Highlights
-
•
Intramedullary spinal dermoid cyst is a unique and rare.
-
•
A quick and accurate diagnosis is needed to achieve good outcome.
-
•
The motor and sensory functions before and after surgery are still the same.
Keywords: Intramedullary spine tumor, Dermoid cysts, Rare case, Case report
Abstract
Introduction
Intramedullary spine dermoid cysts are rare and benign tumors that occur mainly due to the defective closure of the neural tube during the development process. They are slow-growing tumor that manifest in the second and third decades of life. The prevalence of intramedullary dermoid cysts is only 1%.
Presentation of case
We reported a 30 years old female with chief complain of weakness of the right leg in the last 6 months before admission. She complained about back pain and had history of scoliosis. In MRI we found intramedullary tumor at level T11-L1. We performed marginal excision and sent the sample for histopathological examination. The histopathological result was dermoid cyst tumor.
Discussion
During six months of post-operative period, no recurrence was detected, and a complete relief of symptoms is as expected. Early diagnosis is needed for proper handling and to achieve good outcomes.
Conclusion
Dermoid cysts in adults without a history of trauma are a rare case. Surgical excision is the choice of treatment. However, long-term follow up is needed to monitor the sensory-motor function.
1. Introduction
Dermoid cyst rarely occurs in the spine, especially intramedullary. Only 1% of dermoid cyst occurs intramedullary. The predilection ranges from lumbosacral spine (60%), thoracic spine (10%) and cervical spine (5%) [1,2]. Dermoid cyst are histologically different from epidermoid cyst. Dermoid cyst is coated with dermis which contains skin appendages such as hair and sebaceous glands, while epidermoid cyst on the other hand is coated with multilevel squamous epithelium and only contains declaimed keratin [3]. Both lesions must also be distinguished from adult cystic teratomas which contain derivatives from more than one layer of embryological cell. They arise from the remnants of cells due to failure of embryological process involved in neural tube closure. The process begins in the neural tube which is the origin of lower cervical cord and continues to the rostral and caudal part [3,16].
This article reported a 30-year-old female with scoliosis and neurology deficit. We found intramedullary tumor at level T11-L1 from MRI. We performed excision and had done histopathology examination with result dermoid cyst. Written consent has been received from the subject. The authors declare no conflicts of interest. This work has been reported in line with the SCARE criteria [4].
2. Presentation of case
A 30-year-old female was presented with weakness of right leg in the last 6 months before admission. For the last 6 months, the patient could not move her right leg and she also felt numbness. The patient experienced back pain since a year ago. The pain was dull and intermittent. There was no radiating pain. The patient also stated that her spine was bent from birth, and the bending was felt progressing. The left leg was also smaller than the right leg from birth. There was no history of infection, spinal trauma, previous spinal surgery, difficulty in defecating and urinating. No previous medication was reported, and she also denied history of tumor in her family. The patient was a housewife. The clinical appearance of the patient was shown in Fig. 1.
Fig. 1.
Clinical picture of the patient.
On clinical examination we found the general state was normal. Local state of spine showed patient has deformity spinal curve with right angulation of the main spine, rib hump and pelvic tilt. The power on right lower limb was 2, we could not do the power measurement of the left lower limb due to the disfunction of the left leg since birth. Sensory examination revealed hypoesthesia bellow T11 dermatome. Physiological reflexes were normal.
From Plain radiograph of whole spine, we found scoliosis deformity with dominantly curve at thoracolumbal of 106 degree and another curve at main thoracic of 84 degree as was shown in Fig. 2.
Fig. 2.
Whole spine radiographic.
