Abstract
Currently available evidence supports that the predominant route of human-to-human transmission of the SARS-CoV-2 is through respiratory droplets. Indirect hands contact with surfaces contaminated by infectious droplets subsequently touching the mouth, nose or eyes seems to be another route of an indirect contact transmission. Persistence of the virus on different surfaces and other materials has been reported in recent studies: SARS-CoV-2 was more stable on plastic and stainless steel than on copper and cardboard. Viable virus was detected up to 72 h after application to different surfaces, although infectivity decay was also observed. This evidence suggests the likelihood that waste generated from patients affected by COVID-19 or subjects in quarantine treated in private houses or in areas different from hospitals and medical centres could be contaminated by SARS-CoV-2. Consequently, waste streams may represent a route for viral spreading being a potential risk also for the operators directly involved in the different phases of waste management. To address this concern, a specific multidisciplinary working group was settled by the Italian National Institute of Health (ISS) during the COVID-19 emergency, in order to establish guidelines related to solid waste collection, delivering, withdrawal, transport, treatment and disposal. Temporary stop of waste sorting, instructions for the population on how to package waste, instructions for Companies and operators for the adoption of adequate personal protection equipment (PPE), the use and sanitation of proper vehicles were among the main recommendations provided to the community by publications of freely downloadable reports and infographics in layman language. Incineration, sterilization and properly managed landfills were identified as the facilities to be preferentially adopted for the treatment of this kind of waste, considering the main inactivation strategies of SARS-CoV-2 (e.g. treatment length > 9 days and temperature > 70 °C for more than 5 min).
Keywords: Contagious routes, Disposal, SARS-CoV-2, Waste management, Guidelines
Graphical abstract
1. Introduction
Since its first detection occurred in the city of Wuhan (China) in late December 2019 (CDC, 2020) the diffusion of the severe acute respiratory syndrome (SARS) disease, named COVID-19 (Corona Virus Disease 2019), caused by SARS-CoV-2 (officially designated by the Coronavirus Study Group of the International Committee on Taxonomy of Viruses) has grown rapidly, achieving a pandemic level as declared by the WHO on March 11th (WHO, 2020a).
Based on May 14th, 2020 total infected peoples across the world resulted in >4,240,000, with a number of total death >290,000 differently distributed in more than 210 countries (WHO, 2020b). SARS-COV-2 together with SARS-COV (2002−2003) and Middle East Respiratory Syndrome (MERS-CoV, 2012) represent the three highly pathogenic human Coronavirus emerged in the last 20 years (de Wit et al., 2016). Other common human Coronaviruses, HCoV-229E, HCoV-OC43, HCoV-NL63 and HCoV-HKU1 strains, are associated with a wide range of upper respiratory tract infections and, occasionally, lower respiratory tract infections.
SARS-CoV-2 infection can be asymptomatic or be associated with the CoViD-19, a disease with a wide spectrum of respiratory clinical manifestations ranging from fever, dry cough, and dyspnea to pneumonia, pulmonary oedema, acute respiratory distress syndrome, and multiple organ failures, requiring hospitalization in intensive care unit and leading to death in severe cases. Less common symptoms include headache, haemoptysis, nausea, vomiting, and diarrhea (Huang et al., 2020). As for other viral respiratory infections, the main transmission pathway of SARS-CoV-2 viruses is based on respiratory droplets, with average diameter ≥ 5 μm, generated by sneeze, cough, breaths or during normal speaking of infected subjects (Lewis, 2020; National Research Council, 2020; Yu et al., 2018; WHO, 2020c). Airborne transmission, referred to the presence of the virus within droplet nuclei, which are generally considered to be particles <5 μm in diameter, potentially remaining in the air for long periods of time, and therefore transmitted to distances greater than 1 m, is still a matter of debate (Anderson et al., 2020; Morawska and Cao, 2020). According to the WHO recommendations, airborne transmission may be possible in specific circumstances and settings in which procedures or support treatments that generate aerosols are performed (i.e., endotracheal intubation, bronchoscopy, etc.) (WHO, 2020c). Liu et al. (2020) reported the presence of SARS-CoV-2 in the aerosols sampled in the air inside two Hospitals of Wuhan during pandemic peaks. Similar results were also reported by Santarpia et al. (2020) concerning 13 isolation rooms in the Nebraska University Hospital, in which patients infected by SARS-CoV-2 were recovered. Both authors also indicated frequent ventilation of rooms and staying in open spaces as two effective measures for reducing virus diffusion. Different results were reported by Faridi et al. (2020) in investigating air samples from the hospital rooms of patients with confirmed COVID-19 disease. Samples were collected at a distance from 2 to 5 m from patient beds. Despite all air samples were negative, authors suggested in vivo experiments to be conducted using actual patient cough, sneeze and breath aerosols for obtaining airborne size carrier aerosols.
