Supplemental Digital Content is available in the text.
Abstract
Background:
Silicone gel implants are regarded as esthetically superior to saline implants, offering a more natural consistency. They are also considered less susceptible to rippling. However, objective measurements and patient-reported outcome studies are lacking. Similarly, minimal data are available quantitating animation deformity.
Methods:
A 3-year prospective study was undertaken among 223 women undergoing primary subpectoral breast augmentation using either saline (n = 145) or silicone gel (n = 78) implants. Photographs obtained included frontal views with the patient flexing the pectoral muscles. Images were matched, and vertical differences in nipple position were measured. Breast implants were evaluated using high-resolution ultrasound to detect any ripples or folds at least 3 months after surgery. Outcome surveys were administered. Statistical analysis included the χ2 test, point-biserial correlations, and a power analysis.
Results:
Respondents reported visible rippling in 18% of women and palpable rippling in 32% of patients, with no significant difference between women treated with saline and silicone gel implants. Ripples were detected on ultrasound scans in 24% of women with saline implants and in 27% of women with silicone gel implants (difference not significant). Ripples were more common in women with lower body mass indices. Fifty percent of patients demonstrated nipple displacement <1 cm on animation. Nipple displacement occurred either up or down with equal frequency and a mean overall nipple displacement of zero.
Conclusions:
Saline and silicone breast implants produce similar degrees of rippling, as determined on outcome surveys and ultrasound examination. Animation deformities tend to be minor and well-tolerated.
INTRODUCTION
Both saline and silicone gel implants are widely used by plastic surgeons today in the United States, although silicone gel implants are favored.1 In discussing the pros and cons of each implant style, plastic surgeons, including the author, have routinely advised patients that silicone gel implants feel more natural and are less prone to rippling. However, this claim has little scientific foundation. Few objective studies examine differences between saline and silicone implants.2 Similarly, there is a paucity of patient-reported data comparing outcomes.
High-resolution ultrasound is quickly becoming a popular tool in plastic surgery offices.3 This technology allows point-of-care evaluation of breast implants and is accurate in detecting ripples, folds, and other abnormalities. Animation deformity is a well-known complication of subpectoral implants.4,5 This problem was also evaluated using measurements of nipple displacement on matched photographs.
This study was undertaken to obtain objective data comparing saline and silicone gel implants. This information may be used by surgeons and patients when selecting an implant.
PATIENTS AND METHODS
This prospective study began in December 2016 and ended in December 2019. Institutional review board approval was obtained from Chesapeake IRB, now Advarra IRB (Columbia, Md.) before initiation of the study.
Patients
All women undergoing primary cosmetic breast augmentation were asked to take part in the study. Unilateral procedures, mastopexies, breast reconstruction patients, and transgender patients were excluded.
Surgery
All procedures were performed by the author at the Surgery Center of Leawood, Kansas. Total intravenous anesthesia was administered, using a propofol infusion and a laryngeal mask airway. As part of deep venous thrombosis prophylaxis, patients were scanned with Doppler ultrasound before surgery, the day after surgery, and approximately 1 week after surgery.3,6
All implants were placed subpectorally, with preservation of the inframammary ligaments. All implants were manufactured by Mentor (Mentor Corp., Irvine, Calif.). A supra-inframammary incision (<1 cm above the existing inframammary crease) was used in most patients, although occasionally the incision was located more inferiorly (eg, in patients with constricted breasts).7 The pectoralis muscle was released inferiorly and along the inferior sternal border.7,8 Saline implants were inflated to their labeled maximum fill volume.
Clinical and Photographic Evaluation
Clinical, photographic, and ultrasound evaluations were performed on the same day, at least 3 months after surgery. Any visible rippling was noted (Fig. 1). A ruler was included in one of the photographs for calibration. To detect animation deformity, a second frontal photograph was taken, with the patient holding her hands together and flexing her pectoral muscles (Fig. 2). Photographic matching was facilitated by the Canfield 7.4.1 Mirror Imaging software (Canfield Scientific, Fairfield, N.J.).
Fig. 1.
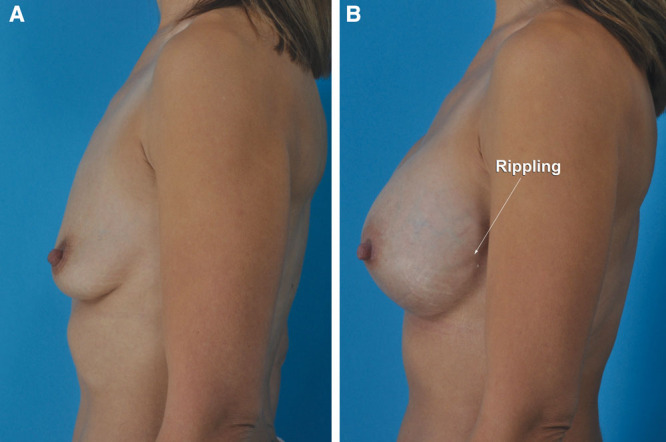
This 41-year-old woman is shown before (A) and 3 months after (B) a subpectoral breast augmentation using Mentor 475 ml smooth, round Moderate Plus Profile MemoryGel implants. Rippling can be seen on the left lateral photograph (B). The patient was unaware of it.
Fig. 2.
