Abstract
Four cases (age range, 60-78 years, male:female = 1:3) who had undergone cholecystectomy presented with fever (n = 1), right abdominal pain with fever (n = 1), appetite loss with fever (n = 1), and absence of symptoms (n = 1). Computed tomography (CT) showed an irregular-shaped invasive mass or fluid collection in the right Morrison's pouch, right paracolic gutter, gallbladder fossa, subphrenic space, or abdominal wall. CT and ultrasound revealed gallstones in the granuloma in 3 cases and an abscess in one case. The inflammatory process induced by dropped gallstones may mimic peritoneal malignancies. Awareness of cholecystectomy and the detection of gallstones in the lesion are essential for the diagnosis of dropped gallstones.
Keywords: Foreign-body granuloma, Dropped gallstone, Laparoscopic cholecystectomy, Spilled gallstone
Introduction
Gallstones are a common digestive disorder, with a prevalence of approximately 10%-20% in North America and Europe and <10% in Asia. Most individuals with gallstones are asymptomatic; however, severe symptoms and complications develop in approximately 1%-3% of asymptomatic or mildly symptomatic patients annually [1]. Acute cholecystitis predominantly occurs as a complication of gallstone disease, and laparoscopic cholecystectomy is widely accepted as a standard surgical procedure, even for patients with acute cholecystitis associated with high-grade inflammation [2]. Dropped gallstones, also known as spilled gallstones, during cholecystectomy is an inevitable complication in patients with calculous cholecystitis due to a brittle gallbladder. In addition, it is challenging to retrieve gallstones in the abdominal cavity. Most cases with dropped gallstones are asymptomatic; however, once abscesses or granulomas develop, patients suffer from general fatigue, fever, pain, and weight loss. The imaging findings may mimic other peritoneal lesions, such as tuberculosis, actinomycosis, peritoneal loose body, and primary and secondary peritoneal tumor [3]. Therefore, the correct diagnosis is required for appropriate management. We report 4 cases of foreign-body granulomas and abscesses caused by dropped gallstones, and demonstrate the various imaging findings and clinical course.
Case presentation
Case 1
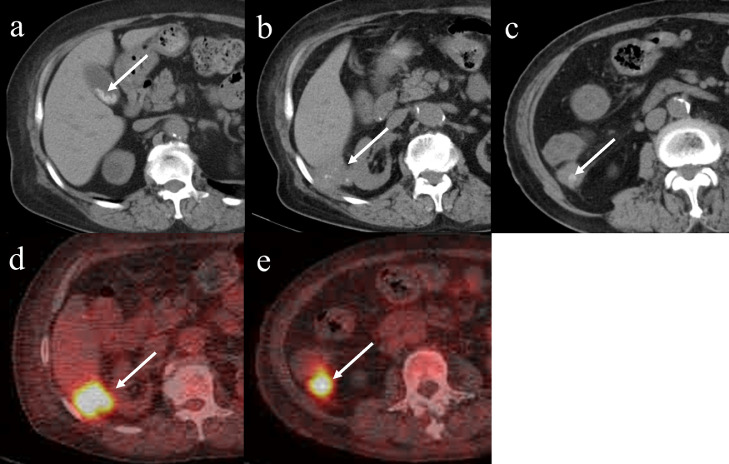
A 67-year-old woman underwent laparoscopic cholecystectomy because of biliary colic caused by gallstones (Fig. 1a). Because of the patient's perforated gallbladder, the gallstones dropped into the peritoneal cavity during laparoscopic cholecystectomy, and they were retrieved as much as possible. She presented with persistent low-grade fever 8 months after laparoscopic cholecystectomy. Computed tomography (CT) images revealed an irregular-shaped soft-tissue mass with invasive growth into the liver parenchyma and abdominal wall that contained punctate and nodular calcification in the right Morrison's pouch and right paracolic gutter, respectively (Figs. 1b and c). 18F-Fluorodeoxyglucose positron emission tomography with CT (FDG-PET/CT) revealed high FDG uptake in the soft-tissue masses (Figs. 1d and e). On CT, the appearance of calcification in the soft-tissue mass in the right paracolic gutter (Fig. 1c) was similar to that of the gallstones on a previous preoperative CT (Fig. 1a), which suggested foreign-body granulomas caused by dropped gallstones during the previous laparoscopic cholecystectomy. Pathological specimen examination obtained by percutaneous biopsy confirmed the foreign-body granuloma associated with fragments of pigment gallstones and chronic suppurative inflammation. No bacteria were detected by tissue culture. The patient underwent antimicrobial treatment, and follow-up CT at 5 months revealed a slight enlargement of the right Morrison's pouch lesion and a decrease in the size of the right paracolic gutter lesion. Biochemical examination 3 years after surgery revealed progression of the inflammatory condition, and percutaneous drainage was performed. Since then, the patient has been asymptomatic.
