Abstract
This article provides an overview of elder abuse screening and detection methods for community-dwelling and institutionalized older adults, including general issues and challenges for the field. Then, discussions of applications in emergency geriatric care, intimate partner violence (IPV), and child abuse are presented to inform research opportunities in elder abuse screening. The article provides descriptions of emerging screening and detection methods and technologies from the emergency geriatric care and IPV fields. We also discuss the variety of potential barriers to effective screening and detection from the viewpoint of the older adult, caregivers, providers, and the health care system, and we highlight the potential harms and unintended negative consequences of increased screening and mandatory reporting. We argue that research should continue on the development of valid screening methods and tools, but that studies of perceived barriers and potential harms of elder abuse screening among key stakeholders should also be conducted.
Keywords: Child abuse, elder abuse screening, emergency geriatric care, intimate partner violence, mandatory reporting
Introduction
Elder abuse is receiving increased attention from researchers, health care providers, social service professionals, and policy makers. A recent definition of “elder abuse” was proposed in The Elder Justice Roadmap Report (Connolly, Brandl, & Breckman, 2014, p. 3): Elder abuse “includes physical, sexual or psychological abuse, as well as neglect, abandonment, and financial exploitation of an older person by another person or entity, that occurs in any setting (e.g., home, community, or facility), either in a relationship where there is an expectation of trust and/or when an older person is targeted based on age or disability.” As defined, various subcategories or types of elder abuse have been described, including physical abuse, sexual abuse, emotional/psychological abuse, neglect, and financial exploitation. Although definitions of “elder” vary by state, age 60 and older is commonly used in both legal and research contexts. As the population ages and the baby boom generation begins to retire in increasing numbers; as lifespan and corresponding years of living with chronic health conditions and disability increases; as needs for informal family caregiving continue to grow with the shift from institution- to home- and community-based care, understanding and addressing elder abuse is critical to the national aging policy agenda. The inclusion of elder abuse and elder justice on the recent White House Conference on Aging agenda is clear evidence of the growing recognition of this complex social problem. This article is the result of a panel on elder abuse screening and detection at a follow-up workshop on elder abuse held at the National Institutes of Health (NIH) in October 2015.
Elder abuse research is fraught with methodological challenges, pitfalls, and barriers to implementation, and addressing the complex needs of abused older adults requires a multidisciplinary team-based approach (Du Mont, Kosa, Macdonald, Elliot, & Yaffe, 2015). Elder abuse is a generally hidden phenomenon—hidden by victims, their families, and perpetrators—involving a range of behaviors that are rarely reported to authorities. There are numerous legal and ethical challenges confronting elder abuse researchers, including issues of mandatory reporting, elder autonomy, cognitive impairment, and Institutional Review Board (IRB) issues around privacy and confidentiality. This article will provide an overview of elder abuse screening and detection methods for community-dwelling and institutionalized older adults, both those who are cognitively intact and with cognitive impairment. Then, discussions of screening and detection methods and lessons learned from the emergency geriatric care, intimate partner violence, and child abuse fields will be used to inform potential applications and research opportunities in elder abuse. The major goal of the article is to stimulate thinking among researchers and practitioners about potential applications and findings from related fields to help move elder abuse screening and detection research forward.
Screening and detection of elder abuse: Summary of methods, issues, and challenges
Detection of elder abuse through screening is the fundamental challenge for researchers and health care providers aiming to prevent further abuse and/or intervene to stop the abuse. A wide range of methods have been used to screen for and detect elder abuse in both community and institutional settings. Some of these are applicable only to cognitively intact older adults, while others are potentially useful for detecting abuse among the cognitively impaired. Table 1 provides an overview of these methods, along with a summary of the major issues and challenges confronting researchers and clinicians attempting to screen for elder abuse. We should note that some of the methods shown in Table 1 could, in addition to elder abuse screening for older adults presenting with symptoms, also be used for “case finding,” a proactive process to identify at-risk individuals from among those who might otherwise be under-recognized. This section provides a brief overview of elder abuse screening and detection methods and challenges in order to provide context for the discussions of emergency geriatric care, intimate partner violence, and child abuse that follow. Much of this section has been adapted from McMullen, Schwartz, Yaffe, & Beach (2014).
Table 1.
Overview summary of elder abuse screening and detection methods and general issues/challenges.
| Screening methods for community-dwelling older adults | Screening methods for older adults in long-term care facilities (Both staff–resident & resident–resident abuse) |
| Direct victim surveys (random sample).a | Resident surveys.a |
| Direct victim surveys (targeted disease).a | Staff surveys. |
| Direct caregiver surveys (targeted disease). | Family surveys. |
| Direct trusted other/perpetrator surveys. | Resident informant/proxy surveys. |
| Health care screening (physicians, emergency department [ED], hospital, dental clinics). | Forensic analysis (bruising)/clinical decision algorithms. |
| Forensic analysis (bruising)/clinical decision algorithms. | Video monitoring of public areas. |
| LTC ombudsman/official reports. | |
| Community “sentinels.” | |
| Social service provider detection (adult day care; home visits). | |
| APS/official reports. | |
| Summary of general issues and challenges in screening for elder abuse (EA) | |
| EA from whose perspective? Older adult victims? Clinicians? Proxy informants? Multiple reports for verification? | |
| If cognitively intact, should we always get the victim’s perspective? What if “objective” clinician judgment, observable evidence of EA, but denied by cognitively intact victim? | |
| Self-report issues (recall, accuracy, willingness to disclosure, embarrassment, fear, etc.). | |
| Health care provider time constraints; knowledge about EA; comfort screening for EA. | |
| Access to and cooperation from long-term care facilities for EA screening and research. | |
| Which screening/measurement tool to use? Many options, though all need more psychometric testing, empiric assessment of measurable benefits/harms, developmental design for implementation. | |
| Interviews vs. self-administered screening? Technology for data collection—e.g., Audio Computer-Assisted. | |
| Self Interviewing (A-CASI); impact on perceived privacy, comfort reporting. | |
| Setting, context important—own home, PCP office, waiting room, ER; presence of others, noisy, busy environments; impact on perceived privacy, comfort reporting. | |
| Neglect particularly challenging—passive (not providing needed help) or active (actively preventing access to food, water, medicine); Co-occurrence with self-neglect? | |
| Financial exploitation also especially challenging—stranger fraud/scams vs. family/trusted others (different dynamics); victim awareness? | |
| Sensitivity to the wider cultural context; differing definitions and conceptions of EA. | |
Cognitively intact only.
Source: Adapted from McMullen, Schwartz, Yaffe, & Beach (2014).
Screening and detection in community-dwelling older adults
As shown in Table 1, a variety of approaches have been used to attempt to screen for and detect elder abuse in community-dwelling older adults. Victim surveys of both general and disease-specific populations are possible for cognitively intact persons (Acierno et al., 2010; Laumann, Leitsch, & Waite, 2008), but not for those who are cognitively impaired. For impaired populations, researchers must use more indirect methods like caregiver or potential perpetrator surveys (Wiglesworth et al., 2010), health care provider screening (Fulmer, Paveza, Abraham, & Fairchild, 2000; Fulmer et al., 2005a; Yaffe, Weiss, & Lithwick, 2012; Yaffe, Wolfson, Lithwick, & Weiss, 2008), reports from social service providers or others who come into frequent contact with older adults (“sentinels”; National Center on Elder Abuse, 1998), forensic analysis of bruising patterns (Wiglesworth et al., 2009), or validated clinical prediction rule-based algorithms in emergency care settings (see below). Note that all of these techniques are also appropriate for cognitively intact older adults. Official Adult Protective Services (APS) reports are another possible detection mechanism, but there is general agreement that elder abuse is greatly under-reported and that these official reports represent merely the “tip of the iceberg” (Panel to Review Risk and Prevalence of Elder Abuse and Neglect et al., 2003). A recent population-based study in New York state, specifically designed to compare self-reported abuse with cases documented by APS and other agencies, estimated that only 1 in 23 cases of elder abuse were reported (Lifespan of Greater Rochester, Inc., 2011). In addition to the challenge of elder abuse detection among the cognitively impaired, attempts thus far to directly interview potential perpetrators or trusted others have generally been less successful (Acierno et al., 2010), and this remains a key challenge for the field. One exception is caregivers of older adults with dementia or physical illness who are willing to report frustrations and behaviors that may be classified as psychologically or physically abusive (Beach et al., 2005; Cooper et al., 2009; Paveza et al., 1992; Wiglesworth et al., 2010).
Screening and detection in older adults in long-term care facilities
Generally, less work has been conducted on the detection of elder abuse in institutional settings. Long-term care resident surveys are possible for those who are cognitively intact, although these direct surveys are rare, given access barriers. More common methods applicable to both cognitively intact and cognitively impaired residents, who make up a large portion of the institutionalized population, include staff surveys (Castle, 2012; Castle & Beach, 2013), and family member surveys (Zhang, Page, Conner, & Post, 2012). These methods have been used to detect both staff-to-resident and resident-to-resident abuse, which Lachs and colleagues have argued is the most prevalent form of abuse occurring in long-term care settings (Lachs, Bachman, Williams, & O’Leary, 2007). Resident informant/proxy surveys are also a possibility (although also rare), as is forensic bruising analyses (Wiglesworth et al., 2009)/clinical prediction rules. An intriguing possibility is the use of video monitoring and direct observation of staff–resident and resident–resident interaction in public areas like hallways and dining areas (Bharucha, Atkeson, & Chen, 2006), although there are obvious ethical considerations around privacy and confidentiality to overcome. Finally, official ombudsman reports are also available but likely represent only a small portion of the cases actually occurring, paralleling the community-based findings on reporting to APS noted above.
General issues and challenges in elder abuse screening and detection
The methods briefly reviewed above each have both strengths and weaknesses. As noted, elder abuse is a largely hidden phenomenon that victims, their families, and perpetrators are reluctant to acknowledge, much less discuss openly with strangers. Table 1 summarizes a few of the key issues and challenges that confront researchers and health care providers as they attempt to screen for and detect elder abuse. They include issues around autonomy versus clinician “objectivity”; potential self-report biases; health care provider time constraints, knowledge, and comfort; access to and cooperation from long-term care facilities; selection of appropriate tools and measures; mode of data collection and use of technology; and how the setting or context in which the abuse screening or questioning occurs may affect responses. As one example, work with cognitively intact community-dwelling older adults has shown that removing the interviewer from the situation in direct victim surveys through use of survey technologies like audio computer-assisted self-interviewing (A-CASI), in which respondents hear recorded questions through headphones and respond privately, can result in prevalence rates for financial and psychological abuse that are two to three times higher than when an interviewer asks the questions (Beach et al., 2010). In contrast, older adults may be more willing to tell their physician directly about abuse given increased trust and rapport. As screening for elder abuse in health care settings becomes more common, issues around health care provider time constraints and the best tools and methods for different care settings (physician offices, emergency departments, dental clinics, etc.) will need to be addressed. The sections on screening for elder abuse in emergency geriatric care settings cover these issues in detail. Table 1 also notes that neglect and financial exploitation pose unique challenges for screening and detection. Finally, any effort to screen for and detect elder abuse must be sensitive to the wider cultural context, and interesting work is occurring both among diverse groups in the United States (DeLiema, Gassoumis, Homeier, & Wilber, 2012; Dong & Simon, 2010) and in the international context (World Health Organization, 2008).