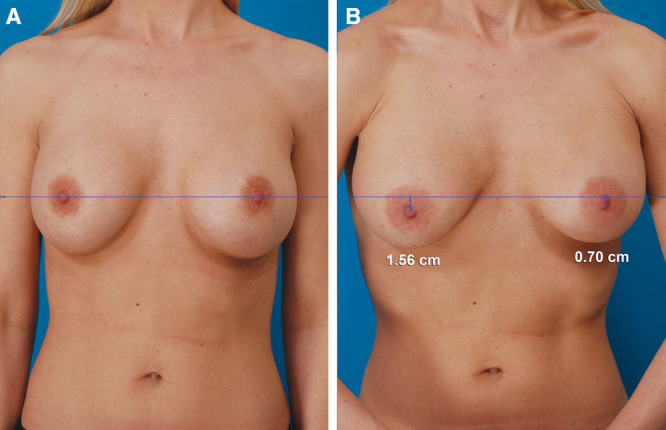
This 29-year-old woman is shown 3 years after a subpectoral breast augmentation using Mentor smooth, round Moderate Plus Profile saline implants inflated to 390 ml per side. Resting (A) and exertional (B) photographs were matched for size and orientation using the Canfield Mirror 7.4.1 Imaging software (Canfield Scientific, Fairfield, N.J.). A horizontal plane was drawn at the level of the resting postoperative nipple position. Right and left postoperative nipple levels while flexing the pectoral muscles were compared using vertical measurements. On flexion of her pectoralis muscles, the nipples displace downward.
Surveys
Surveys were administered by the office staff, usually the sonographer, at least 3 months after surgery. (See survey, Supplemental Digital Content 1, which displays the breast implant survey, http://links.lww.com/PRSGO/B406.) All surveys were administered in person.
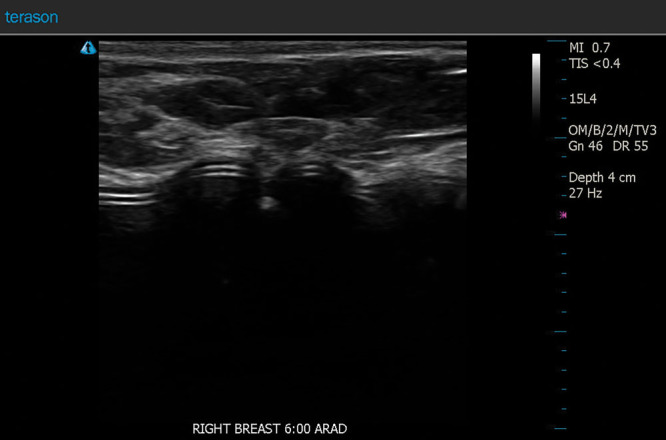
Ultrasound Scans
Ultrasound scans were all performed by the same licensed sonographer using a Terason t3200 Ultrasound System Vascular series (Terason Ultrasound, Burlington, Mass.) (Fig. 3).
Fig. 3.
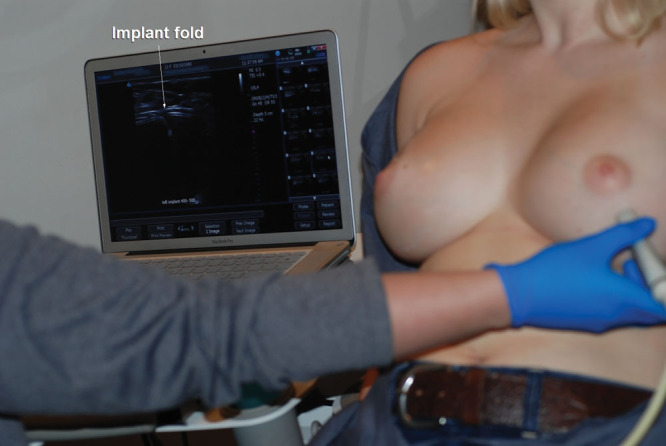
This 22-year-old woman is undergoing an ultrasound scan of the breasts 6 months after a primary subpectoral breast augmentation using smooth, round Mentor Moderate Plus Profile saline implants inflated to 450 ml. A fold is visible in the left implant.
Statistical Analysis
Statistical analyses were performed using SPSS for Mac version 26.0 (SPSS, Inc., Chicago, Ill.). The χ2 test of independence was used to compare dichotomous variables. Point-biserial correlations were computed between dichotomous and continuous variables. An independent t test was used to compare means. A P value <0.05 was considered significant. An a priori power analysis was performed. To achieve 80% power, with an α level of 0.05, sufficient to detect a medium-sized treatment difference (ϕ = 0.30),9 88 subjects would be needed.10
RESULTS
Over the 3-year study period, 223 women underwent primary cosmetic breast augmentation. The mean patient age was 31 years (range, 18–62 years), and the mean follow-up time was 4.6 months (range, 1 day to 3 years). The mean implant volume was 426 ml (range, 250–800 ml). Saline implants were inserted in 65% of patients; silicone gel implants were used in 35% of patients. There were no significant differences in demographic data comparing patients treated with saline and silicone gel implants (Table 1).
Table 1.
Patient Data
| Characteristic | Saline* | Silicone† | Total, % |
|---|---|---|---|
| No. patients | 145 | 78 | 223 |
| Age, y | |||
| Mean | 31.1 | 31.9 | 31.4 |
| Range | 18.2–57.9 | 22.1–61.8 | 18.2–61.8 |
| Follow-up time, mo | |||
| Mean | 4.5 | 4.6 | 4.6 |
| Range | 0.03–36.0 | 0.03–36.0 | 0.03–36.0 |
| Smoking status | |||
| Nonsmoker | 111 | 62 | 173 (77.6) |
| Smoker | 34 | 16 | 50 (22.4) |
| Body mass index, kg/m2 | |||
| Mean | 22.7 | 22.1 | 22.5 |
| Range | 16.3–35.4 | 16.5–38.4 | 16.3–38.4 |
| Right implant volume, ml | |||
| Mean | 424 | 430 | 426 |
| Range | 270–800 | 275–800 | 270–800 |
| Left implant volume, ml | |||
| Mean | 424 | 430 | 426 |
| Range | 250–800 | 275–800 | 250–800 |
| In combination with other procedures | |||
| No | 130 | 68 | 198 (88.8) |
| Yes | 15 | 10 | 25 (11.2) |
*Mentor Style 2000 smooth, round, Moderate Plus Profile saline implant.