Detection of the SARS-CoV-2 virus in stools and sewage has also recently been reported, raising the hypothesis of a faecal-oral transmission (Ding and Liang, 2020; Heller et al., 2020); other studies have highlighted that the ACE2 (angiotensin-converting enzyme 2) receptor proteins used by SARS-CoV-2 for cellular entry are expressed in the gastrointestinal epithelium, demonstrating that SARS-CoV-2 is able to penetrate intestinal cells (Xiao et al., 2020). Therefore, although to date no cases of faecal-oral transmission of the SARS-CoV-2 virus have been reported, a transmission via this route cannot be excluded (Hindson, 2020; Gu et al., 2020).
Indirect hands contact with surfaces contaminated by infectious droplets subsequently touching the mouth, nose or eyes seems to be another route of transmission, which may contribute to the pandemic spreading. For this reason particular care in hand cleaning has been recommended, in addition to social distances (Tobias, 2020) together with the use of protective facial mask.
A great deal of discussion about the contamination (and decontamination) of inanimate surfaces and the persistence of SARS-CoV-2 on different surfaces and materials has been going on. Kampf et al. (2020) reviewed the literature about the persistence of human and veterinary coronaviruses on inanimate surfaces as well as inactivation strategies with biocidal agents, showing that Coronavirus can persist up to 9 days and can effectively be inactivated by different biocidal products. The persistence was also influenced by environmental and climatic conditions (i.e., temperature, humidity, solar radiation). On the other side, van Doremalen et al. (2020) reported that SARS-CoV-2 remained viable on different surfaces as cardboard, copper, stainless steel and plastic from 15 up to 72 h under laboratory conditions indicating also high similarity with the persistence of SARS-CoV-1 virus. Also Chin et al. (2020) investigated the stability of SARS-CoV-2 on different surfaces. Infectious virus could not be recovered from printing and tissue papers after a 3-h incubation, and from treated wood and cloth on day 2. By contrast, SARS-CoV-2 was more stable on glass and banknote (4 days), and on stainless steel and plastic (7 days). A detectable level of infectious virus was found on the outer layer of a surgical mask on day 7. The features related to the persistence of the virus on surfaces represent an environmental and public health problem not only in hospitals, operating theaters, and sanitary waiting rooms, but even in schools, cinemas, museums, and in carrying out activities such as waste collection and treatment.
It is recognized that waste from infected households and quarantine facilities would meet the definition of clinical waste. Nevertheless also waste generated in houses with subjects affected by COVID-19 could represent another potential route for the spread of the virus, hence compelling a particular attention for their management (Nghiem et al., 2020). In this view, specific concern is focused on household waste generated by patients positive to the SARS-CoV-2 tests or in compulsory quarantine treated at home or in areas other than hospitals, clinics and medical centres, managing infectious waste according to specific regulation (DPR, 2003; WHO, 2020d) and consolidated procedures.
It should not be overlooked that, even though there is no definitive evidence regarding the time of persistence of the virus on such waste, and the potential for transmission, there is a diffused perception of citizens, operators and workers that these waste could represent a threat for their health and for the further spreading of the virus (Gomes Mol and Caldas, 2020). These problems resulted even more emphasized for the workers of the informal sector, a very diffused economic activity in some areas of the world, often operating with no Personal Protection Equipment (PPE) and lack of minimal safety and health protection requirements (Cruvinel et al., 2019).
