Abstract
Hand hygiene by washing with soap and water is recommended for the prevention of COVID-19 spread. Soaps and detergents are explained to act by damaging viral spike glycoproteins (peplomers) or by washing out the virus through entrapment in the micelles. Technically, soaps come under a functional category of molecules known as surfactants. Surfactants are widely used in pharmaceutical formulations as excipients. We wonder why surfactants are still not tried for prophylaxis or therapy against COVID-19? That too when many of them have proven antiviral properties. Moreover, lung surfactants have already shown benefits in respiratory viral infections. Therefore, we postulate that surfactant-based prophylaxis and therapy would be promising. We believe that our hypothesis would stimulate debate or new research exploring the possibility of surfactant-based prophylaxis and therapy against COVID-19. The success of a surfactant-based technique would save the world from any such pandemic in the future too.
Keywords: COVID-19, Peplomer, SARS-CoV-2, Spike glycoprotein, Surfactants
Introduction
The pandemic COVID-19 is spreading rapidly all over the world. At present, the search for a therapy to this viral disease is in a ‘to leave no stone unturned’ situation. Washing with soap is recommended for hand hygiene for preventing the spread of COVID-19. Interestingly, the damage to coronavirus spike proteins leads to the virus inactivation [1]. Soaps and detergents are classified under surfactants and are widely explained as damaging peplomers or spike proteins. Inactivation of the Ebola virus, a virus showing spike-protein mediated host attachment, by surfactant nanoemulsion is ideal support for this hypothesis [2]. Surfactants are approved and widely used as pharmaceutical inactive ingredients. Surfactants, including biosurfactants, have been known to have antiviral properties. But their potential in prophylaxis and therapy against COVID-19 is still not explored. Therefore, this hypothesis analyzes the possibility and speculates the use of surfactants against SARS-CoV-2 peplomers for the prophylaxis and treatment of COVID-19.
Hypothesis
Here we postulate that a simple surfactant-based gargle would be enough to stop the spread of this pandemic. In addition to gargle, surfactant-loaded throat paint, mouthwash, nasal drops, and eye drops could be used for prophylaxis. This would be particularly useful among high-risk categories and health workers. In addition to prophylaxis, we postulate that surfactant therapy would be beneficial in the treatment of COVID-19. Further, the use of surfactant against COVID-19 would prevent the spread of this disease.
Surfactant-based prophylaxis against COVID-19
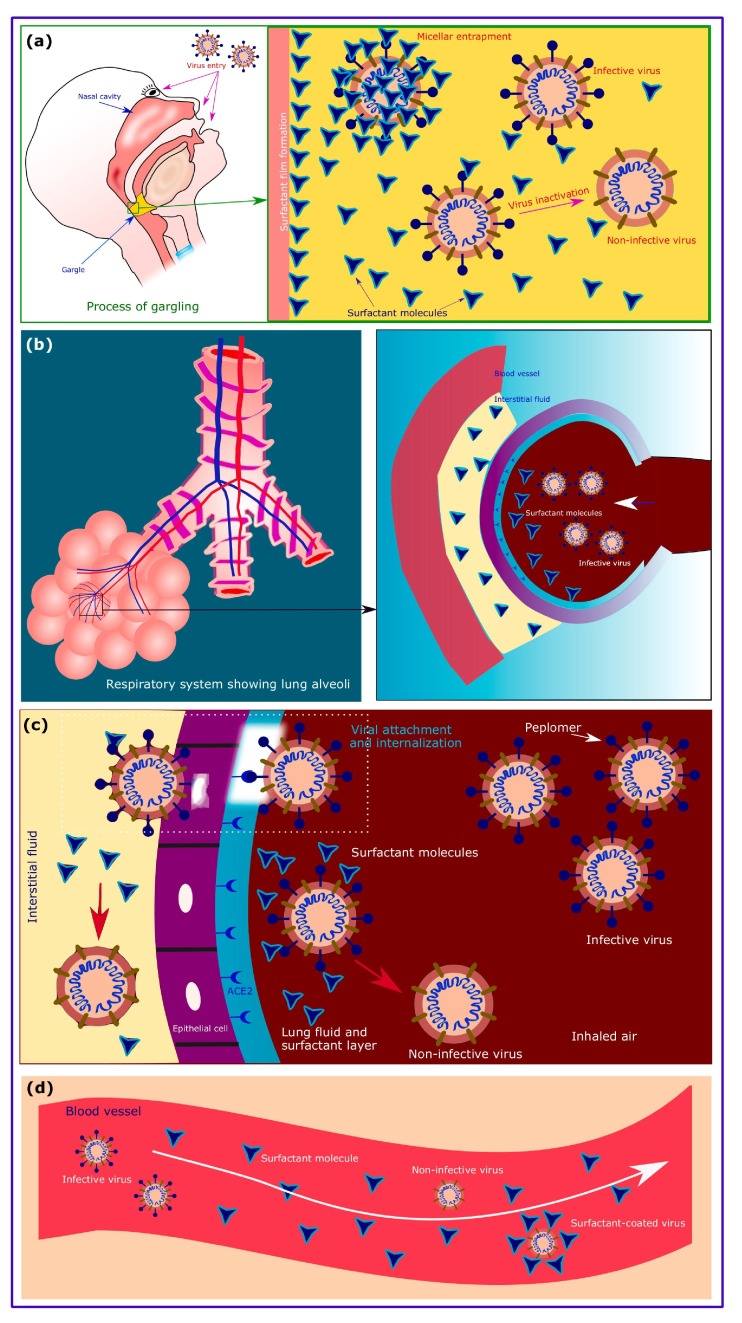
The major route of entry of SARS-CoV-2 is through nose and mouth, and to some extent through eyes. Throat (pharynx) is a common point of entry to the lungs from both mouth and nose. In the case of eyes too, it is described that the virus travels through the lacrimal and nasolacrimal ducts (the tear ducts) and then into the nose, throat, trachea, and finally lung [3]. Thus, any virus accidentally entered through mouth, nose, and/or eyes could be stopped/inactivated at the pharynx or nasopharynx with the use of a surfactant-based gargle (Fig. 1 a). Entrapment of viruses by surfactant micelles could also occur as a mechanism of inactivation. This would be possible when the critical micelle concentration (CMC) for a surfactant is achieved. Most surfactants have low CMC values. A high residence time of the virus in the pharynx would further enhance this prophylactic effect.