Fig. 1.
A 67-year-old woman with dropped gallstones (case 1). Numerous gallstones were seen on noncontrast CT before laparoscopic cholecystectomy (a: arrow). An irregular-shaped soft-tissue mass containing punctate calcifications was observed in the right Morrison's pouch on noncontrast CT (b: arrow). The mass invaded into the liver parenchyma and abdominal wall. The other irregular-shaped soft-tissue mass with nodular calcification was seen in the right paracolic gutter on noncontrast CT (c: arrow). The nodular calcification (c: arrow) was similar to the gallstones on CT before laparoscopic cholecystectomy (a: arrow). The tracer accumulated in the right Morrison's pouch lesion (SUVmax; 9.3) (d: arrow) and right paracolic gutter lesion (SUVmax; 8.0) (e: arrow) 120 minutes after intravenous administration of the tracer on 18F-fluorodeoxyglucose positron emission tomography with CT images. SUVmax; maximum standard uptake value
Case 2
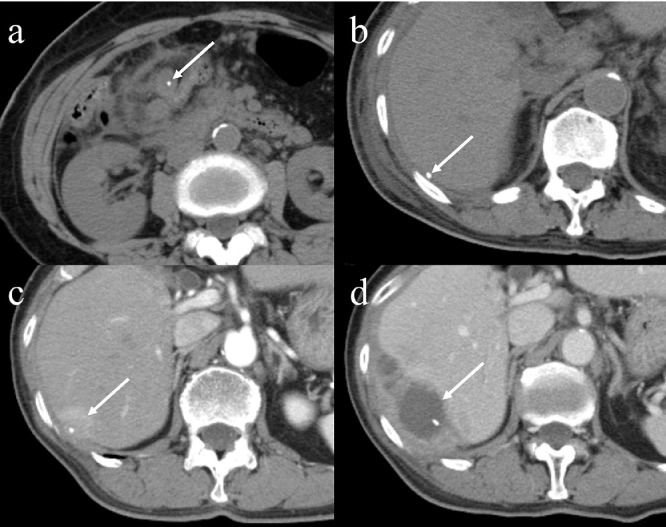
A 60-year-old woman presented with fever and right abdominal pain and was diagnosed with necrotizing cholecystitis based on CT findings (Fig. 2a). She underwent open cholecystectomy, after which perforated gallbladder and abscess spread around the gallbladder were observed. Four days after surgery, CT revealed a calcified stone in the right subphrenic space, which was similar to the gallstone near the perforated gallbladder (Fig. 2b). However, since discharge, the patient has experienced no symptoms, and no abnormal findings have been detected on blood tests. A follow-up CT 3 months after surgery showed a newly developed enhancing soft-tissue lesion around the calcified stone that was invading the right diaphragm and liver parenchyma (Fig. 2c). A diagnosis of foreign-body granuloma caused by a dropped gallstone was made based on the shape of the central calcified stone, which resembled the gallstone observed on the preoperative CT (Fig. 2a). The patient was seen without any specific treatment; however, right abdominal pain appeared seven months after surgery. Although her symptoms improved using antibiotics, they recurred after cessation of antibiotic treatment. One year after surgery, an abscess in the right subphrenic space was found on CT (Fig. 2d), and open surgical drainage was performed. Bacteroides fragilis was detected in the drainage fluid by a culture test.
Fig. 2.
A 60-year-old woman with dropped gallstones (case 2).The calcified gallstone was seen in the inflamed gallbladder on noncontrast CT (a: arrow). The calcified stone was moved to the right subphrenic space on noncontrast CT 4 days after the surgery (b: arrow). Newly developed enhanced soft tissue around the calcified stone on contrast-enhanced CT at 3 months after the surgery (c: arrow). The lesion developed into an abscess on contrast-enhanced CT 1 year after the surgery (d: arrow).
