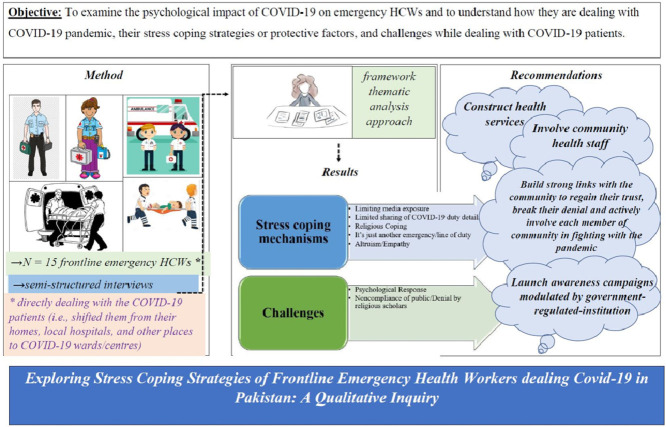
Graphical Abstract
Key Words: Coronavirus disease 2019, Epidemic outbreak, Frontline health workers, Qualitative study
Abstract
Background
The COVID-19 outbreak has gravely impacted the physical and psychological health of people. As the outbreak is ongoing, it is crucial to equip the emergency healthcare workers (HCWs) to be medically and psychologically prepared.
Objective
To examine the psychological impact of COVID-19 on emergency HCWs and to understand how they are dealing with COVID-19 pandemic, their stress coping strategies or protective factors, and challenges while dealing with COVID-19 patients.
Methods
Using a framework thematic analysis approach, 15 frontline emergency HCWs directly dealing with COVID-19 patients from April 2, 2020 to April 25, 2020. The semi-structured interviews were conducted face-to-face or by telephone. Data were analyzed using thematic analysis.
Results
Findings highlighted first major theme of stress coping, including, limiting media exposure, limited sharing of Covid-19 duty details, religious coping, just another emergency approach, altruism, and second major theme of Challenges includes, psychological response and noncompliance of public/denial by religious scholar.
Conclusions
Participants practiced and recommended various coping strategies to deal with stress and anxiety emerging from COVID-19 pandemic. Media was reported to be a principal source of raising stress and anxiety among the public. Religious coping as well as their passion to serve humanity and country were the commonly employed coping strategies.
Introduction
The beginning of 2020 brought a new challenge for the mankind the coronavirus disease 2019 (COVID-19). This virus, having origins in the Wuhan city, gradually spread throughout China and became a global health threat.1 , 2 So far, the COVID-19 is considered the largest outbreak of atypical pneumonia since the severe acute respiratory syndrome (SARS) epidemic which occurred in 2003.3 Contrary to the SARS, the total number of cases and death toll due to the COVID-19 became much higher following weeks of the initial outbreak.4 The epidemic was initially detected in December 2019, when number of pneumonia cases of unspecified etiology were noticed to be linked with epidemiologically related contact with a seafood market and untraced contacts in the city of Wuhan of Hubei Province.5 By late January 2020, the number of cases and death toll due to the COVID-19 escalated exponentially within and beyond Wuhan and spread to all 34 regions of China. Hence, based on the impact, the COVID-19 outbreak was declared by the World Health Organization (WHO) a public health emergency of global concern.6
In Pakistan, on February 26, 2020, the first case of COVID-19 was reported in Karachi.7 According to the Ministry of National Health Services Regulations & Coordination department of Government of Pakistan, the virus steadily spread to other regions of the country and within a span of few days, the confirmed cases due to COVID-19 rose to 56,386. However, 19,142 individuals recovered and there were 1,225 deaths due to this virus.8
Past studies have investigated the epidemiology and clinical characteristics of infected patients,9 , 10 the genomic features of the virus,11 and issues for global health governance.12 Presently, there is limited information related to the psychological impact and mental health of people during the COVID-19. Such an information is particularly significant amidst the ambiguity surrounding an epidemic of such an unmatched magnitude.
A study investigating psychological responses and associated factors during the initial stage of the COVID-19 in general public demonstrated moderate to severe psychological impact as well as moderate to severe depressive, stress, and anxiety symptoms.3 Availability of updated health information and particular precautionary measures were shown to be linked with reduced psychological impact of the outbreak and reduced levels of stress, anxiety, and depression.3
During the times of epidemics, most of the public health authorities and media predominantly are focusing on biological and physical consequences of the outbreak, thus, a reduced attention is paid to the mental health issues. Nevertheless, with the growing mental health burden during the COVID-19 epidemic, the calls for improved mental health support have escalated. For instance, in China, thorough guidelines for emergency psychological crisis intervention for people influenced by COVID-19 were issued by the National Health Commission on 27 January.13 These guidelines stressed the need for multidisciplinary mental health teams to provide mental health services to patients and Health Care Workers (HCW).
