan et al., 2017; Khoo et al., 2008; Permpongkosol et al., 2008; Tang et al., 2015). The prevalence of severe ED was 0.8% to 58.4% and 14.9% to 25% for men 60–69 years (Çayan et al., 2017; Khoo et al., 2008; Permpongkosol et al., 2008; Tang et al., 2015) and ≥70 years (Çayan et al., 2017; Khoo et al., 2008), respectively (Table 1).
The overall prevalence of severe ED for European men was 0% to 35%. European men <60 years had a prevalence of 0% to 4.8% (Corona et al., 2010; Dumbraveanu et al., 2018; Jern et al., 2012), while men >60 years had a prevalence of 15% to 35% (Corona et al., 2010; Dumbraveanu et al., 2018). The age groups showed that European men <60 years in the age group 18–29 years had a prevalence of severe ED of 0.7% (Dumbraveanu et al., 2018), which increased to 1.2% in 30–39 years (Dumbraveanu et al., 2018), 0.6% to 2.2% in 40–49 years (Corona et al., 2010; Dumbraveanu et al., 2018), and 4.8% in 50–59 years (Corona et al., 2010) (Table 1). The prevalence of severe ED was 15% and 35% for men 60–69 years and ≥70 years, respectively (Corona et al., 2010) (Table 1).
Orgasmic Dysfunction
The prevalence of anorgasmia was 0.4% and 3% to 65% in Asian (Rao et al., 2015) and European (Christensen et al., 2011; Corona et al., 2010) men, respectively. Other orgasmic dysfunctions were not reported in any of the Asian studies. The overall prevalence of orgasmic dysfunctions ranged from 4% to 64.2% in European men. The prevalence of orgasmic dysfunction was 4% to 13% and 7.3% to 64.2% for European men <60 years (Corona et al., 2010; Donnelly et al., 2018; Traeen & Stigum, 2010) and >60 years (Corona et al., 2010; Donnelly et al., 2018; Traeen & Stigum, 2010), respectively. The prevalence of orgasmic dysfunctions for European men <60 years was 5% to 6% in 18–29 years (Traeen & Stigum, 2010), 4% to 5% in 30–39 years (Traeen & Stigum, 2010), 3% to 8% in 40–49 years (Corona et al., 2010; Traeen & Stigum, 2010), and 4% to 13% in 50–59 years (Corona et al., 2010; Traeen & Stigum, 2010). The prevalence of orgasmic dysfunction was 7.3% to 15.5%, 10.1% to 13.7%, and 64.2% for European men 60–69 years (Corona et al., 2010; Donnelly et al., 2018; Traeen & Stigum, 2010), ≥70 years (Corona et al., 2010), and ≥80, respectively (Table 1).
Ejaculation Dysfunction
Table 1 presents that the prevalence of PE was 0% to 49.1% of Asian men. The prevalence of PE was 1% to 27% and 0% to 49.1% for men <60 years (Lee et al., 2013; Liang et al., 2010; Park et al., 2010; Quek et al., 2008; Serefoglu et al., 2011) and >60 years (Lee et al., 2013; Quek et al., 2008; Rao et al., 2015; Serefoglu et al., 2011), respectively. The prevalence of PE for Asian men <60 years was lowest in 18–29 years (10.7%–23.4%) (Lee et al., 2013; Park et al., 2010; Quek et al., 2008; Serefoglu et al., 2011), followed by 30–39 years (13%–24.6%) (Lee et al., 2013; Park et al., 2010; Quek et al., 2008; Serefoglu et al., 2011), 40–49 years (9.4%–30.7%) (Lee et al., 2013; Park et al., 2010; Quek et al., 2008; Serefoglu et al., 2011), and 50–59 years (1%–27.8%) (Lee et al., 2013; Quek et al., 2008; Serefoglu et al., 2011). The prevalence of PE was 35.4% to 41.8% and 49.1% for Asian men 60–69 years (Lee et al., 2013; Serefoglu et al., 2011) and ≥70 years (Serefoglu et al., 2011), respectively.
The overall prevalence of PE for European men was 2.7% to 52%. European men <60 years had a prevalence of 9.3% to 52% (Andersen et al., 2008; Hendrickx et al., 2016; Mitchell et al., 2016; Mitchell et al., 2013; Moreau et al., 2016; Quinta Gomes & Nobre, 2014; Traeen & Stigum, 2010), while men >60 years had a prevalence of 3.6% to 28%. The age groups showed that European men <60 years in the age group 18–29 years had a prevalence of PE that ranged from 24% to 28%, which became 22% to 23% in 30–39 years, 19% to 30% in 40–49 years, and 24% to 33% in 50–59 years (Traeen & Stigum, 2010). European men 60–69 years had a prevalence of 28% (Traeen & Stigum, 2010), which decreased to 3.6% to 3.8% in men ≥70 years (Beckman et al., 2008) (Table 1).
The studies on Asian men did not report DE. The overall prevalence of DE was 1.1% to 52.2% for European men. The prevalence of DE was 1.1% to 16% and 11% to 52.2% for men <60 years (Andersen et al., 2008; Hendrickx et al., 2016; Landripet & Stulhofer, 2015; Lee et al., 2016; Mitchell et al., 2013, 2016; Moreau et al., 2016; Quinta Gomes & Nobre, 2014; Traeen & Stigum, 2010) and >60 years (Hendrickx et al., 2016; Lee et al., 2016; Mitchell et al., 2013; Traeen & Stigum, 2010), respectively. The prevalence of DE for European men <60 years was 9% to 10% in 18–29 years, 7% to 8% in 30–39 years, 8% to 11% in 40–49 years (Traeen & Stigum, 2010), and 7% to 16% in 50–59 years (1%–27.8%) (Lee et al., 2016; Traeen & Stigum, 2010). The prevalence of DE was 11% to 14.9%, 33.2%, and 52.2% in European men 60–69 years (Lee et al., 2016; Traeen & Stigum, 2010), ≥70 years (Lee et al., 2016) and ≥80 years (Lee et al., 2016), respectively (Table 1). Anejaculation and retrograde ejaculation were not reported in any of the Asian studies. A European study reported that the prevalence of retrograde ejaculation ranged from 1.4% to 1.8% (Hendrickx et al., 2016).
Sexual Desire Disorder
The overall prevalence of HSDD was 0.7% to 81.4% of Asian men. The prevalence of HSDD was 7% to 50.4% and 0.7% to 81.4% for men <60 years (Kim et al., 2009; Liu et al., 2010; Zhang et al., 2013) and >60 years (Liu et al., 2010; Rao et al., 2015), respectively. The prevalence of HSDD for Asian men <60 years was lowest in 30–39 years (7%) (Zhang et al., 2013), followed by 40–49 years (10.3%–50.4%) (Liu et al., 2010; Zhang et al., 2013), and 50–59 years (48.1%) (Liu et al., 2010). The prevalence of HSDD was 57% and 81.4% of Asian men 60–69 years and ≥70 years, respectively (Liu et al., 2010).
The overall prevalence of HSDD for European men was 0% to 65.5%. European men <60 years had a prevalence of 0% to 37.4% (Andersen et al., 2008; Beutel et al., 2018; Carvalheira et al., 2014; Hendrickx et al., 2016; Holm et al., 2012; Kontula & Haavio-Mannila, 2009; Korfage et al., 2008; Landripet & Stulhofer, 2015; Lee et al., 2016; Mitchell et al., 2013, 2016; Moreau et al., 2016; Quinta Gomes & Nobre, 2014; Traeen & Stigum, 2010), while men >60 years had a prevalence of 0.2% to 65.5% (Beutel et al., 2018; Kontula & Haavio-Mannila, 2009; Korfage et al., 2008; Lee et al., 2016; Mitchell et al., 2013; Traeen & Stigum, 2010). The age groups showed that the European men <60 years in the age group 18–29 years had a prevalence of HSDD ranging from 3.3% to 22% (Carvalheira et al., 2014; Traeen & Stigum, 2010), which became 5.7% to 26.2% in 30–39 years (Carvalheira et al., 2014; Traeen & Stigum, 2010), 3.4% to 27.5% in 40–49 years (Carvalheira et al., 2014; Traeen & Stigum, 2010), and 1.8% to 29.9% in 50–59 years (Carvalheira et al., 2014; Lee et al., 2016; Traeen & Stigum, 2010). European men 60–69 years had a prevalence varying from 41.4% to 46.1% (Korfage et al., 2008; Lee et al., 2016; Traeen & Stigum, 2010) and 37.9% to 65.5% in men ≥70 years (Beutel et al., 2018; Korfage et al., 2008; Lee et al., 2016). The prevalence of HSDD was 49.1% for men ≥80 years (Lee et al., 2016) (Table 1).
None of the Asian studies reported data on hyperactive sexual desire disorder, while only one European study reported that the prevalence varied from 1.7% to 2.7% (Hendrickx et al., 2016). Sexual aversion was also not reported in any of the Asian studies. The prevalence of sexual aversion was 0.9% in European men (Hendrickx et al., 2016).
Androgen Deficiency
Table 1 presents that the overall prevalence of androgen deficiency (AD) was 4.6% to 63% of Asian men (Khoo et al., 2008; Tang et al., 2015). The prevalence of AD was 4.6% to 43.1% and 13.9% to 63% for men <60 years (Khoo et al., 2008; Tang et al., 2015) and >60 years (Khoo et al., 2008; Tang et al., 2015), respectively. The prevalence of AD for Asian men <60 years was lowest in 40–49 years (4.6%–30.3%) (Tang et al., 2015), followed by 50–59 years (6.9%–43.1%) (Khoo et al., 2008; Tang et al., 2015). The prevalence of AD was 13.9% to 57.4% and 63% of Asian men 60–69 years (Khoo et al., 2008; Tang et al., 2015) and ≥70 years (Khoo et al., 2008), respectively. AD was not reported in any of the European studies.
Low Satisfaction
Low satisfaction with sexual activity was reported in 3.2% to 37.6% of Asian men >60 years (Kim & Jeon, 2013). For European men, the proportion of low satisfaction was 4.1% to 28.3%. The prevalence of low satisfaction was 4.1% to 25% and 6% to 28.3% for men <60 years (Castellanos-Torres et al., 2013; Corona et al., 2010; Kontula & Haavio-Mannila, 2009; Korfage et al., 2008; Lee et al., 2016; Ruiz-Muñoz et al., 2013) and >60 years (Beckman et al., 2008; Castellanos-Torres et al., 2013; Corona et al., 2010; Kontula & Haavio-Mannila, 2009; Korfage et al., 2008; Lee et al., 2016), respectively. The prevalence of low satisfaction for European men 40–49 years was 23.2% (Corona et al., 2010) and 18.7% to 25% for 50–59 years (Corona et al., 2010; Lee et al., 2016). The prevalence of low satisfaction was 18.8% to 27.2% and 6% to 28.3% for European men 60–69 years (Corona et al., 2010; Korfage et al., 2008; Lee et al., 2016) and ≥70 years (Beckman et al., 2008; Corona et al., 2010; Korfage et al., 2008; Lee et al., 2016), respectively. The prevalence of low satisfaction was 19.2% in European men ≥80 years (Lee et al., 2016).
