Abstract
Background.
Transplant candidates struggle making decisions about accepting kidneys with variable kidney donor profile index (KDPI) and increased risk donor (IRD) status.
Methods.
This single site, pilot randomized controlled trial evaluated the efficacy of 2 animations to improve KDPI/IRD knowledge, decisional self-efficacy, and willingness. Kidney candidates were randomly assigned to animation viewing plus standard nurse discussion (intervention) or standard nurse discussion alone (control). Linear regression was used to test the significance of animation exposure after controlling for covariates (α < 0.1).
Results.
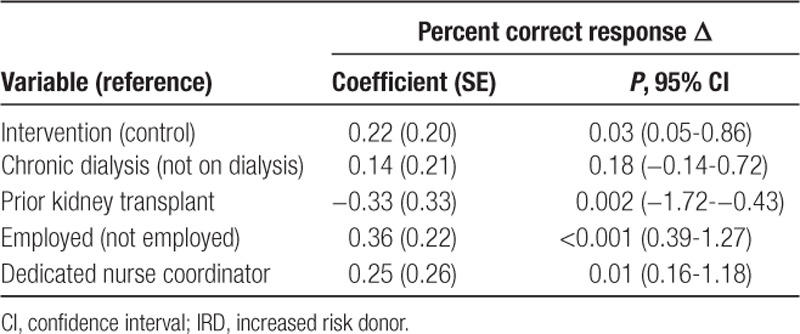
Mean age was 60 years, and 27% were African American. Both intervention (n = 42) and control (n = 38) groups received similar education at similar duration (12.8 versus 11.8 min, respectively), usually by the same dedicated nurse educator (85% versus 75%, respectively). On multivariate analysis, the intervention group (versus control) exhibited significantly increased knowledge (β = 0.23; 95% confidence interval, 0.66-1.77) and IRD willingness (β = 0.22; 95% confidence interval, 0.05-0.86). There were no between-group differences in KDPI >85% willingness or distribution of KDPI/IRD decisional self-efficacy. Over 90% of participants provided positive ratings on each of 11 acceptability items.
Conclusions.
Supporting conventional IRD and KDPI education with educational animations can improve knowledge and IRD willingness compared with standard methods.
INTRODUCTION
Timely access to deceased-donor transplantation is critical for kidney candidates. The majority of candidates do not have living donors, and longer waiting times and elevated exposure to dialysis have a deleterious effect on posttransplant outcomes.1 Several deceased-donor options are available to maximize access to kidney transplantation. Public health service increased risk donor (IRD)2 and high kidney donor profile index (KDPI)3 kidneys offer an opportunity for transplantation and survival benefit4,5 relative to dialysis, albeit with a slightly increased risk of viral disease transmission in the case of IRD,6 and lower graft longevity with high KDPI kidneys.3 Incomplete understanding about KDPI and IRD kidneys can cause confusion among patients and lead to delays in receiving a kidney transplant; therefore, relevant and understandable education is essential.
The current disclosure process predominantly involves a physician and medical staff member verbally explaining the risks and benefits of different types of deceased-donor organs around the time of transplant evaluation and again at the time of organ offer. Transplant evaluation often occurs in a busy outpatient clinic pressured by time, noise, and distractions. Disclosure at the time of organ offer happens several years later, over the phone, in a pressure-filled moment. Additional educational opportunities (eg, classes, repeat clinic visits) are provided by some transplant centers; however, these options are not universal, and face-to-face learning is less accessible to special populations with financial constraints, comorbidities, and limited mobility as well as those who rely on others for transportation.7,8 This educational process is insufficient, inconsistent, and variably comprehensible among patients.9–13
Prior studies suggest that video-based patient education may lead to greater patient comprehension and satisfaction,14 and animated videos in particular can readily overcome barriers of culture, age, time, and literacy.15 A few studies have reported improved knowledge about IRD and KDPI concepts using animated video16 or web-based decision aids17,18; however, these interventions were not equally accessible to patients of all ages, races, literacy, and internet self-efficacy levels, and only 1 study saw a significant impact in interest in IRD organs.18 Additionally, materials were not created with patients’ caregivers in mind. Caregivers, often called “lifelines,”19 increase patient self-efficacy, as patients rely on them heavily for support, decision-making, and remembering information.20-22
With the goal of educating patients and their support networks about kidney donor opportunities, we recently conducted a formative needs analysis and developed 2 theory-based educational animations that provide basic explanations—including the risks and benefits—of high KDPI23 and IRD24 kidneys. Although preliminary results from a 1-arm proof of concept study of the simplifyKDPI23 and IRD-1-2-324 animations are promising, these educational aids still require efficacy testing, both among patients and their caregivers.
