Summary:
Recently, surgical robotic systems have been used to perform microsurgery. Surgical robots have certain properties that make them well suited to microsurgery; for example, they possess 3-dimensional vision, which can be magnified up to 25 times; their movements are up to 5 times more precise than those of surgeons; they possess 7 degrees of wrist articulation; they do not suffer from physiologic tremors; and they can achieve ergonomic surgical positions. The purpose of this study was to report the feasibility of robot-assisted intercostal nerve harvesting in a clinical case. A healthy 57-year-old man suffered a left plexus injury. On diagnosis of clavicular brachial plexus injury, the intercostal nerve transfer to the muscular cutaneous nerve to restore elbow flexion was performed with Da Vinci Xi robot. The harvesting of intercostal nerves using the conventional open approach involves significant surgical exposure, which can lead to perioperative complications. Robot-assisted intercostal nerve harvesting might reduce postoperative pain, shorten patients’ hospital stays, lower complication rates, and produce better quality-of-life outcomes. There are many issues to be solved when performing robotic surgery on peripheral nerves in Japan. However, robot-assisted intercostal nerve harvesting was a feasible surgical procedure, and patient satisfaction was high.
INTRODUCTION
Intercostal nerves are commonly used as donor nerves for brachial plexus reconstruction.1 The intercostal nerves harvesting using conventional open approach involves significant surgical exposure, which can lead to perioperative complications.2 To solve this limitation, a video-assisted intercostal nerve harvesting technique has been reported.3
Recently, surgical robotic systems have been used to perform microsurgery.4–6 Surgical robots have certain properties that make them well suited to microsurgery, for example, they possess 3-dimensional vision, which can be magnified up to 25 times; their movements are up to 5 times more precise than those of surgeons; they possess 7 degrees of wrist articulation; they do not suffer from physiologic tremors; and they can achieve ergonomic surgical positions.7 The possibility of robotic intercostal nerve harvesting has already been demonstrated in a pig model.8 The purpose of this study was to report the feasibility of robot-assisted intercostal nerve harvesting in a clinical case.
CASE PRESENTATION
A healthy 57-year-old man suffered a left plexus injury in a motorcycle accident. In the left upper limb, paralysis of the deltoid, biceps, triceps, and brachioradialis muscles was observed. The wrist joints and fingers were also unable to be moved due to paralysis. Magnetic resonance imaging showed high-intensity changes below the clavicle, and contrast-enhanced computed tomography angiography confirmed that the blood flow through the brachial artery had been disrupted below the clavicle. Based on the above findings, a diagnosis of an infraclavicular brachial plexus injury was made, and a plan to transfer the intercostal nerve to the nerve branch to the biceps of the musculocutaneous nerve to restore elbow flexion was developed.
We presented the patient with 2 options for the intercostal nerve harvesting: open surgery and minimally invasive robot-assisted surgery. Full information regarding the cost and advantages and disadvantages of each method was provided, and the patient’s informed consent was obtained. He chose to undergo minimally invasive robot-assisted surgery. Because this procedure is not covered by the Japanese national health insurance system, it was approved by our university’s ethics committee for medical research (No. 18-096).
The operation was performed 6 months after injury. The patient was placed in the right lateral decubitus position, and the body of the robot was placed in front of the patient (Fig. 1A). A surgical robot system, the Da Vinci Xi (Intuitive Surgical, Inc., Sunnyvale, Calif.), was installed. First, after the left lung had been evacuated, an incision was made along the midline of the axilla, and the fifth intercostal nerve was identified and marked. We then created 3 ports, each 2 cm in diameter, in the left side of the chest (on the ventral side of the anterior axillary line in the seventh intercostal space for the instrument in the left hand, on the middle axillary line in the ninth intercostal space for the camera, and on the dorsal side of the posterior axillary line in the ninth intercostal space for the instrument in the right hand). Next, any adhesion between the visceral pleura and the lung in the intrathoracic cavity was eliminated using a permanent cautery spatula (Intuitive Surgical, Inc.) (Fig. 1B). The previously marked fifth intercostal nerve was identified in the intrathoracic cavity, before being peeled away from the fifth intercostal space in the dorsal to ventral direction using Maryland bipolar forceps (right hand) and fenestrated bipolar forceps (left hand) (Intuitive Surgical, Inc.) (Fig. 2A). Neurolysis was performed on the ventral side, and a sufficient length of the fifth intercostal nerve was collected for the nerve transfer surgery (Fig. 2B) (see Video 1 [online], which summarizes the robot-assisted intercostal nerve harvesting using Da Vinci robot). The absence of sensory feedback is often cited as a fault of surgical robots. However, we had no difficulty with this as reported in previous reports.6
Fig. 1.