Fig. 1.
The diagrammatic presentations of the prophylactic and therapeutic applications of surfactants against COVID-19 (a) how the surfactant-based gargle prevents COVID-19; (b) entry of SARS-CoV-2 virus into lung alveoli; (c) action of surfactant on the SARS-CoV-2 virus. The figure shows the inactivation of the virus by the action of surfactant on viral spike glycoprotein. The surfactant present in the interstitial fluid could also render the virus non-infective. The insert shows the internalization of the virus at low surfactant concentrations; (d) action of surfactant in circulation. The surfactant either inactivates the virus or coats the virus and renders it inactive.
A gargle is a widely used dosage form for throat infections and pain. Most importantly, gargles are considered as external preparations which render a high level of flexibility in choosing the excipients and actives for their preparation. In addition to gargle, similar effects could be expected from surfactant-loaded throat paint, mouthwash, nasal drops, and eye drops. Throat paints even contain chemicals such as phenol and iodine. So a surfactant-based gargle or throat paint would not be of any concern. Most of the aspects mentioned for gargles apply to throat paints and mouthwash too. Among these, surfactant-loaded throat paints also provide good promise for the prevention of infection. Based on the convenience of using gargle compared to throat paint, the former would be most suitable for prophylaxis.
Inclusion of antiviral agents, proteases, astringents (protein precipitants), etc are some of the possible modifications to achieve additional benefits in gargles and mouthwashes. The addition of some protein precipitants such as tannic acid would have added benefit in preventing viral infection. Nevertheless, their interactions should be studied with the surfactant. Their interaction should not interfere with the ability of surfactants to inactivate the virus by interacting with the spike glycoprotein.
The inhalation route would also prove to be useful in the prophylaxis of COVID-19. Inhalation drug delivery devices are helpful in such delivery of surfactants [4]. Surfactants are already reported for pulmonary drug delivery [5], [6]. The use of surfactant in lung and tracheal infections without causing any damage to the cilia is also reported [7]. On systemic delivery, the surfactant reaches both interstitial fluid and lung alveoli. Now when a virus enters the lungs, it has to encounter these surfactant molecules (Fig. 1b). We believe that surfactant therapy will prevent the attachment of the virus through its spike glycoproteins. The surfactant present at the alveolar surface could interfere with the spike glycoproteins resulting in their destruction. This would help avoid the infection when in contact with the virus (Fig. 1c).
Surfactant therapy against COVID-19
Surfactant therapy is already in use for respiratory problems. It is reported that inhalation of lung surfactant improves respiratory diseases. The tremendous benefit of an artificial surfactant against the HINI virus has been proved in mice [8]. Also, surfactants have some role in innate host defense during infections [9]. Thus, it could be reasonably hypothesized that surfactant therapy would be promising in COVID-19 cases. A list of approved lung surfactants is presented in Table 1 [10], [11], [12].