†Mentor Style 1000 Moderate Plus Profile Gel (n = 74); Mentor Style 4000 High Profile Gel (n = 4).
Complications
No systemic complications were encountered. No deep venous thromboses were detected. Five patients had visible rippling that could be seen on photographs (Fig. 1). Four patients had animation deformities as determined by their surgeon. No patients were concerned about it or requested surgical correction. Three patients developed capsular contractures and were treated with open capsulotomies. One patient elected to have larger implants inserted simultaneously. There were no other reoperations for a size change. No significant differences were detected comparing complication and reoperation rates for the 2 patient groups (Table 2).
Table 2.
Complications and Reoperations
| Saline, % | Silicone, % | Total, % | |
|---|---|---|---|
| Complications | |||
| No | 129 (89.0) | 69 (88.5) | 198 (88.8) |
| Yes | 16 (11.0) | 9 (11.5) | 25 (11.2) |
| Rippling | 3 | 2 | 5 |
| Animation deformity | 2 | 2 | 4 |
| Hematoma | 3 | 1 | 4 |
| Capsular contracture | 2 | 1 | 3 |
| Asymmetry | 1 | 2 | 3 |
| Hypertrophic scar | 2 | 1 | 3 |
| Implant deflation | 2 | 0 | 2 |
| Cellulitis | 1 | 0 | 1 |
| Seroma | 0 | 0 | 0 |
| Symmastia | 0 | 0 | 0 |
| Delayed wound healing | 0 | 0 | 0 |
| Deep venous thrombosis | 0 | 0 | 0 |
| Total | 16 | 9 | 25 |
| Reoperations (total intravenous anesthesia) | |||
| Evacuation of hematoma | 2 | 2 | 4 |
| Replacement of deflated implant | 2 | 0 | 2 |
| Open capsulotomy | 1 | 1 | 2 |
| Open capsulotomy and implant replacement with larger size* | 1 | 0 | 1 |
| Implant reposition for symmetry | 0 | 1 | 1 |
| Revisions (local anesthesia) | |||
| Scar revision | 2 | 1 | 3 |
| Total | 8 | 5 | 13 (5.8) |
*One patient had both implants replaced at the time of a right open capsulotomy for capsular contracture.
Photometric Findings
In 50% of the patients, pectoralis flexion produced <1 cm of nipple displacement bilaterally, with no significant difference observed between implant styles. In women who demonstrated nipple displacement >1 cm on animation, the nipple movement was equally divided between moving up (51%) and moving down (49%). The mean nipple displacement was zero (mean, down 0.02 cm; range, down 3.96 cm to up 3.40 cm). There were no cases of the nipple moving up on one side and down on the other.
Survey Results
One hundred seventy-one patients completed the surveys (inclusion rate, 76.7%). The proportion of surveyed women with saline (61%) and silicone gel (39%) implants was similar to the total patient population (Table 3). Overall, 18% of women reported visible rippling (wrinkling) and 32% of women reported palpable rippling. Patients who reported rippling had significantly lower body mass indices (P <0.05) and lower implant volumes (P < 0.05), on average, than the respondents who did not report rippling.
Table 3.
Survey Data
| Characteristic | Saline, % | Silicone, % | Total, % |
|---|---|---|---|
| No. surveys | 105 (61.4) | 66 (38.6) | 171 |
| Age, y | |||
| Mean | 30.3 | 32.0 | 31.0 |
| Range | 18.2–35.9 | 22.1–60.8 | 18.2–60.8 |
| Follow-up time, mo | |||
| Mean | 6.0 | 6.2 | 6.1 |
| Range | 3.0–36.0 | 3.0–36.0 | 3.0–36.0 |
| Visible rippling | |||
| No | 82 (78.1) | 58 (87.9) | 140 (81.2) |
| Yes | 23 (21.9) | 8 (12.1) | 31 (18.1) |
| Palpable rippling | |||
| No | 66 (62.9) | 50 (75.8) | 116 (67.8) |
| Yes | 39 (37.1) | 16 (24.2) | 55 (32.2) |
| Does wrinkling bother you? | |||
| No | 19 (18.1) | 10 (15.2) | 29 (17.0) |
| Yes | 11 (10.5) | 5 (7.6) | 16 (9.4) |
| A little | 11 (10.5) | 2 (3.0) | 13 (7.6) |
| No wrinkling | 64 (60.9) | 49 (74.2) | 113 (66.0) |
| Breast firmness | |||
| Just right | 92 (87.6) | 57 (86.4) | 149 (87.1) |
| Too firm | 9 (8.6) | 5 (7.5) | 14 (8.2) |
| Too soft | 4 (3.8) | 4 (6.1) | 8 (4.7) |
| Look natural? | |||
| No | 2 (1.9) | 2 (3.0) | 4 (2.3) |
| Yes | 98 (93.3) | 60 (90.9) | 158 (92.4) |
| No, but I wanted fake | 5 (4.8) | 4 (6.1) | 9 (5.3) |
| Size | |||
| Just right | 76 (72.4) | 49 (74.2) | 125 (73.1) |
| Prefer larger | 27 (25.7) | 16 (24.2) | 43 (25.1) |
| Prefer smaller | 2 (1.9) | 1 (1.5) | 3 (1.8) |
| Scars well hidden | |||
| No | 6 (5.7) | 7 (10.6) | 13 (7.6) |
| Yes | 99 (94.3) | 59 (89.4) | 158 (92.4) |
| Implants at right level | |||
| Yes | 94 (89.5) | 56 (84.8) | 150 (87.7) |
| Too high | 3 (2.9) | 7 (10.6) | 10 (5.8) |
| Too low | 8 (7.6) | 3 (4.5) | 11 (6.4) |
| Deflation or known leak | |||
| No | 105 (100.0) | 66 (100.0) | 171 (100.0) |
| Yes | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Would you do it again? | |||
| No | 1 (1.0) | 1 (1.5) | 2 (1.2) |
| Yes | 104 (99.0) | 65 (98.5) | 169 (98.8) |
| Choose same implants? | |||
| No (silicone instead) | 12 (11.4) | 0 (0.0) | 12 (7.0) |
| Yes | 93 (88.6) | 66 (100.0) | 159 (93.0) |
| Result rating (1–10)* | |||
| Mean | 9.3 | 9.3 | 9.3 |
| Median | 10 | 10 | 10 |
| Range | 6–10 | 6–10 | 6–10 |
*Patients were asked to rate their result on a scale of 1 (worst) to 10 (best).