This single-site randomized controlled trial aimed to evaluate the efficacy of the simplifyKDPI and IRD-1-2-3 animations among kidney transplant candidates and caregivers. Several outcome measures are targeted in the current study and include pre- and immediately post: (a) KDPI and IRD knowledge (primary outcome), (b) decisional self-efficacy (secondary outcome), and (c) willingness to receive/encourage to receive a KDPI >85% or IRD kidney (primary outcome), as well as (d) animation acceptability (secondary outcome). It is hypothesized that participants viewing the animations will report greater knowledge increases than with standard nurse education alone and that greater knowledge will be associated with greater self-reported IRD and KDPI decisional self-efficacy. We further hypothesize greater patient willingness to accept and caregiver willingness to recommend IRD kidneys but not KDPI >85% kidneys, in keeping with the findings of a previous 1-arm pilot study.
MATERIALS AND METHODS
Study Design and Population
This prospective randomized parallel controlled trial was approved by the University at Buffalo Institutional Review Board (IRB ID 00002050). All participants were recruited from patients and their caregivers who were presenting for initial kidney transplant evaluation at Erie County Medical Center (NY) between April 8, 2019, and August 29, 2019. The eligibility criteria required the participants to be 18 years or older, understand and read English (or have a support person that helps them), have acceptable vision to watch videos, be nonincarcerated, be able to give consent, and not be involved in the former modeling phase of animation development.
Study Procedures
Patients consecutively being placed in exam rooms for the kidney transplant evaluation/reevaluation were given the opportunity to participate in the study. Once eligibility was confirmed by research staff, patients were enrolled if they signed an informed consent form. After enrollment, all eligible caregivers present with the patient were also given the opportunity to participate in the study and were enrolled if they signed an informed consent form. Caregivers that did not enroll were allowed to remain in the exam room during the study. At the start of the study, after participants provided consent, patient-participants (±caregivers) were randomized in a simple 1:1 nonstratified randomization scheme to 2 study groups by the study PI (L.K.), the “animation” group and the “control” group. Randomization was performed using the GRAPHPAD PRISM 2009 statistical software (GraphPad, San Diego, CA); the randomized group allocation sequence was kept in sealed envelopes until each participant was ready to be randomized.
Before exposure to medical providers, all participants completed a self-administered sociodemographic survey followed by pretest surveys including IRD and KDPI knowledge, decisional self-efficacy, and willingness questions. Intervention arm participants watched a 2.16-minute animation about KDPI followed by a 2.05-minute animation about IRD on the exam room computer. Participants only watched each animation once. Both groups received standard transplant nurse education, which was audio-recorded for duration. Standard nurse education included the same information about KDPI and IRD as provided in the videos but was presented verbally and using a fact sheet. Immediately following standard nurse education, identical posttest surveys were completed and 2 interview questions were asked. Intervention group participants completed an Animation Acceptability Survey. Control group patients were offered the opportunity to watch the animations after completing the final posttest survey. Both groups remained in clinic rooms to complete the transplant evaluation with other providers. All participants were compensated with a $25.00 check. The clinical staff caring for the participants were blind to patient study group but were cognizant of which patients were enrolled in the study. Patients were aware of study group after consent.
Sample Size
With 80 total participants randomized in a 1:1 ratio to 2 study arms, the study had 90% power to detect a mean difference of 1.45 points on the knowledge test between the 2 comparison groups, with an SD of 2 and alpha of 0.05 in a 2-tailed analysis.
Instruments
Sociodemographic variables included self-reported age, sex, race, employment, education, marital status, total household income, prior kidney transplantation, and dialysis duration. We also assessed cellular phone and internet access using 6 items adapted from previous studies25,26 (α = 0.74 in our population), and we assessed health literacy adapted from Chew et al27 with 2 items scored on 4-point Likert-type scales: “How often do you have someone help you read hospital materials?” and “How confident are you filling out forms by yourself?” (α = 0.74 in our population).