Reduced/No Sexual Pleasure and Painful Intercourse
None of the Asian studies reported the prevalence of reduced/no sexual pleasure. The prevalence was 3.3% to 26% and 1.8% to 52.2% for European men <60 years (Mitchell et al., 2013, 2016; Moreau et al., 2016) and >60 years, respectively. The proportion of European men reporting reduced/no sexual pleasure increased with age to 8.3% in 50–59 years, 14.9% in 60–69 years, 33.2% in 70–79 years, and 52.2% in 80–89 years (Table 1). The prevalence of painful intercourse was 1.7% to 18% and 1% to 3% for European men <60 years and >60 years, respectively (Christensen et al., 2011; Mitchell et al., 2013, 2016; Moreau et al., 2016).
Method of Assessment
Table 2 presents that eight studies (Asian = 4; European = 4) used interviews and that these studies reported a prevalence of ED of 1%–77% and 3%–37% of Asian (Chung et al., 2015; Hwang et al., 2010; Permpongkosol et al., 2008; Zhang et al., 2013) and European (Beckman et al., 2008; Moreau et al., 2016; Sand et al., 2008; Traeen & Stigum, 2010) men, respectively. A total of 12 Asian (Çayan et al., 2017; Ghalayini et al., 2010; Hao et al., 2011; Huang et al., 2014; Hwang et al., 2010; Jeong et al., 2011; Khoo et al., 2008; Liu et al., 2010; Quek et al., 2008; Rao et al., 2015; Tang et al., 2015; Zhang et al., 2017) and three European (Dumbraveanu et al., 2018; Jern et al., 2012; Landripet & Stulhofer, 2015) studies used the five-item International Index of Erectile Function Questionnaire (IIEF-5) for the assessment of ED, and these studies reported a prevalence varying from 6% to 95% and 15.2% to 88.8% for Asian men and European men, respectively. Most of the Asian (n = 6) (Hao et al., 2011; Huang et al., 2014; Hwang et al., 2010; Khoo et al., 2008; Tang et al., 2015; Zhang et al., 2017) and European (n = 2) (Jern et al., 2012; Landripet & Stulhofer, 2015) studies that used IIEF-5 adopted a variable cut-off score of <22 and reported a prevalence varying from 14.5% to 95% and 15.2% to 30.8% for Asian men and European men, respectively. The Asian studies also used variable cut-off scores of <26 (n = 1; 17%–82.9%) (Çayan et al., 2017), <21 (n = 1; 6.3%–89.2) (Quek et al., 2008) and <18 (n = 1; 18.2%–60.4%) (Jeong et al., 2011). One Asian (Rao et al., 2015) and one European (Dumbraveanu et al., 2018) study did not report a cut-off score for the diagnosis of ED. Only Asian studies used a single question interview or questionnaire to assess ED (n = 5, 0%–57.2%) (Table 1).
Table 2.
Summary of Sexual Dysfunctions, and the Tools Used for the Assessment.
| Dysfunction | Instrument | Asian | European | ||
|---|---|---|---|---|---|
| n | Prevalence (%) | n | Prevalence (%) | ||
| ED | Interview | 4 | 1–77 | 4 | 3–37 |
| Questionnaire | 17 | 0–95 | 9 | 1–88.8 | |
| IIEF-5 | 11 | 6.3–95 | 3 | 15.2–88.8 | |
| IAQ; IIEF-5 | 6 | 17–95 | 1 | 17.2–88.8 | |
| SAQ; IIEF-5 | 5 | 6.3–91.8 | 2 | 15.2–30.8 | |
| Others | |||||
| IAQ; Self-developed | 2 | 56.6–88.3 | — | — | |
| SAQ; Self-developed | 3 | 0–75.9 | 5 | 1–30 | |
| IAQ; EHS | 1 | 11–67 | — | — | |
| SAQ; ADAM | — | — | 1 | 12.5–19.5 | |
| SAQ; ELSA SRA | — | — | 1 | 15.5–88.3 | |
| SAQ; EMAS SFQ-14 | — | — | 2 | 5.2–77.4 | |
| SAQ; EPIC-26 | — | — | 1 | 9.4–60.8 | |
| SAQ; GSSAB | — | — | 1 | 14.2–28.3 | |
| SAQ; SFS | — | — | 1 | 0.9–41.3 | |
| SAQ; IIEF full version | — | — | 1 | 21.1 | |
| PE | Interview | — | — | 3 | 3.6–52 |
| Questionnaire | 6 | 3.3–49.1 | 5 | 2.7–45.2 | |
| IAQ; PEDT | 2 | 10.0–49.1 | — | — | |
| SAQ; PEDT | 1 | 11.3 | — | — | |
| SAQ; Self-developed | 3 | 3.3–41.8 | 3 | 10–28.6 | |
| SAQ; SFS | — | — | 1 | 2.7–10.7 | |
| SAQ; IIEF | — | — | 1 | 45.2 | |
| IELT | 2 | 0–35.4 | — | — | |
| DE | Interview | — | — | 2 | 7–17 |
| Questionnaire | — | — | 7 | 1.3–52.2 | |
| SAQ; Self-developed | 3 | 1.1–10.6 | |||
| SAQ; SFS | — | — | 1 | 1.3–10.7 | |
| SAQ; IIEF | — | — | 1 | 17.5 | |
| SAQ; ELSA SRA | — | — | 1 | 8.3–52.2 | |
| SAQ; GSSAB | — | — | 1 | 6.2–19.9 | |
| HSDD | Interview | 1 | 7.0–17.2 | 2 | 12–28 |
| Questionnaire | 3 | 0.8–81.4 | 12 | 0–65.5 | |
| IAQ; Self-developed | 1 | 0.8 | 1 | 0–65.5 | |
| IAQ; IIEF | 1 | 48.1–81.4 | 1 | 17.2 | |
| SAQ; Self-developed | 1 | 12.2 | 4 | 1.6–30 | |
| SAQ; SFS | — | — | 1 | 1.8–7.3 | |
| SAQ; NASTAL | — | — | 1 | 0.2–29.9 | |
| SAQ; GSSAB | — | — | 1 | 12.8–37.4 | |
| SAQ; Dutch module SAc | — | — | 1 | 40.8–57.7 | |
| SAQ; ADAM | — | — | 1 | 18.3–23.0 | |
| SAQ; ELSA SRA | — | — | 1 | 24.2–49.1 | |
| Anorgasmia | Questionnaire | 1 | 0.4 | 2 | 3–65 |
| IAQ; Self-developed | 1 | 0.4 | — | — | |
| SAQ; Self-developed | — | — | 1 | 23–65 | |
| SAQ; EMAS-SFQ-14 | — | — | 1 | 3–11 | |
| Orgasmic dysfunction | Interview | 1 | 5–14 | 1 | 4–14 |
| Questionnaire | — | — | 2 | 4.0–64.2 | |
| SAQ; EPIC | — | — | 1 | 8.9–64.2 | |
| SAQ; EMAS-SFQ-14 | — | — | 1 | 4.0–18.7 | |
| Low satisfaction | Interview | 1 | 3.2–37.6 | 3 | 4.1–12.3 |
| Questionnaire | — | — | 5 | 13.3–28.3 | |
| SAQ; Self-developed | — | — | 2 | 14.1–27.8 | |
| SAQ; Dutch module SAc | — | — | 1 | 13.3–23.2 | |
| SAQ; EMAS-SFQ-14 | — | — | 1 | 23.2–28.3 | |
| SAQ; ELSA SRA | — | — | 1 | 18.7–22.5 | |
| Sex painful | Interview | — | — | 1 | 13 |
| Questionnaire | — | — | 2 | 1–18 | |
| SAQ; Self-developed | — | — | 2 | 1–18 | |
| Sex not pleasurable | Interview | — | — | 1 | 26 |
| Questionnaire | — | — | 2 | 1.8–6.7 | |
| SAQ; Self-developed | — | — | 2 | 1.8–6.7 | |
Note. CESDS-11 = 11-Item Iowa form of the Center for Epidemiological Studies Depression Scale; BSFI = Brief Sexual Function Inventory; DSM-IV = Manual of Mental Disorder-IV; EMAS SFQ = European Male Aging Study Sexual Function Questionnaire; ELSA SRA-Q = European Longitudinal Study of Aging Sexual Function Assessment Questionnaire; EPIC = The Expanded Prostate Cancer Index Composite; GDS-15 = 15-Item Geriatric Depression Scale; HADS = Anxiety Subscale of the Hospital Anxiety and Depression Scale; IIEF-5 = International Index of Erectile Dysfunction; IELT = intravaginal ejaculation latency time; ISSM = International Society for Sexual Medicine; PEDT = Premature Ejaculation Diagnosis Tool; and SAc = sexual activity.
An equal number of Asian (n = 5; 0%–88.3%) (Hao et al., 2011; Kim et al., 2009; Wong et al., 2009a; 2009b; Zhang et al., 2016) and European (n = 5; 1%–30%) (Andersen et al., 2008; Christensen et al., 2011; Kontula & Haavio-Mannila, 2009; Mitchell et al., 2013; 2016) studies used a self-developed questionnaire for the assessment of ED. An Asian study (n = 1; 11%–67%) used an interviewer-assisted questionnaire (IAQ) of the erection hardness score (Hwang et al., 2010). The European studies, meanwhile, used self-administered questionnaires (SAQ) of androgen deficiency assessment module (ADAM) (n = 1; 12.5%–19.5%) (Holm et al., 2012), the English Longitudinal Study of Aging sexual relationships and activities questionnaires (ELSA SRA-Q) (n = 1; 15.5%–88.3%) (Lee et al., 2016); European Male Aging Study sexual function questionnaires (EMAS SFQ-14) (n = 2; 5.2%–77.2%) (Corona et al., 2010; Lee et al., 2013); the expanded prostate cancer index composite (EPIC-26) (n = 1; 9.4%–60.8%) (Donnelly et al., 2018); the Global Study of Sexual Attitudes and Behaviors (GSSAB) (n = 1; 14.2%–28.3%) (Landripet & Stulhofer, 2015), the Dutch module sexual activity (SAc) (n = 1; 12.0%–26.3%) (Korfage et al., 2008), the sexual functioning scale (SFS) (n = 1; 0.9%–41.3%) (Hendrickx et al., 2016), and the full version of the International Index of Erectile Function (IIEF) (n = 1; 21.1%) (Quinta Gomes & Nobre, 2014) for the assessment of ED.
A total of three European studies used interviews to diagnose PE and reported a prevalence varying from 3.6% to 52% (Beckman et al., 2008; Moreau et al., 2016; Traeen & Stigum, 2010), while six Asian and five European studies used questionnaires for the assessment of PE. A total of three Asian studies used the premature ejaculation diagnosis tool with the IAQ (n = 2; 10.0%–49.1%) or SAQ (n = 1; 11.3%) method (Lee et al., 2013; Rao et al., 2015; Serefoglu et al., 2011). An equal number of Asian (n = 3) (Lee et al., 2013; Liang et al., 2010; Park et al., 2010) and European (n = 3) (Andersen et al., 2008; Mitchell et al., 2016; Mitchell et al., 2013) studies used a self-developed questionnaire and reported a prevalence of PE ranging from 3.3% to 41.8% and 10% to 28.6% for Asian men and European men, respectively. The remaining European studies used the SFS (n = 1; 2.7%–9.3%) (Hendrickx et al., 2016) and the full version of the IIEF (n = 1; 45.2%) (Quinta Gomes & Nobre, 2014) to diagnose PE.