In sum, while researchers have made progress in the screening and detection of elder abuse using a variety of methods/tools in both community and institutional settings, among both cognitively intact and cognitively impaired older adults, many challenges remain. The goal of this article is to gain insight from work in three areas with potential relevance to elder abuse screening and detection: (a) emergency geriatric care, (b) intimate partner violence (IPV), and (c) child abuse. Emergency geriatric care represents the “front line,” or point of entry into the health care system, and it is often the only place that an isolated older adult suffering abuse will make contact with medical professionals. The potential for elder abuse screening and detection in the emergency department (ED) is receiving increased attention from researchers. The fields of IPV and child abuse have obvious relevance in attempts to understand elder abuse and are decades ahead of the burgeoning elder abuse field in terms of research and policy activities. One of the major themes of the National Institutes for Health (NIH) Workshop was potential applications of lessons learned from child abuse and IPV to inform elder abuse research. The sections that follow describe work in these fields that has potential relevance and applications to elder abuse. The article concludes with a summary and discussion of lessons learned from these related research areas and key research priorities for elder abuse research.
Exploring implementation barriers for emergency department elder abuse screening: Pertinent research and overcoming cognitive biases
The ED represents a crucial health care safety net for many vulnerable populations, including aging adults. Emergency medicine specialty societies recognize the unique challenges faced by providers delivering timely, high-quality acute care for older adults and have developed quality indicators (Terrell et al., 2009), resident core competencies (Hogan et al., 2010), research priorities (Carpenter & Gerson, 2008; Carpenter et al., 2011), and clinical guidelines (Rosenberg et al., 2014) to accelerate and promote these efforts. In 1992, the American Medical Association provided guidelines for when and how all clinicians should screen for and document elder mistreatment of all forms, using focused questions to ascertain injury mechanism and patient perceptions of mistreatment (Aravanis et al., 1993). Subsequent research has shown, however, that very few physicians follow the screening guidelines in practice (e.g., Schmeidel, Daly, Rosenbaum, Schmuch, & Jogerst, 2012). For example, one study of APS cases showed that physicians reported just 2% of suspected cases, compared with 25% by social workers/mental health professionals, and 26% by nurses (Rosenblatt, Cho, & Durance, 1996); and a 2004 survey of state APS programs found that only 1.4% of the reports were made by physicians (National Center on Elder Abuse, 2006). The constellation of nonaccidental injury or neglect lumped together as “elder abuse” has been recognized in emergency medicine for over 20 years and is appropriately emphasized in the previously mentioned priorities (Lachs et al., 1997). For example, emergency medicine residents are expected to “demonstrate ability to recognize patterns of trauma (physical/sexual, psychological, neglect/abandonment) that are consistent with elder abuse” (Hogan et al., 2010).
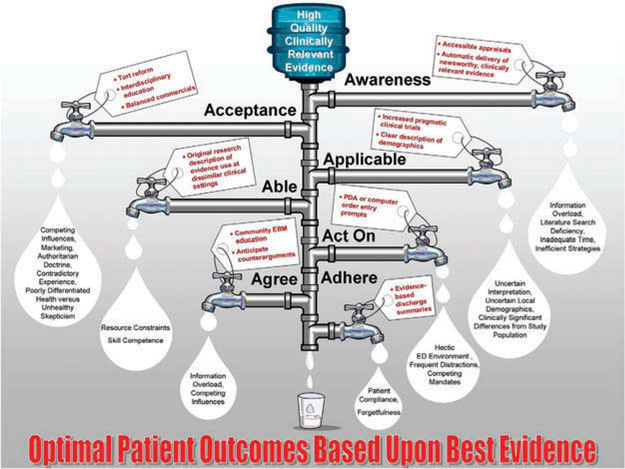
Pilot studies almost 20 years ago demonstrated the feasibility and accuracy of ED nurse screening for elder neglect (Fulmer et al., 2000). Subsequent multicenter observational research indicated that research assistant ED screening significantly underestimates elder neglect in comparison with a designated Neglect Assessment Team (Fulmer et al., 2005a), highlighting the need for an interdisciplinary approach for the assessment of elder neglect (Fulmer et al., 2005b). Preliminary ED-based research is establishing methods to empirically study elder abuse in the often chaotic emergency settings (Bloemen et al., 2016), while providing an initial glimpse into the factors that can be used to identify higher risk patients (Rosen et al., 2016). Nonetheless, elder abuse is infrequently screened for or recognized in the contemporary ED, even in those that specialize in older adults (Hogan, Olade, & Carpenter, 2014). Understanding the Knowledge Translation (KT) Pipeline (Figure 1) is the first step toward improving ED detection of elder abuse (Diner et al., 2007).
Figure 1.
Knowledge translation pipeline.
© John Wiley and Sons. Reproduced by permission of John Wiley and Sons. Permission to reuse must be obtained from the rightsholder.
The KT Pipeline conceptualizes the barriers between research evidence and bedside delivery to improve the quality, cost, and experience of health care for patients. The KT Pipeline also provides specific examples for each type of “leak” and recommendations to slow these leaks, represented by the water drops and the faucet handle, respectively. Awareness of elder abuse as a relevant, prevalent, and remediable ED issue is the initial leak. Obviously, if clinicians are neither aware of elder abuse epidemiology or the screening instruments to accurately and reliably identify cases, then routine consideration will not be expected. Some form of abuse is reported by 7% of community-dwelling, cognitively intact ED patients when queried (Stevens, Richmond, Pereira, Shenvi, & Platts-Mills, 2014). The cognitive bias of “base rate neglect” (inaccurate over- or underrepresentation of disease prevalence; Kane & Carpenter, 2016) contributes to under-recognition, because most ED providers infrequently encounter or even consider elder abuse, and so it is rarely diagnosed.
The next sequential KT Pipeline leak is acceptance. Multiple elder abuse screening instruments and protocols exist (Fulmer, Guadagno, Bitondo Dyer, & Connolly, 2004), but few have been designed for or tested in the complex ED setting (Bond & Butler, 2013; Carpenter & Gerson, 2008; but see Fulmer et al., 2000; Fulmer at al., 2005a). Emergency medicine practice consists of evaluating constellations of signs and symptoms in multiple patients in rapid sequence and assessing the risk for life-threatening health care issues that require time-dependent interventions. Accordingly, emergency medicine has developed significant interest in the scientific and cognitive approach to diagnosis and prognosis (Carpenter, Raja, & Schuur, 2013). Clinical decision instruments are constellations of signs, symptoms, or other bedside tests that more accurately identify a condition than any finding in isolation and when validated can standardize the diagnostic approach across settings (Hunter & Carpenter, 2016; Stiell & Wells, 1999). Deriving useful clinical decision instruments is rigorous and can take over a decade to complete (Hunter & Carpenter, 2016), but failure to adhere to these standards often yields instruments that fail subsequent validation (Perry et al., 2011) or remain unused by skeptical nurses and physicians (Brehaut et al., 2010; Brehaut, Stiell, & Graham, 2006). The culmination of these methods consists of an “impact analysis” in which real-world application of the instrument provides measureable patient-level or societal-level benefits that offset costs and harms. Thus far, no elder abuse screening instrument has been developed, validated, or assessed for impact using these methods, which serves as a significant acceptance barrier for evidence-based risk assessment in the immediate future.
Once awareness and acceptance of elder abuse are addressed, researchers and advocates of ED screening and/or case-finding must ensure that screening instruments are applicable across a variety of health care settings. For example, rural hospital patient populations are often different from urban settings, and they have differing access to inpatient and outpatient resources. Providers must be able to reasonably replicate both the screening and the intervention. For example, if ED guideline recommendations for elder abuse screening are based on studies from outpatient clinics, nursing homes, or hospital wards, or from research that used non-nurse, non-physician ancillary personnel not readily available in busy non-academic emergency settings, both the applicability and the realistic capability to conduct similar case finding will be significantly limited. Therefore, elder abuse researchers must evaluate institutions’ cultural capacity for change, local opinion leaders, the adaptability of screening protocols, and the fidelity of efforts to reproduce expert recommendations in disparate settings (Neta et al., 2015). The final provider-level leak in the KT Pipeline is remembering to act on the information when confronted with the appropriate patient scenario. Disruptive innovation using electronic medical records to remind providers and smart devices to prescreen vulnerable populations provide contemporary resources to offset reliance upon physician memory and personal motivation (Li, Westbrook, Callen, & Georgiou, 2012). However, automated provider-level reminders should not impede department flow. One potential barrier to use of smart devices to screen patients is older adults’ preferences for person-to-person interaction rather than technology (Brahmandam et al., 2015).
The KT Pipeline also describes patient-level leaks in terms of agreement and adherence. In terms of elder abuse screening in ED settings, agreement pertains to patients’ acceptance for health care provider screening in the chaotic emergency setting. The health care provider’s time and attention is frequently scattered across multiple patients, while both patient and provider lack familiarity with one another’s communication style, methods of delivering bedside care, and overriding priorities to ensure optimal outcomes. Furthermore, patient health literacy is frequently problematic, unmeasured, and confounded by underlying cognitive impairment in significant proportions of older adults (Carpenter et al., 2014; Kaphingst, Goodman, MacMillan, Carpenter, & Griffey, 2014). Establishing mutual rapport to facilitate meaningful and compassionate patient-centric elder abuse screening will be essential for many patients to accept this initiative when they often present for different reasons and with alternative care priorities. Adherence with follow-up referrals and recommendations will be dependent upon the level of trust established between the screening/counseling provider and the patient. Shared decision making, a collaborative process in which patients and providers make health care decisions together, could play a key role in this situation (Hess, Grudzen, Thomson, Raja, & Carpenter, 2015).
Understanding the methods required to derive high-quality risk-stratification instruments is essential to advance understanding of effective case finding. Researchers will also need to follow appropriate reporting standards to ensure reproducibility of the protocols. ED elder abuse risk stratifications can be either diagnostic or prognostic. In other words, screening can be used to identify prevalent elder abuse in terms of older adults suffering mistreatment at the time of the evaluation, whether or not that situation led to the current episode of care. Alternatively, screening can be used to predict incident elder abuse and the future sequelae of this mistreatment. Obviously these objectives are not mutually exclusive, since many victims of elder abuse have and will be mistreated repeatedly, so prevalent abuse undoubtedly predicts incident abuse. However, the research reporting standards to diagnose a disease or condition differ from those used to prognosticate future events. Diagnostic research focusing on individual predictors should adhere to the Standards for Reporting of Diagnostic Accuracy (STARD) criteria (Bossuyt et al., 2003), whereas the Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD) standards (Collins, Reitsma, Altman, & Moons, 2015) are appropriate for constellations of signs or symptoms in prognostic applications. Although the STARD criteria are most often applied to more traditional “tests” like a troponin level for acute coronary syndrome, using these standards for individual elder abuse screening elements like suspicious bruising is logical in order to begin quantifying the reliability (interprovider reproducibility), accuracy, and the degree to which the benefits of screening outweigh potential harms.