Knowledge was assessed with a 9-item KDPI/IRD knowledge survey of true-false questions aligned with learning objectives related to the animations and consisted of 2 sections to test patient knowledge of KDPI (maximum 3 points) and IRD (maximum 6 points). The investigators designed the questionnaire for the purposes of this trial through principal component analysis of data from prior feasibility studies.23,24 Knowledge scores were obtained by summing the number of correct answers.
Decision-making self-efficacy about KDPI and IRD kidneys was assessed among patients using single-item 5-point Likert scale statements: “I have all the information I need to make a decision about kidney offers with different Kidney Donor Profile Index (KDPI) scores” and “I have all the information I need to make a decision about increased risk kidneys.” Caregiver statements were modified to begin: “I have all the information I need to help someone make a decision…”
Willingness to accept a hypothetical high KDPI or IRD offer was measured by single-item 5-point Likert scale questions: “I am comfortable getting a kidney transplant that has a KDPI score higher than 85%” and “I am comfortable getting an increased risk kidney transplant.” Among caregiver participants, both questions were modified to begin: “I am comfortable with the patient I’m with getting…”
Consent to receive KDPI >85% offers was assessed through medical record review.
Animation acceptability was measured by 11 5-point Likert scale questions adapted from previous research28 containing measures of satisfaction of viewing experience (5 items), usefulness of the information (4 items), and viewing intent (2 items).
Statistical Analysis
Both control and intervention groups were subdivided into 2 subgroups: caregivers and participants. Baseline characteristics were presented as mean ± SD or proportions. Mean differences in knowledge, self-efficacy, and willingness scores were calculated by subtracting post from baseline scores. Baseline characteristics and outcomes were compared using chi square analysis, independent 2-sample t-test, Wilcoxon Signed-Rank test, or Fisher’s exact test. Effect sizes were calculated from dividing the differences between time-point estimations and baseline by the estimated pooled SD. Covariate adjusted analysis on significant outcomes (knowledge gained and willingness) were conducted using generalized linear models with covariates included in the models using an α threshold of P < 0.1 to estimate the adjusted mean differences between the 2 groups. Acceptability of the intervention was reported as proportions of patients that agree/strongly disagree compared with other responses. Internal consistency of the acceptability scale was examined using Cronbach’s alpha. SPSS Version 24 (IBM Corp, Armonk, NY) was used for analysis.
RESULTS
Of 114 kidney transplant candidates invited to participate, 106 were eligible. Ineligibility occurred because of incarceration (n = 1), or non-English speaking (n = 7). Of all eligible kidney transplant candidates, a total of 80 participated (along with 64 caregivers) and were randomized into the intervention group (42 patients, 36 caregivers) and the control group (38 patients, 28 caregivers). The predetermined recruitment period ended in August 2019.
Baseline Characteristics
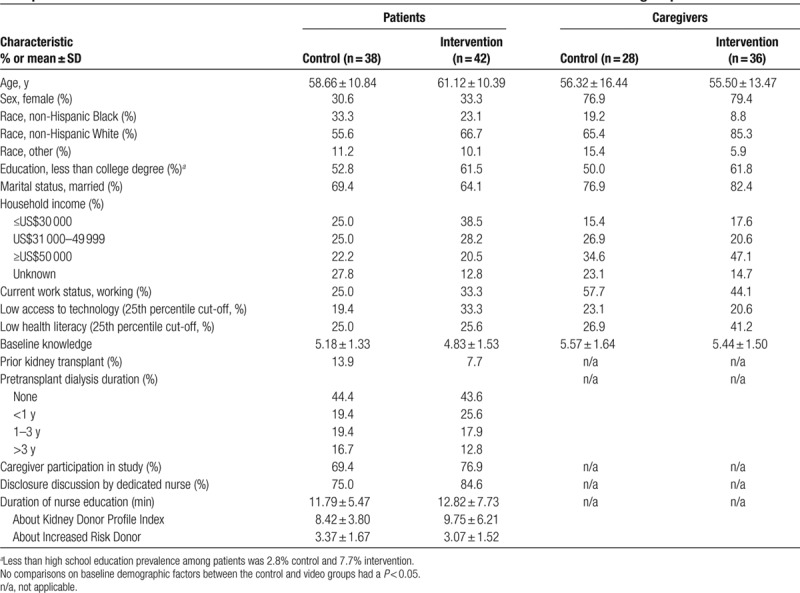
The mean age of the patient-participants was 60.0 years, 27.5% were African American, and 23.8% had low health literacy (Table 1). Of approached caregivers, 73% participated in the study. Baseline characteristics were evenly balanced between patient-participant groups with the exception of higher proportions (by >10% difference) of controls that were African American and higher proportions of intervention cases that had less than college degree, household income <US$30 000, and low access to technology. Both groups received similar education, usually by the same nurse, at similar duration.