DE was reported in only five European studies that used interviews (n = 2; 7%–17%) (Moreau et al., 2016; Traeen & Stigum, 2010), questionnaires with SFS (n = 1; 1.3%–10.7%) (Hendrickx et al., 2016), the full version of the IIEF (n = 1; 17.5%) (Quinta Gomes & Nobre, 2014), ELSA SRA-Qs (n = 1; 8.3%–52.2%) (Lee et al., 2016), and the GSSAB (n = 1; 6.2%–19.9%) (Landripet & Stulhofer, 2015).
HSDD was reported at 7.0% to 17.2% and 12% to 28% in Asian (Zhang et al., 2013) and European (Moreau et al., 2016; Traeen & Stigum, 2010) studies, respectively, that interviewed men for assessment of MSD. A total of three Asian and 11 European studies used questionnaires for the diagnosis of HSDD. Two Asian (Kim et al., 2009; Rao et al., 2015) and five European (Andersen et al., 2008; Beutel et al., 2018; Kontula & Haavio-Mannila, 2009; Mitchell et al., 2013; 2016) studies used a self-developed questionnaire. One Asian (48.1%–81.4%) (Liu et al., 2010) and one European (17.2%) (Quinta Gomes & Nobre, 2014) study used the full version of the IIEF, while the six remaining European studies used SFS (n = 1; 1.8%–7.3%) (Hendrickx et al., 2016), the National Survey of Sexual Attitudes and Lifestyles (NASTAL) (n = 1; 0.2%–29.9%) (Carvalheira et al., 2014), GSSAB (n = 1; 12.8%–37.4%) (Landripet & Stulhofer, 2015), the Dutch module SAc (n = 1; 40.8%–57.7%) (Korfage et al., 2008), ADAM (n = 1; 18.3%–23.0%) (Holm et al., 2012), and ELSA SRA-Q (n = 1; 24.2%–49.1%) (Lee et al., 2016) for the assessment of HSDD.
For orgasmic dysfunctions, the Asian (n = 1; 0.4%) (Rao et al., 2015) and European (n = 2; 3%–65%) (Corona et al., 2010; Donnelly et al., 2018) studies reported anorgasmia using questionnaires. Other orgasmic dysfunctions were assessed through interviews by Asian studies (n = 1; 5%–14%) and by means of EPIC-26 questionnaires (n = 1; 8.9%–64.2%) (Donnelly et al., 2018), and EMAS SFQ-14s (n = 1; 4.0%–18.7%) (Corona et al., 2010) in European studies.
The prevalence of low sexual satisfaction varied from 3.2% to 37.6% and 4.1% to 12.3% of Asian (Kim & Jeon, 2013) and European men (Beckman et al., 2008; Castellanos-Torres et al., 2013; Ruiz-Muñoz et al., 2013), respectively, in studies that interviewed men to assess MSD. The remaining four European studies used self-developed questionnaires (n = 2; 18%–23%) (Kontula & Haavio-Mannila, 2009; Mitchell et al., 2013), the Dutch module SAc (n = 1, 13.3%–23.2%) (Korfage et al., 2008), EMAS SFQ-14s (n = 1; 23.2%–28.3%) (Corona et al., 2010), or ELSA SRA-Qs (n = 1; 18.7%–22.5%) (Lee et al., 2016).
One European study that used interviews reported painful intercourse in 13% of men (Moreau et al., 2016), while interviews using questionnaires (n = 3) reported prevalence ranging from 1% to 18% (Christensen et al., 2011; Mitchell et al., 2016; Mitchell et al., 2013). A European study that interviewed men reported 26% experienced no sexual pleasure (Moreau et al., 2016), while those using questionnaires (n = 2) (Mitchell et al., 2013; Mitchell et al., 2013) reported 1.8% to 6.7% prevalence of the same MSD.
Definition of MSD
The studies used variable definitions and time durations for MSD. The Asian and European studies defined ED alternatively as “erectile difficulties,” “erectile problem,” “impotence,” “inadequate erection,” “less strong erection,” “no or short-term erection,” “poor erection,” and “inability to sustain or achieve an erection sufficient for intercourse,” and 11 Asian studies used an IIEF-5 cut-off score ranging from <18 to <26 for the diagnosis of ED. Three Asian and three European studies did not define the ED at all. The time duration for which ED was diagnosed varied from 6 to 12 months. Although orgasm and ejaculation are two separate phenomena in men, the definitions of these overlapped in the previous studies (Table 1).
Factors of MSD
Age
The prevalence of MSD increased significantly with age for both Asian (Hendrickx et al., 2016; Zhang et al., 2013) and European (Donnelly et al., 2018; Jankowska et al., 2008; Mitchell et al., 2013; Quinta Gomes & Nobre, 2014) men. Age distribution over 60 years of age was not significantly associated with MSD in Asian men (Rao et al., 2015).
Increased age showed a significant positive association with ED or erectile difficulties reported in Asian (Çayan et al., 2017; Hao et al., 2011; Jeong et al., 2011; Kendirci et al., 2014; Khoo et al., 2008; Park et al., 2010; Permpongkosol et al., 2008; Wong et al., 2009b; Zhang et al., 2016; Zhang et al., 2013, 2016, 2017) and European (Andersen et al., 2008; Corona et al., 2010; Jern et al., 2012; Korfage et al., 2008; Lee et al., 2016; Mitchell et al., 2013; Quinta Gomes & Nobre, 2014) men, and with the severity of erectile dysfunction in Asian men (Çayan et al., 2017; Kendirci et al., 2014; Khoo et al., 2008; Tang et al., 2015). Two studies reported that age was not significantly associated with ED in European men (Andersen et al., 2008; Landripet & Stulhofer, 2015).
Ejaculation dysfunctions were also significantly associated with age in Asian (Lee et al., 2013; Liang et al., 2010) and European (Andersen et al., 2008; Ghalayini et al., 2010; Mitchell et al., 2013) men. The prevalence of PE decreased with age in European men (Andersen et al., 2008; Ghalayini et al., 2010; Mitchell et al., 2013), whereas in Asian men the association of PE with age was inconsistent (Lee et al., 2013; Liang et al., 2010). A few Asian and European studies also reported a nonsignificant association of PE with age (Quek et al., 2008; Quinta Gomes & Nobre, 2014; Zhang et al., 2013).
The association of DE with age in European men was inconsistent. While a few studies reported that the prevalence of DE was significantly increased with age (Andersen et al., 2008; Lee et al., 2016), others reported no association with age (Hendrickx et al., 2016; Landripet & Stulhofer, 2015; Mitchell et al., 2013). In some studies, age was a significant predictor of orgasmic difficulties in European men (Lee et al., 2016; Quinta Gomes & Nobre, 2014), however, one European study reported that difficulty in attaining orgasm, delayed orgasm, and early orgasm were not significantly associated with age (Hendrickx et al., 2016).
Age had no significant association with sexual satisfaction in Asian men (Kim & Jeon, 2013). In contrast, the proportion of European men satisfied with their sexual relationship was significantly lower in the oldest age decade compared with the youngest (Corona et al., 2010). Dissatisfaction varied with age in sexually inactive European men but not among sexually active men (Mitchell et al., 2013). For sexually active individuals, the proportion of men reporting distress increased with age (Mitchell et al., 2013). Among European men with ED, concern about ED was highest and lowest in the 50–59 years and ≥70 years bands, respectively (Corona et al., 2010). A few European studies also reported no significant association of sexual satisfaction with age (Castellanos-Torres et al., 2013; Lee et al., 2016; Ruiz-Muñoz et al., 2013).
The prevalence of low sexual desire decreased across the age range that became more obvious in later ages in both Asian and European men (Beutel et al., 2018; Hendrickx et al., 2016; Korfage et al., 2008; Landripet & Stulhofer, 2015; Lee et al., 2016; Quinta Gomes & Nobre, 2014; Zhang et al., 2013). In contrast, hyperactive sexual desire was associated with decreasing age and sexual aversion in European men (Hendrickx et al., 2016). Some studies reported no significant association between age and sexual desire after controlling for the effects of other variables in European men (Kontula & Haavio-Mannila, 2009; Mitchell et al., 2013; Holm et al., 2012). To express this result simply, the negative effects of biological aging on sexual desire disappear when people are satisfied with their sexual experiences, are sexually functioning, and are healthy (Kontula & Haavio-Mannila, 2009).
Socioeconomic Status
Men with lower levels of educational attainment were at higher risk of sexual dysfunction in both Asia and Europe (Çayan et al., 2017; Ghalayini et al., 2010; Hwang et al., 2010; Jankowska et al., 2008; Permpongkosol et al., 2008; Quinta Gomes & Nobre, 2014; Tang et al., 2015), including ED in Asian men (Çayan et al., 2017; Ghalayini et al., 2010; Tang et al., 2015) and orgasmic dysfunctions in European men (Quinta Gomes & Nobre, 2014). The severity of ED also varied by education in Asian men (Permpongkosol et al., 2008). Another Asian study reported that further education up to the university level increased the prevalence of ED (Hwang et al., 2010). Other studies reported that education was not associated with the prevalence of sexual dysfunctions in Asian men (Kim & Jeon, 2013; Rao et al., 2015), including ED (Jeong et al., 2011; Khoo et al., 2008; Zhang et al., 2017) and sexual satisfaction (Kim & Jeon, 2013). In European men, PE, anorgasmia, sexual satisfaction, HSDD, DE, and painful sexual intercourse were not associated with education (Christensen et al., 2011; Kontula & Haavio-Mannila, 2009; Quinta Gomes & Nobre, 2014; Ruiz-Muñoz et al., 2013). One European study reported increased educational level was significantly associated with decreased HSDD (Landripet & Stulhofer, 2015).
MSD was significantly associated with employment in Asian (Permpongkosol et al., 2008; Rao et al., 2015) and European men (Christensen et al., 2011; Corona et al., 2010; Mitchell et al., 2013). Sexual dysfunctions were significantly more prevalent among unemployed Asian and European men (Corona et al., 2010; Donnelly et al., 2018; Mitchell et al., 2013; Rao et al., 2015). The risk factors for ED included occupation in Asian men (Khoo et al., 2008; Tang et al., 2015). Among Asian men, the unemployed occupational status had the highest prevalence of ED, followed by agricultural workers/fishermen, managerial workers, clerical workers, sales workers/merchants, service workers, policemen/soldiers, transportation/communication workers, manufacturing/construction workers, and professional/technical workers (Permpongkosol et al., 2008). Technicians and associate professionals, production and related workers, laborers, and retirees had a higher prevalence of moderate and severe ED compared with other occupational categories in Asian men (Khoo et al., 2008). In another study, being employed or unemployed did not show meaningful differences regarding rates of ED, but being retired was found to be an independent risk factor for having ED compared to working Asian men (Çayan et al., 2017).