Eighty-seven percent of respondents said that their firmness was “just right,” 8% found their breasts too firm, and 5% found them too soft. Most women (73%) rated their postoperative size “just right.” Twenty-five percent of patients would have preferred a larger size, and 2% of women would have preferred smaller breasts. There were no significant differences comparing saline and silicone gel devices.
Ultrasound Evaluation
One hundred forty-eight women underwent ultrasound scans (66.4%). Ripples were defined as a wrinkle in the anterior implant surface (Fig. 4). Ripples along the inferior margin, which were present in the majority of women, were not counted. A fold represented a deeper crease with shell-touching-shell (Fig. 5). Ripples were detected in 37 women, including 24% of patients with saline implants and 27% of women with silicone gel implants (Table 4). In 30 women, the ripples were found bilaterally (81%). Folds were detected in 10% of women with saline implants and 7% of women with silicone gel implants and were bilateral in 2 cases. There was no significant difference in the incidence of ripples or folds comparing saline and silicone gel devices. No implant leaks or ruptures were detected.
Fig. 4.
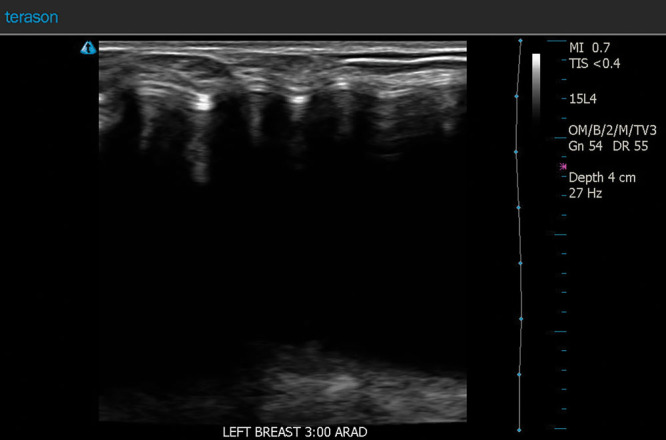
This 31-year-old woman underwent primary subpectoral breast augmentation using 425 ml Mentor MemoryGel silicone gel implants. Her sonogram 3 months after surgery showed rippling of the left breast implant.
Fig. 5.
This 52-year-old woman underwent primary subpectoral breast augmentation using Mentor smooth, round Moderate Plus Profile saline implants filled to their maximum capacity of 360 ml. Her sonogram, performed 3 months after surgery, shows a fold in the right breast implant.
Table 4.
Ultrasound Findings
| Characteristic | Saline, % | Silicone, % | Total, % |
|---|---|---|---|
| No. scans | 88 | 60 | 148 |
| Rippling | |||
| No | 67 (76.1) | 44 (73.3) | 111 (75.0) |
| Yes | 21 (23.9) | 16 (26.7) | 37 (25.0) |
| Folds | |||
| No | 79 (89.8) | 56 (93.3) | 135 (91.2) |
| Yes | 9 (10.2) | 4 (6.7) | 13 (8.8) |
The mean body mass index for women who had rippling and folds was significantly lower (P < 0.05) on average (21.3 versus 22.8 kg/m2) than women without rippling/folds. There was no significant correlation between rippling and either follow-up time or patient age. Rippling and folds were significantly correlated (P < 0.05) with lower mean implant volumes (397 versus 435 ml for patients without ripples).
DISCUSSION
Among surveyed members of the American Society of Plastic Surgeons, 82% of respondents prefer silicone gel implants and 22% use silicone implants exclusively.1 Silicone gel implants are believed to offer a more natural consistency and possibly less rippling than saline implants.2,11–14 The author has counseled women for years that silicone gel implants offer these esthetic advantages and the likelihood of reoperation for rupture is lower because gel implants do not deflate. Of course, saline is completely absorbed in the event of a leak. These considerations are weighed against the disadvantages of silicone gel—greater cost and the fact that rupture is unlikely to be detected without imaging studies.