As the outbreak is ongoing, it is crucial to equip the health care systems and the general public to be medically and psychologically prepared.14 Past studies have shown that HCWs (eg, paramedics, ambulance personnel, and other HCWs) who were at high risk of exposure of infectious disease outbreak exhibited extreme stress, were emotionally influenced and traumatized, and had extreme levels of symptoms of depression and anxiety.15 This is anticipated because the anxiety and fear of being infected is greater with the risk of exposure. There may also be a fear of transmitting infection to their significant others. In majority of HCWs, conflicts and dissonance were shown to emerge as a result of trying to balance professional responsibility, altruism and personal fear for oneself and others.16
A higher susceptibility of developing adverse psychiatric issues has been shown in HCWs serving in emergency departments, intensive care units, and isolation wards compared to those working in other departments, probably because they are directly exposed to the infected patients, and their work is more challenging.17 Likewise, it was shown that as compared to married professionals and nurses; doctors and single professionals were more vulnerable to psychiatric issues.18 A current systematic review on the influence of disaster on mental health of HCWs showed absence of social support and communication, maladaptive coping, and absence of training as common risk factors for developing psychiatric issues.17
Although isolation strategies (eg, social distancing) are adopted globally to minimize the spread of the COVID-19, such strategies are only assisting in protecting lives. Isolation may add to the stress and is very likely to cause psychiatric issues.19 The past evidence from Cognitive Behavior Therapy paradigm emphasizes the need to build resilience.20 Resilience is the ability of a person to recover swiftly from hardships and people using positive emotions in difficult situations have been found to be resilient.21 Past literature shows that extremely resilient people foster their positive emotions which assist them in dealing with stress, boredom, and change.21 Resilience helps in coping with mental and physical health issues, thus, it can act as a protective factor against the onset of psychiatric issues among those facing hardships.22 , 23 Similarly, a systematic review demonstrated negative relationship between resilience and common mental disorders and an association of resilience with health promoting behavior and quality of life.24 However, there is limited knowledge about factors that buffer the negative impact of perceived severity on frontline emergency HCWs’ mental health. Based on the risk-resilience model,25 it is proposed that self-control (ie, a person's ability to reverse or change inner reactions and to suspend undesired behavioral tendencies) may act as buffer against the negative influence of perceived severity of the COVID-19 and mental health problems among people.26
The COVID-19 outbreak has gravely impacted the physical, psychological health and lives of people. It has resulted in various psychiatric issues, for instance, panic disorder, anxiety, and depression. However, no research articles have examined the psychological impact of COVID-19 on the emergency healthcare workers in Pakistan so far; a country having steadily rising confirmed cases and deaths.27 Additionally, the HCWs in Pakistan have been reported to be ill-equipped to deal with the COVID-19.28 Hence, the main purpose of the present study is to understand how emergency healthcare workers are dealing with COVID-19 pandemic, and what are their stress coping strategies or protective factors against stress eventually contributing to their mental health, and challenges they are facing while dealing with COVID-19 patients. This study will, consequently, offer a concrete basis for adapting and executing appropriate mental health intervention policies to cope with this challenge efficiently and effectively. This may help government bodies and healthcare professionals in preserving the psychological wellbeing of the HCWs in the face of COVID-19 outbreak in Pakistan and various parts of the world.
Methods
Research design
This qualitative inquiry used framework thematic analysis approach and made an initial attempt to explore COVID-19 related protective factors and coping mechanisms among emergency frontline HCWs in Pakistan. Thematic analysis is an interpretive procedure, in which data is methodically examined to find patterns within the data to offer a revealing account of the phenomenon.29 This method helps in forming meaningful themes without clearly creating theory.30 This method has been used to generate rich and comprehensive conception of complex phenomena.31 Both authors independently read data multiple times to extract and code any themes related to the research objective.
Participants
Through the convenience sampling method, 15 frontline emergency HCWs directly dealing with COVID-19 patients were recruited between April 2, 2015 and 25 April 2020. Advertisements to recruit participants were shared on different social networking sites. The inclusion criteria included (1) frontline emergency HCWs who directly dealt with the COVID-19 patients (ie, shifted them from their homes, local hospitals and other places to COVID-19 wards/centers), and (2) volunteers who participated in the study. The exclusion criteria were not consenting to participate or withdrawing from the study during the conduction of interview or one week after the interview. Initially, 20 participants consented to be part of the study, however, 5 of them refused due to some personal reasons. The final sample consisted of 15 participants (Table 1 ) who were ensured of the confidentiality and anonymity. The rapport building sessions comprised of sharing purposes of the study with participants before interviews.
Table 1.