Income had a negative association with MSD in Asian men (Kendirci et al., 2014), including ED (Çayan et al., 2017; Ghalayini et al., 2010; Hwang et al., 2010; Permpongkosol et al., 2008; Zhang et al., 2017). European men with a high income had significantly lower odds of painful sexual intercourse (Christensen et al., 2011). Tiredness and work-related stress were the most frequently reported reasons for decreased sexual interest in European men (Carvalheira et al., 2014).
A few studies reported that sociodemographic factors (employment, occupation, house ownership, and income) had no association with MSD, including ED and sexual satisfaction in Asian men (Kim & Jeon, 2013; Zhang et al., 2016) and sexual desire in European men (Kontula & Haavio-Mannila, 2009).
Area of Residence
European men from developing countries reported being less sexually satisfied than those from developed countries (Ruiz-Muñoz et al., 2013). The reasons for decreased sexual interest differed significantly across European countries (Carvalheira et al., 2014). Croatian and Norwegian participants were more likely to have experienced a distressing lack of sexual interest in the past year than their Portuguese counterparts (Carvalheira et al., 2014). One study reported that the likelihood of having ED was higher for Asian men living in urban areas than those living in rural areas (Çayan et al., 2017). Combinations of three problems (urinary, bowel, or sexual dysfunction) were significantly more prevalent amongst European men residing in deprived areas (Donnelly et al., 2018).
A large European study reported that there was a significantly higher prevalence of ED in Tartu (Estonia), followed by Florence (Italy), Malmö (Sweden), and Leuven (Belgium); however, the concern about ED was highest in Florence than Tartu (Corona et al., 2010). Tartu reported the lowest frequency of orgasms (as assessed by achieving orgasm more than half the time) and the lowest satisfaction regarding the timing of orgasm (proportion who were extremely/highly satisfied) (Corona et al., 2010). A few studies reported that the area of residence (living in rural, urban, or deprived areas) did not affect the presence of MSD in either Asian or European men (Mitchell et al., 2013; Rao et al., 2015), including male pelvic dysfunction (combined presence of ED, lower urinary tract symptoms (LUTSs), and ejaculation dysfunction) (Kendirci et al., 2014) in European men and ED in Asian men (Zhang et al., 2017).
Marital Status
The association between marital status and MSD was inconsistent for both Asian and European men. One Asian study reported that unmarried men had a higher prevalence of ED than married men, especially in severe ED cases (Permpongkosol et al., 2008). Single Asian and European men were reported as having significantly higher odds of PE compared to men who had partners or cohabited (Mitchell et al., 2013; Quek et al., 2008). HSDD was significantly more prevalent in European single men (Beutel et al., 2018). A few studies reported that marital status was not related to ED for Asian and European (Jeong et al., 2011; Tang et al., 2015; Zhang et al., 2016, 2017) men, nor to PE, DE, and HSDD for European men (Quinta Gomes & Nobre, 2014). One Asian study also reported that sexual problems were highly prevalent among married men (Rao et al., 2015).
European men who only had intercourse with a regular partner were more satisfied than men had intercourse with various casual partners or both regular and casual partners (Ruiz-Muñoz et al., 2013). An association between low sexual function and having a same-sex partner in the past 5 years was noted in European men. For European men, a strong association between low sexual function and paying for sex in the past year was also reported (Mitchell et al., 2013).
The length of marriage or cohabitation was not associated with ED in Asian and European men (Kim & Jeon, 2013; Zhang et al., 2016). In contrast, sexual boredom as a result of a long-term relationship was significantly and negatively correlated with the level of intimacy and sexual satisfaction in European men (Carvalheira et al., 2014). European men in long-term relationships (≥5 years) were more likely to report a lack of sexual interest with associated personal distress than men in short-term relationships (<5 years) (Carvalheira et al., 2014). Another study reported that the duration of the present relationship had no association with sexual desire in European men (Kontula & Haavio-Mannila, 2009). The family structure and having children had no significant association with sexual disorders among Asian men (Kim & Jeon, 2013; Rao et al., 2015; Zhang et al., 2016).
A high prevalence of sexual dysfunctions, including ED, ejaculation dysfunctions (PE and DE), and HSDD, was observed in Asian and European men who were in estranged relationships or were dissatisfied with their marriage (Kim & Jeon, 2013; Mitchell et al., 2013; Zhang et al., 2013, 2016, 2017). In this regard, relationship-related reasons (passive partner, conflicts, and communication problems) were reported to cause decreased sexual interest in European men (Carvalheira et al., 2014). Sexual satisfaction was significantly higher among European men who contributed to domestic tasks compared with those who did not (Castellanos-Torres et al., 2013). PE was reported to affect Asian men’s overall relationships with their partners (Lee et al., 2013).
The partner’s health and satisfaction with the sexual relationship were reported as independent risk factors for ED in European men (Corona et al., 2010). Asian men whose wives sought medical help for sexual problems were more likely to experience sexual dysfunction, particularly ejaculation dysfunction (Zhang et al., 2013). One study reported that the health status of the spouse had no association with sexual satisfaction in Asian men (Kim & Jeon, 2013). Another study reported that sexual desire was not associated with the partner’s orgasmic dysfunctions in European men (Kontula & Haavio-Mannila, 2009).
Men’s perception of their partner and the partner’s behavior were also associated with sexual dysfunctions. The perception of one’s partner as very attractive significantly reduced the likelihood of European men to report a lack of sexual interest (Carvalheira et al., 2014). Asian men with nonliberal attitudes toward female sexual initiation and refusal were more likely to experience sexual dysfunction, including erectile dysfunction and HSDD (Zhang et al., 2013). Asian men who assumed their partners were less sexually satisfied had significantly higher chances of PE (Lee et al., 2013). Having a sexually skillful partner was a significant predictor of sexual desire for European men (Kontula & Haavio-Mannila, 2009). European men who had concerns about their partner not initiating sex were more dissatisfied with their overall sex life (Lee et al., 2016).
Religion and Ethnicity
Interestingly, a very low prevalence of ED was observed in subjects from two religious minorities in the Asian population: Zhuang and Muslim men. The number of subjects in these ethnic groups was relatively small (Zhang et al., 2017). By ethnicity, 76.7% of Malays, 70.5% of Chinese, 79.3% of Indians, and 66.7% of other ethnicities had ED, but no significant association was reported between ethnicity and ED in Asian men (Khoo et al., 2008).
Smoking and Alcohol Consumption
The occurrence of smoking and alcohol consumption was inconsistently reported to be associated with MSD. A few studies reported that smoking was not associated with ED in Asian men (Huang et al., 2014; Rao et al., 2015). Numerous other studies reported that smoking status, duration, and frequency were positively associated with ED in Asian men (Ghalayini et al., 2010; Jeong et al., 2011; Permpongkosol et al., 2008; Tang et al., 2015; Zhang et al., 2017).
The age-adjusted prevalence of ED in Asian men smoking more than 30 cigarettes daily was significantly higher than in men smoking fewer cigarettes or in men who did not smoke (Zhang et al., 2017). The current and former smokers had a higher risk of ED compared with nonsmokers. Former smokers also had a higher risk of ED compared with nonsmokers or current smokers (Ghalayini et al., 2010; Jeong et al., 2011). Being a current smoker was also a significant risk factor for ED in European men (Andersen et al., 2008; Corona et al., 2010). A statistically significant relationship was reported between the duration of smoking and ED among both current and former smokers, especially for those who had smoked cigarettes for more than 30 years (Permpongkosol et al., 2008).
Some studies also reported that alcohol consumption was not associated with ED for Asian men (Huang et al., 2014; Jeong et al., 2011; Rao et al., 2015; Zhang et al., 2017). Others reported that alcohol consumption, duration, and frequency did have an impact on ED (Permpongkosol et al., 2008; Tang et al., 2015). Bioavailable testosterone (BT) levels were significantly higher in more frequent alcohol consumers who were 35 years of age, as compared to less frequent consumers. In contrast, BT was significantly lower in more frequent alcohol consumers who were 45 years of age, as compared to less frequent consumers. Overall testosterone concentrations were not associated with alcohol use (Holm et al., 2012). Although tea consumption was not associated with ED, caffeine consumption was reported to be associated (Permpongkosol et al., 2008).
General Health
For European men, fair or poor health was significantly associated with less frequent sexual intercourse, low sexual satisfaction, ED, difficulty achieving orgasm, HSDD, and declines in the frequency of sexual activities (Carvalheira et al., 2014; Castellanos-Torres et al., 2013; Donnelly et al., 2018; Kontula & Haavio-Mannila, 2009; Lee et al., 2016; Mitchell et al., 2013; Sand et al., 2008). The risk factors for ED in Asian men included poor health (Khoo et al., 2008; Tang et al., 2015). Another Asian study reported that current health had no association with sexual satisfaction (Kim & Jeon, 2013).
Physical Activity
One study reported that higher physical activity was associated with decreased risk of ED in Asian men (Wong et al., 2009b), while another study instead linked this to sexual dysfunction in European men (Donnelly et al., 2018). Other studies reported that Asian men doing exercise had lower percentages of ED, but that the association was not significant (Huang et al., 2014; Jeong et al., 2011; Permpongkosol et al., 2008).
Difficulty performing activities of daily living and instrumental activities of daily living due to current disease had no association with sexual satisfaction in Asian men (Kim & Jeon, 2013). Sexual desire was not significantly associated with the frequency of exercise in European men (Kontula & Haavio-Mannila, 2009).
Body Mass Index
The association between body mass index (BMI) and MSD was inconsistent in Asian and European men. Increased BMI and obesity were significantly associated with ED in Asian (Ghalayini et al., 2010; Wong et al., 2009b) and European men (Andersen et al., 2008; Corona et al., 2010).
Having abnormal BMI levels demonstrated a significant impact on the presence of male pelvic dysfunction or a combination of all three problems (urinary, bowel, and/or sexual dysfunction) in Asian (Kendirci et al., 2014) and European men (Donnelly et al., 2018). Underweight Asian men had the highest prevalence of severe ED, while obese Asian men had the highest prevalence of mild ED (Permpongkosol et al., 2008).
Other studies reported that abnormal increases or decreases in BMI and waist circumference were not significantly associated with the prevalence of ED in Asian men (Çayan et al., 2017; Huang et al., 2014; Jeong et al., 2011; Permpongkosol et al., 2008; Zhang et al., 2017). PE, sexual satisfaction, and desire were not associated with BMI in European men (Andersen et al., 2008; Kontula & Haavio-Mannila, 2009).
Cardiovascular Diseases
The presence of cardiovascular disease (CVD) was associated with ED in Asian (Çayan et al., 2017; Permpongkosol et al., 2008; Wong et al., 2009a) and European men (Corona et al., 2010; Lee et al., 2016). Hypertension, one of the most important risk factors of CVD, was also associated with ED (Çayan et al., 2017; Huang et al., 2014; Permpongkosol et al., 2008; Quek et al., 2008; Wong et al., 2009b), PE (Lee et al., 2013; Park et al., 2010), sexual problems (Rao et al., 2015), and pelvic disorders (Kendirci et al., 2014) in Asian men. The more severe forms of ED displayed an increased association with hypertension and CVD (Çayan et al., 2017; Huang et al., 2014). High blood pressure was also significantly associated with less sexual intercourse, frequent masturbation, and ED in European men (Lee et al., 2016).