One critical and mostly unexplored component of elder abuse screening that adherence to STARD and TRIPOD reporting standards will help to overcome is potential harms of routine screening. Importantly, screening implies risk assessment of large, heterogeneous populations often presenting to health care providers for unrelated reasons but considered to be at risk based on the presence of signs or symptoms, whereas case finding implies a more proactive and focused risk stratification for at-risk populations without awaiting signs/symptoms to manifest. Unintended adverse consequences of screening or case finding can occur at the level of the institution, the health care provider, the patient, or the family. At the level of the institution, screening all older adults presenting to the ED would be an expensive, time-consuming process and could quickly overwhelm institutional and community resources, particularly if an untested protocol lacked adequate diagnostic or prognostic specificity. The unintended (and unstudied) adverse effects of elder abuse screening for health care providers include guilt and malpractice concerns for inevitable false positives, a situation that will be more common with less specific instruments. Caregivers in whom elder abuse is wrongly suspected and investigated could experience undeserved shame and reluctance to seek medical assistance in the future for the suspected victim of mistreatment. Similarly, patients who experience elder abuse screening and interventions, but are ultimately false positives, might also experience unneeded expenses, lost time, and resulting reluctance to seek medical care in the future. These adverse outcome scenarios are not unrealistic and deserve scientific evaluation by reporting the specificities for both risk factors and screening protocols, as well as the downstream consequences of those false positives when applied to real patients.
A role for forensic research to aid detection in the ED
The last section provided an overview of potential barriers to screening for elder abuse in the ED setting, along with guidance on standards for the effective development and implementation of elder abuse diagnosis and prognosis protocols. This section discusses the potential of specific forensic methods for the detection of elder abuse in the ED setting. The literature on detection of child abuse and neglect in the ED setting is briefly discussed to provide context and to highlight special challenges for elder abuse screening.
For older adults who are evaluated by health care providers in the ED or another setting, clues to the presence of physical elder abuse, sexual abuse, or neglect may exist in physical examination, radiographic imaging, or laboratory testing. Identifying pathognomonic evidence-based forensic injury patterns and biomarkers that should not occur from an accident is the cornerstone of detecting physical child abuse, which emergency physicians, radiologists, and other health care providers do commonly. Child abuse literature includes systematic reviews and large comparison studies describing key features that distinguish between inflicted physical abuse and unintentional injury (Baldwin, Pandya, Wolfgruber, Drummond, & Hosalkar, 2011; Daria et al., 2004; Kemp et al., 2008,2010; Maguire & Mann, 2013; Maguire, Mann, Sibert, & Kemp, 2005; Maguire, Moynihan, Mann, Potokar, & Kemp, 2008; Maguire et al., 2009, 2013; Pandya et al., 2009; Pierce, Kaczor, Aldridge, O’Flynn, & Lorenz, 2010; Piteau, Ward, Barrowman, & Plint, 2012; Sugar, Taylor, & Feldman, 1999; Valvano, Binns, Flaherty, & Leonhardt, 2009), such as metaphyseal fractures and bruising not over bony prominences. (See the discussion of child abuse literature below.) Describing analogous patterns in older adults that differentiate between elder abuse or neglect and the sequelae of accidental trauma or illness is more challenging than in children. This is due to the normal physiologic changes that occur with aging (Collins, 2006; Collins & Presnell, 2007; Collins & Sellars, 2005; Rosenblatt et al., 1996), including osteopenia, thinning of the skin, and easy bruising, as well as medications including blood thinners commonly used by older adults and the increased propensity of these patients to suffer standing-level falls.
Despite these challenges, systematic research similar to the work that provides the foundation for child abuse identification is critically needed to inform elder abuse detection, with the goal of identifying pathognomonic injury patterns and forensic findings. To date, physical findings, injury patterns, and other biomarkers potentially suggestive of abuse have been described (Bird et al., 1998; Bond & Butler, 2013; Chan et al., 2013; Chen & Koval, 2002; Cowen & Cowen, 2002; Dong & Simon, 2013; Friedman, Avila, Tanouye, & Joseph, 2011; Geroff & Olshaker, 2006; Golden, 2004; Heyborne, 2007; Kurrle, 2004; Lachs et al., 1997; Liao & Mosqueda, 2006; Palmer, Brodell, & Mostow, 2013; Senn, McDowell, & Alder, 2001; Yaffe & Tazkarji, 2012), but these descriptions have not been systematically validated or related to confirmed elder abuse cases. We were able to find only four studies (Murphy, Waa, Jaffer, Sauter, & Chan, 2013; Rosen et al., 2016; Wiglesworth et al., 2009; Ziminski, Wiglesworth, Austin, Phillips, & Mosqueda, 2013) that systematically evaluated injury patterns in elder abuse. Wiglesworth and colleagues compared bruises in 67 confirmed elder abuse victims to older adults with accidental trauma, finding that victims of elder abuse had bruises that were more often large (> 5 cm) and found on the face, lateral right arm, or posterior torso (Wiglesworth et al., 2009).
Ziminski and colleagues extended this work, finding that head and neck bruises were more common when victims were choked, punched, or beaten up, while lateral/anterior arm bruises were more common when the victim was grabbed (Ziminski et al., 2013). Murphy and colleagues, in a literature review, identified 839 reported cases of physical elder abuse and found that two-thirds of injuries that occur in elder abuse are to the upper extremity and maxillofacial region (Murphy et al., 2013). Rosen and colleagues examined injury patterns in ED visits in older adults living in the community in New Haven, Connecticut, from 1985 to 1992, independently known to be victims of physical elder abuse (Rosen et al., 2016). They found that abuse-related injuries were most common to the head, neck, and upper extremities. They also found that 42% of purportedly accidental injuries had suspicious characteristics, most commonly that the injury occurred more than 1 day prior to presentation or included maxillofacial injuries. Expanding on these preliminary findings is crucial to give health care providers and legal authorities the tools to identify elder abuse and intervene early to prevent sequelae (Pillemer et al., 2011).
Additional systematic research describing injury patterns in elder abuse and identifying differences between abuse-related and unintentional injuries is ongoing. Given the challenges in identifying elder abuse victims, researchers interested in studying this population need to be creative. Strategies currently being employed include examination of legal case files and use of large national databases.
Investigators working in this area have developed methodologic tools to facilitate and standardize this research, including a comprehensive, novel classification system for acute geriatric injuries and a protocol for standardized photography of acute injuries. To allow for a detailed analysis of a wide variety of injury patterns, Reisig and colleagues have developed a novel classification system/taxonomy (Reisig et al., 2015). This taxonomy uses a three-step process to fully describe and classify visible acute geriatric injuries. It includes 9 unique types of visible injury and 7 characteristics common to all injury types, including 6 body regions and 247 precise anatomic locations. Bloemen and colleagues have designed a novel protocol for standardized photography of acute injuries by nonprofessional photographers (Bloemen et al., 2016). The protocol describes in detail appropriate types of photographs and body positioning to characterize injuries on various body regions and includes instructional diagrams. Future research should use and refine these tools and assess their added value/accuracy/reliability in comparison to existing criterion standards (Glasziou, Irwig, & Deeks, 2008).
An important goal of forensic research should be using the findings to develop valid, reliable, pragmatic, and easy-to-use clinical prediction rules (CPRs) that will assist busy health care providers in identifying elder abuse. CPRs can supplement and increase the accuracy of a clinician’s diagnostic and prognostic assessments (Green, 2013; Randolph, Guyatt, Calvin, Doig, & Richardson, 1998; Stiell & Wells, 1999), and many have become an important part of standard routine medical practice (Green, 2013), particularly in the ED. CPRs have been developed to assist providers in child abuse assessment (Hymel et al., 2013; Pierce et al., 2010). Given that elder abuse is currently dramatically under-recognized, creating an easy-to-apply CPR may significantly improve identification. For example, an “elder abuse score” may be developed that includes several forensic as well as demographic and historical characteristics. If, in assessing a geriatric patient, a health care provider identifies enough characteristics to reach the threshold score, interventions such as additional history taking and examination, social work evaluation, and, if appropriate, Adult Protective Services contact should be undertaken.
Screening in intimate partner violence research
We next discuss relevant findings from the intimate partner violence (IPV) research, focusing on basic definitions and prevalence, barriers to screening for IPV in older adults, and the use of digital technologies as a possible solution.
Intimate partner violence among the elderly
Intimate partner violence (IPV) among the elderly is another form of elder abuse and mistreatment that occurs between partners in a marital or intimate relationship. IPV is repeated physical and sexual violence, and controlling behaviors, by a current or former intimate spouse or partner (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006). The Centers for Disease Control and Prevention definition also includes actual or threatened IPV acts, and verbal insults, humiliation, isolation, stalking, and financial abuse (Centers for Disease Control and Prevention, 2015). Available rates estimate IPV among elders ranges from 2% to 25% (Lachs & Pillemer, 2004; National Center on Elder Abuse, 2010).
Two patterns of elder IPV have been identified, “IPV grown old” and “Late Onset IPV” (National Committee for the Prevention of Elder Abuse, 2008; Sev’er, 2009). IPV grown old is the same pattern of IPV that has always been a part of a couple’s relationship. The intimate abusive behaviors between the couple continue as they move into late adulthood. The late onset IPV describes a pattern of IPV that begins in late adulthood and is thought to be related to retirement, which may bring on new roles for the couple; disability, especially cognitive impairment; and sexual changes related to the aging process or cognitive impairment. Although IPV victimization rates for women decrease with age, the adverse physical and mental health outcomes associated with IPV is similar for younger and older women (Fisher, Zink, & Regan, 2011; Mouton, 2003).
Issues for identifying intimate partner violence among older adults
Cultural attitudes and myths about the nature of intimate relationships among older couples often decreases the awareness of health providers and other helping professionals for the need to determine if IPV might be occurring. Adults aged 65 and older are often perceived as one homogeneous group of late adulthood. As older adults are generally healthier and living longer it has become apparent that there may be several age-unique stages, which may influence the nature of their intimate relationship. For example, couples between the ages of 60 and 80 may still be sexually active, and forced/unwanted sex may cause injuries to reproductive tissue and increase risk for sexually transmitted infections. Also, during this age period cognitive impairment may begin or progress to more obvious changes, resulting in demanding or forced sex from a long-term male sexual partner. Beyond 80 years, one or both partners may become frail, have more severe cognitive impairment, or one partner may have died. In the case of severe cognitive impairment, demands for sex, forced sex, or other physically abusive sex may increase. In some cases, women who have been victims of long-term abuse by their male partners may become physically abusive toward their frail male partners.