Handel et al13 compared textured gel implants with textured saline implants, finding an advantage for textured gel implants. Textured saline implants are known to be susceptible to rippling.13–15 Textured surfaces may affect the palpability of breast implant shells.16 Tissue adherence to the implant may increase the rippling risk.17 Handel et al13 did not compare smooth gel and smooth saline implants. This comparison takes on new importance as most US surgeons now prefer smooth devices1 because of the link between texturing and breast implant–associated anaplastic large-cell lymphoma (BIA-ALCL).18
Although it is considered a complication, rippling results from normal deformation of a breast implant when it is positioned in the flat, upright, or lateral position.17 Subpectoral implant placement is a well-known method to maximize soft tissue cover.17 Suboptimal implant filling increases the risk of rippling.17 Consequently, most plastic surgeons fill saline implants to the maximum recommended fill volume. “Gel fill” refers to the amount of silicone gel placed within a given shell size.16 Allergan Natrelle Inspira implants (Allergan plc, Dublin, Ireland) have a high gel fill ratio.16 However, clinical data substantiating any clinical advantages are lacking.16
Gel implants that feature greater cohesivity (ie, more silicone cross-linking)16 are believed to cause less rippling, at the expense of greater implant firmness.16,17 Surprisingly, rippling and folds occur even in the presence of the most cohesive “form stable” implant styles.17,19,20
More cohesive gel implants are designed to minimize gel bleed.17 With increased cohesiveness to reduce gel bleed and (possibly) reduce rippling, the advantage of a more natural consistency using silicone gel may be lost.8,21 A saline implant is softer and feels more natural than an overly firm silicone gel implant. Similar to the findings of an earlier outcome study,21 survey results show that excessive firmness is more likely to be an issue for women (8.2%) than excessive softness (4.7%).
Rippling rates increase over time.22 In a large retrospective study, Codner et al23 reported a rippling rate of 7.1%, with no significant difference in rippling rates comparing saline (482 patients) and silicone gel (330 patients) implants. However, in a subgroup comparison of underweight patients (body mass index <18.5 kg/m2) treated with subglandular implants, an association was found between rippling and saline implants (P = 0.045). Similar to the present study, the risk of rippling decreased with greater body mass indices. Saline implant deflation occurred in 2.7% of patients reported by Codner et al.23 Only 2 saline implant deflations occurred in the present study (0.9%). However, the follow-up times were short, all <3 years. In a 10-year clinical study by the author,24 with a large number of patients implanted with saline devices (490 patients), 4 patients returned with deflations (0.8%).
Walker et al25 mailed questionnaires to patients with Allergan Natrelle saline implants. The authors reported wrinkling in 13.7% of patients and implant palpability/visibility in 12.1% of patients. The authors compared these figures with data (1.2% and 1.6%, respectively) for women treated with Inamed (now Allergan) silicone gel implants,26 finding an advantage for silicone implants in terms of “look and feel.” However, 69.5% of the saline implants were textured versus 41.0% of the silicone gel implants. Moreover, the authors compared patient-reported survey responses with surgeon-reported data from a separate study. To the author’s knowledge, there is no published “apples to apples” comparison of rippling rates and patient-reported outcomes between women implanted with subpectoral smooth saline implants and smooth silicone gel devices.8
Plastic surgeons are well aware that most women, when holding both implants in their hands in the office, prefer silicone gel. However, in vivo, especially in a subpectoral pocket, this difference may be more difficult to discern, particularly in a woman who has a moderate breast volume already.8 Saline implants do have a number of advantages compared with silicone gel.27 The incision is shorter.2 A rupture is clinically obvious, and the leaked saline poses no health risk.23,27 By contrast, detection of a silicone gel implant rupture often requires (expensive) magnetic resonance imaging or a high-resolution ultrasound examination.3,27 Even these studies are not always reliable.2,28 The absence of silicone gel makes silicone bleed a non-issue, whether or not such leakage is implicated in systemic disease. There are few reliable data regarding capsular contracture rates,29,30 although some authors report an advantage for saline implants.27 Saline implants are also much less expensive than silicone gel.27 A recent study found greater cost-effectiveness for saline implants used in breast reconstruction.31
The advantages of saline as a filler at the time of redo surgery are seldom discussed in the literature.8,27,32 This is a highly relevant issue, as 10-year core studies find that between 29.7% and 36.5% of women return for redo surgery.27,33,34 A capsular contracture is more easily treated in the presence of a saline implant, by open capsulotomy.32 There is usually no need for a capsulectomy, site change, or implant exchange (or acellular dermal matrix), making the revision surgery much less expensive and easier for patients.32 A thin capsule around a saline implant is gradually absorbed after explantation.35,36 By contrast, capsules around silicone gel implants are exposed to silicone bleed, which can increase inflammation within the capsule36 and increase the risk of capsular contracture.32,37,38 Silicone granulomas may develop.39,40 Capsules can become thickened and calcified39–41 and are unlikely to be absorbed.41,42 A capsulectomy may be indicated,39 with its attendant morbidity39 and additional cost both for surgery and pathologic examination of the capsule. A more innocuous effect on the capsule around a saline implant is an underappreciated advantage of these devices.43
Both BIA-ALCL and Breast Implant Illness have heightened the awareness of possible immunologic effects of foreign bodies.43–46 A particle theory for BIA-ALCL is gaining recognition.43,44 Silicone shedding from the surface is eliminated by choosing smooth implants. Silicone bleed through the elastomer shell is eliminated with saline implants, making smooth saline implants a reasonable choice.
Patient satisfaction is the major determinant of success in cosmetic surgery.47 Patient satisfaction rates are >86% for both saline and silicone gel implants.21,25,27,48–50 The implants look the same in patients.11 However, silicone gel implants are much more profitable for breast implant companies and are more heavily promoted.8 Sientra Inc. (Santa Barbara, Calif.) does not even manufacture saline implants.8
Survey responses were notable for breast size assessments. Despite an average implant volume of 426 ml, 25% of women would have preferred a larger size. Only 2% of respondents would have preferred a smaller size. A preference for a larger size was also found in a previous outcome study,21 challenging the conventional wisdom to be conservative in implant sizing. A significant correlation between larger implant volumes and patient satisfaction has been documented.21,51
The surveys found a higher rate of rippling among women treated with saline implants, but the difference was not significant. One must consider that women with saline implants are already advised that they have a higher risk of rippling, so there may be a degree of bias in their assessments. This prejudice is less likely to affect ultrasound examinations. It makes sense that leaner women, with less subcutaneous fat, are more likely to have rippling, reflected in both survey responses and ultrasound findings.