The presence of previous strokes, atherosclerosis, and coronary artery disease significantly increased the odds of moderate to severe ED in Asian men (Çayan et al., 2017; Huang et al., 2014). The use of beta-blockers and thiazides was independently associated with increased odds of ED in Asian men (Wong et al., 2009a). The risk of moderate to severe ED and pelvic dysfunctions in Asian men increased with the presence of dyslipidemia (Çayan et al., 2017; Kendirci et al., 2014). Other studies reported no association of dyslipidemia with ED (Huang et al., 2014) and PE (Quek et al., 2008) in Asian men. A few studies reported no association between CVD, cerebrovascular diseases, and hypertension with ED in Asian men (Jeong et al., 2011; Zhang et al., 2017).
Diabetes Mellitus
The presence of diabetes mellitus was associated with increased odds of ED in Asian (Çayan et al., 2017; Huang et al., 2014; Permpongkosol et al., 2008; Quek et al., 2008; Wong et al., 2009a; Zhang et al., 2017) and European (Corona et al., 2010; Lee et al., 2016) men. Diabetes was also associated with sexual problems (Rao et al., 2015), ejaculation dysfunctions (Lee et al., 2013; Quek et al., 2008), and pelvic dysfunction (Kendirci et al., 2014) in Asian men. Severe forms of ED were more significantly associated with diabetes (Çayan et al., 2017; Huang et al., 2014). One Asian study reported no significant age-adjusted association between diabetes and ED (Ghalayini et al., 2010).
Lower Urinary Tract Symptoms
LUTSs were associated with ED in Asian (Çayan et al., 2017; Khoo et al., 2008; Quek et al., 2008; Wong et al., 2009a; 2009b; Zhang et al., 2017) and European men (Corona et al., 2010; Dumbraveanu et al., 2018). The risk factors for ED included genitourinary diseases in Asian men (Tang et al., 2015). The severity of LUTSs determined the severity of ED in a dose–response relationship in Asian and European men, particularly in later years (Çayan et al., 2017; Dumbraveanu et al., 2018; Wong et al., 2009a; 2009b). Nocturia and nocturnal polyuria were associated with ED in both Asian and European men (Dumbraveanu et al., 2018; Quek et al., 2008). LUTSs were also negatively associated with orgasm frequency in European men (Corona et al., 2010).
Mental Health
Anxiety before sexual activity was one of the most common comorbid symptoms for sexual difficulties in European men (Carvalheira et al., 2014). It had significant associations with ED in European (Jern et al., 2012) and PE in Asian (Park et al., 2010; Quek et al., 2008) men. Erectile problems increased with increasing psychiatric symptoms in European men (Jern et al., 2012).
Being depressed was associated with an increased risk of ED in Asian (Jeong et al., 2011; Khoo et al., 2008; Wong et al., 2009a; Wong et al., 2009b) and European (Corona et al., 2010; Jern et al., 2012) men. A significant association was also observed between PE and depression in Asian men (Park et al., 2010; Quek et al., 2008). In Asian men, shorter intravaginal ejaculation latency time was associated with higher stress levels (Park et al., 2010). Depression and cognitive functions had no association with sexual satisfaction in Asian men (Kim & Jeon, 2013).
Depression was significantly associated with all sexual function parameters (erectile function, libido, ejaculatory function, sexual problems, and sexual satisfaction) in European men (Corona et al., 2010). European men with higher levels of depression were more likely to report a lack of sexual interest (Carvalheira et al., 2014) and low sexual satisfaction (Mitchell et al., 2013). Sexual desire was not associated with stress symptoms in European men (Kontula & Haavio-Mannila, 2009).
Prostatitis
Men suffering from prostatitis or prostatitis-like symptoms had a significantly higher prevalence of ED in Asia, and this increased with age (Çayan et al., 2017; Hao et al., 2011; Huang et al., 2014; Permpongkosol et al., 2008). A positive association was reported between moderate to severe ED and benign prostatic hyperplasia in Asian men (Huang et al., 2014).
Prostatitis-like symptoms significantly increased the prevalence of PE in Asian men (Lee et al., 2013; Liang et al., 2010; Park et al., 2010), while the presence of chronic prostatitis increased prevalence to more than double that of the whole population (Liang et al., 2010).
Other Diseases
Asian men who had experienced other serious diseases, trauma, or injuries to the spinal cord or pelvic region had higher chances of getting ED than those who had not (Permpongkosol et al., 2008). Arthritis had a significant association with PE in Asian men (Lee et al., 2013), while it was linked to ED, delayed orgasm, and HSDD in European men (Lee et al., 2016). Asthma was also associated with ED, HSDD, low frequency of sexual activities, and delayed orgasm in European men (Lee et al., 2016).
Asian men with PE had a higher prevalence of thyroid disease (hyperthyroidism) (Lee et al., 2013; Park et al., 2010). No association was reported between the prevalence of ED and the presence of peptic ulcers in Asian men (Permpongkosol et al., 2008). Low sexual function was also associated with previous sexually transmitted infections (STIs) in European men (Mitchell et al., 2013). Another study reported no association between a recent STI diagnosis and sexual dysfunctions in European men (Moreau et al., 2016). The number of current diseases had no association with sexual satisfaction in Asian men (Kim & Jeon, 2013).
Behavior and Self-Esteem
The importance of sex-life in old age had no association with sexual satisfaction in Asian men (Kim & Jeon, 2013). European men who considered their sexual life to be important had an increased likelihood of high sexual desire (Kontula & Haavio-Mannila, 2009). A high sexual desire among men was significantly associated with sexual self-esteem and self-confidence about erectile function (Carvalheira et al., 2014; Kontula & Haavio-Mannila, 2009). Low sexual function was associated with a lack of sexual competence (defined as lack of vigor, regret about the timing, autonomy of the decision, and use of a reliable form of contraception) during first intercourse and with sexual experiences in the past 4 weeks (Mitchell et al., 2013). Asian men who cared more about their sexual life and were sexually satisfied experienced improved erection hardness (Hwang et al., 2010).
Pornography
No statistically significant associations between frequency of pornography use and ED, DE, and HSDD were observed in European (Portuguese and Norwegian) men. In the Croatian men surveyed in 2011, the relationship between moderately frequent pornography use and ED was significant (Landripet & Stulhofer, 2015). In the Croatian men surveyed in 2014, no significant associations between pornography use and sexual health disturbances (ED, DE and HSDD) were observed (Landripet & Stulhofer, 2015). European men who found pornography arousing had an increased likelihood of high sexual desire (Kontula & Haavio-Mannila, 2009). But another study reported that the frequency of pornography use was not associated with a sexual interest in European men (Carvalheira et al., 2014). When compared with men who reported decreased or stable frequency of pornography use in the past 12 months, those with increased pornography use did not display higher odds of ED, HSDD, or DE (Landripet & Stulhofer, 2015).
Mutual Relationship of Sexual Disorders
In European men, the significant association between ED generally and ED during first intercourse suggested that erectile problems during the first intercourse experience were predictive to some degree of ED problems later in life (Jern et al., 2012). European men with ED had significantly higher odds of personal dissatisfaction with all quality of life attributes, particularly regarding satisfaction with their sex life, overall health, orgasmic problems, and DE (Lee et al., 2016; Moreau et al., 2016; Sand et al., 2008; Traeen & Stigum, 2010). Good erectile function was a positive predictor of high sexual desire among European men (Carvalheira et al., 2014; Kontula & Haavio-Mannila, 2009; Traeen & Stigum, 2010).
No significant association was reported between ED and AD in Asian (Kendirci et al., 2014; Tang et al., 2015) and European (Holm et al., 2012) men. ED was significantly associated with late-onset hypogonadism in Asian men (Tang et al., 2015). Higher fasting blood glucose levels and lower follicle-stimulating hormone levels were reported in cases of moderate to severe ED compared to no/mild ED (Huang et al., 2014).
PE was significantly associated with ED, HSDD, and low sexual satisfaction in Asian men (Lee et al., 2013; Park et al., 2010). Good orgasmic functions were a positive predictor of high sexual desire among European men (Carvalheira et al., 2014; Kontula & Haavio-Mannila, 2009; Traeen & Stigum, 2010).
European men with sexual dysfunction were significantly less satisfied, and dissatisfaction increased with the number of sexual disorders (Moreau et al., 2016). Sexual satisfaction was lower in Asian men with distressing sexual difficulties compared to individuals with nondistressing sexual difficulties (Hendrickx et al., 2016). European men who reported distressing HSDD also reported a much higher number of other sexual difficulties than men who did not report a lack of sexual interest (Carvalheira et al., 2014). Being satisfied with sexual function increased the likelihood of high sexual desire in European men (Kontula & Haavio-Mannila, 2009).
It was also noted that constructs of masculinity (man of honor, control of own life, respect of friends, good job, coping with problems on own, active sex life, financial stability, physically attractive, and successful with women) did not vary significantly between men with erectile dysfunction and men without erectile dysfunction (Sand et al., 2008).
Sexual Activity and Dysfunction
Most of the European men reported that the main reason for not having intercourse was due to personal reasons, followed by MSDs (Beckman et al., 2008). Sexual activities (intercourse and masturbation) were significantly associated with ED, the severity of ED, male pelvic dysfunction, LUTSs, time of ejaculation, distressing sexual difficulties, dissatisfaction, and more than one sexual dysfunction, in both Asian and European men (Çayan et al., 2017; Hendrickx et al., 2016; Kendirci et al., 2014; Korfage et al., 2008; Lee et al., 2013, 2016; Moreau et al., 2016; Park et al., 2010; Quek et al., 2008). One study reported that most of the sexually inactive European men reported that they were not dissatisfied, distressed, or avoiding sex because of sexual difficulties (Mitchell et al., 2013). Sexual desire was not associated with preferring more frequent intercourse in Asian and European men (Carvalheira et al., 2014; Kontula & Haavio-Mannila, 2009).
Discussion
This is the first systematic review to summarize and compare the prevalence of MSDs and associated factors in Asian and European populations. A previous literature review was published on the sexual dysfunction of Asian men that did not report the selection of studies (Ho et al., 2011) and a systematic review that did not compare Asian men with European men (Lewis, 2011).