Screening for intimate partner violence in the elderly
Screening for IPV at any age still remains controversial. The United States Preventive Services Task Force (USPSTF) concluded that the current evidence is insufficient to assess the balance of benefits and harms of routine screening of all older adults for abuse and neglect (Moyer, 2013). Therefore, it is important for health care providers and other professionals routinely involved with the care of older adults to distinguish IPV from other forms of violence against elders. Consideration must be given to what findings/situations trigger screening for IPV in the elderly (i.e., cognitive impairment, depression, alcohol misuse or other substance misuse, etc.). Method of data collection for IPV screening is also a key consideration. In contrast to paper or pencil self-report tools, digital media such as Audio Computer-Assisted Interviewing (A-CASI) or other hand-held devices—which could be adapted for low-literate populations, non-English- or limited-English-speaking populations—may be effective (see previous discussion and additional comments below).
Universal screening for intimate partner violence is controversial
Intimate partner violence (IPV) has been acknowledged as a major public health problem. Many studies have documented adverse physical and mental health outcomes associated with IPV (Campbell & Lewandowski, 1997; Coker et al., 2002; Hathaway et al., 2000; Tjaden & Thoennes, 1998). Several professional health organizations—the American Congress of Obstetricians and Gynecologists, American Academy of Family Physicians, American College of Emergency Physicians, American Academy of Pediatricians, and Emergency Nurses Association—have written position statements and protocols calling for universal screening of all women at any point that they enter into a health care setting. However, there remains skepticism and controversy about the benefits of universal screening of all women. As noted above, The USPSTF concluded that the current evidence was insufficient to assess the balance of benefits and harms for screening all elderly or vulnerable adults (physical or mentally dysfunctional) for abuse or neglect (Moyer, 2013). However, the USPSTF did recommend that health care providers should screen for IPV among women of childbearing age and refer women who screen positive. The recommendations against universal IPV screening of all women, including older adults, was influenced by the lack of established reliability and validity among screening tools, as well as low specificity and sensitivity; fewer than 10% of physicians routinely screening for IPV, there is a lack of cultural sensitivity among existing screening tools, and there is a lack of systematic education for health care providers about best practices for screening and intervention (Rabin, Jennings, Campbell, & Bair-Merritt, 2009; Walton, Aerts, Burkhart, & Terry, 2015).
Promising strategies for screening for intimate partner violence
Researchers continue to study the best approaches for accurate, culturally appropriate, and cost-effective screening. Digital strategies are being tested in a variety of settings and have demonstrated very positive outcomes for IPV screening. One study compared and contrasted IPV rates in African American and women of African heritage in the United States and the U.S. Virgin Islands (Stockman et al., 2014). Screening was conducted by using A-CASI. Women found the technology very acceptable, and screening rates were high and accurate. The advantage of using A-CASI technology was the ability to accommodate low literacy levels as well as multiple languages, and the use of earphones that gave a sense of privacy, thus reducing some of the stigma related to revealing IPV (Sabri et al., 2013; Stockman et al., 2013, 2014). These findings are similar to those by Beach and colleagues mentioned earlier in the elder abuse context (2010). My Plan, another digital application, uses a combination of smart phone applications and Internet resources to help IPV victims resolve decisional conflicts related to their situation. The application provides screening, helps women to assess the danger/lethality of their intimate partner relationships, and helps prioritize what is important to them and what resources they need. Women are able to safely use this smartphone application in private settings and develop a safety plan that is appropriate for their situation (Galvez, Mankowski, Braun, & Glass, 2009; Glass, Eden, Bloom, & Perrin, 2010; Lindsay et al., 2013). Another researcher is currently testing the effectiveness of technology-based applications for screening in perinatal home visiting. Nurse home visitors use computer tablets to conduct IPV screening and help women to access the potential danger of their intimate relationship. Women use headphones, can listen to the screening questionnaires, can touch the screen with their answers, and can select English or Spanish language. Initial interviews with women show the technology is acceptable and makes it easier to talk with the home visitor about their situation. Home visitors have also said for some women in their caseloads it helps them enter into the conversation about their situations (Bullock, Bacchus, & Sharps, 2014).
Although the USPSTF has not recommended the universal screening for IPV among older adults, digital screening methods may enhance reliability and validity for IPV screening in this population. Digital technologies may help to address concerns about literacy, language, stigma, and/or sensitivity about revealing their IPV status. Digital technologies are highly adaptable and could be used in a variety of settings where elders reside, such as their own homes, assisted living facilities, nursing homes, and health care settings such as EDs and urgent care centers. A key issue is whether older adults are able and/or willing to use technology for screening and other research-related activity, given their less frequent use of computers and the Internet compared to their younger counterparts (58% of 65+ are online vs. 81% age 50–64; Perrin & Duggan, 2015). However, the large, aging Baby Boomer cohort is more technology-savvy than prior cohorts, and Internet use among those 65 and older has grown faster in this age group than in any other over the past 15 years (Perrin & Duggan, 2015). Thus, digital technologies are a promising tool to aid in the screening and detection of IPV among older adults.
Insights from the field of child abuse and neglect
We conclude with a brief overview of the effects of laws creating mandatory reporting of child abuse, which provide a valuable cautionary tale for elder abuse screening and detection efforts. The field of child abuse and neglect offers some important insights and caution regarding efforts to screen and detect elder maltreatment. By 1967, all 50 states and the District of Columbia had enacted mandatory reporting laws based on the United States Children’s Bureau’s model reporting law. In 1974, Congress enacted the Child Abuse Prevention and Treatment Act (Public Law 93–247: CAPTA). CAPTA provided a federal definition of child maltreatment, funds for states to implement prevention and treatment efforts, and a mandate to carry out a national incidence study of child maltreatment. State definitions of child maltreatment had to conform to requirements articulated in CAPTA in order for states to receive federal funds. The requirements include enforcing mandatory child abuse and neglect reporting laws, investigating reports of abuse and neglect, and educating the public about abuse and neglect. CAPTA has been reauthorized numerous times, with major modifications to the definition of child maltreatment and enhancing service delivery. The pre-1970s structure of the child welfare system was significantly altered by states enacting mandatory reporting laws and then the federal government establishing a standard definition of child abuse and neglect. The number of reports increased substantially. With public awareness campaigns, the development of toll-free hotlines, and the expansion of the definition of child maltreatment, reports increased from thousands each year to millions. As a consequence, investigations of suspected child maltreatment increased from thousands to as many as 3 million each year at the peak of reporting. The costs of investigations and manning hotlines are born almost entirely by the city, county, or state. As a result of mandatory reporting laws, state child protective service agencies became essentially investigatory institutions.
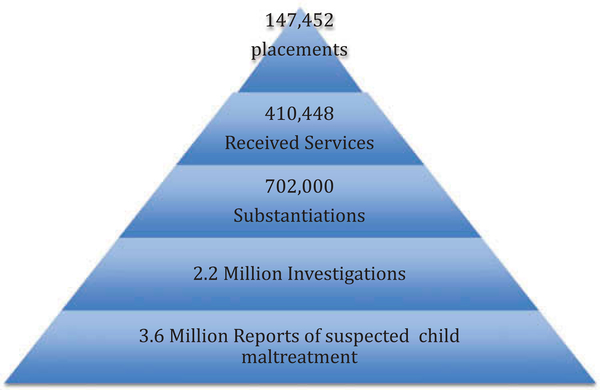
Drinking through a firehose
As a result of mandatory reporting laws, states and counties have had to, metaphorically speaking, drink through a fire hose. In 2014, according to the National Child Abuse and Neglect Data System (NCANDS; U.S. DHHS, 2016), there were 3.6 million referrals for suspected child maltreatment involving 6.6 million children. As a result of the investigations, an estimated 702,208 children were considered victims of maltreatment at the hands of parents or caregivers. Of 702,208 victims of maltreatment, 119,517 (17%) experienced physical abuse; 526,744 (75%) experienced neglect; 58,266 (8.3%) experienced sexual abuse; 42,290 (7%) experienced psychological maltreatment; and the remainder experienced medical neglect or other forms of maltreatment (U.S. DHHS, 2016).
The pathway from reporting to services highlights the fact that screening and detecting do not directly lead to services for perpetrators and protection for victims. The path is best represented by a pyramid (Figure 2). Of the 3.6 million reports, less than 1/3 were substantiated after investigation, while only 11% of the children and families received services. These statistics have remained relatively consistent over the past 25 years. The promise that mandatory reporting would bring victims out from behind closed doors has been fulfilled, but the child protective service system is metaphorically drowning in reports, most of which do not lead to either help for families or protection for children.
Figure 2.
The pathway from child abuse reporting to services.
Who reports?
In terms of who is meeting the mandate of reporting, the most recent data from the NCANDS (U.S. DHHS, 2016) indicate that the single largest category of reporters was professionals, who made 62.7% of all reports in 2014. Of the professionals, the most reports were submitted by legal and law enforcement personnel (18.1%), followed by educational personnel (17.7%), and social service personnel (11.0%). Medical personnel submitted only 9.2% of reports of suspected child abuse and neglect. A second source of data on screening and detection of child abuse and neglect is the National Incidence Study of Child Abuse and Neglect (Sedlak et al., 2010). The study found that, in terms of recognizing (but not necessarily reporting) child abuse and neglect, schools were the leading sources of maltreatment recognition, followed by hospitals. What is also important to recognize is that not all the professionals who recognize suspected child maltreatment actually reported the suspected maltreatment to state or county agencies (Zellman, 1990).
The apparent false promise of mandatory reporting laws
Despite the implementation of mandatory reporting statutes throughout the United States in the late 1960s, a report of suspected abuse in no way ensures the safety of an abused child, nor does a report create a high probability of moving a child out of harm’s way. Less than 20 years after mandatory reporting laws were implemented, Dr. Eli Newberger recognized the limits and false promise offered by mandatory reporting: “The promise implicit in the child abuse reporting laws is an empty promise for many children” (Newberger, 1983). Newberger’s concern was that the increase in reporting, and even the increase in the number of identified “victims,” was not being met with an increase in effective services for those families and children identified by mandatory reporters.
The concern over effective services for suspected victims of child maltreatment is still an issue two decades after Newberger’s pessimistic assessment. Child welfare systems still have serious shortcomings and limitations in terms of their ability to achieve the goals of safety and well-being for maltreated children.
Summary
The enactment of mandatory child maltreatment laws has clearly achieved the goal of stimulating reports of child abuse and neglect. However, all mandated reporters do not report all cases of suspected maltreatment. More importantly, the fact that a report is submitted does not directly lead to an intervention or the provision of effective services. Mandatory reporting of child maltreatment is carried out in the context of a legal, adversary system. First, while in many states a mandated reporter need only have a reasonable suspicion of child maltreatment to submit a report, the standard for substantiation is most often “probable cause,” which means the allegation must be more likely to be true than not. Second, the provision of services, both services for the family and protection of the child, is most often the result of a legal determination that the child is “dependent.” That legal determination is also based on the standard of “probable cause.” Because of the legal threshold for substantiation and state intervention, nearly 64% of suspected cases of child maltreatment end with neither the provision of any service nor any steps to protect the suspected victim(s).
Elder abuse is not a direct parallel to child maltreatment. Perpetrators of elder mistreatment do not have the same legal protection of their rights as do parents of children. A police officer may remove a victim of elder abuse from a home without a court order. Removal of a child from the home of legal caregivers requires a court order. On the other hand, the field of elder abuse would do well to observe the problems caused by a flood of reports of mistreatment that cannot be matched by existing and evidence-based effective interventions. While we may develop means of screening and detecting elder mistreatment, we must be mindful that once we identify victims, we must offer ethical, humane, and effective intervention.