In this context, the European Commission states that there is no evidence regarding the transmission of the virus via household waste management, recommending the continuity of proper municipal waste management services, including waste sorting for recycling (EC, 2020). Nevertheless, this generic suggestion neglects the complexity of the waste management, dismissing the prominent role played by the socio-economic implications, being quite distant from the realistic perception of the problems faced by the general population and the other stakeholders. Best management practices for handling such waste results a challenging activity due to the disperse nature of cases and infected individuals along with lack of scientific evidences (Nghiem et al., 2020). Based on the Association of Cities and Regions for Sustainable Resource Management (ACR+, 2020) during the lockdown period both public authorities and operators were forced to adapt waste management procedure and practices for ensuring safety and health care protection to workers. Within the EU area different procedures were adopted by the Member States. The UK government has allowed higher amount of temporarily stored waste, if not removable due COVID-19 crisis, incineration of SARS-CoV-2 infected waste and disposal of PPE used by health care workers treating patients at their home without any modification to plant permission (ACR+, 2020). The German National Government indicated to dispose packaging, paper and organic waste in the residual waste bin. In the USA no particular regulations were introduced for managing household waste suspected to be infected by the SARS-CoV-2, beside the adoption of PPE and other precautions already being imposed by safety regulation for workers. Similar indications were also supplied by the Israelian Ministry of Environmental protection, by the Ramallah Municipality in Palestine and by the Peruvian Ministry of Environment. All these indicate that at the current state of the art there is a lack of knowledge about the infection potential of waste, leading the different countries to adopt different procedures with different approaches and based on different perceptions, reflecting somewhat the social and economic differences, of the potential risk of SARS-CoV-2 spread by waste management.
Based on these considerations, since the 15th March 2020, during the peak of Covid-19 pandemic, a multidisciplinary working group (WG) was appointed at the Italian National Institute of Health (ISS) gathering medical, biological, environmental, hygiene and engineering experts also involving different stakeholders such as local authorities, and waste management companies. The aim of the WG has been to provide pragmatic response and guidelines for the management of the waste generated by patients that resulted positive to the SARS-CoV-2 tests and/or in compulsory quarantine treated at home or in areas other than hospitals and medical centres (ISS, 2020). A continuous update of knowledge has been carried out as new scientific evidence on the persistence or transmission of SARS-CoV-2 thorough waste and similar products becomes available, leading to the issue of two revisions to be issued.
2. Waste management
The Covid-19 serious emergency has presented new and significant challenges for the provision of waste collection services and for operators collecting and handling such waste. Nevertheless the structure of SARS-CoV-2 may have important implications for waste management. In fact, SARS-CoV-2 virion is a small spherical particle (≈100 nm diameter), with a positive single stranded RNA genome within a fragile lipid envelope. Just due to the nature of the lipid envelope, the viral particles may become non-viable (i.e. non-infectious) once the envelope is damaged, even though their RNA may still be detected.
Taking into account this challenge, the main goal of the WG was the development of feasible practices and procedures aimed to minimize risks by preventing exposure of the population and workers to SARS-CoV-2 through contaminated waste, ensuring health protection by adequate waste management, based on the current scientific evidence of persistence of the virus on different surface and materials.
Consequently, a first step was the identification of the main potential routes of infection and exposure scenario along the different waste management phases.
Routes of infections:
-
1)
direct contact with contaminated objects and/or surfaces (Kampf et al., 2020; van Doremalen et al., 2020);
-
2)
contact with airborne droplets at a distance <2 m (Faridi et al., 2020; Liu et al., 2020; Santarpia et al., 2020).
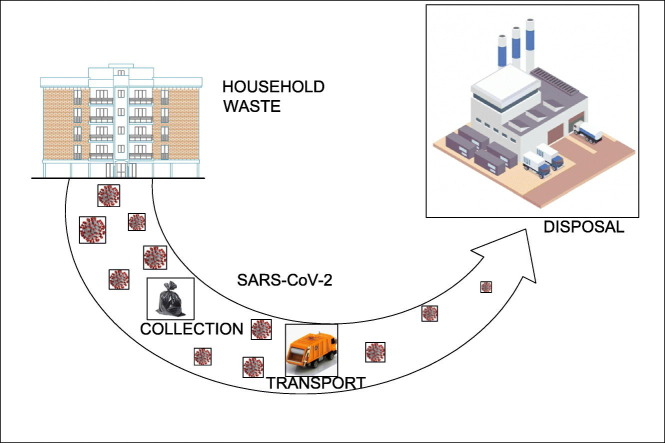
Waste management phases, as depicted in Fig. 1 , representing a potential exposure to the virus:
-
1)
waste packing and delivering by the users;
-
2)
waste withdrawal by workers and/or trained volunteers;
-
3)
waste transport;
-
4)
waste treatment.