Although Asian societies are still conservative about the description, diagnosis, and treatment of sexual dysfunctions, an equally significant number of population-based studies were published on various aspects of MSD in Asian men as studies on European men. Out of the 25 Asian studies (Chung et al., 2015; Ghalayini et al., 2010; Hao et al., 2011; Huang et al., 2014; Jeong et al., 2011; Kim et al., 2009; Kim & Jeon, 2013; Lee et al., 2013; Liang et al., 2010; Park et al., 2010; Rao et al., 2015; Tang et al., 2015; Wong et al., 2009a; 2009b; Zhang et al., 2013, 2016, 2017) analyzed, 17 were carried out in East Asian countries and regions (China, Hong Kong, South Korea, and Taiwan) (Chung et al., 2015; Hao et al., 2011; Hwang et al., 2010, 2014; Jeong et al., 2011; Khoo et al., 2008; Kim et al., 2009; Kim & Jeon, 2013; Lee et al., 2013; Liang et al., 2010; Liu et al., 2010; Park et al., 2010; Permpongkosol et al., 2008; Quek et al., 2008; Tang et al., 2015; Wong et al., 2009a; Wong et al., 2009b; Zhang et al., 2016; Zhang et al., 2013, 2017), including 15 studies covering Chinese (Chung et al., 2015; Hao et al., 2011; Huang et al., 2014; Kim et al., 2009; Liang et al., 2010; Tang et al., 2015; Wong et al., 2009a; 2009b; Zhang et al., 2013, 2016, 2017) and Korean (Jeong et al., 2011; Kim & Jeon, 2013; Lee et al., 2013; Park et al., 2010) populations and three studies took place in South East Asian countries (Malaysia and Thailand). Of the remaining five studies, four were from Western Asia (Jordan and Turkey) (Çayan et al., 2017; Ghalayini et al., 2010; Kendirci et al., 2014; Serefoglu et al., 2011), and only one was from South Asia (India) (Rao et al., 2015). In contrast, in European countries, large studies were recently carried out that included men from many countries (Corona et al., 2010; Lee et al., 2013; Sand et al., 2008). No such recent, wide-ranging study was found for Asian men. Most of the studies carried out on Asian men are small in terms of the sample sizes and number of sexual dysfunctions investigated. As a result, the management policies developed based on the European data have also been applied to the Asian populations.
The prevalence of sexual dysfunction varied due to differences in the ages and time periods investigated and the definitions and data collection strategies adopted (telephone interviews, IAQs, SAQs, and mail questionnaires). Some general observations can be made. The prevalence of low satisfaction, HSDD, and the various types of ED were generally higher in Asian men compared to European men, whereas the prevalence of anorgasmia and PE was higher in European men compared to Asian men. In both Asian and European men, age was an independent positive factor of almost all the MSDs investigated. PE increased with age in Asian men of all ages and in European men <60 years. In European men >60 years, the prevalence of PE decreased with age.
The prevalence of MSD in both Asian and European men was generally greater in questionnaire-based studies than interview-based studies. One instance of the masculinity in most of the societies being portrayed as a sexual superpower and of someone self-reporting their own MSD was disgraceful (Tomlinson, 1998). The ED prevalence reported that was based on IIEF-5 was higher than that of interviews and other questionnaires, both for the Asian and European men (Hao et al., 2011; Tang et al., 2015). Sometimes, of men who reported in self-assessment that they did not have ED, one in four were reported to have mild to moderate ED when evaluated using IIEF-5 (Hwang et al., 2010).
The Asian studies did not report on DE, orgasmic dysfunction, and anejaculation or retrograde ejaculation firstly because, unlike PE, these conditions are poorly understood and considered uncommon forms of male sexual dysfunction (Abdel-Hamid & Saleh, 2011; Butcher et al., 2015). This review reported a high prevalence of DE (up to 52.2%) in European men (Lee et al., 2016). Although treating anejaculation or retrograde ejaculation is important, particularly to men who intend to become fathers, the prevalence of this condition was only reported in one study on European men (Hendrickx et al., 2016; Mehta & Sigman, 2015). Secondly, for these ejaculatory problems to be reported as a disorder, the men suffering from them were required to have suffered from personal distress (Gray et al., 2018). There is no gold standard for diagnosis of DE, nor is there a specifically defined time of latency, and even physicians from developed countries have an inconsistent practice pattern for diagnosing DE (Abdel-Hamid & Saleh, 2011; Butcher et al., 2015). Thirdly, most men may be more concerned about a decreased time to ejaculation, while an increased time to ejaculation is not considered a sexual dysfunction, but is instead viewed as increased sexual stamina. Although this increased stamina may increase pleasure and intimacy at first, it causes distress, painful intercourse, and decreased sexual activity when the problem persists for a long time.
Orgasmic dysfunctions (early or delayed orgasm) were also only reported in European men. Anorgasmia was also under-reported among Asian men and displayed a considerably low prevalence (Rao et al., 2015). These dysfunctions have no specified time threshold, and although orgasm and ejaculation are two separate phenomena in men, definitions in a few previous studies have overlapped (Castellanos-Torres et al., 2013; Liu et al., 2010; Ruiz-Muñoz et al., 2013; Zhang et al., 2017). It is suggested that only one in four men routinely achieve orgasm in all sexual encounters. Therefore, most of the men perceive it as a normal function that may lower the chances of reporting of abnormal orgasmic delay on assessment. Orgasmic dysfunction also causes distress, painful intercourse, and reduced frequency of sexual intercourse (Jenkins & Mulhall, 2015).
Although low sexual satisfaction is predictive of conservative attitudes about sex, lack of importance attributed to sexual issues, lack of sexual expression, and use of restricted sexual techniques (Haavio-Mannila & Kontula, 1997), interestingly only one of the Asian studies reported this (3.2%–37.6%), which is comparable to European men (4.1%–28.3%) (Beckman et al., 2008; Castellanos-Torres et al., 2013; Corona et al., 2010; Kim & Jeon, 2013; Kontula & Haavio-Mannila, 2009; Korfage et al., 2008; Lee et al., 2016; Ruiz-Muñoz et al., 2013), who are often considered to have more open or progressive attitudes.
The review also reported that only one European study reported on hyperactive sexual desire disorder (Hendrickx et al., 2016). The fact that HSDD was considerably higher in Asian men compared to European men may be due to the former’s more conservative background (Montgomery, 2008). It was also suggested that sexual guilt significantly decreased sexual desire in Asian men as compared to Euro-Canadian men (Brotto et al., 2012). Reduced/no sexual pleasure was also not reported among Asian men. Sexual pleasure is generally given a low level of attention in the field of reproductive health (John et al., 2015).
The prevalence and factors of painful intercourse have rarely been diagnosed among men and are not typically discussed in the routine diagnosis of sexual dysfunction (Heiman, 2002). The present review also showed that it was reported in only one European study.
Both the Asian and European studies reported a significant association between one or more MSDs and sociodemographic factors (age, education, employment, income, area of residence, and marital status), lifestyle habits (smoking and physical activity) and health factors (general health, BMI, CVD, diabetes mellitus, arthritis, and LUTSs). The effects of religion, ethnicity, alcohol, tea and caffeine consumption, prostatitis, thyroid dysfunctions, and spinal cord and pelvic injuries were only studied in Asian men. Likewise, the roles of pornography use, STIs, and asthma were only investigated in European men.
Limitations
The review was limited to a certain number of published studies, which may create bias because of the high probability that unpublished studies also have significant results. Other sources of bias were that studies published in languages other than English and studies of which the full text could not be found were not included in the review. Most of the Asian studies were on East Asian populations; therefore, these data cannot be generalized to men from all of Asia, as vast cultural, religious, and socioeconomic differences exist across this continent. Ideally, a meta-analysis of the prevalence should be performed, but due to various definitions of MSD and study designs involved, it was not possible.
Recommendations for Future Research
There is a need to conduct large or multicenter studies on various Asian populations for better assessment and proper treatment of MSDs. It is crucial to emphasize the use of standard definition and criteria of MSDs for valid comparison worldwide along with validated tools for its assessment. Men in Asian populations particularly should be investigated for the prevalence of DE, anejaculation or retrograde ejaculation, orgasmic dysfunction, hyperactive sexual disorder, low sexual satisfaction, reduced sexual pleasure, and painful intercourse. Men should also be investigated for the association of MSDs with religion, ethnicity, alcohol, tea and caffeine consumption, pornography use, STIs, asthma, prostatitis, thyroid dysfunctions, and spinal cord and pelvic injuries. Men should be made aware that sexual dysfunctions are like other systematic dysfunctions that occur due to genetic and environmental factors, and that they are curable. Healthcare professionals should approach sexual function as a normal bodily process that plays an important part in the quality of life of the individual.
Conclusions
The prevalence of ED and HSDD was higher in Asian men compared to European men, whereas the prevalence of anorgasmia and PE was higher in European men compared to Asian men. In both Asian and European men, age was an independent positive factor of almost all the MSDs investigated. The other factors were marital status, socioeconomic status, and comorbidities (CVD, LUTSs, prostatitis, diabetes, hypertension, and psychological disorders). The study suggests monitoring changes in sexual functions with age in both Asian and European men. Men with a low socioeconomic and single status who have other diseases should also be investigated for sexual dysfunctions, and vice versa. Considering the differences between Asian and European data on MSDs, further studies are needed to provide a more concrete and detailed explanation of these differences. There is a particular need to conduct large studies on the various Asian populations for the effective management of MSDs.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval Statement: Not applicable
Consent for publication: Not applicable
ORCID iD: Irfan, Muhammad  https://orcid.org/0000-0002-5308-2359
https://orcid.org/0000-0002-5308-2359
Data Sharing Statement: No additional data are available.