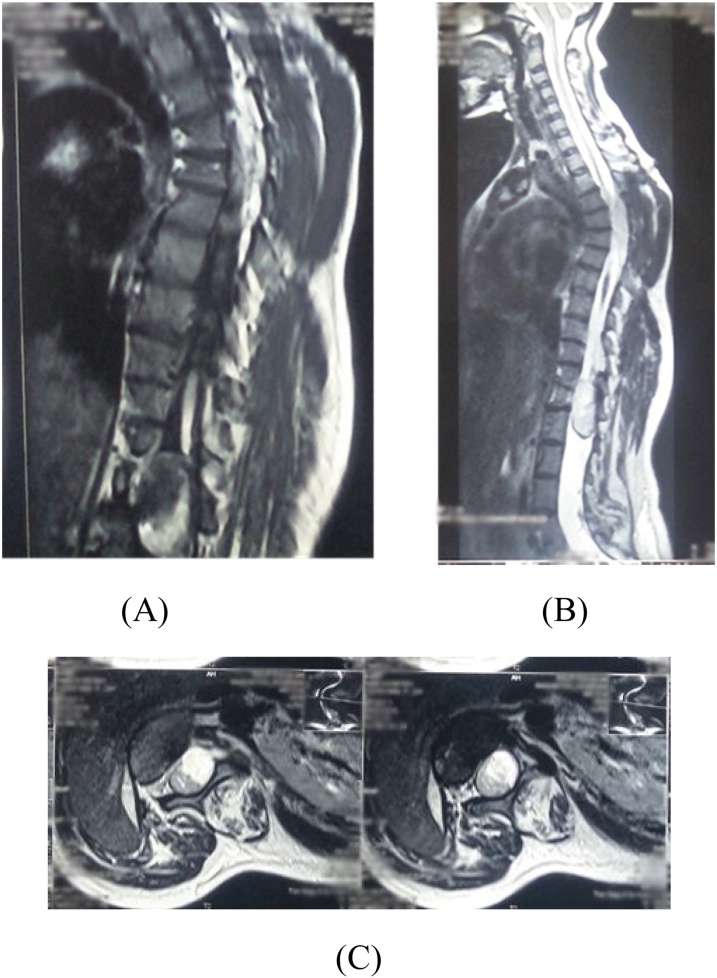
Magnetic resonance imaging (MRI), shown in Fig. 3, of the whole spine we found T2-T8 thoracic vertebral scoliosis with left convexity and T8-L5 level thoracolumbar with right convexity. A heterogenous intramedullary mass lesion (Intramedullary solid-cystic density mass). Oval size ± 4.3 × 2.4 cm as high as T11-L1 with syringomyelia in the cranial as high as T8,9,10. It was heterogeneously hyperintense on T2-weighted image and hypointense on T1-weight image. From MRI we suspected intramedullary tumor with suspected spinal astrocytoma for differential diagnosis.
Fig. 3.
Magnetic resonance imaging (MRI) of whole spine, (A) T1-Weighted (sagittal), (B) T2-weighted (sagittal), (C) T2-weighted (axial).
Our patient underwent an excisional tumor, the procedure was explained in Fig. 4. The procedure was performed by an orthopaedic spine consultant. The cyst was evacuated, and near total excision was done from the spinal cord. The result of histopathological examination, as seen in Fig. 5, of the tumor is dermoid cyst.
Fig. 4.
Steps of the surgical procedure.
Fig. 5.
Histopathology appearance; a. epidermis, b. creatine, c. hair shaft, d. cholesterol crystal.
After surgery, we referred the patient to medical rehab where she underwent physiotherapy for 2 weeks in order to be fully independent for basic activity of daily living (ADL). We also advice the patient to come to the orthopedic and medical rehab clinic. The patient explained that she did not feel any back pain anymore and she also felt no disturbance of the motor and sensory function. After six months, the operating outcomes were reassessed and there were no further disturbance in the patient.
3. Discussion
Dermoid cyst a rely occur in the spine, especially at the intramedullary site which was first described in 1745 by Verratus [2,5]. Intraspinal dermoid cysts, also called ‘spinal cutaneous inclusion tumors’ are rare, benign, slow-growing tumors that account for less than 1 percent of spinal tumors [6,7]. They are known to have a predilection for the lumbosacral spine 60%, thoracic spine 10% and cervical spine 5% [1,2]. In this case report, it was reported that a 30-year-old female patient with congenital scoliosis and left leg smaller than the right foot had complaints of weakness of the right leg in the last 6 months. After an MRI examination we get an intramedullary tumor as high as Th 11-L1.