Fig. 1.
Management phases of waste produced by subjects positive or suspected positive to SARS-CoV-2.
2.1. Waste packing and delivering by the users
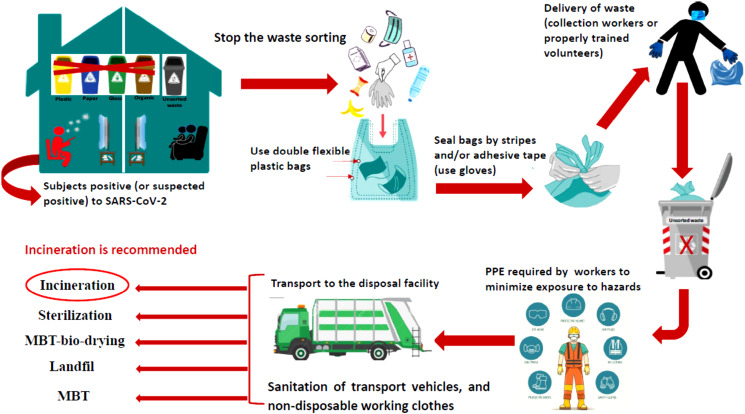
The potential routes of infection related to management activities of the household waste (generated by subjects positive to SARS-CoV-2 or suspected positive) from packing at home to the transport could the identified: i) contact with contaminated surfaces and objects during the waste handling; ii) potential generation of aerosol during withdrawal. In the hypothesis that objects and materials contained in the household waste (i.e. plastics, paper, metals, glasses, food, masks, other medical devices) could be contaminated by SARS-CoV-2, a first general recommendation was to stop the waste sorting putting all the waste commingled in the same bag, irrespective of the origin and type of material. This was done to reduce the risk of splitting the potentially infected materials in several recyclables and not recyclables streams, hence decreasing the probability of the diffusion of the virus.
Waste should be adequately packaged in order to protect waste handlers and the public from possible injury and disease that may result from contact with the waste. To prevent both the leak of waste from the bags and their mixing with the ones generated by other users, it was recommended to always use double flexible plastic bags, possibly characterized by a colour different from the bags commonly used for the waste collection in the given area. Furthermore it was recommended to carefully wrap eventually sharp materials intended to be inserted in the bags. The integrity of the packaging must be preserved through handling, storage, transportation and treatment. Before the delivery of these wastes to collection workers or properly trained volunteers, it was recommended to adequately seal garbage bags by stripes and/or adhesive tape. A similar approach was also indicated by the German government (ACR+, 2020). Never use bare hands but disposable (i.e. single use) gloves of the correct size, avoiding any compression or compaction which can destroy the integrity of the packaging and/or generate possible aerosol droplets. The disposable gloves used for such purposes have to be discharged in a new waste bag, taking the utmost care to peel downwards, away from the wrist, turning the glove inside out.
2.2. Waste withdrawal by workers and/or trained volunteers
Dedicated withdrawal, when possible, could be preferable with specific time scheduling to favour specific pathways for the household waste coming from users affected by SARS-CoV-2 or in quarantine. ACR+ (2020) reports that average life span of SARS-CoV-2 in the ambient is of about 72 h recommending such delay in waste collection in order to avoid or decrease the risk for the presence of active viruses on these materials. Even if this indication is in line with the work of Kampf et al. (2020), concerning the investigation of the persistence of the coronaviruses on single materials under laboratory conditions, no scientific evidence is at the moment available for the persistence of the virus on waste. The moisture status, the presence of biodegradable compounds, food residues and other similar materials reasonably suggest that the persistence of SARS-CoV-2 on waste could be different with respect to the one detected on isolated smooth surfaces. Consequently a delay in the collection of 72 h appears not enough for ensuring the safety of workers.
The developed guidelines also gave indication about the PPE that workers and/or specifically trained volunteers involved in the collection of these bags have to wear (e.g. mask filters and, above the specific safety equipment already requested by the current legislation, a disposable coverall). PPE together with particular care in personal hygiene were also indicated as the most effective approaches for preventing the virus spreading among workers of both formal and informal waste management sector (WIEGO, 2020).