Discussion
This article provides an overview of screening and detection for elder abuse, followed by discussions of potential applications in the ED setting and relevant work in IPV and child abuse. The article reviews various approaches and methods to elder abuse screening, highlighting challenges and methodological issues that confront researchers. The sections on the ED setting, IPV, and child abuse provide valuable insights and examples that can inform the elder abuse field. These insights include potential methods and approaches that show promise, barriers that must be overcome, and possible negative impacts of increased elder abuse screening and detection. Highlights from the sections on ED screening, IPV, and child abuse are summarized in Table 2.
Table 2.
Summary of key insights on elder abuse screening and detection from emergency geriatric care, IPV, and child abuse research.
| Emergency geriatric care | • KT pipeline as a model for understanding potential barriers to implementation of effective EA screening in the ED setting. • ED physicians lack of awareness of EA epidemiology/screening tools. • Existing EA screening tools have not been rigorously designed and tested as clinical decision instruments for diagnosis and prognosis, limiting acceptance by ED physicians. • There are questions about the applicability of EA screening protocols across clinical settings and patient populations. • Ability to act on screening information in the busy, hectic ED setting is a barrier. • Patient acceptance of EA screening in the ED may also be a problem. • Low patient health literacy may be a barrier to effective EA screening. • Adherence to treatment protocols depends on trust between patient and provider—shared decision making may play a key role. • Different standards may be required for diagnosis (identifying ongoing/current EA) and prognosis (predicting future EA). • We must acknowledge the potential harms of routine EA screening—time-consuming process that could overwhelm resources; false positives; physician guilt/malpractice; caregivers—falsely accused, reluctance to seek future medical help; older adult—lost time, expenses; reluctance to seek future medical help. • Describing patterns in older adults that differentiate between elder abuse or neglect and the sequelae of accidental trauma or illness is more challenging than in children. • Investigators working in this area have developed methodologic tools to facilitate and standardize this research, including a comprehensive, novel classification system for acute geriatric injuries and a protocol for standardized photography of acute injuries. • An important goal of this forensic research should be using the findings to develop valid, reliable, pragmatic, and easy-to-use clinical prediction rules (CPRs) that will assist busy health care providers in identifying elder abuse. |
| Intimate partner violence (IPV) research | • Available rates estimating IPV among elders range from 2% to 25%. • Two patterns of elder IPV have been identified, “IPV grown old” and “Late Onset IPV.” • Cultural attitudes and myths about the nature of intimate relationships among older couples often decreases the awareness of health providers and other helping professionals for the need to determine if IPV might be occurring. • Screening for IPV at any age still remains controversial. The USPSTF concluded that the current evidence is insufficient to assess the balance of benefits and harms of routine screening of all older adults for abuse and neglect. • Digital (A-CASI and Smartphone applications) strategies are being tested in a variety of settings and have demonstrated very positive outcomes for IPV screening. • Given that older adults are becoming more technology-savvy, digital screening methods offer promise for IPV screening in this population. |
| Child abuse research | • In 1974, Congress enacted the Child Abuse Prevention and Treatment Act (Public Law 93–247: CAPTA). • The requirements include enforcing mandatory child abuse and neglect reporting laws, investigating reports of abuse and neglect, and educating the public about abuse and neglect. • As a consequence, investigations of suspected child maltreatment increased from thousands to as many as 2 million each year at the peak of reporting. • The promise that mandatory reporting would bring victims out from behind closed doors has been fulfilled, but the child protective service system is metaphorically drowning in reports, most of which do not lead to either help for families or protection for children. • The single largest category of reporters was professionals, who made 62.7% of all reports in 2014. Medical personnel submitted only 9.2% of reports of suspected child abuse and neglect. • Despite the implementation of mandatory reporting statues throughout the United States in the late 1960s, a report of suspected abuse in no way ensures the safety of an abused child, nor does a report create a high probability of moving a child out of harm’s way. • Because of the legal threshold for substantiation and state intervention, nearly 64% of suspected cases of child maltreatment end with neither the provision of any service nor any steps to protect the suspected victim(s). • The field of elder abuse would do well to observe the problems caused by a flood of reports of mistreatment that cannot be matched by existing and evidence-based effective interventions. • While we may develop means of screening and detecting elder mistreatment, we must be mindful that once we identify victims, we must offer ethical, humane, and effective intervention. |
General themes and key research priorities
This article provides a broad overview of the methods, tools, barriers, challenges, and potential negative impacts of screening for elder abuse by drawing on work in emergency geriatric care, IPV, and child abuse. This section discusses a few of the major themes that emerge, along with implications for key research priorities to move the elder abuse screening and detection field forward.
There is a critical need for the continued development of novel screening and detection methods, tools, and technologies
This review highlights the fact that elder abuse screening and detection methods are underdeveloped, and th0at much work remains to be done to provide researchers and health professionals with validated tools for this purpose. While a variety of methods have (or could be) used to detect abuse in both community-dwelling and institutionalized older adults, serious barriers and challenges remain, and each method has both strengths and weaknesses. The work in the ED setting on the development of comprehensive, novel classification systems for acute geriatric injuries, and a protocol for standardized photography of acute injuries, provides an excellent example of the type of cutting-edge research that will need to be done. The use of technology-based screening tools like A-CASAI and smart-phone applications to enhance screening like those described in the IPV section is another example. On a more basic level, the field needs brief validated screening tools and behavior-specific survey items that are culturally appropriate for use in a variety of standardized assessment settings. Researchers also will need to capitalize on the revolution in technology for health-related data capture, including physiological monitoring, “smart home” technology, and video capture techniques in long-term care facilities to design better elder abuse screening and detection methods (Beach, in press).
There are substantial barriers to effective elder abuse screening and detection, and they should be the focus of research
The article highlights the potential barriers to elder abuse screening and detection from a variety of perspectives. Elder abuse is a complex, generally hidden phenomenon—it is thought to be prevalent yet it is often undetected and undocumented. Major barriers to effective elder abuse screening include victim cognitive impairment resulting in inability to report abuse; unwillingness to report by victims due to shame, fear, etc.; and general lack of access to abuse perpetrators. Researchers need to continue to develop strategies to overcome these barriers, including use of indirect detection methods and technology-based solutions. The section on screening and detection in the ED setting discussed physician- and patient/caregiver-level barriers. At the patient and caregiver levels, cultural values and perceptions of shame, doubt, guilt, and fear must be overcome to provide the opportunity for clinicians, ancillary health care providers, law enforcement, and community contacts to explore the possibility of abuse. Research methodologists, ethicists, and funders need to develop instruments and methods to better understand these issues. The provider-level issues include increasingly limited face-to-face exposure with patients, as well as malpractice environments that expect the correct answer with certainty in every case, with monetary penalties on the line if errors or misperceptions occur. Health care systems’ obstacles include a continual barrage of priorities, unfunded mandates, bureaucratic requirements, and inspections from a variety of special interest groups that are perceived to impede innovation and slow patient care. Researchers will need to explore and fully understand these provider- and health care-system-level issues prior to attempts to implement routine screening for elder abuse in ED and clinical settings. Health care provider attitudes and beliefs about the nature of older adults’ intimate relationships and sexuality as a potential barrier to IPV screening should also be the focus of research.
The potential harms of routine elder abuse screening should also be the focus of research
The field of elder abuse is dominated by calls for increased screening and detection, given that the vast majority of cases are never reported to authorities. There is obvious concern for abuse victims and a desire to intervene to stop the abuse. A key theme that emerges from this article is the potential harms and unintended adverse consequences that may result from increased detection of abuse through routine screening. While the field has focused on “false negatives”—abuse missed by health care professionals—the field also needs to consider the potential impact of “false positives.” These include the potentially devastating impact of a false accusation for a caregiver or family member, the older adult whose autonomy is threatened, the physician who feels pressure to protect the older adult but also faces potential malpractice lawsuits. False positives could also lead older adults and their caregivers to be reluctant to seek future medical care, and lead physicians to avoid elder abuse screening altogether. Another potentially negative consequence of increased elder abuse screening in settings like the ED is the potential to overwhelm already taxed resources. Finally, as noted in the section on child abuse research, mandatory reporting may simply result in a flood of mistreatment reports that cannot be matched by existing and evidence-based effective interventions. Once we identify victims, we must offer ethical, humane, and effective intervention. Researchers need to more fully understand the potential harms of increased screening from the perspective of older adults, caregivers, and health care providers.
Conclusions
Effective screening and detection of elder abuse is a necessary precursor to meaningful intervention. The hidden nature of elder abuse makes detection extremely challenging. Researchers have developed a variety of direct and indirect methods for screening and detection, but significant work remains to be done. The fields of emergency geriatric care, IPV, and child abuse offer key insights about potential innovations, but also raise fundamental questions about barriers and unintended negative consequences of increased elder abuse screening. Researchers should continue to develop and refine screening tools and approaches using scientifically valid methods and by collaborating in multidisciplinary teams. The field should also take a wider view and conduct multimethod research focused on perceptions of and solutions for specific barriers and potential negative impacts of routine screening as perceived by key stakeholders.
Acknowledgment
This article is based on the proceedings of the National Institutes of Health workshop on October, 30, 2015: Multiple Approaches to Understanding and Preventing Elder Abuse.
Funding
Dr. Rosen’s participation was supported by a GEMSSTAR (Grants for Early Medical and Surgical Subspecialists’ Transition to Aging Research) grant from the National Institute on Aging (R03 AG048109). Dr. Rosen is also the recipient of a Jahnigen Career Development Award, supported by the John A. Hartford Foundation, the American Geriatrics Society, the Emergency Medicine Foundation, and the Society of Academic Emergency Medicine.