Despite the similar findings regarding rippling, there may be less tangible advantages of silicone gel implants. Although the difference has not been quantitated, women who have had both types of implants frequently report a more natural consistency for silicone gel implants (in the absence of a capsular contracture or highly cohesive gel). In the event of a leak, there is likely to be no change in shape and size, and no unexpected and inconvenient return to the surgeon for implant replacement. Most women with some degree of silicone bleed are asymptomatic and unaware of it. The clinical importance of a small undetected intracapsular silicone bleed remains unknown.43
In performing the outcome study, an ad hoc survey was chosen.7 Although more comprehensive surveys exist, they are of limited value when comparing specific surgical parameters of interest. Succinct questions contained on a single page (see survey, Supplemental Digital Content 1, which displays the breast implant survey, http://links.lww.com/PRSGO/B406) lend themselves to high patient compliance and ease of data interpretation and comparison with previous studies.7,21 When surveys are done in person by an interviewer, patients are more likely to take greater interest and answer all of the questions.7,21
Most classifications of animation deformity are limited by subjectivity.52–54 Quantitating nipple movement requires exact matching of standardized images, facilitated by imaging software. Spear et al4 reported that distortion of the breast during pectoralis muscle contraction is common (77.5% of women) after a subpectoral breast augmentation but is rarely severe. These surgeons released the inferior attachments of the pectoralis along the inframammary fold but left the sternal fibers intact.4 Kim et al5 recently evaluated nipple movement and area of skin contour irregularity in subpectoral tissue expander/implant-based breast reconstructions. Animation deformity tends to be more common (100% in one study54) and more severe in breasts reconstructed with subpectoral implants because of the loss of the glandular tissue covering the implants and closer approximation of the pectoralis muscle to the skin.55 In the present study, none of the patients complained about animation deformity, including fitness enthusiasts. The author prefers to release the muscle very cautiously (to avoid symmastia) from its origin along the lower sternal border, in addition to its inferior origin along the inframammary fold.7,8 This maneuver allows the muscle to retract superiorly,4 reducing muscle tension over the implant. A surprising finding was that nipple movement was not predominantly upward as expected, but equally as often downward. In patients with >1 cm of nipple displacement, there was no overall net movement in either direction. It is possible that the additional muscle release creates a more balanced effect on nipple level during pectoralis contraction.
Limitations of the Study
This study is limited to smooth saline implants and minimally cohesive smooth silicone gel implants implanted subpectorally. The maximum follow-up time was 3 years. It is likely that some patients will go on to develop rippling in the future.22 A minimum 3-month time period was chosen because breast swelling has largely resolved at this time.56 Longer follow-up times are generally preferred but come at the cost of a reduced inclusion rate.56,57 Higher inclusion rates (ie, fewer patients lost to follow-up) reduce sampling bias.4,58
Strengths of the Study
This comparative prospective level II study includes objective measurements on matched photographs, a reliable technology (ultrasound) for detection of implant ripples and folds, and inclusion of all-important patient-reported outcomes. Because the author performed the operations using the same method in the same facility, over the same time period, confounders are avoided. The author has no financial conflicts with breast implant manufacturers.
CONCLUSIONS
Outcome surveys and ultrasound scans show that rippling rates are similar when comparing saline and silicone gel implants. Animation deformities tend to be minor and well-tolerated.
Patients need to be properly informed of the pros and cons so that they can participate in the decision-making process. Plastic surgeons should be prepared to insert either device, in accordance with the patient’s preference.
ACKNOWLEDGMENTS
The author thanks Christina Staab, RT, for data collection and sonograms and Jane Zagorski, PhD, for statistical analyses.
Supplementary Material
Footnotes
Published online 4 June 2020.
Disclosure: Dr. Swanson receives royalties from Springer Nature (Cham, Switzerland).