TABLE 1.
Comparison of baseline and education session characteristics between intervention and control groups
Knowledge
Patient Knowledge
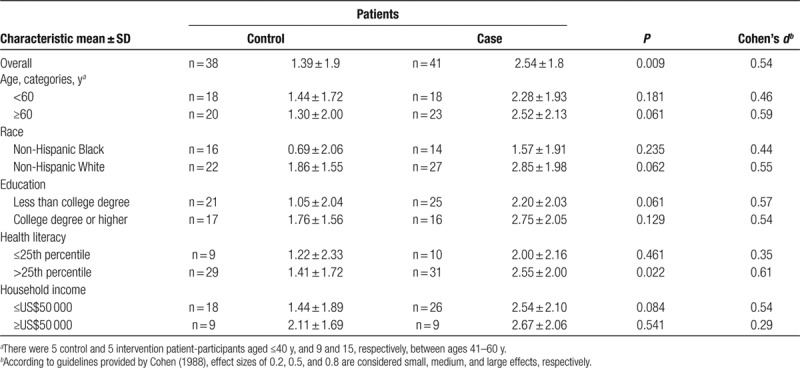
With regard to IRD and KDPI knowledge among patients, the intervention group (4.83 ± 1.53) and the control group (5.18 ± 1.33) had similar baseline knowledge scores (P = 0.280) (Table 1). On immediate postexposure testing, knowledge increased by +2.54 in the intervention group and +1.39 in the control group. This between-group difference in the improvement of poststudy scores was significant (P = 0.019) (Table 2). Multivariate analyses adjusting for confounders (Table 2) including race, caregiver participation, and dialysis status found that animation viewing was associated with a significant likelihood of improvement in knowledge score (β = 0.23; 95% CI, 0.06-1.77) (Table 3). Medium effect size increases for knowledge were found for the whole cohort (d = 0.54) and in the context of age ≥60 years (d = 0.59), AA race (d=0.44), low health literacy (d = 0.35), lower levels of educational achievement (d = 0.57), and low income (d = 0.54) (Table 4).
TABLE 2.
Factors associated with knowledge and IRD willingness (univariate linear regression analysis)
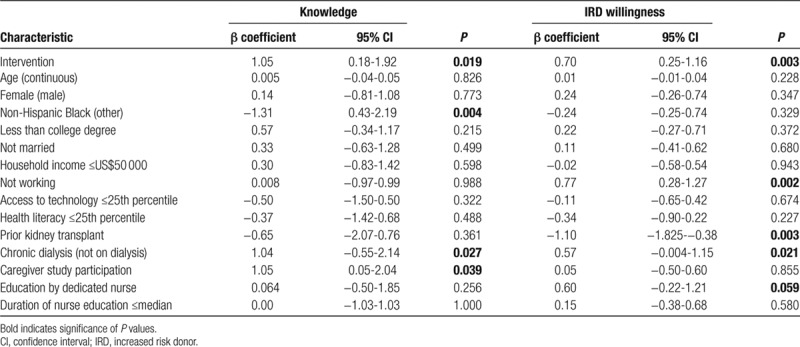
TABLE 3.