Case 3
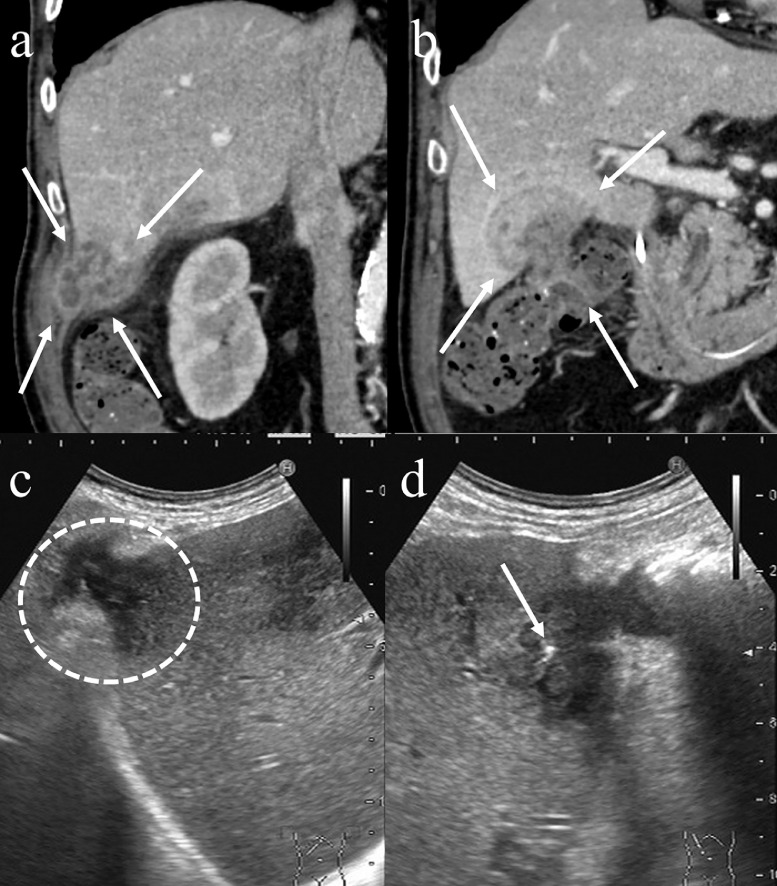
A 78-year-old man presented with appetite loss and right upper quadrant pain 5 months after laparoscopic cholecystectomy for calculous cholecystitis. Contrast-enhanced CT revealed 2 irregular-shaped lesions with multilocular fluid collection and thick septation in the right Morrison pouch and gallbladder fossa invading the liver, abdominal wall, and colon (Figs. 3a and b). No calcification was detected inside the lesions on noncontrast CT. Ultrasound (US) examination revealed a hyperechoic lesion, which suggested gallstones in these lesions within the gallbladder fossa (Figs. 3c and d). Colonoscopy demonstrated no tumor in the colon. An abscess caused by the dropped gallstones was diagnosed clinically based on CT and US findings. Percutaneous biopsy was performed, and granuloma with abscess formation was identified on the histopathologic examination. The patient was treated with antibiotics, and clinical symptoms and inflammatory findings improved.
Fig. 3.
A 78-year-old man with dropped gallstones (case 3). Two irregular-shaped masses with multilocular fluid collection and thick septation that invaded the liver, abdominal wall, and colon were seen in the right Morrison's pouch (a: arrow) and the gallbladder fossa on contrast-enhanced CT (b: arrows). The hypoechoic mass in the right Morrison's pouch invaded both the liver parenchyma and abdominal wall on US (c: circle). The hypoechoic mass in the gallbladder fossa invaded the liver parenchyma and revealed a hyperechoic lesion on US (d: arrow).
Case 4
A 67-year-old woman underwent laparoscopic cholecystectomy for calculous cholecystitis caused by gallstones (Fig. 4a). During the surgery, gallstones dropped into the peritoneal cavity as a result of gallbladder wall perforation. Because the patient had no symptoms or abnormal findings in a blood examination, she was observed without therapy. CT obtained 3 months after surgery demonstrated a soft-tissue lesion with calcification adjacent to the right rectus abdominal muscle, possibly in the port site of the laparoscopy (Fig. 4b). The calcification within the lesion resembled gallstones presented on the preoperative CT (Fig. 4a); therefore, a diagnosis of foreign-body granuloma caused by dropped gallstones was made. CT obtained 6 months after surgery revealed that one of the calcified foci had disappeared, and the size of the surrounding soft tissue had decreased (Fig. 4c). The patient currently presents with no symptoms and is still under observation.
Fig. 4.
A 67-year-old woman with dropped gallstones (case 4). Several gallstones were seen in the distended gallbladder with a thickened wall on noncontrast CT (a: arrows). The mass containing 2 calcified foci, which invaded the surrounding soft tissue, was observed next to the right rectus abdominal muscle on noncontrast CT at three months after the surgery (b: arrow). The mass decreased in size, and one of the calcifications disappeared on noncontrast CT 6 months after the surgery (c: arrow).