Dermoid cyst can be congenital or acquired. These cysts constitute 1–2% of intraspinal tumors and are more common in children (10–17%). Congenital lesions are believed to result from the insertion of ectodermal cells during nerve tube closure in the third to fifth week of fetal life. Obtained lesions can occur due to trauma or surgery [8]. Common locations of dermoid cysts are scalp, skull, intracranial, and intraspinal, especially intradural extramedullary; rarely intramedullary and associated with other spinal defects [9]. In this patient however, the tumor was reported to occur in adult phase of life and there was no previous history of trauma. This indicate the atypical dermoid cyst case.
Symptoms generally occur slowly and are nonspecific, manifesting in childhood often cause delays in diagnosis. Young children and infants often experience severe pain, motor regression, weakness. Symptoms depend on the location, extent of the tumor and are the result of lesions that occupy spaces that cause compression of adjacent structures. Motor disturbances, pain, sensory disturbance, and urological dysfunction often occur [1,2]. Dermoid cysts usually appear in childhood or adulthood with a history of trauma. In this case even though the patient has an anomalous spinal development anomaly in the form of scoliosis, dermoid cyst appears at an older age after he experiences significant symptoms.
These cysts are often diagnosed when they appear clinically as neurological manifestations, from paresthesia to paralysis and sphincter complications [10]. In this case, the patient experiences numbness, weakness, and paresis develop into total immobility. The case series of epidermoid and dermoid spinal cord tumors presented by Bradford prove most cases present with urinary symptoms, either retention or incontinence [11], however, the patients in our case denied of having those symptoms. Gercek et al. also reported the case of a patient with a dyssynergia bladder dermoid cyst [12]. This case provides an excellent clinical picture of an intramedullary spinal dermoid cyst without classic symptoms of incontinence or signs of spinal dysraphism.
In our case, we also established the diagnosis of dermoid cysts in spinal surgery patients with the help of MRI and histopathological evaluation. The characteristics of signal intensity in MRI is vary, depending on cystic content. The two main components of fluid and fat appear hyperintense on T-1 weighted images that are most consistent with similar findings mentioned by Do-Dai DD et al. [9,11]. Areas with very hyper intensity reflect the secretion of sebaceous glands and liquid lipid metabolites. The solid portion of the tumor is slightly hypointense to isointense compared to the spinal cord. On the T2-weighted image, the area of T1 hyperintensity shows a relatively decreased signal intensity and heterogeneous dense part of the hyperintense tumor. The differential diagnosis of spinal dermoid cysts includes spinal lipoma, epidermoid cysts and myxopapillary ependymoma. MRI distinguishes the dermoid from lipoma based on the non-fat component of the previous one [9]. Fat hyperintensity is most specific for dermoid that are not seen in ependymomas and epidermoid. Intrinsic shortening of Tl also allows differentiation of the dermoid from the epidermoid [13]. In this case Magnetic resonance imaging (MRI) of the whole spine we found T2-T8 thoracic vertebral scoliosis with left convexity and T8-L5 level thoracolumbar with right convexity. A heterogenous intramedullary mass lesion (Intramedullary solid-cystic density mass). Oval size ± 4.3 × 2.4 cm as high as T11-L1 with syringomyelia in the cranial as high as T8,9,10. It was heterogeneously hyperintense on T2-weighted image and hypointense on T1-weight image. From MRI we suspected intramedullary tumor with suspected spinal astrocytoma for differential diagnosis.