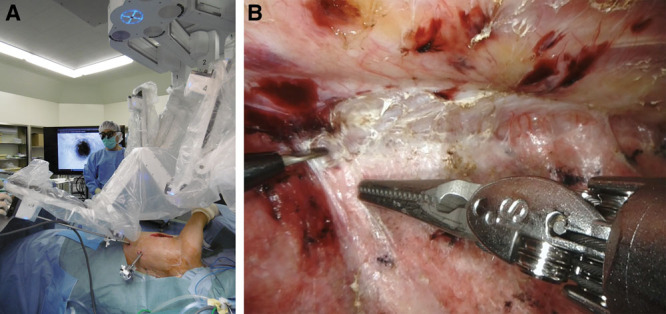
Intraoperative findings. A, The patient was placed in the right lateral decubitus position, and the body of the robot was placed in front of the patient. B, Adhesion between the visceral pleura and the lung in the intrathoracic cavity was eliminated using a permanent cautery spatula.
Fig. 2.
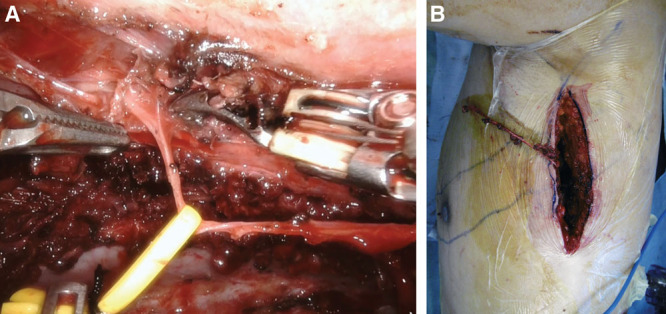
Robot-assisted intercostal nerve harvesting. A, The intercostal nerve was peeled away from the fifth intercostal space in the dorsal to ventral direction using Maryland bipolar forceps (right hand) and fenestrated bipolar forceps (left hand). B, A sufficient length of the fifth intercostal nerve was collected for the nerve transfer surgery.
Video 1. Nerve harvesting summary. Video 1 from “Robot-assisted intercostal nerve harvesting: a technical note about the first case in Japan”.
After the operation, there were no respiratory complications and no pain at the nerve-harvesting site. The patient could walk by himself from the day after the operation.
DISCUSSION
The refinement of open intercostal nerve transfer procedures for restoring elbow flexion after brachial plexus injuries has improved the outcomes.9–11 The disadvantages of the conventional open approach for intercostal nerve harvesting include the relatively long skin incisions required and the risk of pleural damage and wound infections.2,11,12 On the other hand, leaving the periosteum of the ribs intact during dissection of the intercostal nerves is crucial if thoracic cage deformities are to be avoided.12 Therefore, moving from open surgery to less invasive surgery is important for improving patient’s satisfaction. However, thoracoscopic intercostal nerve harvest still presents difficulties because endoscopic instruments are not capable of sufficient fine movement and interfere with surgeon precision.3,8
As with other reported robot-assisted thoracic surgeries, robotic intercostal nerve harvesting might reduce postoperative pain, shorten patients’ hospital stays, lower complications rates, and produce better quality-of-life outcomes.13,14 In fact, in the present case, the postoperative wound pain was mild, and walking was possible from the day after the operation. One of the tasks to solve of robotic surgery is its versatility. The surgical procedure used in the present case requires an operator who is familiar with robot surgery. Although it took about 3 hours to eliminate intrathoracic adhesion, the intercostal nerve was extracted in about an hour. Further education is required before robotic surgery can be widely used in the field of peripheral neurosurgery.
Potential complications associated with robotic intercostal nerve harvesting include pneumothorax, atelectasis due to single-lung ventilation, and iatrogenic intrathoracic injuries. Therefore, this technique requires the presence of a specialized anesthesiologist. However, there is no clinical impact on respiratory function postoperatively.9,15 Another disadvantage of robotics is the cost of acquiring, maintaining, and operating the system. The robotic microsurgery is not covered by the Japanese national health insurance system, so it costs about 3 million yen.