References
- Acierno R, Hernandez MA, Amstadter AB, Resnick HS, Steve K, Muzzy W, & Kilpatrick DG (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The national elder mistreatment study. American Journal of Public Health, 100, 292–297. doi: 10.2105/AJPH.2009.163089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aravanis SC, Adelman RD, Breckman R, Fulmer TT, Holder E, Lachs M, … Sanders AB (1993). Diagnostic and treatment guidelines on elder abuse and neglect. Archives of Family Medicine, 2, 371–388. doi: 10.1001/archfami.2.4.371 [DOI] [PubMed] [Google Scholar]
- Baldwin K, Pandya NK, Wolfgruber H, Drummond DS, & Hosalkar HS (2011). Femur fractures in the pediatric population: Abuse or accidental trauma? Clinical Orthopaedics and Related Research®, 469, 798–804. doi: 10.1007/s11999-010-1339-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach SR (in press). The role of technology in elder abuse research In Dong X (Ed.), Elder abuse: Research, practice and policy. New York, NY: Springer Science. [Google Scholar]
- Beach SR, Schulz R, Degenholtz HB, Castle NG, Rosen J, Foz AR, & Morycz RK (2010). Using audio computer-assisted self-interviewing and interactive voice response to measure elder mistreatment in older adults: Feasibility and effects on prevalence estimates. Journal of Official Statistics, 26, 507–533. [PMC free article] [PubMed] [Google Scholar]
- Beach SR, Schulz R, Williamson GM, Miller LS, Weiner MF, & Lance CE (2005). Risk factors for potentially harmful informal caregiver behavior. Journal of the American Geriatrics Society, 53, 255–261. doi: 10.1111/j.1532-415.2005.53111.x [DOI] [PubMed] [Google Scholar]
- Bharucha AJ, Atkeson C, & Chen D (2006). CareMedia: Automated video and sensor analysis for geriatric care [abstract]. Journal of the American Medical Directors Association, 7, B9. [Google Scholar]
- Bird PE, Harrington DT, Barillo DJ, McSweeney A, Shirani KZ, & Goodwin CW (1998). Elder abuse: A call to action. Journal of Burn Care & Rehabilitation, 19, 522–527. doi: 10.1097/00004630-199811000-00011 [DOI] [PubMed] [Google Scholar]
- Bloemen EM, Rosen T, Cline Schiroo JA, Clark S, Mulcare MR, Stern ME, … Hargarten S (2016). Photographing injuries in the acute care setting: Development and evaluation of a standardized protocol for research, forensics, and clinical practice. Academic Emergency Medicine, 23, 653–659. doi: 10.1111/acem.12955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond MC, & Butler KH (2013). Elder abuse and neglect: Definitions, epidemiology, and approaches to emergency department screening. Clinics in Geriatric Medicine, 29, 257–273. doi: 10.1016/j.cger.2012.09.004 [DOI] [PubMed] [Google Scholar]
- Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, & Lijmer JG (2003). The STARD statement for reporting studies of diagnostic accuracy: Explanation and elaboration. Annals of Internal Medicine, 138, W1–W12. doi: 10.7326/0003-4819-138-1-200301070-00012-w1 [DOI] [PubMed] [Google Scholar]
- Brahmandam S, Holland WC, Mangipudi S, Braz VA, Medlin R, Jones CW, & Platts-Mills TF (2015). Willingness and ability of older emergency department patients to provide clinical information using a tablet computer. Journal of the American Geriatrics Society, 63, S101–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brehaut JC, Graham ID, Wood TJ, Taljaard M, Eagles D, Lott A, … Stiell IG (2010). Measuring acceptability of clinical decision rules: Validation of the Ottawa acceptability of decision rules instrument (OADRI) in four countries. Medical Decision Making, 30, 398–408. doi: 10.1177/0272989X09344747 [DOI] [PubMed] [Google Scholar]
- Brehaut JC, Stiell IG, & Graham ID (2006). Will a new clinical decision rule be widely used? The case of the Canadian C-spine rule. Academic Emergency Medicine, 13, 413–420. doi: 10.1197/j.aem.2005.11.080 [DOI] [PubMed] [Google Scholar]
- Bullock L, Bacchus L, & Sharps P (2014). Why ACA-mandated screening matters. Health eBulletin: Futures without Violence, 2014(Summer), 4–6. [Google Scholar]
- Campbell JC, & Lewandowski LA (1997). Mental and physical health effects of intimate partner violence on women and children. Psychiatric Clinics of North America, 20, 353–374. doi: 10.1016/S0193-953X(05)70317-8 [DOI] [PubMed] [Google Scholar]
- Carpenter CR, & Gerson L (2008). Geriatric emergency medicine In LoCicero J, Rosenthal RA, Katic M, & Pompei P (Eds.), A Supplement to New Frontiers in Geriatrics Research: An Agenda for Surgical and Related Medical Specialties (2nd ed., pp. 45–71). New York, NY: The American Geriatrics Society. [Google Scholar]
- Carpenter CR, Heard K, Wilber ST, Ginde AA, Stiffler K, Gerson LW, … Miller DJ (2011). Research priorities for high-quality geriatric emergency care: Medication management, screening, and prevention and functional assessment. Academic Emergency Medicine, 18, 644–654. doi: 10.1111/j.1553-2712.2011.01092.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter CR, Kaphingst KA, Goodman MS, Lin MJ, Melson AT, & Griffey RT (2014). Feasibility and diagnostic accuracy of brief health literacy and numeracy screening instruments in an urban emergency department. Academic Emergency Medicine, 21, 137–146. doi: 10.1111/acem.12315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle NG (2012). Resident-to-resident abuse in nursing homes as reported by nurse aides. Journal of Elder Abuse & Neglect, 24, 340–356. doi: 10.1080/08946566.2012.661685 [DOI] [PubMed] [Google Scholar]
- Castle N, & Beach S (2013). Elder abuse in assisted living. Journal of Applied Gerontology, 32, 248–267. doi: 10.1177/0733464811418094 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Intimate partner violence surveillance uniform definitions and recommended data elements version 2.0. Atlanta, GA: National Center for Injury Prevention and Control. [Google Scholar]
- Chan KL, Choi WM, Fong DYT, Chow CB, Leung M, & Ip P (2013). Characteristics of family violence victims presenting to emergency departments in Hong Kong. The Journal of Emergency Medicine, 44, 249–258. doi: 10.1016/j.jemermed.2012.01.061 [DOI] [PubMed] [Google Scholar]
- Chen AL, & Koval KJ (2002). Elder abuse: The role of the orthopaedic surgeon in diagnosis and management. The Journal of the American Academy of Orthopaedic Surgeons, 10, 25–31. doi: 10.5435/00124635-200201000-00005 [DOI] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, & Smith PH (2002). Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine, 23, 260–268. doi: 10.1016/S0749-3797(02)00514-7 [DOI] [PubMed] [Google Scholar]
- Collins GS, Reitsma JB, Altman DG, & Moons KG (2015). Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. Annals of Internal Medicine, 162, 735–736. doi: 10.7326/L15-5093-2 [DOI] [PubMed] [Google Scholar]
- Collins KA (2006). Elder maltreatment: A review. Archives of Pathology and Laboratory Medicine, 130, 1290–1296. doi: 10.1043/1543-2165(2006)130[1290:EMAR]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Collins KA, & Presnell SE (2007). Elder neglect and the pathophysiology of aging. The American Journal of Forensic Medicine and Pathology, 28, 157–162. doi: 10.1097/PAF.0b013e31805c93eb [DOI] [PubMed] [Google Scholar]
- Collins KA, & Sellars K (2005). Vertebral artery laceration mimicking elder abuse. The American Journal of Forensic Medicine and Pathology, 26, 150–154. doi: 10.1097/01.paf.0000163824.61361.f4 [DOI] [PubMed] [Google Scholar]
- Connolly MT, Brandl B, & Brekman R (2014). Elder justice roadmap report. Washington, DC: U.S. Department of Justice. [Google Scholar]
- Cooper C, Selwood A, Blanchard M, Walker Z, Blizard R, & Livingston G (2009). The determinants of family carers’ abusive behaviour to people with dementia: Results of the CARD study. Journal of Affective Disorders, 121, 136–142. doi: 10.1016/j.jad.2009.05.001 [DOI] [PubMed] [Google Scholar]
- Cowen HJ, & Cowen PS (2002). Elder mistreatment: Dental assessment and intervention. Special Care in Dentistry, 22, 23–32. doi: 10.1111/j.1754-4505.2002.tb01206.x [DOI] [PubMed] [Google Scholar]
- Daria S, Sugar NF, Feldman KW, Boos SC, Benton SA, & Ornstein A (2004). Into hot water head first: Distribution of intentional and unintentional immersion burns. Pediatric Emergency Care, 20, 302–310. doi: 10.1097/01.pec.0000125658.05196.b1 [DOI] [PubMed] [Google Scholar]
- DeLiema M, Gassoumis ZD, Homeier DC, & Wilber KH (2012). Determining prevalence and correlates of elder abuse using promotores: Low-income immigrant Latinos report high rates of abuse and neglect. Journal of the American Geriatrics Society, 60, 1333–1339. doi: 10.1111/j.1532-5415.2012.04025.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diner BM, Carpenter CR, O’Connell T, Pang P, Brown MD, Seupaul RA, … Mayer D (2007). Graduate medical education and knowledge translation: Role models, information pipelines, and practice change thresholds. Academic Emergency Medicine, 14, 1008–1014. doi: 10.1197/j.aem.2007.07.003 [DOI] [PubMed] [Google Scholar]
- Dong X, & Simon MA (2010). Is impairment in physical function associated with increased risk of elder mistreatment? Findings from a community-dwelling Chinese population. Public Health Reports, 125, 743–753. doi: 10.2307/41434832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, & Simon MA (2013). Association between elder abuse and use of ED: Findings from the Chicago health and aging project. The American Journal of Emergency Medicine, 31, 693–698. doi: 10.1016/j.ajem.2012.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Mont J, Kosa D, Macdonald S, Elliot S, & Yaffe M (2015). Determining possible professionals and respective roles and responsibilities for a model comprehensive elder abuse intervention: A delphi consensus survey. PLoS One, 10, e0140760. doi: 10.1371/journal.pone.0140760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher BS, Zink T, & Regan SL (2011). Abuses against older women: Prevalence and health effects. Journal of Interpersonal Violence, 26, 254–268. doi: 10.1177/0886260510362877 [DOI] [PubMed] [Google Scholar]
- Friedman LS, Avila S, Tanouye K, & Joseph K (2011). A case-control study of severe physical abuse of older adults. Journal of the American Geriatrics Society, 59, 417–422. doi: 10.1111/j.1532-5415.2010.03313.x [DOI] [PubMed] [Google Scholar]
- Fulmer T, Guadagno L, Bitondo Dyer C, & Connolly MT (2004). Progress in elder abuse screening and assessment instruments. Journal of the American Geriatrics Society, 52, 297–304. doi: 10.1111/j.1532-5415.2004.52074.x [DOI] [PubMed] [Google Scholar]
- Fulmer T, Paveza G, Abraham I, & Fairchild S (2000). Elder neglect assessment in the emergency department. Journal of Emergency Nursing, 26, 436–443. doi: 10.1067/men.2000.110621 [DOI] [PubMed] [Google Scholar]