Table 1.
Potential surfactants used in the pharmaceutical industry and approved for clinical use.
| Sl. No. | Name/class of surfactant | Present approved use | Approval details | [Ref.] |
|---|---|---|---|---|
| 1 | Lung surfactants – natural and synthetic [E.g.: colfosceril palmitate (Exosurf®), beractant (Alveofact®), poractant alpha (Curosurf®), calfactant (Infasurf®), lucinactant (KL4®), pumactant (Artificial Lung Expanding Compound or ALEC), and recombinant human surfactant protein C (Lusupultide, Venticute®)] | Respiratory distress syndrome in neonates. | USFDA approved lung surfactants | [10], [11], [12] |
| 2 | Polysorbate (non-ionic) | Approved inactive ingredient in intravenous, inhalation (respiratory), oral, nasal, ophthalmic, topical, and other formulations. Useful for external preparations too. | Included in the inactive ingredients database of USFDA. Included in Pharmacopoeia. | [22], [23], [24], [25] |
| 3 | Poloxamer (non-ionic) | Approved inactive ingredient in intravenous, inhalation (respiratory), oral, nasal, ophthalmic, topical, and other formulations. Useful for external preparations too. | Included in the inactive ingredients database of USFDA. Included in Pharmacopoeia. | [22], [24], [25] |
| 4 | Sodium lauryl sulfate (anionic) | Approved inactive ingredient in inhalation (respiratory), oral, topical, and other formulations. Useful for external preparations too. | Included in the inactive ingredients database of USFDA. Included in Pharmacopoeia. | [22], [24] |
| 5 | Cetrimide (cationic) | Pharmaceutical aid and bactericide. | Included in Pharmacopoeia. | [24], [25], [26] |
| 6 | Bile salt surfactants | Emulsifier and solubilizer. Used in combination with phospholipids in mixed micelles formulation. | Used in marketed formulations | [27], [28] |
| 7 | Phospholipids (zwitterionic) | Emulsifier and solubilizer. | Used in marketed formulations worldwide | [28], [29] |
| 8 | Vitamin E TPGS (semi-synthetic) | Solubilizer, absorption and permeation enhancer, and emulsifier. | Approved by USFDA. Included in Pharmacopoeia. | [24], [25], [30] |
| 9 | Polyoxyl 35 castor oil (semi-synthetic) | Emulsifying, solubilizing, and wetting agents. | Included in Pharmacopoeia. | [24], [25], [26] |
Lung surfactant is considered as a physiological barrier to viral infections. The lipid portion is mainly responsible for the antiviral activity [13], [14]. Inhibition of the H1N1 influenza virus is also possible with the lipid part [15]. Yet another advantage of lung surfactant phospholipids is their inhibition of virus-mediated inflammation and infection. Palmitoyl-oleoyl-phosphatidylglycerol has shown such activity [16]. Meanwhile, the antiviral activity of the protein part is also established [17]. Moreover, it is noteworthy that the lung surfactant protein has the ability for selective recognition of SARS coronavirus spike glycoprotein and subsequent macrophage activation [18].
Recently, the use of bear bile has been proposed against COVID-19 [19]. Bile contains bile salts that can function as surfactants [20]. We believe that these bio-surfactants present in the bear bile would have made a major contribution to the observed activity.
Now about the role of surfactant inside a cell, we postulate that the surfactant may reach the cells and the extracellular fluid. The surfactant would interfere with one or more steps of viral replication. Moreover, the spread of viruses from one cell to the adjacent one might be interrupted by the presence of a surfactant in the extracellular or interstitial fluid. This effect would be most important with the target site of SARS-CoV-2, the alveolar epithelial cell.
Surfactants against the spread of COVID-19
The next aspect or advantage of surfactant therapy is the prevention of virus spread. At first, let us consider the most common method of spread, the droplet contact transmission method. The presence of a surfactant near the cell membrane could interfere with the viral budding process by affecting the viral envelope formation. Each drop of the saliva of a patient could host millions of infective viruses which could be simply inactivated by the use of a surfactant-based gargle or mouthwash [21]. Now assuming the possibility of viral spread through blood, and possibly other body fluids too, the surfactant molecules in circulation would either coat the virus or destroy its peplomer and this renders it non-infective (Fig. 1d). Most importantly, these mechanisms could result in the loss of contagiousness of a patient. Therefore, we believe that surfactant-based methods could prevent the spread of this pandemic. Moreover, if we could demonstrate the utility of this method, it would be a solution to stop such viral infections in the future too.