References
- Abdel-Hamid I. A., Saleh E. S. (2011). Primary lifelong delayed ejaculation: Characteristics and response to Bupropion. The Journal of Sexual Medicine, 8(6), 1772–1779. doi: 10.1111/j.1743-6109.2010.02131.x [DOI] [PubMed] [Google Scholar]
- Al-Turki Y. A. (2012). Erectile dysfunction and its association to cardiovascular risk factors among men 60 years and above at primary care clinic, Riyadh, Saudi Arabia. Middle East Journal of Age and Ageing, 9(4), 13. [Google Scholar]
- Andersen I., Heitmann B. L., Wagner G. (2008). Obesity and sexual dysfunction in younger Danish men. The Journal of Sexual Medicine, 5(9), 2053–2060. doi: 10.1111/j.1743-6109.2008.00920.x [DOI] [PubMed] [Google Scholar]
- Beckman N., Waern M., Gustafson D., Skoog I. (2008). Secular trends in self reported sexual activity and satisfaction in Swedish 70 year olds: Cross sectional survey of four populations, 1971-2001. British Medical Journal, 337(7662), a279. doi: 10.1136/bmj.a279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beutel M. E., Burghardt J., Tibubos A. N., Klein E. M., Schmutzer G., Brähler E. (2018). Declining sexual activity and desire in Men—findings from representative German surveys, 2005 and 2016. The Journal of Sexual Medicine, 15(5), 750–756. 10.1016/j.jsxm.2018.03.010 [DOI] [PubMed] [Google Scholar]
- Brotto L. A., Woo J. S., Gorzalka B. B. (2012). Differences in sexual guilt and desire in east Asian and Euro-Canadian men. Journal of Sex Research, 49(6), 594–602. doi: 10.1080/00224499.2011.618956 [DOI] [PubMed] [Google Scholar]
- Butcher M. J., Welliver R. C., Jr., Sadowski D., Botchway A., Kohler T. S. (2015). How is delayed ejaculation defined and treated in North America? Andrology, 3(3), 626–631. doi: 10.1111/andr.12041 [DOI] [PubMed] [Google Scholar]
- Carvalheira A., Træen B., Štulhofer A. (2014). Correlates of men’s sexual interest: A cross-cultural Study. The Journal of Sexual Medicine, 11(1), 154–164. 10.1111/jsm.12345 [DOI] [PubMed] [Google Scholar]
- Castellanos-Torres E., Álvarez-Dardet C., Ruiz-Muñoz D., Pérez G. (2013). Social determinants of sexual satisfaction in Spain considered from the gender perspective. Annals of Epidemiology, 23(3), 150–156. 10.1016/j.annepidem.2012.12.010 [DOI] [PubMed] [Google Scholar]
- Çayan S., Kendirci M., Yaman Ö., Aşçı R., Orhan İ., Usta M. F., Ekmekçioğlu O., Kadıoğlu A. (2017). Prevalence of erectile dysfunction in men over 40 years of age in Turkey: Results from the Turkish society of andrology male sexual health study group. Turkish Journal Urology 43(2), 122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen B. S., Gronbaek M., Osler M., Pedersen B. V., Graugaard C., Frisch M. (2011). Sexual dysfunctions and difficulties in denmark: Prevalence and associated sociodemographic factors. Archives of Sexual Behavior, 40(1), 121–132. doi: 10.1007/s10508-010-9599-y [DOI] [PubMed] [Google Scholar]
- Chung R. Y., Chan D., Woo J., Kwok T., Leung J. C. S., Lai F. T. T., Wong S. Y. S. (2015). Erectile dysfunction is associated with subsequent cardiovascular and respiratory mortality in cohort of 1,436 Chinese elderly men. The Journal of Sexual Medicine, 12(7), 1568–1576. 10.1111/jsm.12918 [DOI] [PubMed] [Google Scholar]
- Corona G., Lee D. M., Forti G., O’Connor D. B., Maggi M., O’Neill T. W., Pendleton N., Bartfai G., Boonen S., Casanueva F. F., Finn J. D., Giwercman A., Han T. S., Huhtaniemi I. T., Kula K., Lean M. E., Punab M., Silman A. J., Vanderschueren D., Wu F. C. (2010). Age-related changes in general and sexual health in middle-aged and older men: Results from the European male ageing study (EMAS). The Journal of Sexual Medicine, 7(4 Pt 1), 1362–1380. doi: 10.1111/j.1743-6109.2009.01601.x [DOI] [PubMed] [Google Scholar]
- DeLamater J., Karraker A. (2009). Sexual functioning in older adults. Current Psychiatry Reports, 11(1), 6–11. [DOI] [PubMed] [Google Scholar]
- Donnelly D. W., Donnelly C., Kearney T., Weller D., Sharp L., Downing A., Wilding S., Wright P., Kind P., Catto J. W. F., Cross W. R., Mason M. D., McCaughan E., Wagland R., Watson E., Mottram R., Allen M., Butcher H., Hounsome L., Gavin A. (2018). Urinary, bowel and sexual health in older men from Northern Ireland. British Journal of Urology International, 122(5), 845–857. doi: 10.1111/bju.14182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumbraveanu I., Ceban E., Banov P. (2018). Lower urinary tract symptoms and erectile dysfunction in men from the republic of Moldova. Journal of Medicine & Life, 11(2), 153–159. [PMC free article] [PubMed] [Google Scholar]
- Ghalayini I. F., Al-Ghazo M. A., Al-Azab R., Bani-Hani I., Matani Y. S., Barham A. E., Harfeil M. N., Haddad Y. (2010). Erectile dysfunction in a Mediterranean country: Results of an epidemiological survey of a representative sample of men. International Journal of Impotence Research, 22(3), 196–203. doi: 10.1038/ijir.2009.65 [DOI] [PubMed] [Google Scholar]
- Gray M., Zillioux J., Khourdaji I., Smith R. P. (2018). Contemporary management of ejaculatory dysfunction. Translational Andrology and Urology, 7(4), 686–702. doi: 10.21037/tau.2018.06.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haavio-Mannila E., Kontula O. (1997). Correlates of increased sexual satisfaction. Archives of Sexual Behavior, 26(4), 399–419. [DOI] [PubMed] [Google Scholar]
- Hao Z. Y., Li H. J., Wang Z. P., Xing J. P., Hu W. L., Zhang T. F., Zhang X. S., Zhou J., Tai S., Liang C. Z. (2011). The prevalence of erectile dysfunction and its relation to chronic prostatitis in Chinese men. Journa of Andrology, 32(5), 496–501. doi: 10.2164/jandrol.110.012138 [DOI] [PubMed] [Google Scholar]
- Hassan A., Aburisheh K., Sheikh T. J., Meo S. A., Ahmed N. A., Al Sharqawi A. H. (2014). Prevalence of erectile dysfunction among Saudi type 2 diabetic patients. European Review for Medical and Pharmacological Sciences, 18(7), 1048–1057. [PubMed] [Google Scholar]
- Heiman J. R. (2002). Sexual dysfunction: Overview of prevalence, etiological factors, and treatments. Journal of Sex Research, 39(1), 73–78. doi: 10.1080/00224490209552124 [DOI] [PubMed] [Google Scholar]
- Hendrickx L., Gijs L., Enzlin P. (2016). Original research: Sexual difficulties and associated sexual distress in Flanders (Belgium): A representative population-based survey study. The Journal of Sexual Medicine, 13(4), 650–668. doi: 10.1016/j.jsxm.2016.01.014 [DOI] [PubMed] [Google Scholar]
- Ho C. C., Singam P., Hong G. E., Zainuddin Z. M. (2011). Male sexual dysfunction in Asia. Asian Journal of Andrology, 13(4), 537–542. doi: 10.1038/aja.2010.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoekstra T., Lesman-Leegte I., Couperus M. F., Sanderman R., Jaarsma T. (2012). What keeps nurses from the sexual counseling of patients with heart failure? Heart & Lung, 41(5), 492–499. 10.1016/j.hrtlng.2012.04.009 [DOI] [PubMed] [Google Scholar]
- Huang Y.-P., Chen B., Ping P., Wang H.-X., Hu K., Yang H., Zhang T., Feng T., Jin Y., Han Y. F., Wang Y. X., Huang Y. R. (2014). Asexuality development among middle aged and older men. PLoS ONE, 9(3), 1–8. doi: 10.1371/journal.pone.0092794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huhtaniemi I. (2014). Late-onset hypogonadism: Current concepts and controversies of pathogenesis, diagnosis and treatment. Asian Journal of Andrology, 16(2), 192–202. doi: 10.4103/1008-682x.122336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang T. I., Tsai T. F., Lin Y. C., Chiang H. S., Chang L. S. (2010). A survey of erectile dysfunction in Taiwan: Use of the erection hardness score and quality of erection questionnaire. The Journal of Sexual Medicine, 7(8), 2817–2824. doi: 10.1111/j.1743-6109.2010.01837.x [DOI] [PubMed] [Google Scholar]
- Isha D., Avinash De S., Sushma S. (2016). Sexuality in older adults: Clinical and psychosocial dilemmas. Journal of Geriatric Mental Health, 3(2), 131–139. doi: 10.4103/2348-9995.195629 [DOI] [Google Scholar]
- Jankowska E. A., Szklarska A., Lopuszanska M., Medras M. (2008). Age and social gradients in the intensity of aging males’ symptoms in Poland. Aging Male, 11(2), 83–88. doi: 10.1080/13685530701778020 [DOI] [PubMed] [Google Scholar]
- Jenkins L. C., Mulhall J. P. (2015). Delayed orgasm and anorgasmia. Fertility and Sterility 104(5), 1082–1088. doi: 10.1016/j.fertnstert.2015.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong J. Y., Lee S. K., Kang Y. W., Jang S. N., Choi Y. J., Kim D. H. (2011). Relationship between ED and depression among middle-aged and elderly men in Korea: Hallym aging study. International Journal of Impotence Research, 23(5), 227–234. doi: 10.1038/ijir.2011.32 [DOI] [PubMed] [Google Scholar]
- Jern P., Gunst A., Sandnabba K., Santtila P. (2012). Are early and current erectile problems associated with anxiety and depression in young men? A retrospective self-report study. Journal of Sex & Marital Therapy, 38(4), 349–364. doi: 10.1080/0092623x.2012.665818 [DOI] [PubMed] [Google Scholar]
- John N. A., Babalola S., Chipeta E. (2015). Sexual pleasure, partner dynamics and contraceptive use in Malawi. International Perspectives on Sexual and Reproductive Health, 41(2), 99–107. doi: 10.1363/4109915 [DOI] [PubMed] [Google Scholar]
- Justo D., Arbel Y., Mulat B., Mashav N., Saar N., Steinvil A., Heruti R., Banai S., Lerman Y. (2010). Sexual activity and erectile dysfunction in elderly men with angiographically documented coronary artery disease. International Journal of Impotence Research, 22(1), 40–44. doi: 10.1038/ijir.2009.45 [DOI] [PubMed] [Google Scholar]
- Kafka M. P. (2010). Hypersexual disorder: A proposed diagnosis for DSM-V. Archives of Sexual Behavior, 39(2), 377–400. doi: 10.1007/s10508-009-9574-7 [DOI] [PubMed] [Google Scholar]
- Kendirci M., Asci R., Yaman O., Cayan S., Orhan I., Usta M. F., Ekmekcioglu O., Kadioglu A. (2014). Prevalence of male pelvic dysfunction: Results from the Turkish society of andrology male sexual health study group. Andrology, 2(2), 219–224. doi: 10.1111/j.2047-2927.2013.00176.x [DOI] [PubMed] [Google Scholar]
- Khoo E. M., Tan H. M., Low W. Y. (2008). Erectile dysfunction and comorbidities in aging men: An Urban cross-sectional study in Malaysia. The Journal of Sexual Medicine, 5(12), 2925–2934. 10.1111/j.1743-6109.2008.00988.x [DOI] [PubMed] [Google Scholar]
- Kim J. H., Lau J. T. F., Cheuk K. K. (2009). Sexlessness among married Chinese adults in Hong Kong: Prevalence and associated factors. The Journal of Sexual Medicine, 6(11), 2997–3007. 10.1111/j.1743-6109.2009.01367.x [DOI] [PubMed] [Google Scholar]
- Kim O., Jeon H. O. (2013). Gender differences in factors influencing sexual satisfaction in Korean older adults. Archives of Gerontology and Geriatrics, 56(2), 321–326. 10.1016/j.archger.2012.10.009 [DOI] [PubMed] [Google Scholar]
