Summary:
Carbon ion radiotherapy (CIRT) has been used for malignant tumors that are difficult to excise surgically, such as sacral chordoma, and the success of its outcomes is attributable to the high dose concentration and biological effects. CIRT has produced successful clinical outcomes, and it is considered to have fewer adverse effects on surrounding normal tissues; moreover, complications have been rarely reported. We describe a 75-year-old woman with a full-thickness sacral defect, who had received CIRT for sacral chordoma 3 years earlier. Computed tomography showed sacral bone destruction, and a colonoscopy revealed rectal necrosis. Rectectomy in addition to sacral bone resection was necessary, which resulted in a huge sacral defect of slightly anxious viability. We performed reconstruction of the sacral defect by using pedicled vertical rectus abdominis myocutaneous (VRAM) flap, obliterating sacral defects and intrapelvic dead space that occurred after rectectomy. Six months after surgery, the wound had healed well, and no complication was observed. Sacral complications after CIRT may affect surrounding normal tissues such as the rectum, and it would be difficult to reconstruct the resulting complications. The vertical rectus abdominis myocutaneous flap is considered useful for the simultaneous obliteration of sacral defects and intrapelvic dead space after CIRT.
In recent years, carbon ion radiotherapy (CIRT) has been used in the treatment of malignant tumors that are difficult to excise surgically, such as sacral chordoma. Local recurrence and survival rates after CIRT have been better than those after surgery.1 In comparison with conventional radiotherapy, the dose of CIRT delivered to lesions is lower, and CIRT is considered to have fewer adverse effects on surrounding normal tissues. Moreover, there have been only a few reports about complications after CIRT.2 On the other hand, it is a relatively new treatment. We describe a case of successful reconstruction with the use of pedicled vertical rectus abdominis myocutaneous (VRAM) flap for sacral and rectal necrosis that occurred as a complication of CIRT.
CASE PRESENTATION
The patient was a 75-year-old woman who had received CIRT (6720 cGy in 16 fractions) for sacral chordoma 3 years earlier. Two years and 6 months after the radiotherapy, she visited Gunma University Hospital because of sacral pain, tissue necrosis, and rectum-to-sacrum fistula. She received a proctostomy and underwent palliative debridement of necrotic tissue by the gastroenterologic and orthopedic surgeons in our hospital. After the operation, the sacral wound was left open, and the patient consulted plastic surgery for reconstruction of the wound.
At the first visit, we observed a sacral skin ulcer. Central necrosis of subcutaneous tissue and bone had led to a full-thickness defect, and the rectum was exposed through the defect (Fig. 1A). Computed tomography showed the sacral bone destruction and cystic changes, and a colonoscopy revealed that the rectal mucosa was necrotic (Fig. 1B). The patient did not complain of urination disorder or any other myelopathy.
Fig. 1.
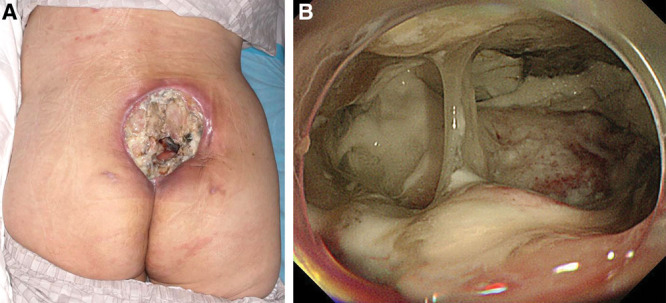
Clinical and endoscopic findings. A, Tissue necrosis from the skin to the bone was observed in the sacrum, and the rectum was exposed through the sacral defect. B, Colonoscopy revealed rectal intestinal necrosis.
Orthopedic and gastroenterologic surgeons performed radical debridement and sacrectomy with the patient in the prone position until viable tissue was exposed. Then, after repositioning in the supine position, rectectomy with Miles procedure was performed. Subsequently, a VRAM flap was created and elevated and then transferred to the sacral region through the intrapelvic space, and the donor site was closed in a layered manner. The insertion of the rectus abdominis was preserved to avoid excess tension on the pedicle. After the patient was moved into the prone position, the flap was carefully brought out from intrapelvic space and set into the sacral defect (Fig. 2).
Fig. 2.

The rectus abdominis myocutaneous flap was elevated and brought into the sacral defect through the intrapelvic space.