Adjusted knowledge by generalized linear regression model
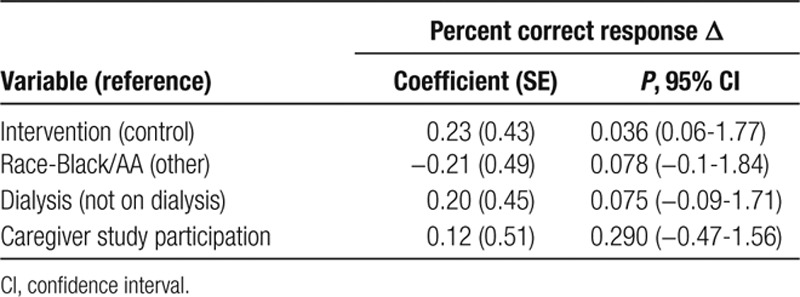
TABLE 4.
Prepost change in knowledge score
Caregiver Knowledge
With regard to caregivers, the intervention group (+2.31 ± 1.76) showed a greater increase in knowledge score compared with the control group (+1.54 ± 1.76); however, this difference was not statistically significant in between-group comparisons (P = 0.09).
Decision-making Self-efficacy
Patient Decisional Self-efficacy
Among patients, there were no between group differences in decisional self-efficacy about KDPI (intervention n = 41, +1.63 ± 1.02 versus control n = 38, +1.26 ± 1.18; P = 0.14) or IRD kidneys (intervention n = 41, +1.46 ± 0.98 versus control n = 38, +1.16 ± 1.35; P = 0.39).
Caregiver Decisional Self-efficacy
Among caregivers, there were no between group differences in decisional self-efficacy about KDPI (intervention n = 35, +1.29 ± 0.83 versus control n = 28, +1.36 ± 1.06; P = 0.77) or IRD kidneys (intervention n = 35, +2.31 ± 1.76 versus control n = 28, +1.21 ± 1.17; P = 0.09).
Willingness
Patient IRD Willingness
Willingness to accept an IRD kidney increased among animation viewers (n = 38; +0.76 ± 0.99) to a significantly greater extent compared with standard education (control n = 38, +0.05 ± 1.04; P = 0.003) (Table 2). Multivariate analyses adjusting for dedicated nurse education, employment status, previous kidney transplant, and dialysis status found that animation viewing remained associated with a significant likelihood of IRD willingness (β = 0.22; 95% CI, 0.05-0.86) (Table 5).
TABLE 5.
Adjusted willingness to receive IRD kidney by generalized linear regression model
Patient KDPI Willingness or Consent
Willingness to accept a KDPI >85% kidney decreased in the intervention (−0.51 ± 1.29) and control groups (−0.53 ± 1.33) and did not differ significantly between the groups (P = 0.96). Additional regression analysis did not show an association of age, KDPI knowledge (3 items), or the interaction of age and KDPI knowledge with willingness. The proportion of subjects signing consent to receive KDPI >85% kidney offers was 13.5% in the control group and 27.5% in the intervention group (P = 0.13). Among the subset of participants ≥60 years of age, consent to KDPI >85% was 5.6% and 17.6%, respectively (P = 0.28).
Caregiver IRD and KDPI willingness. Caregivers had similar reductions of comfort with the patient they were with getting a KDPI >85% kidney in intervention (−0.41 ± 1.42) and control (−0.28 ± 1.49) groups (P = 0.73). Caregivers reported similar increases in IRD kidney willingness on behalf of the patient in the intervention (+0.66 ± 1.03) and control (+0.39 ± 1.07) groups (P = 0.32).
Acceptability
Among those assigned to the intervention group, 42 patients (100%) and 36 caregivers (92%) completed a brief survey shortly after the nurse education. Most participants and caregivers agreed or strongly agreed that they felt comfortable using videos to learn (99% and 100%); the videos were acceptable to people of their race or culture (96% and 92%), credible (96% and 97%), easy to watch (98% and 100%), easy to understand (99% and 100%), clear (99% and 100%), and interesting (97% and 97%); the videos helped them make better decisions (97% and 97%) or increased transplant interest (94% and 69%); and they would recommend the video to a friend (100% and 100%) and use videos like this in the future (96% and 97%) (Figure 1). The Cronbach’s α estimates for the subscales were acceptable, with α ranging from 0.74 to 0.85, and the total score was excellent (α = 0.92).
FIGURE 1.
Screenshots of the simplifyKDPI and IRD 1-2-3 videos. IRD, increased risk donor; KDPI, kidney donor profile index.