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Hidalgo DA, Sinno S. Current trends and controversies in breast augmentation. Plast Reconstr Surg. 2016;137:1142–1150. [DOI] [PubMed] [Google Scholar]
- 2.Chang EI, Hammond DC. Clinical results on innovation in breast implant design. Plast Reconstr Surg. 2018;1424S The Science of Breast Implants31S–38S. [DOI] [PubMed] [Google Scholar]
- 3.Swanson E. The expanding role of diagnostic ultrasound in plastic surgery. Plast Reconstr Surg Glob Open. 2018;6:e1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spear SL, Schwartz J, Dayan JH, et al. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg. 2009;33:44–48. [DOI] [PubMed] [Google Scholar]
- 5.Kim JYS, Qiu CS, Chiu WK, et al. A quantitative analysis of animation deformity in prosthetic breast reconstruction. Plast Reconstr Surg. 2019;144:291–301. [DOI] [PubMed] [Google Scholar]
- 6.Swanson E. Prospective study of Doppler ultrasound surveillance for deep venous thromboses in 1000 plastic surgery outpatients. Plast Reconstr Surg. 2020;145:85–96. [DOI] [PubMed] [Google Scholar]
- 7.Swanson E. The supra-inframammary fold approach to breast augmentation: avoiding a double bubble. Plast Reconstr Surg Glob Open. 2017;5:e1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swanson E. Breast augmentation. In: Evidence-based Cosmetic Breast Surgery. 2017:Cham, Switzerland: Springer; 33–74. [Google Scholar]
- 9.Faul F, Erdfelder E, Lang AG, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. [DOI] [PubMed] [Google Scholar]
- 10.Cohen J. Analysis of variance. In: Statistical Power Analysis for the Behavioral Sciences. 1988:2nd ed Hillsdale, N.J.: Lawrence Erlbaum; 273–406. [Google Scholar]
- 11.Hidalgo DA, Spector JA. Breast augmentation. Plast Reconstr Surg. 2014;133:567e–583e. [DOI] [PubMed] [Google Scholar]
- 12.Spring MA, Macias LH, Nadeau M, et al. Secondary augmentation-mastopexy: indications, preferred practices, and the treatment of complications. Aesthet Surg J. 2014;34:1018–1040. [DOI] [PubMed] [Google Scholar]
- 13.Handel N, Jensen JA, Black Q, et al. The fate of breast implants: a critical analysis of complications and outcomes. Plast Reconstr Surg. 1995;96:1521–1533. [DOI] [PubMed] [Google Scholar]
- 14.Handel N, Cordray T, Gutierrez J, et al. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. 2006;117:757–767; discussion 768. [DOI] [PubMed] [Google Scholar]
- 15.Hall-Findlay EJ. Breast implant complication review: double capsules and late seromas. Plast Reconstr Surg. 2011;127:56–66. [DOI] [PubMed] [Google Scholar]
- 16.Mohebali K, Wixtrom RN. Breast implant engineering and performance. Plast Reconstr Surg. 2018;1424S The Science of Breast Implants6S–11S. [DOI] [PubMed] [Google Scholar]
- 17.Nahabedian MY. Round form-stable breast implants: diagnosis and management of complications. Plast Reconstr Surg. 2019;144:73S–81S. [DOI] [PubMed] [Google Scholar]
- 18.Brody GS, Deapen D, Taylor CR, et al. Anaplastic large cell lymphoma occurring in women with breast implants: analysis of 173 cases. Plast Reconstr Surg. 2015;135:695–705. [DOI] [PubMed] [Google Scholar]
- 19.Weum S, de Weerd L, Kristiansen B. Form stability of the Style 410 anatomically shaped cohesive silicone gel-filled breast implant in subglandular breast augmentation evaluated with magnetic resonance imaging. Plast Reconstr Surg. 2011;127:409–413. [DOI] [PubMed] [Google Scholar]
- 20.Hammond DC. Discussion. Form stability of the style 410 anatomically shaped cohesive silicone gel-filled breast implant in subglandular breast augmentation evaluated with magnetic resonance imaging. Plast Reconstr Surg. 2011;127:414–416. [DOI] [PubMed] [Google Scholar]
- 21.Swanson E. Prospective outcome study of 225 cases of breast augmentation. Plast Reconstr Surg. 2013;131:1158–1166; discussion 1167–1168. [DOI] [PubMed] [Google Scholar]
- 22.Derby BM, Codner MA. Textured silicone breast implant use in primary augmentation: core data update and review. Plast Reconstr Surg. 2015;135:113–124. [DOI] [PubMed] [Google Scholar]
- 23.Codner MA, Mejia JD, Locke MB, et al. A 15-year experience with primary breast augmentation. Plast Reconstr Surg. 2011;127:1300–1310. [DOI] [PubMed] [Google Scholar]
- 24.Swanson E. Prospective comparative clinical evaluation of 784 consecutive cases of breast augmentation and vertical mammaplasty, performed individually and in combination. Plast Reconstr Surg. 2013;132:30e–45e; discussion 46e–47e. [DOI] [PubMed] [Google Scholar]
- 25.Walker PS, Walls B, Murphy DK. Natrelle saline-filled breast implants: a prospective 10-year study. Aesthet Surg J. 2008;28:19–25. [DOI] [PubMed] [Google Scholar]
- 26.Spear SL, Murphy DK, Slicton A, et al. ; Inamed Silicone Breast Implant U.S. Study Group Inamed silicone breast implant core study results at 6 years. Plast Reconstr Surg. 2007;1207 Suppl 18S–16S; discussion 17S. [DOI] [PubMed] [Google Scholar]
- 27.Rohrich RJ, Reece EM. Breast augmentation today: saline versus silicone—what are the facts? Plast Reconstr Surg. 2008;121:669–672. [DOI] [PubMed] [Google Scholar]
- 28.Collis N, Litherland J, Enion D, et al. Magnetic resonance imaging and explantation investigation of long-term silicone gel implant integrity. Plast Reconstr Surg. 2007;120:1401–1406. [DOI] [PubMed] [Google Scholar]
- 29.Wan D, Rohrich RJ. Revisiting the management of capsular contracture in breast augmentation: a systematic review. Plast Reconstr Surg. 2016;137:826–841. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz MR. Evidence-based medicine: breast augmentation. Plast Reconstr Surg. 2017;140:109e–119e. [DOI] [PubMed] [Google Scholar]