- Kontula O., Haavio-Mannila E. (2009). The impact of aging on human sexual activity and sexual desire. Journal of Sex Research, 46(1), 46–56. doi: 10.1080/00224490802624414 [DOI] [PubMed] [Google Scholar]
- Korfage I. J., Roobol M., de Koning H. J., Kirkels W. J., Schröder F. H., Essink-Bot M.-L. (2008). Does “Normal” aging imply urinary, bowel, and erectile dysfunction? A general population survey. Urology, 72(1), 3–9. 10.1016/j.urology.2008.01.058 [DOI] [PubMed] [Google Scholar]
- Landripet I., Stulhofer A. (2015). Is pornography use associated with sexual difficulties and dysfunctions among younger heterosexual men? The Journal of Sexual Medicine, 12(5), 1136–1139. doi: 10.1111/jsm.12853 [DOI] [PubMed] [Google Scholar]
- Lee D. M., Nazroo J., O’Connor D. B., Blake M., Pendleton N. (2016). Sexual health and well-being among older men and women in England: Findings from the english longitudinal study of ageing. Archives of Sexual Behavior, 45(1), 133–144. doi: 10.1007/s10508-014-0465-1 [DOI] [PubMed] [Google Scholar]
- Lee D. M., Tajar A., Ravindrarajah R., Pye S. R., O’Connor D. B., Corona G., O’Connell M., Gielen E., Boonen S., Vanderschueren D., Pendleton N., Finn J. D., Bartfai G., Casanueva F. F., Forti G., Giwercman A., Han T. S., Huhtaniemi I. T., Kula K., . . . O’Neill T. W. (2013). Frailty and sexual health in older European men. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 68(7), 837-844. doi: 10.1093/gerona/gls217 [DOI] [PubMed] [Google Scholar]
- Lee S. W., Lee J. H., Sung H. H., Park H. J., Park J. K., Choi S. K., Kam S. C. (2013). The prevalence of premature ejaculation and its clinical characteristics in Korean men according to different definitions. International Journal of Impotence Research, 25(1), 12–17. doi: 10.1038/ijir.2012.27 [DOI] [PubMed] [Google Scholar]
- Lewis R. W. (2011). Epidemiology of sexual dysfunction in Asia compared to the rest of the world. Asian Journal of Andrology, 13(1), 152–158. doi: 10.1038/aja.2010.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang C. Z., Hao Z. Y., Li H. J., Wang Z. P., Xing J. P., Hu W. L., Zhang T. F., Ge W. W., Zhang X. S., Zhou J., Li Y., Zhou Z. X., Tang Z. G., Tai S. (2010). Prevalence of Premature Ejaculation and its correlation with chronic prostatitis in Chinese Men. Urology, 76(4), 962–966. 10.1016/j.urology.2010.01.061 [DOI] [PubMed] [Google Scholar]
- Liu C. C., Juan H. C., Lee Y. C., Wu W. J., Wang C. J., Ke H. L., Li W. M., Yeh H. C., Li C. C., Chou Y. H., Huang C. H., Huang S. P. (2010). The impact of physical health and socioeconomic factors on sexual activity in middle-aged and elderly Taiwanese men. Aging Male, 13(2), 148–153. doi: 10.3109/13685531003657792 [DOI] [PubMed] [Google Scholar]
- McMahon C. G. (2014). Management of ejaculatory dysfunction. Internal Medicine Journal, 44(2), 124–131. doi: 10.1111/imj.12344 [DOI] [PubMed] [Google Scholar]
- Mehta A., Sigman M. (2015). Management of the dry ejaculate: A systematic review of aspermia and retrograde ejaculation. Fertility and Sterility 104(5), 1074–1081. doi: 10.1016/j.fertnstert.2015.09.024 [DOI] [PubMed] [Google Scholar]
- Mitchell K. R., Geary R., Graham C., Clifton S., Mercer C. H., Lewis R., Macdowall W., Datta J., Johnson A. M., Wellings K. (2016). Sexual function in 16- to 21-year-olds in Britain. Journal of Adolescent Health, 59(4), 422–428. doi: 10.1016/j.jadohealth.2016.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell K. R., Mercer C. H., Ploubidis G. B., Jones K. G., Datta J., Field N., Copas A. J., Tanton C., Erens B., Sonnenberg P., Clifton S., Macdowall W., Phelps A., Johnson A. M., Wellings K. (2013). Sexual function in Britain: Findings from the third national survey of sexual attitudes and lifestyles (Natsal-3). The Lancet, 382(9907), 1817–1829. 10.1016/S0140-6736(13)62366-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mola J. R. (2015). Erectile dysfunction in the older adult male. Urologic Nursing, 35(2), 87–93. [PubMed] [Google Scholar]
- Montgomery K. A. (2008). Sexual desire disorders. Psychiatry (Edgmont (Pa. : Township)), 5(6), 50–55. [PMC free article] [PubMed] [Google Scholar]
- Moreau C., Kågesten A. E., Wm Blum R. (2016). Sexual dysfunction among youth: An overlooked sexual health concern. BMC Public Health, 16(1), 1–10. doi: 10.1186/s12889-016-3835-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutagaywa R. K., Lutale J., Aboud M., Kamala B. A. (2014). Prevalence of erectile dysfunction and associated factors among diabetic men attending diabetic clinic at Muhimbili National Hospital in Dar-es-Salaam, Tanzania. The Pan African Medical Journal, 17(1), 227. doi: 10.11604/pamj.2014.17.227.2695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni Lochlainn M., Kenny R. A. (2013). Sexual activity and aging. Journal of the American Medical Directors Association, 14(8), 565–572. 10.1016/j.jamda.2013.01.022 [DOI] [PubMed] [Google Scholar]
- Palacios-Ceña D., Carrasco-Garrido P., Hernández-Barrera V., Alonso-Blanco C., Jiménez-García R., Fernández-de-las-Peñas C. (2012). Sexual behaviors among older adults in Spain: Results from a population-based national sexual health survey. The Journal of Sexual Medicine, 9(1), 121–129. 10.1111/j.1743-6109.2011.02511.x [DOI] [PubMed] [Google Scholar]
- Park H. J., Park J. K., Park K., Lee S. W., Kim S. W., Yang D. Y., Moon, du G., Min K. S., Moon K. H., Yang S. K., Hyun J. S., Park N. C. (2010). Prevalence of premature ejaculation in young and middle-aged men in Korea: A multicenter internet-based survey from the Korean Andrological Society. Asian Journal Andrology, 12(6), 880–889. doi: 10.1038/aja.2010.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Permpongkosol S., Kongkakand A., Ratana-Olarn K., Tantiwong A., Tantiwongse K. (2008). Increased prevalence of erectile dysfunction (ED): Results of the second epidemiological study on sexual activity and prevalence of ED in Thai males. Aging Male, 11(3), 128–133. doi: 10.1080/13685530802278128 [DOI] [PubMed] [Google Scholar]
- Quek K. F., Sallam A. A., Ng C. H., Chua C. B. (2008). Prevalence of Sexual Problems and Its association with social, psychological and physical Factors among men in a Malaysian population: A cross-sectional study. The Journal of Sexual Medicine, 5(1), 70–76. 10.1111/j.1743-6109.2006.00423.x [DOI] [PubMed] [Google Scholar]
- Quinta Gomes A., Nobre P. (2014). Prevalence of sexual problems in Portugal: Results of a population-based study using a stratified sample of men aged 18 to 70 Years. Journal of Sex Research, 51(1), 13–21. doi: 10.1080/00224499.2012.744953 [DOI] [PubMed] [Google Scholar]
- Ralph D. J., Wylie K. R. (2005). Ejaculatory disorders and sexual function. British Journal of Urology International, 95(9), 1181–1186. doi: 10.1111/j.1464-410X.2005.05536.x [DOI] [PubMed] [Google Scholar]
- Ruiz-Muñoz D., Wellings K., Castellanos-Torres E., Álvarez-Dardet C., Casals-Cases M., Pérez G. (2013). Sexual health and socioeconomic-related factors in Spain. Annals of Epidemiology, 23(10), 620–628. doi: 10.1016/j.annepidem.2013.07.005 [DOI] [PubMed] [Google Scholar]
- Sand M. S., Fisher W., Rosen R., Heiman J., Eardley I. (2008). Original research: Erectile dysfunction and constructs of masculinity and quality of life in the multinational men’s attitudes to life events and sexuality (MALES) study. The Journal of Sexual Medicine, 5(3), 583–594. doi: 10.1111/j.1743-6109.2007.00720.x [DOI] [PubMed] [Google Scholar]
- Sathyanarayana Rao T. S., Ismail S., Darshan M. S., Tandon A. (2015). Sexual disorders among elderly: An epidemiological study in south Indian rural population. Indian Journal of Psychiatry, 57(3), 236–241. doi: 10.4103/0019-5545.166618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serefoglu E. C., Yaman O., Cayan S., Asci R., Orhan I., Usta M. F., Ekmekcioglu O., Kendirci M., Semerci B., Kadioglu A. (2011). The comparison of premature ejaculation assessment questionnaires and their sensitivity for the four premature ejaculation syndromes: Results from the Turkish society of andrology sexual health survey. The Journal of Sexual Medicine, 8(4), 1177–1185. doi: 10.1111/j.1743-6109.2010.02183.x [DOI] [PubMed] [Google Scholar]
- Spetz Holm A. C., Fredrikson M. G., Hammar M. L. (2012). Symptoms of testosterone deficiency in early middle aged men. Aging Male, 15(2), 78–84. doi: 10.3109/13685538.2012.669435 [DOI] [PubMed] [Google Scholar]
- Tang W. H., Zhuang X. J., Shu R. M., Guan D., Ji Y. D., Zhang B. L., Wang C. G., Zhuang L. H., Yang Z., Hong K., Ma L. L., Jiang H., Zhou S. J., Gu Y. Q. (2015). The prevalence of erectile dysfunction among subjects with late-onset hypogonadism: A population-based study in China. International Journal of Clinical and Experimental Medicine, 8(8), 13901–13910. [PMC free article] [PubMed] [Google Scholar]
- Tomlinson J. (1998). ABC of sexual health: Taking a sexual history. British Medical Journal, 317(7172), 1573–1576. doi: 10.1136/bmj.317.7172.1573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traeen B., Stigum H. (2010). Sexual problems in 18–67-year-old Norwegians. Scandinavian Journal of Public Health, 38(5), 445–456. doi: 10.1177/1403494810371245 [DOI] [PubMed] [Google Scholar]
- WHO. Proposed working definition of an older person in Africa for the MDS project. http://www.who.int/healthinfo/survey/ageingdefnolder/en/index.html
- Wong S. Y., Leung J. C., Woo J. (2009). A prospective study on the association between lower urinary tract symptoms (LUTS) and erectile dysfunction: Results from a large study in elderly Chinese in Southern China; The Journal of Sexual Medicine, 6(7), 2024–2031. doi: 10.1111/j.1743-6109.2009.01295.x [DOI] [PubMed] [Google Scholar]
- Wong S. Y. S., Leung J. C. S., Woo J. (2009). Sexual activity, erectile dysfunction and their correlates among 1,566 Older Chinese men in Southern China. The Journal of Sexual Medicine, 6(1), 74–80. doi: 10.1111/j.1743-6109.2008.01034.x [DOI] [PubMed] [Google Scholar]
- Wylie K., Kenney G. (2010). Review: Sexual dysfunction and the ageing male. Maturitas, 65(1), 23–27. doi: 10.1016/j.maturitas.2009.10.018 [DOI] [PubMed] [Google Scholar]
- Zhang H., Fan S., Yip P. (2016). The association between female sexual dysfunction and the husband’s erectile dysfunction: Evidence from married couples in Hong Kong. Journal of Sex & Marital Therapy, 42(3), 214–222. doi: 10.1080/0092623X.2014.996931 [DOI] [PubMed] [Google Scholar]
- Zhang H., Yip A. W. C., Fan S., Yip P. S. F. (2013). Male sexual dysfunction: Sexual dysfunction among Chinese married men aged 30-60 years: A population-based study in Hong Kong. Urology, 81(2), 334–339. doi: 10.1016/j.urology.2012.11.003 [DOI] [PubMed] [Google Scholar]
- Zhang X., Yang B., Li N., Li H. (2017). Prevalence and risk factors for erectile dysfunction in Chinese adult males. The Journal of Sexual Medicine, 14(10), 1201–1208. doi: 10.1016/j.jsxm.2017.08.009 [DOI] [PubMed] [Google Scholar]