In conclusion, there are many issues to be solved when performing robotic surgery on peripheral nerves in Japan. However, robot-assisted intercostal nerve harvesting is a feasible surgical procedure, and patient satisfaction is high.
ACKNOWLEDGMENT
The study was carried out in accordance with the Declaration of Helsinki and the appropriate ethical framework.
PATIENT CONSENT STATEMENT
The patient provided written consent for the use of his image.
Footnotes
Published online 16 June 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Seddon HJ. Nerve grafting. J Bone Joint Surg Br. 1963;45:447–461. [PubMed] [Google Scholar]
- 2.Kovachevich R, Kircher MF, Wood CM, et al. Complications of intercostal nerve transfer for brachial plexus reconstruction. J Hand Surg Am. 2010;35:1995–2000. [DOI] [PubMed] [Google Scholar]
- 3.Mikami Y, Tajiri Y, Kawano K, et al. Thoracoscope-assisted intercostal nerve transfer. J Jpn Soc Surg Hand. 2008;24:996–999. [Google Scholar]
- 4.Liverneaux P, Nectoux E, Taleb C. The future of robotics in hand surgery. Chir Main. 2009;28:278–285. [DOI] [PubMed] [Google Scholar]
- 5.Mantovani G, Liverneaux P, Garcia JC, Jr, et al. Endoscopic exploration and repair of brachial plexus with telerobotic manipulation: a cadaver trial. J Neurosurg. 2011;115:659–664. [DOI] [PubMed] [Google Scholar]
- 6.Naito K, Facca S, Lequint T, et al. The Oberlin procedure for restoration of elbow flexion with the da Vinci robot: four cases. Plast Reconstr Surg. 2012;129:707–711. [DOI] [PubMed] [Google Scholar]
- 7.Liverneaux P, Berner SH, Bednar MS, et al. Telemicrosurgery: Robotic Assisted Microsurgery. 2013Paris, France: Springer Verlag; [Google Scholar]
- 8.Miyamoto H, Serradori T, Mikami Y, et al. Robotic intercostal nerve harvest: a feasibility study in a pig model. J Neurosurg. 2016;124:264–268. [DOI] [PubMed] [Google Scholar]
- 9.Krakauer JD, Wood MB. Intercostal nerve transfer for brachial plexopathy. J Hand Surg Am. 1994;19:829–835. [DOI] [PubMed] [Google Scholar]
- 10.Nagano A, Ochiai N, Okinaga S. Restoration of elbow flexion in root lesions of brachial plexus injuries. J Hand Surg Am. 1992;17:815–821. [DOI] [PubMed] [Google Scholar]
- 11.Wahegaonkar AL, Doi K, Hattori Y, et al. Technique of intercostal nerve harvest and transfer for various neurotization procedures in brachial plexus injuries. Tech Hand Up Extrem Surg. 2007;11:184–194. [DOI] [PubMed] [Google Scholar]
- 12.Pondaag W, Malessy MJA. Intercostal and pectoral nerve transfers to reinnervate the biceps muscle in obstetric brachial plexus lesions. J Hand Surg Eur. 2014;39:647–652. [DOI] [PubMed] [Google Scholar]
- 13.Balduyck B, Hendriks JM, Lauwers P, et al. Quality of life after anterior mediastinal mass resection: a prospective study comparing open with robotic-assisted thoracoscopic resection. Eur J Cardiothorac Surg. 2011;39:543–548. [DOI] [PubMed] [Google Scholar]
- 14.Louie BE, Farivar AS, Aye RW, et al. Early experience with robotic lung resection results in similar operative outcomes and morbidity when compared with matched video-assisted thoracoscopic surgery cases. Ann Thorac Surg. 2012;93:1598–1604; discussion 1604. [DOI] [PubMed] [Google Scholar]
- 15.Chalidapong P, Sananpanich K, Kraisarin J, et al. Pulmonary and biceps function after intercostal and phrenic nerve transfer for brachial plexus injuries. J Hand Surg Br. 2004;29:8–11. [DOI] [PubMed] [Google Scholar]