DISCUSSION
The overarching goal of this efficacy trial was to test the power of 2 previously developed animations as vehicles for teaching potential kidney candidates and their caregivers about KDPI and IRD to inform decision-making.
Knowledge
We found that both animation plus standard education and standard education alone were associated with improved short-term IRD and KDPI knowledge. The observed difference in the change in knowledge scores between these 2 groups was statistically significant, indicating that animation education provides an additional advantage to impact patient knowledge. The gains in knowledge that we observed occurred within a diverse population, and the moderate effect size increases within subgroups suggest promise for impacting low literacy learners and other groups with difficulty accessing text-based education programs. The observed difference in the change in caregiver knowledge is promising but not conclusive because of the low numbers of caregivers studied, and we recommend that a sufficiently powered study be performed.
Decisional Self-efficacy
It is interesting to note that the posteducation decisional self-efficacy scores in the intervention group were not significantly higher than the control group, despite the finding of greater knowledge acquisition among those exposed to the intervention. This negative finding is in contrast to our hypothesis of a positive relationship between knowledge acquisition and self-reported efficacy expectations.29,30 The absence of a between-group difference may be the result of a “ceiling effect” since patients in both the intervention and control groups may already have been receiving very good organ offer education from the nurse educator.
Willingness
IRD. The addition of animation to standard education had a favorable impact on IRD willingness, suggesting that even 1 short dose of information reinforcement using animation media can impact decision-making. These results are consistent with a prior study evaluating different video educational approaches to organ donor readiness, which showed that dramatic, positive impact on willingness to consider donation can be achieved with 1-minute video interventions when the correct message is effectively delivered.31
KDPI. Willingness to receive a high KDPI kidney was low in both the intervention and control groups, consistent with our prior feasibility study findings. Actual consent to receive high KDPI offers was proportionately greater, by >10%, in the intervention group, but did not reach significance. This finding suggests promise that the intervention may increase access to kidney transplantation. The decision to accept different types of kidney offers should be based on a patient’s evaluation of accurate information about the possible risks and benefits of all treatment options, as well as the long-term impact on their health and lifestyle. Since KDPI knowledge was equally high between those agreeing/strongly agreeing to be willing to accept KDPI >85% kidneys and less agreeable counterparts, our data suggests these decisions were derived from a knowledgeable basis. However, qualitative analyses of the disclosure discussions may yield more nuanced information about whether patients’ values and preferences are concordant with their organ selection choices.
Acceptability
One potential concern regarding animation education is whether its impersonal nature and use of animated characters might result in decreased learner satisfaction. Among patients and caregivers randomized to the animation, mean ratings for viewing experience, satisfaction, and viewing intent of the animations were high, further supporting evidence of demand for this educational method. Ratings were also high among a subset of patients aged ≥60 years (data not shown). An additional area to explore with future research is the effect of age on receptiveness to animation-based supplemental education. Previous results have revealed generational differences in how actively patients engage in medical decision-making.32
Limitations
Blinding of nurse educators prevented us from engaging providers in shared decision-making training, which has been shown to augment the effect of patient decision aids.33 Thus, our findings may underestimate the impact of our animations where provider shared decision-making training is included. Our choice of a comparator, usual care, is not an ideal comparison for animation viewing assessments. An alternative may have been to randomize control subjects to a time-matched subject information page. Additionally, the intervention group had 2 methods of teaching and a longer educational duration, which may have increased knowledge irrespective of the animation approach. Our sample size was relatively small, thus larger studies are warranted. Use of single-center sampling limits external validity of our findings to patients with characteristics similar to those of our study population, predominantly non-Hispanic White and non-Hispanic Black. The absence of an additional follow-up period limited our ability to determine any effects of the intervention on recall or long-term behaviors, such as talking with a physician or accepting an organ offer, both important outcomes future studies should seek to evaluate. There is a risk for self-report bias and test-retest bias stemming from the prepost survey methods adopted. The extent to which the donor information contained within the animation was contaminated by the views of the nurse educator is unclear.
CONCLUSIONS
This single-center efficacy randomized controlled trial provides insights into the impact of 2 novel educational animations for subjects learning about and considering KDPI and IRD offers. The animations were acceptable to a diverse group of patients and caregivers, helped patients acquire essential knowledge to make informed deceased-donor decisions, and improved patient willingness to accept IRD kidneys.