Furthermore, to minimize the risk of contact, workers are also requested to dress disposable gloves under the working ones as well as disposable covers on their working boots. At the end of the working shift, all the disposable clothes have to be removed in dedicated areas of the looker rooms (respecting the rules of social distance of at least 1 m) and be properly disposed. The specific procedure to be followed by the operators was described and depicted in a specific infographic in layman language, freely downloadable from the ISS web site (https://www.iss.it/en/coronavirus).
In case the worker accidentally manipulates a damaged bag, hence directly touching waste with working non-disposable gloves, the operator has to notify the person responsible of the Company to replace them immediately.
The guidelines also gave indication on the action to be taken by the Company for the sanitation of cockpit of the transport vehicles, the locker room and the non-disposable working clothes.
2.3. Waste transport
In order to minimize further possible contact of potentially contaminated waste with other waste surfaces or equipments, once withdrawn they have to be transported directly to the disposal facility without any pre-treatment. Furthermore, it is also recommended to avoid the use of collection and transport vehicles with automatic compaction systems. In fact, for the optimization of the waste loading capacity and hence collection costs, larger size collection vehicles >6m3 are equipped with hydraulic systems able to achieve a compaction ratio of the waste loaded up to 1:4 (Di Maria and Micale, 2013). Such high compaction ratio generally produce rips in the bags with leakage of waste material in the loading bed of the vehicle representing another potential route for the diffusion of the virus, in particular if the same vehicle is successively employed for another collection route without preliminary disinfection.
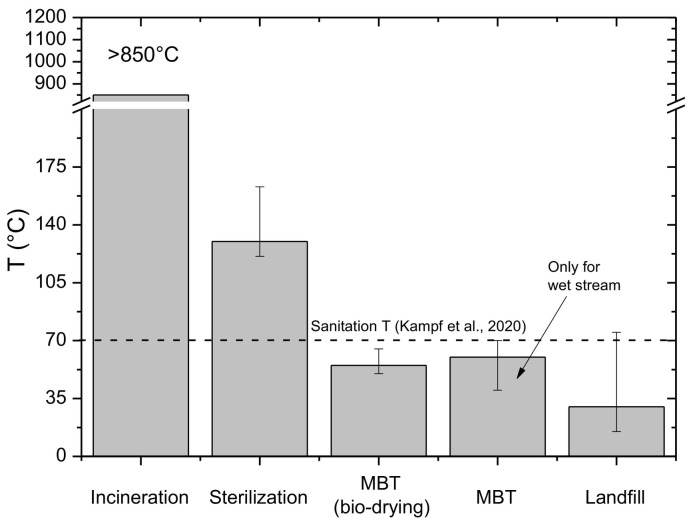
2.4. Waste treatment
High temperatures (>70 °C) maintained for times longer than 5 min have been reported to be very effective for the inactivation of the SARS-CoV-2 (Chin et al., 2020) indicating incineration, also in facilities authorized for not hazardous waste, as the safer and preferable disposal technology (Fig. 2 ). In these facilities the combustion efficiency is ensured by specific devices able to maintain temperature >850 °C and the residence of waste in the furnace >1 h (Di Maria et al., 2018) (Fig. 2). Also in this case, in order to minimize the risk of contact with other waste and surfaces, it is important to directly introduce these waste into the furnace hopper with priority with respect to the other waste stored in the plant. To this aim differently colored bags, whether used, could help the operators to better identify them. Furthermore flexible bags should be preferred to solid bins, in particular for small size facilities (i.e. <100,000 t/year), to avoid difficulties for their handling by crane bridges, clogging of the furnace feeder and risks of emission peaks in the flue gases in particular concerning HCl from PVC containers. If incineration resulted not possible the second recommended option is sterilization as the one already used for infective medical waste mainly based on a preliminary waste shredding followed by its treatment in autoclave at temperature ranging from 121 °C to 163 °C (Windfeld and Brooks, 2016) generally by saturated steam (DPR, 2003; WHO, 2020d). By the way, sterilization is not a definitive treatment since the outlet materials cannot be used for recycling operation but only for the production of solid recovered fuel, incineration and landfilling. Furthermore daily treatment capacity of sterilization facilities is usually limited, when compared to the incinerators, resulting not adequate during crisis periods such as a pandemic when the amount of waste to be processed could significantly rise.