Showing participant characteristics (N = 15)
| Participant No. | Age | Designation | Gender | Qualification | Years in Service |
|---|---|---|---|---|---|
| P1 | 29 | Emergency Medical Technician | Male | Higher Secondary + Diploma | 5 |
| P2 | 33 | Emergency Medical Technician | Male | Bachelors degree | 7 |
| P3 | 32 | Emergency Medical Technician | Male | Masters degree | 8 |
| P4 | 32 | Emergency Ambulance Driver | Male | Secondary | 5 |
| P5 | 30 | Emergency Medical Technician | Male | Higher Secondary | 7 |
| P6 | 33 | Emergency Medical Technician | Male | Higher Secondary | 8 |
| P7 | 36 | Emergency Ambulance Driver | Male | Secondary | 10 |
| P8 | 34 | Emergency Ambulance Driver | Male | Secondary | 8 |
| P9 | 28 | Emergency Medical Technician | Male | Higher Secondary + Diploma | 4 |
| P10 | 30 | Emergency Medical Technician | Male | Higher Secondary + Diploma | 5 |
| P11 | 29 | Emergency Medical Technician | Male | Bachelors degree | 4 |
| P12 | 34 | Emergency Medical Technician | Male | Bachelor degree + Diploma | 6 |
| P13 | 38 | Emergency Medical Technician | Male | Higher Secondary + Diploma | 12 |
| P14 | 32 | Emergency Medical Technician | Male | Higher Secondary | 7 |
| P15 | 28 | Emergency Medical Technician | Male | Higher Secondary | 2 |
Interview outline
The outline of interview protocols was designed by going through past literature, discussing with experts of qualitative research as well as conducting some preinterviews with frontline HCWs. The interview protocols also included probes for the actual question (ie, how do you see the COVID-19 in Pakistan/what is your perception about the COVID-19 in Pakistan?). The interviews were conducted in a national language (ie, Urdu) of Pakistan in which the researcher and participants both were comfortable in sharing their perspectives.
Data collection
The qualitative interviews were conducted after participants read and understood the explanatory statements as well as signed written informed consents. The interviewer possessed a PhD in Psychology degree with ample experience in qualitative interview and had worked on numerous qualitative research projects on resilience and protective factors of various communities. Additionally, the interviewer was a well-versed clinical psychologist with almost 10 years’ experience of evidence-based practice, teaching, and scientific research. Hence, the researcher was able to conduct this research.
The locations of conducting interviews were chosen based on the ease and convenience of each participant. A relaxed setting, comprising 2 chairs and a small table between each participant and interviewer, was maintained. The interviews were recorded, which were kept strictly confidential. Additionally, personal space was ensured to listen to participants clearly without interfering in their space. The room where interviews were conducted quiet, had minimal distractions, sufficient lightning, and adequate temperature. The emergence of similar responses after 15 interviews showed acquisition of data saturation, hence, no further interviews were conducted. Each interview took approximately one hour.
Additionally, participants were requested to pause interview and take a break or prevent further interviews in case they experienced emotional distress/discomfort during the interview. In case of emotional distress/discomfort, they were provided a list of counselling services which provided free of cost psychological help, however, none of the participants displayed any distress. Participations in this study was voluntary and participants were under no obligation. They could draw from the study from it began, during the interviews were conducted or one week after the data had been collected. The researchers maintained an unbiased stance while conducting interviews and kept amiable relationship with the participants. Before conducting actual interview with each participant, 1 or 2 rapport building sessions were conducted.
Data analysis
After recording interviews, transcription process began, and the data were subsequently analyzed through thematic analysis approach.
Transcription
Braun and Clarke31 have recommended various ways of transcription based on the analytical methods. Orthographic transcription was done, and it consisted of a “verbatim” account of all verbal as well as nonverbal expressions. Hence, all the verbal, and nonverbal responses were written down. Analysis were performed by both authors independently. They read the transcript multiple times, condensed, and obtained meaningful statements, and devised the themes and sub-themes. The discrepancies between both authors were settled through mutual discussion and a consensus was reached. This process was done independently of findings from any past studies. To analyze data as well as to maintain anonymity of participants, numbers were assigned to each participant.
Ethical review
The study was conducted in accordance with the Ethical Standards of the 1964 Helsinki Declaration and its Later Amendments or Comparable Ethical Standards. Written informed consent was obtained from all participants as well as participants consented for the findings to be published. Additionally, formal approval was taken from the concerned authorities for data collection. The authors ensure that there was no academic misconduct such as plagiarism, data fabrication, falsification, and repeated publication.
Results
The sample comprised of 15 males between 28 and 38 years of age with a mean age of 31.87 ± 2.82. The working experience ranged from 2 to 12 years with a mean of 6.53 ± 2.44. The minimum qualification of the participants was a secondary school certification. Table 1 shows the participants’ characteristics.
This qualitative inquiry aimed at exploring the psychological impact of COVID-19 on emergency HCWs and understanding how they dealt with COVID-19 pandemic, their stress coping strategies or protective factors against stress, and challenges. Themes presented in Figure 1 reflect the most repeated themes drawn from the responses of the participants (Fig 1).
Figure 1.
Showing theme chart.
Stress coping mechanisms
Limiting media exposure
Participants reported that one of the major elements of stress is prolonged exposure to news and social media. They shared that news create panic and unreliable sources of breaking news related to COVID-19 are prevalent everywhere. Additionally, they suggested limiting the exposure to media/news and practiced the same with their families. Participant 3 shared his views: “Another problem is the hype created by media and social media about coronavirus, I am not denying the severity of the problem, but checking social media repeatedly aggravates anxiety and I have now limited this exposure to get breaking news and asked my children also not to be obsessed with news updates, as I am not sure the source of the message/news.”