Discussion
Gallbladder perforation and dropped gallstones during cholecystectomy have been reported to occur in 6%-40% and in 1%-20% of cases, respectively [4], [5], [6], [7], [8]. Dropped gallstones may cause further complications, including granulomas and abscesses in 20% of cases with dropped gallstones and in 0.08%-2.9% of all laparoscopic cholecystectomy cases [5,6,8]. The retrieval of dropped gallstones after gallbladder perforation is difficult, particularly during laparoscopic surgery, because the operative field view is limited. Patients may develop various nonspecific symptoms, such as fever, pain, and weight loss, with a duration of months or years after cholecystectomy, with one case developing complications 10 years after surgery[9], [10], [11].
Granulomas and abscesses from dropped gallstones are thought to develop as a result of mechanical pressure caused by the stones, reaction to foreign bodies, stimulation of bile, and infection of bacterial species present in the gallstone. The type of gallstone can also influence development; in particular, pigment gallstones present a higher risk than cholesterol stones because the former often contain bacterial microcolonies [12]. A larger size (>1.5 cm) and number (>15 stones) of dropped gallstones and older patient age are also risk factors [4,8,13]. Antibiotic treatment and percutaneous drainage are often selected as the initial steps for management. In cases with protracted inflammation associated with residual stones, open surgery may be required to completely remove the dropped gallstones and prevent recurrence. Fistula formation is known to be an unusual complication of dropped gallstones [3]. Gallstones may migrate through a fistula to the extra-abdominal cavity, such as the gastrointestinal tract, diaphragm, and abdominal wall. The gallstone may be removed naturally through a fistula (as in one of our current cases), with the dropped gallstone found in the abdominal wall (case 4).
In imaging studies, granulomas and abscesses related to dropped gallstones are typically seen as a soft-tissue mass and fluid collection that sometimes infiltrate into the surrounding structures. Differential diagnosis may include peritoneal loose body, primary and secondary peritoneal neoplasms, malignant lymphoma, and sarcoma for granuloma type and simple abscess, actinomycosis, tuberculosis, and necrotizing tumors for abscess type [3]. However, a history of cholecystectomy and the identification of dropped gallstones within the granulomas or abscesses on imaging are crucial for diagnosis the etiology. In this case series, the use of CT enabled the clear visualization of the granulomas or abscesses in all 4 cases, and calcified foci corresponding to dropped gallstones were identified as high-density structures in 3 of 4 cases. The reason for this is that cholesterol gallstones or low-calcium gallstones are iso-dense on CT [14]. However, US successfully revealed a gallstone in case 3. Thus, US examination is valuable for detecting stones that fail to be identified on CT so essential for the diagnosis of dropped gallstones [15]. In the current case series, the lesions were found in the right colic gutter (case 1), Morison's pouch (case 1 and 3), right subphrenic space (case 2), gallbladder fossa (case 3), and abdominal wall (case 4). According to a previous report, gallstones often drop in the right subphrenic space, Morison's pouch, gallbladder fossa, and pelvic cavity. However, unusual locations, such as the retroperitoneum, gastric wall, right thorax, abdominal wall, and the incisional and trocar sites, have been described [11], [16]. Calcified foci in the mass or fluid collection on CT and US is essential for diagnosing this etiology, especially in an unusual site.
18F-FDG-PET/CT demonstrated high FDG uptake in the lesion in one case, presumably representing the presence of high-grade active inflammation or malignant tumors (case 1). 18F-FDG-PET also demonstrated a various degree of FDG uptake in foreign-body granulomas caused by dropped gallstones [17]. Thus, 18F-FDG-PET studies may have limited value in differentiating granulomas and abscesses related to dropped gallstones from other malignant tumors.
Conclusion
We have reported cases of foreign-body granulomas with and without abscesses caused by dropped gallstones. Gallbladder perforation and dropped gallstones are possible complications of cholecystectomy. In patients who have undergone cholecystectomy in whom an irregular soft-tissue mass or fluid collection infiltrating the surrounding tissue is detected on imaging, foreign-body granulomas or abscesses caused by dropped gallstones should be considered. The identification of dropped gallstoneswithin the lesion is essential for differentiating this condition from other mimicking diseases.
Footnotes
Acknowledgements: No funding was received for this study. The authors would like to thank Enago (www.enago.jp) for the English language review.
Declaration of Competing Interest: The authors have no competing interests to report.