The best diagnosis to find out the type of tumor is histopathological examination. From the histopathological examination obtained aggregates of keratinocytes along with keratin flakes with degeneration. These tumors are usually surrounded by a multi-layered, cornified epithelium with a collagen stroma lying in the dermis and hypodermis with cutaneous appendages, such as hair follicles, hair, sebaceous and sweat glands as well as sebum [2,5]. Dermoid cysts are histologically different from epidermoid because they are coated with dermis which contains skin appendages such as hair and sebaceous glands. The epidermoid on the other hand is coated with multilevel squamous epithelium and only contains declaimed keratin [3]. Both lesions must also be distinguished from adult cystic teratomas which contain derivatives from more than one embryological cell layer. They arise from the remnants of cells due to failure of the embryological process involved in the closure of nerve tubes. This process begins in the area of the neural tube that is destined to become a lower cervical cord and continues to the rostral and caudal [16]. Patient underwent excision cyst and performed histopathology examination we have obtained the results of preparations with information on the origin of intradural tumors showing pieces of connective tissue in layers of layered squamous epithelium keratin with hair follicles containing hair shaft, cholesterol crystals and pieces of calcification. Can be concluded is a dermoid cyst.
The treatment of choice for dermoid cysts is the excision of the total mass at an early stage. Excision of total mass is possible for extramedullary dermoid cysts; However, in intramedullary dermoid cysts, the capsule is attached to the spinal cord and often causes difficulty in complete resection through surgery [9,10,14]. In our case, the tumor had a well-defined boundary so that total resection can be performed. Dermoid cysts can rupture during surgery, after trauma, or spontaneously. This can cause the spread of content along the subarachnoid and ventricular spaces which causes aseptic chemical meningitis [5]. In this case there were no postoperative chemical meningitis, after removal of intramedullary dermoid cysts.
Kane et al. published a series of 54 patients with intramedullary spinal cord tumors treated with surgery reported that adjuvant postoperative radiotherapy was not used routinely if complete tumor removal was achieved, it can be concluded that the effectiveness of radiotherapy is still unclear and has not been demonstrated [13]. Especially for patients with low-grade tumors do not need radiotherapy [14,15]. In this patient no postoperative radiotherapy was performed.
In the early postoperative course, we observed CSF leaks and meningitis [14]. Cases of recurrence of literature are rare. Surgical removal can be complicated by capsule compliance. Partial capsule removal might increase the recurrence rate but even so, recurrence seems to be rare and is associated with giant and extended cyst features, which represent a real surgical challenge. Long-term follow-up is required [15].
Postoperative results are closely correlated with histological type and infiltrative tumor growth rate. Lesions located in the thoracic region appear to have an increased risk of surgical morbidity. But the most important predictive factor for postoperative outcomes is preoperative neurological conditions. According to Sandalcioglu IE et al. to get a good functional outcome that operative treatment should be performed in an early stage of the disease [14].
In this patient we did not get any signs of CSF leak and no signs of meningitis were found. The motor and sensory functions before and after surgery are still the same. During intraoperative we monitor motor function using EMG, we do not get any changes in motor function during the operation until the operation is finished.
4. Conclusion
Dermoid cysts in adults without a history of trauma are special and rare events. A quick and accurate diagnosis is needed for proper handling and can produce good outcomes. We already performed an excisional surgery to remove all of the dermoid cyst. There was no difference from the motoric and the sensory result post operation Rehabilitation after surgery are needed to get optimal results.
Funding
The authors report no external source of funding during the writing of this article.
Ethical approval
Ethical approval was not required in the treatment of the patient in this report.
Consent
Written consent has been received from the subject.
Author contribution
Luthfi Gatam contributes in the study concept or design, data collection, analysis and interpretation, oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team.
Prima Enky Merthana contributes to the study concept or design, data collection and writing the paper.
Registration of research studies
Does not need any registration.
Guarantor
Luthfi Gatam is the sole guarantor of this submitted article.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of Competing Interest
The authors declare no conflicts of interest.