Use of health animations may be helpful for patients to understand important fundamental concepts related to their health, have more fruitful conversations with providers and their social network, and reinforce learned concepts. From a clinical standpoint, increasing patient knowledge about transplantation and preparing learners for meetings with providers while they await services seems feasible with health animations. Having animations available to play on television monitors, for example, is one way to efficiently expose patients to this information. After provider discussion, animations can be made available on the internet to prime and reinforce information discussed during the office visit. They can also be made available for sharing between individuals and on social media to enhance support network participation in patient decision-making.
ACKNOWLEDGMENTS
The authors acknowledge the assistance of Danielle Wittek, Rachel Seibert, and Virginia Leyh during data collection.
Footnotes
Published online 23 June, 2020.
All authors participated in the intellectual content, conception, and design of the article, took public responsibility for it, and have agreed to have their name listed as contributors. Neither this article nor parts of it have been previously submitted for publication. None of the authors received any financial interest, direct or indirect, related to this work.
L.K. participated in research design, data collection and analysis, article preparation, and editing. M.K., C.C., and T.F. participated in analysis and editing. B.D. participated in article writing.
The authors declare no conflicts of interest.
This resource is supported by Research for Health in Erie County, Inc.
REFERENCES
- 1.Meier-Kriesche HU, Kaplan B; Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation. 2002; 74:1377–1381 [DOI] [PubMed] [Google Scholar]
- 2.U.S. Department of Health & Human Services. Understanding the risk of transmission of HIV, hepatitis B, and hepatitis C from U.S. PHS increased risk donors. Available at https://optn.transplant.hrsa.gov/media/2270/dtac_guidance_risks_201706.pdf. Accessed January 30, 2020
- 3.U.S. Department of Health & Human Services. Kidney donor profile index (KDPI) guide for clinicians. Available at https://optn.transplant.hrsa.gov/resources/guidance/kidney-donor-profile-index-kdpi-guide-for-clinicians/. Accessed January 30, 2020
- 4.Bowring MG, Massie AB, Henderson M, et al. Consent and labeling in the use of infectious risk donor kidneys: a response to “Information Overload”. Am J Transplant. 2018; 18:2608–2609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chow EK, Massie AB, Muzaale AD, et al. Identifying appropriate recipients for CDC infectious risk donor kidneys. Am J Transplant. 2013; 13:1227–1234 [DOI] [PubMed] [Google Scholar]
- 6.Pruett TL, Clark MA, Taranto SE. Deceased organ donors and PHS risk identification: impact on organ usage and outcomes. Transplantation. 2017; 101:1670–1678 [DOI] [PubMed] [Google Scholar]
- 7.Mohr DC, Siddique J, Ho J, et al. Interest in behavioral and psychological treatments delivered face-to-face, by telephone, and by internet. Ann Behav Med. 2010; 40:89–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berzoff J, Swantkowski J, Cohen LM. Developing a renal supportive care team from the voices of patients, families, and palliative care staff. Palliat Support Care. 2008; 6:133–139 [DOI] [PubMed] [Google Scholar]
- 9.Ahsanuddin S, Bento S, Swerdlow N, et al. Candidate comprehension of key concepts in kidney transplantation. Ann Transplant. 2015; 20:124–131 [DOI] [PubMed] [Google Scholar]
- 10.Grams ME, Womer KL, Ugarte RM, et al. Listing for expanded criteria donor kidneys in older adults and those with predicted benefit. Am J Transplant. 2010; 10:802–809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gruttadauria M, Dunn C, Lin J, et al. Patients’ expectations for longevity of kidney transplant. Prog Transplant. 2019; 29:48–53 [DOI] [PubMed] [Google Scholar]
- 12.Lewis L, Dolph B, Said M, et al. Enabling conversations: African American patients’ changing perceptions of kidney transplantation. J Racial Ethn Health Disparities. 2019; 6:536–545 [DOI] [PubMed] [Google Scholar]
- 13.Crenesse-Cozien N, Dolph B, Said M, et al. Kidney transplant evaluation: inferences from qualitative interviews with African American patients and their providers. J Racial Ethn Health Disparities. 2019; 6:917–925 [DOI] [PubMed] [Google Scholar]