References
- 1.Friedman GD. Natural history of asymptomatic and symptomatic gallstones. Am J Surg. 1993;165(4):399–404. doi: 10.1016/s0002-9610(05)80930-4. [DOI] [PubMed] [Google Scholar]
- 2.Khalid M, Rashid M. Gallstone abscess: a delayed complication of spilled gallstone after laparoscopic cholecystectomy. EmergRadiol. 2009;16(3):227–229. doi: 10.1007/s10140-008-0730-5. [DOI] [PubMed] [Google Scholar]
- 3.Nayak L, Menias CO, Gayer G. Dropped gallstones: spectrum of imaging findings, complications and diagnostic pitfalls. Br J Radiol. 2013;86(1028) doi: 10.1259/bjr.20120588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zehetner J, Shamiyeh A, Wayand W. Lost gallstones in laparoscopic cholecystectomy: all possible complications. Am J Surg. 2007;193(1):73–78. doi: 10.1016/j.amjsurg.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 5.Schäfer M, Suter C, Klaiber C, Wehrli H, Frei E, Krähenbühl L. Spilled gallstones after laparoscopic cholecystectomy. A relevant problem? A retrospective analysis of 10,174 laparoscopic cholecystectomies. Surg Endosc. 1998;12(4):305–309. doi: 10.1007/s004649900659. [DOI] [PubMed] [Google Scholar]
- 6.Memon MA, Deeik RK, Maffi TR, Fitzgibbons RJ. The outcome of unretrieved gallstones in the peritoneal cavity during laparoscopic cholecystectomy.A prospective analysis. Surg Endosc. 1999;13(9):848–857. doi: 10.1007/s004649901118. [DOI] [PubMed] [Google Scholar]
- 7.Rammohan A, Srinivasan UP, Jeswanth S, Ravichandran P. Inflammatory pseudotumour secondary to spilled intra-abdominal gallstones. Int J Surg Case Rep. 2012;3(7):305–307. doi: 10.1016/j.ijscr.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woodfield JC, Rodgers M, Windsor JA. Peritoneal gallstones following laparoscopic cholecystectomy: incidence, complications, and management. SurgEndosc. 2004;18(8):1200–1207. doi: 10.1007/s00464-003-8260-4. [DOI] [PubMed] [Google Scholar]
- 9.Morrin MM, Kruskal JB, Hochman MG, Saldinger PF, Kane RA. Radiologic features of complications arising from dropped gallstones in laparoscopic cholecystectomy patients. AJR Am J Roentgenol. 2000;174(5):1441–1445. doi: 10.2214/ajr.174.5.1741441. [DOI] [PubMed] [Google Scholar]
- 10.Singh K, Wang ML, Ofori E, Widmann W, Alemi A, Nakaska M. Gallstone abscess as a result of dropped gallstones during laparoscopic cholecystectomy. Int J Surg Case Rep. 2012;3(12):611–613. doi: 10.1016/j.ijscr.2012.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bartels AK, Murali AR, Zamora JG. Subhepatic sterile abscess 10 years after laparoscopic cholecystectomy. ACG Case Rep J. 2015;2(2):113–115. doi: 10.14309/crj.2015.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stewart L, Smith AL, Pellegrini CA, Motson RW, Way LW. Pigment gallstones form as a composite of bacterial microcolonies and pigment solids. Ann Surg. 1987;206(3):242–250. doi: 10.1097/00000658-198709000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brockmann JG, Kocher T, Senninger NJ, Schürmann GM. Complications due to gallstones lost during laparoscopic cholecystectomy. SurgEndosc. 2002;16(8):1226–1232. doi: 10.1007/s00464-001-9173-8. [DOI] [PubMed] [Google Scholar]
- 14.Singh AK, Levenson RB, Gervais DA, Hahn PF, Kandarpa K, Mueller PR. Dropped gallstones and surgical clips after cholecystectomy: CT assessment. J Comput Assist Tomogr. 2007;31(5):758–762. doi: 10.1097/RCT.0b013e3180340358. [DOI] [PubMed] [Google Scholar]
- 15.Viera FT, Armellini E, Rosa L, Ravetta V, Alessiani M, Dionigi P. Abdominal spilled stones: ultrasound findings. Abdom Imaging. 2006;31(5):564–567. doi: 10.1007/s00261-005-0241-8. [DOI] [PubMed] [Google Scholar]
- 16.Horton M, Florence MG. Unusual abscess patterns following dropped gallstones during laparoscopic cholecystectomy. Am J Surg. 1998;175(5):375–379. doi: 10.1016/S0002-9610(98)00048-8. [DOI] [PubMed] [Google Scholar]
- 17.Gorospe Luis. Intraperitoneal spilled gallstones presenting as fever of unknown origin after laparoscopic cholecystectomy: FDG PET/CT Findings. Clin Nucl Med. 2012;37(8):819–820. doi: 10.1097/RLU.0b013e31824c6042. [DOI] [PubMed] [Google Scholar]