References
- 1.Kumar S., Gupta S., Puri V., Gupta R.K., Malik R. Intramedullary dermoids in children. Indian Pediatr. 1990;27(6):626–629. [PubMed] [Google Scholar]
- 2.Najjar M.W., Kusske J.A., Hasso A.N. Dorsal intramedullary dermoids. Neurosurg. Rev. 2005;28(4):320–325. doi: 10.1007/s10143-005-0382-9. [DOI] [PubMed] [Google Scholar]
- 3.Li Q., You C., Zan X., Chen N., Zhou L., Xu J. Mature cystic teratoma (dermoid cyst) in the sylvian fissure: a case report and review of the literature. J. Child Neurol. 2012;27(2):211–217. doi: 10.1177/0883073811415681. [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 5.Sanaullah M., Mumtaz S., Memon A.A., Hashim A.S.M., Bashir S. Intramedullary dermoid cyst with relatively atypical symptoms. J. Med. Case Rep. 2013;7(104) doi: 10.1186/1752-1947-7-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rapoport R.J., Flanders A.E., Tartaglino L.M. Intradural extramedullary causes of myelopathy. Semin. Ultra-Sound CT MR. 1994;15(3):189–225. doi: 10.1016/S0887-2171(05)80072-1. [DOI] [PubMed] [Google Scholar]
- 7.Gujarathi A., Patil A., Naware S.S., Kulkarni Vilas M. Intramedullary dermoid cyst a rare case report. J. Krishna Inst. Med. Sci. Univ. 2014;3(2):136–139. [Google Scholar]
- 8.Van Aalst J., Hoekstra F., Beuls E.A., Cornips E.M., Weber J.W., Sival D.A., Creytens D.H., Vles J.S. Intraspinal dermoid and epidermoid tumors: report of 18 cases and reappraisal of the literature. Pediatr. Neurosurg. 2009;45(4):281–290. doi: 10.1159/000235602. [DOI] [PubMed] [Google Scholar]
- 9.Bradford F.K. Intramedullary dermoid cyst. Ann. Surg. 1938;107(1):107–115. doi: 10.1097/00000658-193801000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gercek E., Kaplan M., Erol F.S., Overen M.F. Dissynergic bladder and hydronephrosis in a case of spinal intramedullary dermoid cyst. Fırat Tıp Dergisi. 2009;14(2):137–140. [Google Scholar]
- 11.Do-dai D.D., Brooks M.K., Goldkamp A., Erbay S., Bhadelia R.A. Magnetic resonance imaging of intramedullary spinal cord lesions: a pictorial review. Curr. Probl. Diagn. Radiol. 2010;39(4):160–185. doi: 10.1067/j.cpradiol.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 12.De Maio P.N., Mikulis D.J., Kiehl T.R., Guha A. AIRP best cases in radiologic-pathologic correlation: Spinal conus dermoid cyst with lipid dissemination. Radiographics. 2012;32(4):1215–1221. doi: 10.1148/rg.324115018. [DOI] [PubMed] [Google Scholar]
- 13.Kane P.J., El-Mahdy W., Singh A., Powell M.P., Crockard H.A. Spinal intradural tumours: Part II – intramedullary. Br. J. Neurosurg. 1999;13(6):558–563. doi: 10.1080/02688699943051. [DOI] [PubMed] [Google Scholar]
- 14.Sandalcioglu I.E., Gasser T., Asgari S., Lazorisak A., Engelhorn T., Egelhof T., Stolke D., Wiedemayer H. Functional outcome after surgical treatment of intramedullary spinal cord tumors: experience with 78 patients. Int. Spinal Cord Soc. 2005;43(1):34–41. doi: 10.1038/sj.sc.3101668. [DOI] [PubMed] [Google Scholar]
- 15.Graillon T., Rakotozanany P., Meyer M., Dufour H., Fuentes S. Intramedullary epidermoid cyst in adult: case report and update literature review. Neurochirurgie. 2017;63(2):99–102. doi: 10.1016/j.neuchi.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Falavigna A., Righesso O., Hauschild L., Scatola F. Concomitant dermoid cysts of conus medullaris and cauda equina. Global Spine J. 2015;5 doi: 10.1055/s-0035-1554594. [DOI] [PubMed] [Google Scholar]