- 14.Gagliano ME. A literature review on the efficacy of video in patient education. J Med Educ 1988; 63:785–792 [DOI] [PubMed] [Google Scholar]
- 15.Leiner M, Handal G, Williams D. Patient communication: a multidisciplinary approach using animated cartoons. Health Educ Res. 2004; 19:591–595 [DOI] [PubMed] [Google Scholar]
- 16.Axelrod DA, Kynard-Amerson CS, Wojciechowski D, et al. Cultural competency of a mobile, customized patient education tool for improving potential kidney transplant recipients’ knowledge and decision-making. Clin Transplant [Epub ahead of print. April 9, 2017]. doi: 10.1111/ctr.12944. [DOI] [PubMed] [Google Scholar]
- 17.Gordon EJ, Sohn MW, Chang CH, et al. Effect of a mobile web app on kidney transplant candidates’ knowledge about increased risk donor kidneys: a randomized controlled trial. Transplantation. 2017; 101:1167–1176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Volk ML, Roney M, Fagerlin A. Pilot test of a patient decision aid about liver transplant organ quality. Liver Transpl. 2014; 20:850–855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis LA, Ryszkiewicz E, Schenk E, et al. Lung transplant or bust: patients’ recommendations for ideal lung transplant education. Prog Transplant. 2014; 24:132–141 [DOI] [PubMed] [Google Scholar]
- 20.Lefaiver CA, Keough VA, Letizia M, et al. Quality of life in caregivers providing care for lung transplant candidates. Prog Transplant. 2009; 19:142–152 [DOI] [PubMed] [Google Scholar]
- 21.Song MK, Devito Dabbs AJ, Studer SM, et al. Exploring the meaning of chronic rejection after lung transplantation and its impact on clinical management and caregiving. J Pain Symptom Manage. 2010; 40:246–255 [DOI] [PubMed] [Google Scholar]
- 22.Browne T. The relationship between social networks and pathways to kidney transplant parity: evidence from black Americans in Chicago. Soc Sci Med. 2011; 73:663–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kayler LK, Dolph B, Seibert R, et al. Development of the living donation and kidney transplantation information made easy (KidneyTIME) educational animations. Clin Transplant. 2020; 34:e13830. [DOI] [PubMed] [Google Scholar]
- 24.Kayler LK, Majumder M, Dolph B, et al. Development and preliminary evaluation of IRD-1-2-3: an animated video to inform transplant candidates about increased risk donor kidneys. Transplantation. 2020; 104:326–334 [DOI] [PubMed] [Google Scholar]
- 25.Zhang X, Melanson TA, Plantinga LC, et al. Racial/ethnic disparities in waitlisting for deceased donor kidney transplantation 1 year after implementation of the new national kidney allocation system. Am J Transplant. 2018; 18:1936–1946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGillicuddy JW, Weiland AK, Frenzel RM, et al. Patient attitudes toward mobile phone-based health monitoring: questionnaire study among kidney transplant recipients. J Med Internet Res. 2013; 15:e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008; 23:561–566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ornelas IJ, Ho K, Jackson JC, et al. Results from a pilot video intervention to increase cervical cancer screening in refugee women. Health Educ Behav. 2018; 45:559–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berikai P, Meyer PM, Kazlauskaite R, et al. Gain in patients’ knowledge of diabetes management targets is associated with better glycemic control. Diabetes Care. 2007; 30:1587–1589 [DOI] [PubMed] [Google Scholar]
- 30.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977; 84:191–215 [DOI] [PubMed] [Google Scholar]
- 31.Rodrigue JR, Fleishman A, Vishnevsky T, et al. Organ donation video messaging: differential appeal, emotional valence, and behavioral intention. Clin Transplant. 2014; 28:1184–1192 [DOI] [PubMed] [Google Scholar]
- 32.Hesse BW, Nelson DE, Kreps GL, et al. Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Arch Intern Med. 2005; 165:2618–2624 [DOI] [PubMed] [Google Scholar]
- 33.Légaré F, Labrecque M, LeBlanc A, et al. Training family physicians in shared decision making for the use of antibiotics for acute respiratory infections: a pilot clustered randomized controlled trial. Health Expect. 2011; 14Suppl 196–110 [DOI] [PMC free article] [PubMed] [Google Scholar]