- 31.Siotos C, Sarmiento S, McColl M, et al. Cost-effectiveness analysis of silicone versus saline implant-based breast reconstruction using the BREAST-Q. Plast Reconstr Surg. 2019;143:276e–284e. [DOI] [PubMed] [Google Scholar]
- 32.Swanson E. Open capsulotomy: an effective but overlooked treatment for capsular contracture after breast augmentation. Plast Reconstr Surg Glob Open. 2016;4:e1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spear SL, Murphy DK; Allergan Silicone Breast Implant U.S. Core Clinical Study Group Natrelle round silicone breast implants: core study results at 10 years. Plast Reconstr Surg. 2014;133:1354–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maxwell GP, Van Natta BW, Bengtson BP, et al. Ten-year results from the Natrelle 410 anatomical form-stable silicone breast implant core study. Aesthet Surg J. 2015;35:145–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Friedman HI, Friedman AC, Carson K. The fate of the fibrous capsule after saline implant removal. Ann Plast Surg. 2001;46:215–221. [DOI] [PubMed] [Google Scholar]
- 36.Thomsen JL, Christensen L, Nielsen M, et al. Histologic changes and silicone concentrations in human breast tissue surrounding silicone breast prostheses. Plast Reconstr Surg. 1990;85:38–41. [DOI] [PubMed] [Google Scholar]
- 37.Caffee HH. The influence of silicone bleed on capsule contracture. Ann Plast Surg. 1986;17:284–287. [DOI] [PubMed] [Google Scholar]
- 38.Moyer HR, Ghazi BH, Losken A. The effect of silicone gel bleed on capsular contracture: a generational study. Plast Reconstr Surg. 2012;130:793–800. [DOI] [PubMed] [Google Scholar]
- 39.Young VL. Guidelines and indications for breast implant capsulectomy. Plast Reconstr Surg. 1998;102:884–891; discussion 892,893–894. [PubMed] [Google Scholar]
- 40.Copeland M, Choi M, Bleiweiss IJ. Silicone breakdown and capsular synovial metaplasia in textured-wall saline breast prostheses. Plast Reconstr Surg. 1994;94:628–633; discussion 634. [PubMed] [Google Scholar]
- 41.Hardt NS, Yu L, LaTorre G, et al. Complications related to retained breast implant capsules. Plast Reconstr Surg. 1995;95:364–371. [DOI] [PubMed] [Google Scholar]
- 42.Rockwell WB, Casey HD, Cheng CA. Breast capsule persistence after breast implant removal. Plast Reconstr Surg. 1998;101:1085–1088. [DOI] [PubMed] [Google Scholar]
- 43.Swanson E. Evaluating the necessity of capsulectomy in cases of textured breast implant replacement. Ann Plast Surg. February 25, 2020. [E-pub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 44.Hammond D. The potential role of particulates in the etiology of ALCL. October 6, 2019. Paper presented at 1st World Consensus Conference on BIA-ALCL Rome, Italy: Available at https://www.youtube.com/watch?v=YxPFayQsjUo&t=14536s. Accessed December 10, 2019 [Google Scholar]
- 45.Webb LH, Aime VL, Do A, et al. Textured breast implants: a closer look at the surface debris under the microscope. Plast Surg (Oakv). 2017;25:179–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Santanelli di Pompeo F. A critical review of literature. October 6, 2019. Paper presented at 1st World Consensus Conference on BIA-ALCL Rome, Italy: Available at https://www.youtube.com/watch?v=YxPFayQsjUo&t=14536s. Accessed December 10, 2019 [Google Scholar]
- 47.Ching S, Thoma A, McCabe RE, et al. Measuring outcomes in aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 2003;111:469–480; discussion 481. [DOI] [PubMed] [Google Scholar]
- 48.Gutowski KA, Mesna GT, Cunningham BL. Saline-filled breast implants: a Plastic Surgery Educational Foundation multicenter outcomes study. Plast Reconstr Surg. 1997;100:1019–1027. [DOI] [PubMed] [Google Scholar]
- 49.Hetter GP. Satisfactions and dissatisfactions of patients with augmentation mammaplasty. Plast Reconstr Surg. 1979;64:151–155. [DOI] [PubMed] [Google Scholar]
- 50.Young VL, Nemecek JR, Nemecek DA. The efficacy of breast augmentation: breast size increase, patient satisfaction, and psychological effects. Plast Reconstr Surg. 1994;94:958–969. [DOI] [PubMed] [Google Scholar]
- 51.Huang GJ, Wichmann JL, Mills DC. Transaxillary subpectoral augmentation mammaplasty: a single surgeon’s 20-year experience. Aesthet Surg J. 2011;31:781–801. [DOI] [PubMed] [Google Scholar]
- 52.Pelle-Ceravolo M, Del Vescovo A, Bertozzi E, et al. A technique to decrease breast shape deformity during muscle contraction in submuscular augmentation mammaplasty. Aesthetic Plast Surg. 2004;28:288–294. [DOI] [PubMed] [Google Scholar]
- 53.Nigro LC, Blanchet NP. Animation deformity in postmastectomy implant-based reconstruction. Plast Reconstr Surg Glob Open. 2017;5:e1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Becker H, Fregosi N. The impact of animation deformity on quality of life in post-mastectomy reconstruction patients. Aesthet Surg J. 2017;37:531–536. [DOI] [PubMed] [Google Scholar]
- 55.Fracol M, Qiu CS, Chiu MW, et al. The relationship between animation deformity and patient-reported outcomes: application of the BREAST-Q to a quantitative stratification of animation severity. Plast Reconstr Surg. 2020;145:11–17. [DOI] [PubMed] [Google Scholar]
- 56.Swanson E. Prospective photographic measurement study of 196 cases of breast augmentation, mastopexy, augmentation/mastopexy, and breast reduction. Plast Reconstr Surg. 2013;131:802e–819e. [DOI] [PubMed] [Google Scholar]
- 57.Sarwer DB, Gibbons LM, Magee L, et al. A prospective, multi-site investigation of patient satisfaction and psychosocial status following cosmetic surgery. Aesthet Surg J. 2005;25:263–269. [DOI] [PubMed] [Google Scholar]
- 58.Sackett DL, Straus SE, Richardson WS, et al. Therapy. In: Evidence-based Medicine. 2000:2nd edToronto, Ontario, Canada: Churchill Livingstone; 105–154. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