Fig. 2.
Temperature levels achievable in the different treatment facilities.
Mechanical biological treatment (MBT) can also be considered as possible disposal option but only if the waste undergoes to an effective sanitation treatment before any sorting operation and only if no manual operation are performed. MBT can operate virus inactivation by temperature and/or by time. Concerning the inactivation by temperature, the mechanical biological stabilate process, also known as bio-drying (Di Maria et al., 2012) showed more favourable features. In fact, the whole unsorted waste, after a simple shredding, is moved into aerobic biocells where the heat generated by the spontaneous degradation of the organic fraction causes a contemporary increase of the temperatures and a reduction of the humidity. Temperature >55 °C are usually maintained for a period >10 days and the whole process is characterized by a high level of automation. Kampf et al. (2020) reported a persistence of coronaviruses at temperature ranging from 20 °C to 40 °C of 2 h up to 5 days suggesting that the performances of mechanical stabilate process appear adequate with respect to sanitation efficiency. The second group of MBT technology appears less effective for the sanitation: the waste is preliminary sorted in two main streams (Di Maria, 2012): a dry stream rich mainly in plastics, paper, cardboard and other high calorific materials; a wet stream mainly consisting of organic fraction. After this first sorting, the dry stream is moved toward further sorting operation, whereas the wet one is moved to the biostabilization section. The latter generally consists of an aerobic process, during which the heat generated by the degradation of the organic fraction causes an increase of temperature > 40 °C up to about 70 °C for about two weeks. In this case the sanitation of the wet stream resulted quite effective, whereas the one of the dry stream can be achieved only if adequate storage periods are provided. In any case in all the operations for the waste storage (e.g. handling, pressing, wrapping) any contact of the workers with the waste have to be avoided. In is also worthy to highlight that at room temperature and around 4 °C the persistence of coronaviruses on different surfaces and materials was detected up to >28 days (Kampf et al., 2020).
Landfilling showed adequate features for both sanitation, based on survival period (Kampf et al., 2020) and avoidance of further diffusion routes if the potentially infected waste are placed in dedicated areas clearly identified providing also a daily coverage preferable with water proof liners. Furthermore landfilling represents also the final destination and no more treatments are necessary. However, due to the degradation of biodegradable compounds and heat accumulation phenomena, temperatures up to 75 °C were detected in the landfill bodies (Di Maria et al., 2016), indicating that also for these facilities the temperature levels can contribute to the sanitation process.
3. Communication strategy
Bearing in mind the perceived risk from the citizens, operators and workers, and the need to give indications to be properly implemented, once developed, the Guidelines were disseminated using different media and considering the different targeted audiences: on line publication in a special section of the ISS website named “ISS per COVID-19” [https://www.iss.it/en/coronavirus] from which they are freely downloadable; delivered to specific mailing list of local authorities; delivered to specific associations; communicated by press release. In addition infographic sheets were prepared that could be used to have at a glance the information for the relevant users (e.g. people at home, operators for waste withdrawal, workers and managers at their working place). This communication activity is deemed to be one of the keystone activities to increase the awareness of the population on practical measures to contain spreading of the virus and risk prevention.
4. Conclusion
In view of the persistence of the SARS-CoV-2 on different surfaces and materials, waste generated by COVID-19 patients treated at home or subjects in quarantine at home or in special centres other than hospitals and medical centres, may represent a possible route for potential spreading of infection.
This awareness is highly perceived as a concrete risk by all the workers and also by the trained volunteers involved in this activity. Availability of clear and adequate procedures and methods able to avoid the potential risk of further contagious is strongly requested. According to this perspective the multidisciplinary working group, involving different stakeholders above the strictly health care ones (e.g. public administration, waste management companies, universities), of the Italian National Institute of Health (ISS) has delivered specific guidelines. Waste management through its different phases (i.e. delivery, collection, transport, disposal) can represent a further route for the spreading of the SARS-CoV-2 mainly by the contact with contaminated surfaces and objects. For this reason all the necessary cautions have to be taken to hinder the potential diffusion of the contagious virus proposing viable guidelines able to consider also the socio-economic conditions and the available technologies of the specific considered contexts. The multidisciplinary approach along with the involvement of main stakeholders resulted a winning approach.