P5 shared: “It is much challenging these days to differentiate the actual facts from the fake news and media is bombarded with both, it's wise to rely on established sources for information regarding COVID-19. I Initially I used to check news and updates on social media almost every hour, since I have limited this exposure, I am feeling better.”
Limited sharing of COVID-19 duty details
Participants also highlighted their significant coping mechanism of not revealing detailed information regarding the duties they have performed in dealing with COVID-19 patients. Participants believed that sharing of such information may increase vulnerability of their significant others and exacerbate their anxiety and fear related to COVID-19.
P2 shared: “my utmost effort, to reveal the minimal information to my family regarding my exact duty of dealing with coronavirus patients, in my opinion is beneficial in dealing their existing stress.”
P12 shared: “If I reveal that how many hours, I am engaged in dealing/shifting the coronavirus patients, my family may get sick with the fear and it will increase their stress.”
P11 shared: “I have only shared with my wife that I am engaged in dealing with coronavirus patients but no in much details, and I regret to share because I know it is very stressful and alarming for her, but my do not know any details about my current duty.”
Religious coping
An important theme extracted from the data is religious coping. Considering the data from Muslim participants, religious coping was one of the significant themes. The faith-based practices and belief system is seen to play an integral role in lives of the selected sample to cope with the pandemic of COVID-19. Some of the excerpts are shared:
According to P10: “My coping is based on my faith that every disease/illness/virus comes from God and it cannot harm us without His will, so coronavirus is no exception. I know I have to take precautionary measures and I do that but ultimately believing that this virus too is a test from God, helps me cope better and I feel relaxed when I remind this to myself.”
Similarly, P4 said “Let's recall the verses from the holy Quran ‘every soul will taste death’ I think it's actually the fear of death that is associated with this pandemic and according to my belief system day for death is fixed by God for every individual, so I do not have much choice here and I know I could die without this virus and even could survive after getting diagnosed with it, so I rest my case to God and do not fear it and try to focus on my duty with this attitude of helping others during this tiring times.”
P1 shared: “I believe coronavirus is a wrath from God and it is the time to consult Him more for forgiveness, this makes me sad but remembrance of God while performing this challenging duty gives me strength and courage and it's a coping for me to manage my own stress.”
According to P5: “Fear of God is better than Fear of corona.”
This is a noteworthy theme reflecting the high regard of religious values and faith among participants. Since, the participants are using religious coping and put emphasis on their faith in order to deal with challenging situations such as pandemic, it can be concluded that faith/religion could be an element of resilience for the selected participants and served as protective factor.
It is just another emergency/line of duty
Some of the participants shared their coping of dealing with COVID-19 related stress by conceptualizing it as just another emergency, as they are trained for a wide range of emergencies. They seemed to normalize their stress by recalling their nature of duty and reminding themselves that it is not the first time they have dealt with threatening events.
P13 shared: “We are emergency health workers and provide emergency ambulance services too, so it is nothing new for me except the fact that we need some additional precautionary measures of wearing personal protective equipment's (PPE).”
P12 shared: “Yes, no doubt this pandemic situation and dealing directly with coronavirus patients is threatening and anxiety provoking but I think it's all related to how you perceive it. I keep reminding myself that it is my duty to provide healthcare in emergencies and I am just performing the same duty which I am doing from past one decade.”
P2 shared: “It is my line of duty if I am overwhelmed with stress how would the rest of the people around me would cope. I tell myself and to all the coronavirus patients I deal that it is a temporary situation, and this too shall pass.”
The way participants neutralized/ normalized the actions of performing the special duties of dealing with Covid-19 patients and reflected their sense of responsibility in the quotes above, shows their motivation and professional attitude to not only fulfil their job responsibilities but also to serve humanity.
Altruism/Empathy
Most of the participants shared that their reasons to enter this profession of emergency health provider services was their passion to serve humanity and they have reflected empathetic attitude toward COVID-19 patients
P7 shared his thoughts: “My thoughts (while shifting a patient diagnosed or suspected with coronavirus) are always revolving around patient's family members, even when I am back from duty. I am an ambulance driver and I have shifted 12 patients so far from their homes to quarantine centers. When I arrived at their place to take them, I saw their family members crying and this indeed is a touching moment when there is uncertainty that whether the patients will be back to their family or not. I keep on ruminating that this could me my family too and this gives me the empathy to relate with their circumstances and I try to perform my duty with devotion.”
P9 shared his perspective: “I try to focus the positive aspect that I am serving humanity and my job is contributing to saving people's life.”
P13 shared: “My reason to join this service was my passion to do something for a greater cause, something for humanity and I think it is the high time to play my part and perform my duties with commitment.”
P15 shared: “Today I interacted with a family coming back from Iran, and they were tested positive for Covid-19 including their 5 years old daughter and we got instructions to transfer the child to children hospital alone and rest of the patients/family members to other field hospitals/quarantine centers. The child was crying, and she was too scary to get isolated and this was the time I could not control my feelings and I requested authorities to shift the mother and child in the same quarantine center. I also has a 5-year-old daughter and I related exactly.”