Postoperatively, the wound healed completely, and computed tomography revealed that the intrapelvic dead space and sacral region were filled with the rectus abdominis flap (Fig. 3). No complication of sacral or donor site was observed at the postoperative 6-month follow-up visit.
Fig. 3.

Sacral appearance after the reconstruction.
DISCUSSION
Sacral full-thickness tissue defects with rectum necrosis are rarely reported as complications of CIRT; we demonstrated that it could be successfully reconstructed with a transpelvic VRAM flap. Sacral full-thickness tissue necrosis containing rectum after CIRT is extremely rare and dangerous; only 2 cases have been reported, and both patients died.2 To the best of our knowledge, our case is the first in which reconstruction for sacral complications of CIRT was successful.
CIRT has been used as a treatment for unresectable malignant tumors, such as sacral chordoma, and the success of its outcomes is attributable to the high dose concentration and biological effects. Imai et al1 reported that the 5-year rate of local control after CIRT for chordoma was 77.2%, whereas those rates after surgery have ranged from 35% to 50%. The mechanism of CIRT is the release of low radiation dose along the travel path, except for the maximum energy at the end of the path (Bragg peak); thus, CIRT allows selective irradiation of the target tumor, sparing the surrounding normal tissues.3 Although CIRT causes relatively little damage to surrounding normal tissues, once the damage occurs, the normal tissues become sublethally compromised as a result of extensive tissue destruction, and recovery cannot be expected. In our case, the damage affected not only the surrounding tissue but also the rectum. Because sacral chordoma is close to the rectum, it is important for surgeons to anticipate rectal complications after CIRT, and if the rectum is damaged, resection should be considered.2
Reconstruction of a sacral full-thickness defect like that of our patient is challenging.4,5 Three representative flaps have been reported for sacral reconstruction: gluteus maximus flap, transpelvic VRAM flaps, and free flaps; no significant difference in complications between these methods has been reported.6 However, after CIRT, adjacent blood vessels such as the superior and inferior gluteal vessels may be damaged and may not be reliable as pedicles for pedicled flaps or as recipients for free flaps. Miles et al7 advocated the use of bilateral gluteal advancement flaps in patients with no preoperative radiation therapy and intact gluteal vessels; in contrast, in patients with a history of radiation to the sacral area, the use of the transpelvic VRAM flap should be considered. In addition, rectectomy may be required because rectal complications after CIRT may result in intrapelvic dead space. Placement of a pedicled VRAM flap after rectal resection could obliterate sacral defects and intrapelvic dead space. We consider such a flap suitable for reconstruction of a sacral defect after CIRT.
Footnotes
Published online 16 June 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Imai R, Kamada T, Araki N; Working Group for Bone and Soft Tissue Sarcomas Carbon ion radiation therapy for unresectable sacral chordoma: an analysis of 188 cases. Int J Radiat Oncol Biol Phys. 2016;95:322–327. [DOI] [PubMed] [Google Scholar]
- 2.Ukon Y, Outani H, Nagata S, et al. Rectotumoral fistula formation occurring more than 5 years after carbon ion radiotherapy for sacral chordoma: a case report. Mol Clin Oncol. 2019;10:487–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lorenzo C, Andrea P, Barbara V, et al. Surgical spacer placement prior carbon ion radiotherapy (CIRT): an effective feasible strategy to improve the treatment for sacral chordoma. World J Surg Oncol. 2016;14:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manrique OJ, Rajesh A, Asaad M, et al. Surgical outcomes after abdominoperineal resection with sacrectomy and soft tissue reconstruction: lessons learned. J Reconstr Microsurg. 2020;36:64–72. [DOI] [PubMed] [Google Scholar]
- 5.Houdek MT, Bakri K, Tibbo ME, et al. Outcome and complications following vertical rectus abdominis myocutaneous flap surgery to reconstruct sacrectomy defects. Plast Reconstr Surg. 2018;142:1327–1335. [DOI] [PubMed] [Google Scholar]
- 6.Asaad M, Rajesh A, Wahood W, et al. Flap reconstruction for sacrectomy defects: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2020;73:255–268. [DOI] [PubMed] [Google Scholar]
- 7.Miles WK, Chang DW, Kroll SS, et al. Reconstruction of large sacral defects following total sacrectomy. Plast Reconstr Surg. 2000;105:2387–2394. [DOI] [PubMed] [Google Scholar]