A description on selected surfactants useful for the prophylaxis and/or therapy of COVID-19 is provided in the supplementary material along with other details regarding the validity of the proposed hypothesis.
Testing of the hypothesis
Two aspects should be studied to identify the potential of surfactant-based strategies against COVID-19. The first one is to identify the surfactant and its concentration or dose for its use. The critical micelle concentration would be the best point to start with for every surfactant. The second one is to check its safety profile for the intended use and route of administration. The in vitro studies would be sufficient for the primary screening of the surfactant and the required concentration or dose. A detailed study of the effect of surfactant on viral spike protein would be appropriate at this stage. Many surfactants are approved for pharmaceutical use as inactive ingredients and therefore issues related to safety will not be a concern (Table 1) [22]. The hypothesis may be tested under two categories. In one type of testing, the prophylactic action should be studied. In the other, therapeutic effect should be studied.
Conclusion
We believe that our hypothesis would stimulate debate or new research exploring the possibility of surfactant-based prophylaxis and therapy against COVID-19. The future and required clinical trials on surfactant-based therapeutics against COVID-19 would be further dependent on how this pandemic emerges in the future. It is presumed that this hypothesis would trigger some research in this unconventional approach against COVID-19.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors thank Prof. (Dr.) R. Chandni, Professor of Medicine & HOD of Emergency Medicine, Government Medical College, Kozhikode, India, for the valuable suggestions during the preparation of the manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mehy.2020.110081.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Sturman L.S., Ricard C.S., Holmes K.V. Conformational change of the coronavirus peplomer glycoprotein at pH 8.0 and 37 degrees C correlates with virus aggregation and virus-induced cell fusion. J Virol. 1990;64:3042–3050. doi: 10.1128/jvi.64.6.3042-3050.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chepurnov A.A., Bakulina L.F., Dadaeva A.A., Ustinova E.N., Chepurnova T.S., Baker J.R. Inactivation of Ebola virus with a surfactant nanoemulsion. Acta Trop. 2003;87:315–320. doi: 10.1016/S0001-706X(03)00120-7. [DOI] [PubMed] [Google Scholar]
- 3.Bitko V., Musiyenko A., Barik S. Viral infection of the lungs through the eye. J Virol. 2007;81:783–790. doi: 10.1128/JVI.01437-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ibrahim M., Verma R., Garcia-Contreras L. Inhalation drug delivery devices: technology update. Med Devices (Auckl) 2015;8:131–139. doi: 10.2147/MDER.S48888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin H.-R., Li Y.-S., Lin Y.-J. Novel microencapsulated Pluronic–chitosan nanomicelles for lung delivery. Colloid Polym Sci. 2016;294:1209–1216. doi: 10.1007/s00396-016-3879-6. [DOI] [Google Scholar]
- 6.Pellosi D.S., d’Angelo I., Maiolino S., Mitidieri E., di Villa D., Bianca R. In vitro/in vivo investigation on the potential of Pluronic® mixed micelles for pulmonary drug delivery. Eur J Pharm Biopharm. 2018;130:30–38. doi: 10.1016/j.ejpb.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Hashemi M.M., Holden B.S., Taylor M.F., Wilson J., Coburn J., Hilton B. Antibacterial and antifungal activities of poloxamer micelles containing ceragenin CSA-131 on ciliated tissues. Molecules. 2018;23:596. doi: 10.3390/molecules23030596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fukushi M., Yamashita M., Miyoshi-Akiyama T., Kubo S., Yamamoto K., Kudo K. Laninamivir octanoate and artificial surfactant combination therapy significantly increases survival of mice infected with lethal influenza H1N1 virus. PLoS One. 2012;7 doi: 10.1371/journal.pone.0042419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsieh I.-N., De Luna X., White M.R., Hartshorn K.L. The role and molecular mechanism of action of surfactant protein d in innate host defense against Influenza A virus. Front Immunol. 2018;9:1368. doi: 10.3389/fimmu.2018.01368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guttentag S., Foster C.D. Update in Surfactant Therapy. Neoreviews. 2011 doi: 10.1542/neo.12-11-e625. [DOI] [Google Scholar]