Challenges/Issues
Psychological response
The COVID-19 pandemic has affected almost every individual in the world, and it was expected to have more severe psychological impact on the frontline emergency workers. The participants shared mixed views; some reported to have exaggerated stress while dealing with COVID-19 patients while others reflected resilience and managed their emotions in an appropriate manner as shared in the previous set of themes. All the participants acknowledge fear and anxiety as common prevalent symptoms due to uncertain situations.
P5 shared his views: “Obviously, Stress is much prevalent among all, not only the front liners but also among public. My stress is related to my children, what if I take the virus home and transfer to my children, this is my major stress, though I am taking all the precautionary measures, but I also have concerns related to the quality of PPE provided.”
P1 shared: “My appetite and sleep cycle are disturbed since I am doing duty for quarantine center.”
According to P6: “The 4 days of the last week were bit relaxed as I did not deal any emergency but from past few days I have got very busy as I am regularly exposing to coronavirus patients and it is stressful, tension and stress never ends, once one is managed, next is there and this pandemic is getting scary day by day.”
As mentioned by P8: “I was not having any emotional problem while performing these duties but yesterday felt bad, I had to deal with a family diagnosed with coronavirus, it was a rich family lived in a porched area, they refused to get admitted to the quarantine center setup by the state and preferred famous private center/hospital but send their servant to the one which they refused for them. This class difference makes me angry.”
Noncompliance of public/Denial by religious scholars
Another theme extracted from the data is public's noncompliance with the instructions issued by the Government to fight COVID-19. According to participants, people were not abiding by the instructions and worsening the situation. The participants shared in following words:
P6 said: “People need more awareness to understand the severity of the problem, not showing compliance is a way of welcoming the virus.”
P8 shared: “If people cannot stay at home and follow the instructions all our efforts are in vein and we can never control the spread.”
According to P9: “It's not the case that I am hopeless about future, I am an optimistic person and I hope and pray that world will soon recover from this pandemic, but here in our country we can only win this battle against COVID-19 if public show compliance and stay home, unfortunately there is lack of awareness among masses.”
P13 said: “I belong to a rural village and people in my village are not worried about this pandemic because they are not aware about the severity and they are moving freely, we need more awareness campaigns specially for rural areas.”
As mentioned by P2: “Worldwide and even in Muslim countries mosques are closed and public gathering congregation for Friday prayer and other prayers are prohibited but here religious authorities/scholars are still in the state of denial.”
P14 further shared: “Religious scholars rather than denying the severity should get involve in educating themselves first and then educating masses about keeping a social distance and offering prayers at home during this pandemic.”
Discussion
This study was conducted to understand how emergency frontline HCWs in Pakistan directly dealing COVID-19 patients are interpreting their experiences and what stress coping strategies they are employing. The findings of thematic analysis revealed that participants practiced and recommended various coping strategies to deal with stress and anxiety emerging from COVID-19 pandemic. For instance, participants shared that media was a principal source of elevating stress and anxiety among the public. Additionally, it was revealed that there was no way to confirm the authenticity of updates or news shared across various media which was adding to the uncertainty in this pandemic. Findings of past studies have also shown the role of media in exacerbating mental health issues.32, 33, 34 Studies have also demonstrated the role of televised traumatic content among general public in developing distress posttraumatic psychopathology.35 Likewise, participants also disclosed limited details about their work schedules to protect their significant others from any distress or anxiety. This limited self-disclosure to prevent distress among significant others was also documented in studies conducted on patients with HIV.36, 37, 38
Religious coping, their passion to serve humanity and country were also frequently employed coping strategies. These findings resonate with previous literature on healthcare workers about commitment to their profession as a primary motivation to continue to work.39, 40, 41 In harmony with past studies, by attributing religious meaning to the COVID-19 pandemic, participants were strengthening their coping.42, 43, 44, 45 Additionally, in contrast to avoiding responsibilities as shown in past studies,41 , 46 participants in the present study were willing to perform their duties even amidst the COVID-19 outbreak and considered it as another emergency. In line with the past studies,47, 48, 49 participants’ willingness to respond in uncertain and insecure situation of COVID-19 were their beliefs in duty, positive opinions and views regarding their roles during the pandemic which also influenced their resilience and coping mechanisms.
Similar to past studies, participants of present study acknowledge some fear and anxiety due to uncertain conditions.50 , 51 However, resilience and managing emotions appropriately drove participants to continue working. Participants also shared their concerns about noncompliance of the public and revealed that such behavior from the community was worsening the scenario of country. Various findings on epidemic such as Ebola and SARS have also shown that different kinds of noncompliance hampered the ability of governments and healthcare departments to work efficiently in dealing with the epidemics.52 , 53 One of the reasons of this noncompliance as well as denial of severity of COVID-19 by religious scholars could be mistrust in government. Studies have shown that individuals who mistrusted in government were much less likely to abide by government-directed mechanisms formulated to deal with various epidemics.54, 55, 56, 57 Furthermore, some participants revealed lack of awareness about availability of mental health services especially in rural areas.