- Fulmer T, Paveza G, VandeWeerd C, Fairchild S, Guadagno L, Bolton-Blatt M, & Norman R (2005b). Dyadic vulnerability and risk profiling for elder neglect. The Gerontologist, 45, 525–534. doi: 10.1093/geront/45.4.525 [DOI] [PubMed] [Google Scholar]
- Fulmer T, Paveza G, VandeWeerd C, Guadagno L, Fairchild S, Norman R, & Bolton-Blatt M (2005a). Neglect assessment in urban emergency departments and confirmation by an expert clinical team. Journal of Gerontology: Medical Sciences, 60, 1002–1006. doi: 10.1093/gerona/60.8.1002 [DOI] [PubMed] [Google Scholar]
- Galvez G, Mankowski ES, Braun MF, & Glass N (2009). Development of an iPod audio computer-assisted self-interview to increase the representation of low-literacy populations in survey research. Field Methods, 21, 407–415. doi: 10.1177/1525822X09350903 [DOI] [Google Scholar]
- Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH, & WHO multi-country study on women’s health and domestic violence against women study team. (2006). Prevalence of intimate partner violence: Findings from the WHO multi-country study on women’s health and domestic violence. The Lancet, 368, 1260–1269. doi: 10.1016/S0140-6736(06)69523-8 [DOI] [PubMed] [Google Scholar]
- Geroff AJ, & Olshaker JS (2006). Elder abuse. Emergency Medicine Clinics of North America, 24, 491–505. doi: 10.1016/j.emc.2006.01.009 [DOI] [PubMed] [Google Scholar]
- Glass N, Eden KB, Bloom T, & Perrin N (2010). Computerized aid improves safety decision process for survivors of intimate partner violence. Journal of Interpersonal Violence, 25, 1947–1964. doi: 10.1177/0886260509354508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasziou P, Irwig L, & Deeks JJ (2008). When should a new test become the current reference standard? Annals of Internal Medicine, 149, 816–822. doi: 10.7326/0003-4819-149-11-200812020-00009 [DOI] [PubMed] [Google Scholar]
- Golden GS (2004). Forensic odontology and elder abuse—a case study. Journal of the California Dental Association, 32, 336–340. [PubMed] [Google Scholar]
- Green SM (2013). When do clinical decision rules improve patient care? Annals of Emergency Medicine, 62, 132–135. doi: 10.1016/j.annemergmed.2013.02.006 [DOI] [PubMed] [Google Scholar]
- Hathaway JE, Mucci LA, Silverman JG, Brooks DR, Mathews R, & Pavlos CA (2000). Health status and health care use of Massachusetts women reporting partner abuse. American Journal of Preventive Medicine, 19, 302–307. doi: 10.1016/S0749-3797(00)00236-1 [DOI] [PubMed] [Google Scholar]
- Hess EP, Grudzen CR, Thomson R, Raja AS, & Carpenter CR (2015). Shared decision-making in the emergency department: Respecting patient autonomy when seconds count. Academic Emergency Medicine, 22, 856–864. doi: 10.1111/acem.12703 [DOI] [PubMed] [Google Scholar]
- Heyborne RD (2007). Elder abuse: Keeping the unthinkable in the differential. Academic Emergency Medicine, 14, 566–567. doi: 10.1197/j.aem.2007.01.015 [DOI] [PubMed] [Google Scholar]
- Hogan TM, Losman ED, Carpenter CR, Sauvigne K, Irmiter C, Emanuel L, & Leipzig RM (2010). Development of geriatric competencies for emergency medicine residents using an expert consensus process. Academic Emergency Medicine, 17, 316–324. doi: 10.1111/j.1553-2712.2010.00684.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan TM, Olade TO, & Carpenter CR (2014). A profile of acute care in an aging America: Snowball sample identification and characterization of United States geriatric emergency departments in 2013. Academic Emergency Medicine, 21, 337–346. doi: 10.1111/acem.12332 [DOI] [PubMed] [Google Scholar]
- Hunter BR, & Carpenter CR (2016). The development of clinical prediction rules In Wilson MP, Guluma KZ, & Hayden SR (Eds.), Doing Research in Emergency and Acute Care (pp. 139–147). Oxford, UK: Wiley-Blackwell. [Google Scholar]
- Hymel KP, Willson DF, Boos SC, Pullin DA, Homa K, Lorenz DJ, … Narang SK (2013). Derivation of a clinical prediction rule for pediatric abusive head trauma. Pediatric Critical Care Medicine, 14, 210–220. doi: 10.1097/PCC.0b013e3182712b09 [DOI] [PubMed] [Google Scholar]
- Kane B, & Carpenter C (2016). Cognition and decision making In Fondahn E, De Fer TM, Lane M, & Vannucci A (Eds.), Washington Manual of Patient Safety and Quality Improvement (pp. 195–209). St. Louis, MO: Wolters Kluwer. [Google Scholar]
- Kaphingst K, Goodman MS, MacMillan WD, Carpenter CR, & Griffey RT (2014). Effect of cognitive dysfunction on the relationship between age and health literacy. Patient Education and Counseling, 95, 218–225. doi: 10.1016/j.pec.2014.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp AM, Dunstan F, Harrison S, Morris S, Mann M, & Rolfe KS (2008). Patterns of skeletal fractures in child abuse: Systematic review. British Medical Journal, 337(a1518). doi: 10.1136/bmj.a1518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp AM, Joshi AH, Mann M, Tempest V, Liu A, Holden S, & Maguire S (2010). What are the clinical and radiological characteristics of spinal injuries from physical abuse: A systematic review. Archives of Disease in Childhood, 95, 355–360. doi: 10.1136/adc.2009.169110 [DOI] [PubMed] [Google Scholar]
- Kurrle S (2004). Elder abuse. Australian Family Physician, 33, 807–812. [PubMed] [Google Scholar]
- Lachs M, Bachman R, Williams CS, & O’Leary JR (2007). Resident-to-resident elder mistreatment and police contact in nursing homes: Findings from a population-based cohort. Journal of the American Geriatrics Society, 55, 840–845. doi: 10.1111/j.1532-5415.2007.01195.x [DOI] [PubMed] [Google Scholar]
- Lachs MS, & Pillemer K (2004). Elder abuse. The Lancet, 364, 1263–1272. doi: 10.1016/S0140-6736(04)17144-4 [DOI] [PubMed] [Google Scholar]
- Lachs MS, Williams CS, O’Brien S, Hurst L, Kossack A, Siegal A, & Tinetti ME (1997). ED use by older victims of family violence. Annals of Emergency Medicine, 30, 448–454. doi: 10.1016/S0196-0644(97)70003-9 [DOI] [PubMed] [Google Scholar]
- Laumann EO, Leitsch SA, & Waite LJ (2008). Elder mistreatment in the United States: Prevalence estimates from a nationally representative study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 63, S248–S254. doi: 10.1093/geronb/63.4.S248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Westbrook J, Callen J, & Georgiou A (2012). The role of ICT in supporting disruptive innovation: A multi-site qualitative study of nurse practitioners in emergency departments. BMC Medical Informatics and Decision Making, 12, 27. doi: 10.1186/1472-6947-12-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao S, & Mosqueda L (2006). Physical abuse of the elderly: The medical director’s response. Journal of the American Medical Directors Association, 7, 242–245. doi: 10.1016/j.jamda.2006.02.007 [DOI] [PubMed] [Google Scholar]
- Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, and New York City Department for the Aging. (2011). Under the radar: New York state elder abuse prevalence study. Self-reported prevalence and documented case surveys. New York, NY: New York State Office of Children and Family Services. [Google Scholar]
- Lindsay M, Messing JT, Thaller J, Baldwin A, Clough A, & Bloom T, … Glass GN (2013). Survivor feedback on a safety decision aid smartphone application for college-age women in abusive relationships. Journal of Technology in Human Services, 31, 368–388. doi: 10.1080/15228835.2013.861784 [DOI] [Google Scholar]
- Maguire S, & Mann M (2013). Systematic reviews of bruising in relation to child abuse—what have we learnt: An overview of review updates. Evidence-Based Child Health: A Cochrane Review Journal, 8, 255–263. doi: 10.1002/ebch.1909 [DOI] [PubMed] [Google Scholar]
- Maguire S, Mann MK, Sibert J, & Kemp A (2005). Are there patterns of bruising in childhood which are diagnostic or suggestive of abuse? A systematic review. Archives of Disease in Childhood, 90, 182–186. doi: 10.1136/adc.2003.044065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguire S, Moynihan S, Mann M, Potokar T, & Kemp AM (2008). A systematic review of the features that indicate intentional scalds in children. Burns, 34, 1072–1081. doi: 10.1016/j.burns.2008.02.011 [DOI] [PubMed] [Google Scholar]
- Maguire S, Pickerd N, Farewell D, Mann M, Tempest V, & Kemp AM (2009). Which clinical features distinguish inflicted from non-inflicted brain injury? A systematic review. Archives of Disease in Childhood, 94, 860–867. doi: 10.1136/adc.2008.150110 [DOI] [PubMed] [Google Scholar]
- Maguire SA, Upadhyaya M, Evans A, Mann MK, Haroon MM, Tempest V, … Kemp AM (2013). A systematic review of abusive visceral injuries in childhood—their range and recognition. Child Abuse and Neglect, 37, 430–445. doi: 10.1016/j.chiabu.2012.10.009 [DOI] [PubMed] [Google Scholar]
- McMullen T, Schwartz K, Yaffe M, & Beach S (2014). Elder abuse and its prevention: Screening and detection In IOM and NRC (Eds.), Elder abuse and its prevention: Workshop summary. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Mouton CP (2003). Intimate partner violence and health status among older women. Violence Against Women, 9, 1465–1477. doi: 10.1177/1077801203259238 [DOI] [Google Scholar]
- Moyer VA (2013). Screening for intimate partner violence and abuse of elderly and vulnerable adults: U.S. preventive services task force recommendation statement. Annals of Internal Medicine, 158, 478–486. doi: 10.7326/0003-4819-158-6-201303190-00588 [DOI] [PubMed] [Google Scholar]
- Murphy K, Waa S, Jaffer H, Sauter A, & Chan A (2013). A literature review of findings in physical elder abuse. Canadian Association of Radiologists Journal, 64, 10–14. doi: 10.1016/j.carj.2012.12.001 [DOI] [PubMed] [Google Scholar]
- National Center on Elder Abuse. (1998). The national elder abuse incidence study: Final report. Prepared for the Administration on Aging in collaboration with Westat, Inc. [Google Scholar]
- National Center on Elder Abuse. (2006). The 2004 survey of state adult protective services: Abuse of adults 60 years of age and older. Washington, DC: Author; Retrieved from http://www.napsa-now.org/wp-content/uploads/2012/09/2-14-06-FINAL-60+REPORT.pdf [Google Scholar]
- National Center on Elder Abuse. (2010). Why should I care about elder abuse? Washington, DC: U.S. Administration on Aging; Retrieved from http://www.ncea.aoa.gov/Resources/Publication/docs/WhatIsAbuse_2010.pdf [Google Scholar]
- National Committee for the Prevention of Elder Abuse. (2008). Domestic violence. Retrieved from http://www.preventelderabuse.org/elderabuse/domestic.html
- Neta G, Glasgow RE, Carpenter CR, Grimshaw JM, Rabin BA, Fernandez ME, & Brownson RC (2015). A framework for enhancing the value of research for dissemination and implementation. American Journal of Public Health, 105, 49–57. doi: 10.2105/AJPH.2014.302206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newberger EH (1983). The helping hand strikes again: Unintended consequences of child abuse reporting. Journal of Clinical Child Psychology, 12, 307–311. doi: 10.1080/15374418309533149 [DOI] [Google Scholar]