CRediT authorship contribution statement
Francesco Di Maria:Methodology, Writing - original draft.Eleonora Beccaloni:Validation.Lucia Bonadonna:Writing - review & editing.Carla Cini:Supervision.Elisabetta Confalonieri:Supervision.Giuseppina La Rosa:Investigation.Maria Rosaria Milana:Writing - review & editing, Investigation.Emanuela Testai:Writing - review & editing, Investigation.Federica Scaini:Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors wish to thank Dr. Giusy Bonanno Ferraro for her valid contribution.
Editor: Damia Barcelo
References
- ACR+ Municipal waste management and COVID-19- phase 1. 2020. https://acrplus.org/en/municipal-waste-management-covid-19-phase1#international Available at.
- Anderson E.L., Turnham P., Griffin J.R., Clarke C.C. Consideration of the aerosol transmission for COVID-19 and public health. Risk Anal. 2020;40(5):902–907. doi: 10.1111/risa.13500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (Centers of Disease Control and Prevention) Coronavirus disease 2019 (COVID-2019) 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fsummary.html Available at.
- Chin A.W.H., chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.L., Chan M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe. 2020 doi: 10.1016/S2666-5247(20)30003-3. Correspondance. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruvinel V.R.N., Marques C.P., Cardoso V., Novaes M.R.C.G., Araújo W.N., Angulo-Tuesta A., Escalda P.M.F., Galato D., Brito P., da Silva E.N. Health conditions and occupational risks in a novel group: waste pickers in the largest open garbage dump in Latin America. BMC Public Health. 2019;581:16–19. doi: 10.1186/s12889-019-6879-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Maria F. Upgrading of a mechanical biological treatment (MBT) plant with a solid anaerobic digestion batch: a real case study. Waste Manag. Res. 2012;30(10):1089–1094. doi: 10.1177/0734242X12451306. [DOI] [PubMed] [Google Scholar]
- Di Maria F., Micale C. Impact of source segregation intensity of solid waste on fuel consumption and collection costs. Waste Manag. 2013;33:2170–2176. doi: 10.1016/j.wasman.2013.06.023. [DOI] [PubMed] [Google Scholar]
- Di Maria F., Sordi A., Micale C. Energy production from mechanical biological treatment and composting plants exploiting solid anaerobic digestion batch: an Italian case study. Energ. Conver. Manag. 2012;56:112–120. [Google Scholar]
- Di Maria F., Bidini G., Lasagni M., Boncompagni A. On time measurement of the efficiency of a waste-to-energy plant and evaluation of the associated uncertainty. Applied Thermal Energy. 2018;129:338–344. [Google Scholar]
- Ding, S., Liang, T.J. 2020. Is SARS-CoV-2 also an enteric pathogen with potential fecal-oral transmission: a COVID-19 virological and clinical review. Gastroenterology. S0016-5085(20)30571–0. [DOI] [PMC free article] [PubMed]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith M.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:12. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DPR. 2003. Decreto del Presidente della Repubblica 15 luglio 2003, n.254. Regolamento recante disciplina della gestione dei rifiuti sanitari a norma dell'articolo 24 della legge 31 luglio 2002, n. 179. (Regulation for the management of medical waste according to art. 24 of the legislation n. 179 of 31st July 2002). Official Journal of Italian Republic n. 211, 11.09.2003.
- EC Waste management in the coronavirus crisis. 2020. https://ec.europa.eu/info/sites/info/files/waste_management_guidance_dg-env.pdf Available at.