Based on these findings some recommendations are suggested. For instance, it is critical to construct not only health services but also strong links with the community, to regain their trust, break their denial and actively involve each member of community in fighting with the pandemic. The role of community health staff is very critical in this as they can link communities and health facilities.58 Additionally, it is crucial to build on HCWs prevailing coping strategies. Implementation research should be conducted to develop a better understanding of the role of peer networks in supporting health workers. Furthermore, there is a need of awareness campaigns modulated by government-regulated institutions.
Strengths
This study in one of the initial attempts to explore the coping mechanisms and challenges of frontline HCWs in Pakistan in relation to COVID-19. Most of the prevailing qualitative studies are retrospective in nature, contrarily, this study was conducted in earlier stage of pandemic. Additionally, instead of just conducting interviews directly, a few rapport building sessions were conducted with each participant to familiarize them with the interviewer as well as the purpose of the study. This resulted in a thorough comprehension of participants’ experiences. Contrary to the findings of past studies, the participants of present study demonstrated a variety of coping strategies/protective factors that were buffering against the challenges of COVID-19 pandemic.
Limitations
There are some limitations of this study. The study was carried out when the pandemic was ongoing and we were conscious of not distracting the participants from essential work, hence, interviews were often paused or interrupted because the participants had to attend some other emergency calls and duties. Due to qualitative nature of study, the findings lack generalizability, and only explore the perspectives of emergency frontline HCWs. Consequently, it cannot disclose other perspectives, such as those of other HCWs, administrators, community members, and patients. Furthermore, we were conscious of social/physical distancing guidelines enforced by the government, hence, focus group discussions could not be conducted. Sample was also kept small owing to the exploratory nature of the study. This study did not report findings of HCWs from private facilities who may have different experiences of the pandemic and different coping mechanisms, which need exploration. The study used thematic analysis approach; thus, it may not capture the in-depth analysis and only reported the themes analyzed for semantic and latent meanings. In similar future studies, a more in-depth approach such as phenomenology or grounded theory could be employed for additional linguistic analysis of the data.
Authors’ own reflections
Although the authors have prior experience of conducting qualitative studies and using multiple data collection methods including semi-structured interviews, focus group discussions, and ethnographic observation, the data collection during the pandemic was a challenging task, especially ensuring the social distancing and all the precautionary measures for the study participants as well as the research assistant collecting data. The authors recruited a research assistant who had an adequate experience of interviewing and working in the health sector; thus, a separate research gatekeeper was not required.
Conclusions
This study presented a thorough and in-depth understanding of how the frontline emergency HCWs are dealing with COVID-19 pandemic, their stress coping strategies, or protective factors, and challenges while dealing with COVID-19 patients through thematic analysis method. It was found that during the pandemic, media was mentioned to be a major source of exacerbating anxiety and stress levels of masses as authenticity of updates or news shared could not be ascertained. Furthermore, religious coping, passion to serve humanity and country, considering this pandemic just an emergency, as well as positive opinions, and views regarding their roles during the pandemic boosted their resilience and coping mechanisms. The findings suggest launching of massive and prolonged public awareness programs to improve the information of the general population, aiming on modes of transmission, and situation-specific preventive strategies along with tackling mistrust, myths, and misconceptions. Health systems strengthening should be promoted by providing frontline HCWs with essential information about available mental health services to improve their self-esteem, resilience, and capability of HCWs to respond to the pandemic. Additionally, findings serve as a reference and inspiration for future mental health research studies on resilience and need for resilience-based interventions, training and supportive for emergency healthcare workers in Pakistan and region. This may help government bodies and healthcare professionals in preserving the psychological wellbeing of the HCWs in the face of COVID-19 outbreak in Pakistan and various parts of the world.
Acknowledgments
We are thankful to the participants of our study for giving us their valuable time and participating in the study.
Footnotes
Funding Source: This research received no funding.
Conflicts of interest/Competing interests: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics approval: The study was conducted in accordance with the Ethical Standards of the 1964 Helsinki Declaration and its Later Amendments or Comparable Ethical Standards. Written informed consent was obtained from all participants as well as participants consented for the findings to be published. Additionally, formal approval was taken from the concerned authorities for data collection.
Research data for this article: The data that support the findings of this study are available from the corresponding author [FRC], upon reasonable request.
Code availability (software application or custom code): Not applicable.
Author Contributions: All authors (ie, F.R.C. and K.M.) have contributed equally to this work. F.R.C. conceived the idea of this paper, supervised the entire process, and added important intellectual content. KM contributed substantially in the manuscript write-up. K.M. extracted themes and F.R.C. rechecked the results of thematic analysis. All authors have also agreed to be accountable for all aspects of this manuscript in ensuring that questions related to the accuracy or integrity of any part of this manuscript are appropriately investigated and resolved.
References
- 1.Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in china. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10:1206. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nishiura H, Jung S-m, Linton NM, et al. The Extent of Transmission of Novel Coronavirus in Wuhan, China. J Clin Med. 2020;9:330. doi: 10.3390/jcm9020330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ. 2020;368:m408. doi: 10.1136/bmj.m408. [DOI] [PubMed] [Google Scholar]
- 7.Abid K, Bari YA, Younas M, Tahir Javaid S, Imran A. Progress of COVID-19 epidemic in Pakistan. Asia Pac J Public Health. 2020;4:154–156. doi: 10.1177/1010539520927259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.GoP, Coronavirus in Pakistan, 2020, Ministry of National Health Services Regulations & Coordination, Government of Pakistan. Available at: https://covid.gov.pk/. Accessed August 5, 2020.