- Palmer M, Brodell RT, & Mostow EN (2013). Elder abuse: Dermatologic clues and critical solutions. Journal of the American Academy of Dermatology, 68, e37–42. doi: 10.1016/j.jaad.2011.03.016 [DOI] [PubMed] [Google Scholar]
- Pandya NK, Baldwin K, Wolfgruber H, Christian CW, Drummond DS, & Hosalkar HS (2009). Child abuse and orthopaedic injury patterns: Analysis at a level I pediatric trauma center. Journal of Pediatric Orthopaedics, 29, 618–625. doi: 10.1097/BPO.0b013e3181b2b3ee [DOI] [PubMed] [Google Scholar]
- Panel to Review Risk and Prevalence of Elder Abuse and Neglect, Committee on National Statistics, Division of Behavioral and Social Sciences and Education, National Research Council, Bonnie RJ, & Wallace RB (2003). Elder mistreatment: Abuse, neglect, and exploitation in an aging America. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Paveza GJ, Cohen D, Eisdorfer C, Freels S, Semla T, Ashford JW, … Levy P (1992). Severe family violence and Alzheimer’s disease: Prevalence and risk factors. The Gerontologist, 32, 493–497. doi: 10.1093/geront/32.4.493 [DOI] [PubMed] [Google Scholar]
- Perrin A, & Duggan M (2015, June). Americans internet access: 2000–2015. Washington, DC: Pew Research Center; Retrieved from http://www.pewinternet.org/files/2015/06/2015-06-26_internet-usage-across-demographics-discover_FINAL.pdf [Google Scholar]
- Perry JJ, Sharma M, Sivilotti ML, Sutherland J, Symington C, Worster A, … Stiell IG (2011). Prospective validation of the ABCD2 score for patients in the emergency department with transient ischemic attack. Canadian Medical Association Journal, 183, 1137–1145. doi: 10.1503/cmaj.101668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce MC, Kaczor K, Aldridge S, O’Flynn J, & Lorenz DJ (2010). Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics, 125, 67–74. doi: 10.1542/peds.2008-3632 [DOI] [PubMed] [Google Scholar]
- Pillemer K, Breckman R, Sweeney CD, Brownell P, Fulmer T, Berman J, … Lachs MS (2011). Practitioners’ views on elder mistreatment research priorities: Recommendations from a research-to-practice consensus conference. Journal of Elder Abuse and Neglect, 23, 115–126. doi: 10.1080/08946566.2011.558777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pines JM, Carpenter CR, Raja A, & Schuur J (2013). Evidence-based emergency care: Diagnostic testing and clinical decision rules (2nd ed.). Oxford, UK: Wiley-Blackwell. [Google Scholar]
- Piteau SJ, Ward MG, Barrowman NJ, & Plint AC (2012). Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: A systematic review. Pediatrics, 130, 315–323. doi: 10.1542/peds.2011-1545 [DOI] [PubMed] [Google Scholar]
- Rabin RF, Jennings JM, Campbell JC, & Bair-Merritt MH (2009). Intimate partner violence screening tools. American Journal of Preventive Medicine, 36, 439–445. e4. doi: 10.1016/j.amepre.2009.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randolph AG, Guyatt GH, Calvin JE, Doig G, & Richardson WS (1998). Understanding articles describing clinical prediction tools. Evidence based medicine in critical care group. Critical Care Medicine, 26, 1603–1612. doi: 10.1097/00003246-199809000-00036 [DOI] [PubMed] [Google Scholar]
- Reisig C, Rosen T, LoFaso VM, Bloemen EM, Mulcare MR, Stern ME, … Lachs MS (2015, May). Describing injuries in geriatric patients: Development of a comprehensive taxonomy for research and practice. Paper presented at the Society of Academic Emergency Medicine Annual Scientific Meeting, San Diego, CA. [Google Scholar]
- Rosen T, Bloemen EM, LoFaso VM, Clark S, Flomenbaum N, & Lachs MS (2016). Emergency department presentations for injuries in older adults independently known to be victims of elder abuse. The Journal of Emergency Medicine, 50, 518–526. doi: 10.1016/j.jemermed.2015.10.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg MS, Carpenter CR, Bromley M, Caterino JM, Chun A, Gerson L, … Wilber ST (2014). Geriatric emergency department guidelines. Annals of Emergency Medicine, 63, e7–e25. doi: 10.1016/j.annemergmed.2014.02.008 [DOI] [PubMed] [Google Scholar]
- Rosenblatt DE, Cho KH, & Durance PW (1996). Reporting mistreatment of older adults: The role of physicians. Journal of the American Geriatrics Society, 44, 65–70. doi: 10.1111/j.1532-5415.1996.tb05640.x [DOI] [PubMed] [Google Scholar]
- Sabri B, Stockman JK, Bertrand DR, Campbell DW, Callwood GB, & Campbell JC (2013). Victimization experiences, substance misuse, and mental health problems in relation to risk for lethality among African American and African Caribbean women. Journal of Interpersonal Violence, 28, 3223–3241. doi: 10.1177/0886260513496902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmeidel AN, Daly JM, Rosenbaum ME, Schmuch GA, & Jogerst GJ (2012). Health care professionals’ perspectives on barriers to elder abuse detection and reporting in primary care settings. Journal of Elder Abuse & Neglect, 24(1), 17–36. doi: 10.1080/08946566.2011.608044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedlak AJ, Mettenburg J, Basena M, Petta I, McPherson K, Greene A, & Li S (2010). Fourth national incidence study of child abuse and neglect (NIS-4): Report to Congress. Washington, DC: U.S. Department of Health and Human Services, Administration for Children and Families; Retrieved from http://www.acf.hhs.gov/sites/default/files/opre/nis4_report_congress_full_pdf_jan2010.pdf [Google Scholar]
- Senn DR, McDowell JD, & Alder ME (2001). Dentistry’s role in the recognition and reporting of domestic violence, abuse, and neglect. Dental Clinics of North America, 45, 343–363. ix. [PubMed] [Google Scholar]
- Sevèr A (2009). More than wife abuse that has gone old: A conceptual model for violence against the aged in Canada and the US. Journal of Comparative Studies, 40, 279–292. [Google Scholar]
- Stevens TB, Richmond NL, Pereira GF, Shenvi CL, & Platts-Mills TF (2014). Prevalence of nonmedical problems among older adults presenting to the emergency department. Academic Emergency Medicine, 21, 651–658. doi: 10.1111/acem.12395 [DOI] [PubMed] [Google Scholar]
- Stiell IG, & Wells GA (1999). Methodologic standards for the development of clinical decision rules in emergency medicine. Annals of Emergency Medicine, 33, 437–447. doi: 10.1016/S0196-0644(99)70309-4 [DOI] [PubMed] [Google Scholar]
- Stockman JK, Lucea MB, Bolyard R, Bertand D, Callwood GB, Sharps PW, … Campbell JC (2014). Intimate partner violence among African American and African Caribbean women: Prevalence, risk factors, and the influence of cultural attitudes. Global Health Action, 7, 24772. doi: 10.3402/gha.v7.24772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockman JK, Lucea MB, Draughon JE, Sabri B, Anderson JC, Bertrand D, & Campbell JC (2013). Intimate partner violence and HIV risk factors among African American and African Caribbean women in clinic-based settings. AIDS Care, 25, 472–480. doi: 10.1080/09540121.2012.722602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugar NF, Taylor JA, & Feldman KW (1999). Bruises in infants and toddlers: Those who don’t cruise rarely bruise. Puget Sound pediatric research network. Archives of Pediatrics and Adolescent Medicine, 153, 399–403. doi: 10.1001/archpedi.153.4.399 [DOI] [PubMed] [Google Scholar]
- Terrell KM, Hustey FM, Hwang U, Gerson LW, Wenger NS, & Miller DK (2009). Quality indicators for geriatric emergency care. Academic Emergency Medicine, 16, 441–449. doi: 10.1111/j.1553-2712.2009.00382.x [DOI] [PubMed] [Google Scholar]
- Tjaden P, & Thoennes N (1998). Prevalence, incidence, and consequences of violence against women: Findings from the national violence against women survey. Washington, DC: National Institute of Justice, U.S. Department of Justice. [Google Scholar]
- U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth, and Families, Children’s Bureau. (2016). Child maltreatment 2014. Retrieved from: http://www.acf.hhs.gov/programs/cb/research-data-technology/statistics-research/child-maltreatment
- Valvano TJ, Binns HJ, Flaherty EG, & Leonhardt DE (2009). Does bruising help determine which fractures are caused by abuse? Child Maltreatment, 14, 376–381. doi: 10.1177/1077559508326356 [DOI] [PubMed] [Google Scholar]
- Walton LM, Aerts F, Burkhart H, & Terry T (2015). Intimate partner violence screening and implications for health care providers. Online Journal of Health Ethics, 11. doi: 10.18785/ojhe.1101.05 [DOI] [Google Scholar]
- Wiglesworth A, Austin R, Corona M, Schneider D, Liao S, Gibbs L, & Mosqueda L (2009). Bruising as a marker of physical elder abuse. Journal of the American Geriatrics Society, 57, 1191–1196. doi: 10.1111/j.1532-5415.2009.02330.x [DOI] [PubMed] [Google Scholar]
- Wiglesworth A, Mosqueda L, Mulnard R, Liao S, Gibbs L, & Fitzgerald W (2010). Screening for elder abuse and neglect of people with dementia. Journal of the American Geriatrics Society, 58, 493–500. doi: 10.1111/j.1532-5415.2010.02737.x [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2008). A global response to elder abuse and neglect: Building primary health care capacity to deal with the problem worldwide: Main report. Geneva, Switzerland: Author. [Google Scholar]
- Yaffe MJ, & Tazkarji B (2012). Understanding elder abuse in family practice. Canadian Family Physician, 58(1336–1340), e695–698. [PMC free article] [PubMed] [Google Scholar]
- Yaffe MJ, Weiss D, & Lithwick M (2012). Seniors’ self-administration of the Elder Abuse Suspicion Index (EASI): A feasibility study. Journal of Elder Abuse & Neglect, 24, 277–292. doi: 10.1080/08946566.2011.652930 [DOI] [PubMed] [Google Scholar]
- Yaffe MJ, Wolfson C, Lithwick M, & Weiss D (2008). Development and validation of a tool to improve physician identification of elder abuse: The Elder Abuse Suspicion Index (EASI)©. Journal of Elder Abuse & Neglect, 20, 276–300. doi: 10.1080/08946560801973168 [DOI] [PubMed] [Google Scholar]
- Zellman GL (1990). Report decision-making patterns among mandated child abuse reporters. Child Abuse & Neglect, 14, 325–336. doi: 10.1016/0145-2134(90)90004-D [DOI] [PubMed] [Google Scholar]
- Zhang Z, Page C, Conner T, & Post LA (2012). Family members’ reports of non-staff abuse in Michigan nursing homes. Journal of Elder Abuse & Neglect, 24, 357–369. doi: 10.1080/08946566.2012.661687 [DOI] [PubMed] [Google Scholar]
- Ziminski CE, Wiglesworth A, Austin R, Phillips LR, & Mosqueda L (2013). Injury patterns and causal mechanisms of bruising in physical elder abuse. Journal of Forensic Nursing, 9, 84–91. quiz E1–2. 10.1097/JFN.0b013e31827d51d0 [DOI] [PubMed] [Google Scholar]