- 11.Jeon G.W. Surfactant preparations for preterm infants with respiratory distress syndrome: past, present, and future. Korean J Pediatr. 2019;62:155–161. doi: 10.3345/kjp.2018.07185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walther F.J., Gordon L.M., Waring A.J. Advances in synthetic lung surfactant protein technology. Expert Rev Respir Med. 2019;13:499–501. doi: 10.1080/17476348.2019.1589372. [DOI] [PubMed] [Google Scholar]
- 13.Perino J., Crouzier D., Spehner D., Debouzy J.-C., Garin D., Crance J.-M. Lung surfactant DPPG phospholipid inhibits vaccinia virus infection. Antiviral Res. 2011;89:89–97. doi: 10.1016/j.antiviral.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Glasser J.R., Mallampalli R.K. Surfactant and its role in the pathobiology of pulmonary infection. Microbes Infect. 2012;14:17–25. doi: 10.1016/j.micinf.2011.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Numata M., Mitchell J.R., Tipper J.L., Brand J.D., Trombley J.E., Nagashima Y. Pulmonary surfactant lipids inhibit infections with the pandemic H1N1 influenza virus in several animal models. J Biol Chem. 2020;295:1704–1715. doi: 10.1074/jbc.RA119.012053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Numata M., Chu H.W., Dakhama A., Voelker D.R. Pulmonary surfactant phosphatidylglycerol inhibits respiratory syncytial virus–induced inflammation and infection. Proc Natl Acad Sci. 2010;107 doi: 10.1073/pnas.0909361107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Eijk M., Hillaire M.L.B., Rimmelzwaan G.F., Rynkiewicz M.J., White M.R., Hartshorn K.L. Enhanced antiviral activity of human surfactant protein d by site-specific engineering of the carbohydrate recognition domain. Front Immunol. 2019;10:2476. doi: 10.3389/fimmu.2019.02476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leth-Larsen R., Zhong F., Chow V.T.K., Holmskov U., Lu J. The SARS coronavirus spike glycoprotein is selectively recognized by lung surfactant protein D and activates macrophages. Immunobiology. 2007;212:201–211. doi: 10.1016/j.imbio.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fobar R. China promotes bear bile as coronavirus treatment, alarming wildlife advocates. Natl Geogr Mag 2020. https://www.nationalgeographic.com/animals/2020/03/chinese-government-promotes-bear-bile-as-coronavirus-covid19-treatment/. [accessed March 31, 202].
- 20.Hofmann A.F., Mysels K.J. Bile salts as biological surfactants. Colloids Surf. 1987;30:145–173. doi: 10.1016/0166-6622(87)80207-X. [DOI] [Google Scholar]
- 21.Wang W.-K., Chen S.-Y., Liu I.-J., Chen Y.-C., Chen H.-L., Yang C.-F. Detection of SARS-associated coronavirus in throat wash and saliva in early diagnosis. Emerg Infect Dis. 2004;10:1213–1219. doi: 10.3201/eid1007.031113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.FDA. Inactive ingredients database download. Inactive Ingredients Database 2020. https://www.fda.gov/drugs/drug-approvals-and-databases/inactive-ingredients-database-download. [accessed May 4, 2020].
- 23.WHO. The International Pharmacopoeia 2019. https://apps.who.int/phint/en/p/docf/. [accessed May 5, 2020].
- 24.USP36-NF31. United States Pharmacopoeia and National Formulary. Rockville, MD: United States Pharmacopeial Convention; 2013.
- 25.Indian Pharmacopoeia. Eighth ed. Ghaziabad, India: The Indian Pharmacopoeia Commission; 2018.
- 26.Rowe R.C., Sheskey P.J., Owen S.C., editors. Handbook of Pharmaceutical Excipients. fifth ed. Pharmaceutical Press; London: 2006. [Google Scholar]
- 27.Hammad M.A., Müller B.W. Increasing drug solubility by means of bile salt–phosphatidylcholine-based mixed micelles. Eur J Pharm Biopharm. 1998;46:361–367. doi: 10.1016/S0939-6411(98)00037-X. [DOI] [PubMed] [Google Scholar]
- 28.Li J., Wang X., Zhang T., Wang C., Huang Z., Luo X. A review on phospholipids and their main applications in drug delivery systems. Asian J Pharm Sci. 2015;10:81–98. doi: 10.1016/j.ajps.2014.09.004. [DOI] [Google Scholar]
- 29.van Hoogevest P., Wendel A. The use of natural and synthetic phospholipids as pharmaceutical excipients. Eur J Lipid Sci Technol. 2014;116:1088–1107. doi: 10.1002/ejlt.201400219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang C., Wu T., Qi Y., Zhang Z. Recent Advances in the Application of Vitamin E TPGS for Drug Delivery. Theranostics. 2018;8:464–485. doi: 10.7150/thno.22711. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.