- 9.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 13.National Health Commission of the People's republic of China. The guidelines of psychological crisis intervention for COVID-19 pneumonia. 2020. Available at:http://www.nhc.gov.cn/jkj/s3577/202001/6adc08b966594253b2b791be5c3b9467. Accessed April 6, 2020.
- 14.Patel A, Jernigan DB. Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak-United States, December 31, 2019-February 4, 2020. Am J Transplant. 2020;20:889. doi: 10.1111/ajt.15805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McAlonan GM, Lee AM, Cheung V, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52:241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 16.Tiong WW, Koh GC. Ethical considerations in the review of Singapore's H1N1 Pandemic Response Framework in 2009. Ann Acad Med Singapore. 2013;42:246–250. [PubMed] [Google Scholar]
- 17.Naushad VA, Bierens JJ, Nishan KP, et al. A systematic review of the impact of disaster on the mental health of medical responders. Prehospital Disaster Med. 2019;34:632–643. doi: 10.1017/S1049023X19004874. [DOI] [PubMed] [Google Scholar]
- 18.Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med. 2004;54:190–196. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rhodes KV, Lauderdale DS, Stocking CB, Howes DS, Roizen MF, Levinson W. Better health while you wait: a controlled trial of a computer-based intervention for screening and health promotion in the emergency department. Ann Emerg Med. 2001;37:284–291. doi: 10.1067/mem.2001.110818. [DOI] [PubMed] [Google Scholar]
- 20.Padesky CA, Mooney KA. Strengths‐based cognitive–behavioural therapy: a four‐step model to build resilience. Clin Psychol Psychother. 2012;19:283–290. doi: 10.1002/cpp.1795. [DOI] [PubMed] [Google Scholar]
- 21.Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol. 2004;86:320. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Färber F, Rosendahl J. The Association between resilience and mental health in the somatically Ill: a systematic review and meta-analysis. Deutsches Ärzteblatt Int. 2018;115:621. doi: 10.3238/arztebl.2018.0621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arnetz J, Rofa Y, Arnetz B, Ventimiglia M, Jamil H. Resilience as a protective factor against the development of psychopathology among refugees. J Nerv Ment Dis. 2013;201:167. doi: 10.1097/NMD.0b013e3182848afe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cal SF, Sá LRd, Glustak ME, Santiago MB. Resilience in chronic diseases: a systematic review. Cogent Psychol. 2015;2 [Google Scholar]
- 25.Masten AS. Ordinary magic: resilience processes in development. Am Psychol. 2001;56:227. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 26.Tangney J, Baumeister R, Boones A. High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. J Pers. 2004;72:271–324. doi: 10.1111/j.0022-3506.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- 27.WHO: Coronavirus disease 2019 (COVID-19). Situation Report – 72. 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200401-sitrep-72-covid-19.pdf?sfvrsn=3dd8971b_2. Accessed August 5, 2020.
- 28.Stratford C. Pakistan ill-equipped to fight COVID-19: healthcare workers. Al Jazeera. 2020 [Google Scholar]
- 29.Smith J, Firth J. Qualitative data analysis: the framework approach. Nurse Res. 2011;18:52–62. doi: 10.7748/nr2011.01.18.2.52.c8284. [DOI] [PubMed] [Google Scholar]
- 30.Tesch R. The Falmer Press; Hampshire, UK: 1990. Qualitative Research—Analysis Types and Software Protocols. [Google Scholar]
- 31.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 32.Shensa A, Sidani JE, Dew MA, Escobar-Viera CG, Primack BA. Social media use and depression and anxiety symptoms: a cluster analysis. Am J Health Behav. 2018;42:116–128. doi: 10.5993/AJHB.42.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McNaughton-cassill ME. The news media and psychological distress. Anxiety Stress Coping. 2001;14:193–211. [Google Scholar]
- 34.Keles B, McCrae N, Grealish A. A systematic review: the influence of social media on depression, anxiety and psychological distress in adolescents. Int J Adolesc Youth. 2020;25:79–93. [Google Scholar]
- 35.Bodas M, Siman-Tov M, Peleg K, Solomon Z. Anxiety-inducing media: the effect of constant news broadcasting on the well-being of Israeli television viewers. Psychiatry. 2015;78:265–276. doi: 10.1080/00332747.2015.1069658. [DOI] [PubMed] [Google Scholar]
- 36.Petrak JA, Doyle AM, Smith A, Skinner C, Hedge B. Factors associated with self‐disclosure of HIV serostatus to significant others. Br J Health Psychol. 2001;6:69–79. doi: 10.1348/135910701169061. [DOI] [PubMed] [Google Scholar]
- 37.Armistead L, Morse E, Forehand R, Morse P, Clark L. African-American women and self-disclosure of HIV infection: rates, predictors, and relationship to depressive symptomatology. AIDS Behav. 1999;3:195–204. [Google Scholar]