- Faridi S., Niazi S., Sadeghi K., Naddafi K., Yavarian J., Shamsipour M., Jandaghi N.Z.S., Sadeghiniiat K., Nabizadeh R., Yunesian M., Momeniha F., Mokamel A., Hassanvand M.S., MokhtariAzad T. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci. Total Environ. 2020;725:138401. doi: 10.1016/j.scitotenv.2020.138401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomes Mol M.P., Caldas S. Can the human coronavirus epidemic also spread through solid waste? Waste Management and Research. 2020;38(5):485–486. doi: 10.1177/0734242X20918312. [DOI] [PubMed] [Google Scholar]
- Gu J., Han B., Wang J. COVID-19: gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158:1518–1519. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller L., Mota C.R., Greco D.B. COVID-19 faecal-oral transmission: are we asking the right questions? Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindson J. COVID-19: faecal–oral transmission? Nat. Rev. Gastroenterol. Hepatol. 2020;17:259. doi: 10.1038/s41575-020-0295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis D. Is the coronavirus airborne? Experts can’t agree. Nature. 2020;580:175. doi: 10.1038/d41586-020-00974-w. [DOI] [PubMed] [Google Scholar]
- Liu Yuan, Ning Z., Chen Y., Guo M., Liu Yingle, Gali N.K., Sun L., Duan Y., Cai J., Westerdahl D., Env D., Liu X., Ho K.-F., Kan H., Fu Q., Lan K. 2020. Aerodynamic Characteristics and RNA Concentration of SARS-CoV-2 Aerosol in Wuhan Hospitals during COVID-19 Outbreak. bioRxiv. [DOI] [Google Scholar]
- Morawska L., Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council . The National Academies Press. National Academies Press; Washington, D.C: 2020. Rapid Expert Consultation on the Possibility of Bioaerosol Spread of SARS-CoV-2 for the COVID-19 Pandemic (April 1, 2020) [DOI] [Google Scholar]
- Nghiem L.D., Morgan B., Donner E., Short M.D. Case Studies in Chemical and Environmental Egineering. vol. 1. 2020. The COVID-19 pandemic: Considerations for the waste and wastewater services sector; p. 100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santarpia J.L., Rivera D.N., Herrera V., Morwitzer M.J., Creager H., Santarpia G.W., Crown K.K., Brett-Major D., Schnaubelt E., Broadhurst M.J., Lawler J.V., Reid S.P., Lowe J.J. 2020. Transmission Potential of SARS-CoV-2 in Viral Shedding Observed at the University of Nebraska Medical Center. medRxiv 2020.03.23.20039446. [DOI] [Google Scholar]
- Tobias A. Evaluation of the lockdown for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO COVID-19 2020 situation summary – updated 19 April 2020. 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html#covid19-pandemic Available at.
- WHO Coronavirus disease (COVID-19). Situation report 115. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200514-covid-19-sitrep-115.pdf?sfvrsn=3fce8d3c_6 Available at.
- WHO Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. 2020. https://www.who.int/publications-detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations Available at.
- WHO Laboratory biosafety guidance related to coronavirus disease 2019 (COVID-19) 2020. https://apps.who.int/iris/bitstream/handle/10665/331138/WHO-WPE-GIH- 2020.1-eng.pdf Available at.
- WIEGO Recommendations for the prevention of the spread of coronavirus disease (COVID-19) among solid waste workers. 2020. https://acrplus.org/images/project/Covid-19/COVID-19_Technical_Note_Waste_Pickers_WIEGO_2020_web1.pdf Available at.
- Windfeld E.S., Brooks M.S.L. Medical waste management – a review. J. Environ. Manag. 2016;163:98–108. doi: 10.1016/j.jenvman.2015.08.013. [DOI] [PubMed] [Google Scholar]
- de Wit E., van Doremalen N., Falzarano D., Munster V.J. SARS and MERS: recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016;14:523e34. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao F., Tang M., Zheng X. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158:1831–1833. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H., Afshar-Mohajer N., Theodore A.D., Lednicky J.A., Fan Z.H., Wu C.Y. An efficient virus aerosol sampler enabled by adiabatic expansion. J. Aerosol Sci. 2018;117:74–84. doi: 10.1016/j.jaerosci.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISS, 2020. Gruppo di Lavoro ISS Ambiente e Rifiuti. Indicazioni ad interim per la gestione dei rifiuti urbani in relazione alla trasmissione dell'infezione da SARS-CoV-2. Versione del 31 Maggio 2020. Roma: Istituto Superiore di Sanità; 2020. (Rapporto ISS COVI-19, n.3/2020 Rev. 2). Available at: https://www.iss.it/documents/20126/0/Rapporto+ISS+COVID-19++3_2020+Rev2.pdf/4cbaa7b5-713f-da61-2cac-03e5d3d155b3?t=1591277298239. (accessed 07.07.2020)