- 38.Simoni JM, Mason HR, Marks G, Ruiz MS, Reed D, Richardson JL. Women's self-disclosure of HIV infection: rates, reasons, and reactions. J Consult Clin Psychol. 1995;63:474. doi: 10.1037//0022-006x.63.3.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hewlett BL, Hewlett BS. Providing care and facing death: nursing during Ebola outbreaks in central Africa. J Transcult Nurs. 2005;16:289–297. doi: 10.1177/1043659605278935. [DOI] [PubMed] [Google Scholar]
- 40.Raven J, Wurie H, Witter S. Health workers’ experiences of coping with the Ebola epidemic in Sierra Leone's health system: a qualitative study. BMC Health Serv Res. 2018;18:251. doi: 10.1186/s12913-018-3072-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kollie ES, Winslow BJ, Pothier P, Gaede D. Deciding to work during the Ebola outbreak: the voices and experiences of nurses and midwives in Liberia. Int J Africa Nurs Sci. 2017;7:75–81. [Google Scholar]
- 42.Heaner G. Religion, law and human rights in post-conflict Liberia. Afr Hum Rights Law J. 2008;8:458–485. [Google Scholar]
- 43.Rabelo I, Lee V, Fallah MP, et al. Psychological distress among Ebola survivors discharged from an Ebola Treatment Unit in Monrovia, Liberia—a qualitative study. Front Public Health. 2016;4:142. doi: 10.3389/fpubh.2016.00142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.James PB, Wardle J, Steel A, Adams J. Post‐Ebola psychosocial experiences and coping mechanisms among Ebola survivors: a systematic review. Trop Med Int Health. 2019;24:671–691. doi: 10.1111/tmi.13226. [DOI] [PubMed] [Google Scholar]
- 45.Munawar K, Tariq O. Exploring relationship between spiritual intelligence, religiosity and life satisfaction among elderly Pakistani Muslims. J Relig Health. 2018;57:781–795. doi: 10.1007/s10943-017-0360-x. [DOI] [PubMed] [Google Scholar]
- 46.Zuger A, Miles SH. Physicians, AIDS, and occupational risk: historic traditions and ethical obligations. JAMA. 1987;258:1924–1928. [PubMed] [Google Scholar]
- 47.Barnett DJ, Thompson CB, Errett NA, et al. Determinants of emergency response willingness in the local public health workforce by jurisdictional and scenario patterns: a cross-sectional survey. BMC Public Health. 2012;12:164. doi: 10.1186/1471-2458-12-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Devnani M. Factors associated with the willingness of health care personnel to work during an influenza public health emergency: an integrative review. Prehospital Disas Med. 2012;27:551–566. doi: 10.1017/S1049023X12001331. [DOI] [PubMed] [Google Scholar]
- 49.Gee S, Skovdal M. The role of risk perception in willingness to respond to the 2014–2016 West African Ebola outbreak: a qualitative study of international health care workers. Glob Health Res Policy. 2017;2:21. doi: 10.1186/s41256-017-0042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khalid I, Khalid TJ, Qabajah MR, Barnard AG, Qushmaq IA. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clini Med Res. 2016;14:7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liao Q, Cowling BJ, Lam WW, Ng DM, Fielding R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: ten cross-sectional surveys. BMC Infect Dis. 2014;14:169. doi: 10.1186/1471-2334-14-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Claude KM, Underschultz J, Hawkes MT. Social resistance drives persistent transmission of Ebola virus disease in Eastern Democratic Republic of Congo: a mixed-methods study. PLoS One. 2019;14:e0223104. doi: 10.1371/journal.pone.0223104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Obenauer J, Rübsamen N, Garsevanidze E, Karch A, Mikolajczyk RT. Changes in risk perceptions during the 2014 Ebola virus disease epidemic: results of two consecutive surveys among the general population in Lower Saxony, Germany. BMC Public Health. 2018;18:628. doi: 10.1186/s12889-018-5543-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Blair RA, Morse BS, Tsai LL. Public health and public trust: survey evidence from the Ebola virus disease epidemic in Liberia. Soc Sci Med. 2017;172:89–97. doi: 10.1016/j.socscimed.2016.11.016. [DOI] [PubMed] [Google Scholar]
- 55.Salmon DA, Dudley MZ, Glanz JM, Omer SB. Vaccine hesitancy: causes, consequences, and a call to action. Vaccine. 2015;33:D66–D71. doi: 10.1016/j.vaccine.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 56.Whetten K, Leserman J, Whetten R, et al. Exploring lack of trust in care providers and the government as a barrier to health service use. Am J Public health. 2006;96:716–721. doi: 10.2105/AJPH.2005.063255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nuriddin A, Jalloh MF, Meyer E, et al. Trust, fear, stigma and disruptions: community perceptions and experiences during periods of low but ongoing transmission of Ebola virus disease in Sierra Leone, 2015. BMJ Glob Health. 2018;3 doi: 10.1136/bmjgh-2017-000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Legard R, Keegan J, Ward K. In: Ritchie J., Lewis J., editors. Sage Publications; London: 2003. [Google Scholar]