Abstract
Rationale and Objectives
Predictive models and anecdotal articles suggest radiology practices were losing 50%-70% of their normal imaging volume during the COVID-19 pandemic. Using actual institutional data, we investigated the change in imaging utilization and revenue during this public health crisis.
Materials and Methods
Imaging performed within the 8-week span between March 8 and April 30, 2020 was categorized into the COVID-19 healthcare crisis timeframe. The first week of this date range and the 10 weeks prior were used to derive the normal practice expected volume. A rolling 7-day total value was used for volume tracking and comparison. Total imaging utilization was derived and organized by patient setting (outpatient, inpatient, emergency) and imaging modality (X-ray, CT, Mammography, MRI, Nuclear Medicine/PET, US). The three highest volume hospitals were analyzed. Revenue information was collected from the hospital billing system.
Results
System-wide imaging volume decreased by 55% between April 7 and 13, 2020. Outpatient exams decreased by 68% relative to normal practice. Emergency exams decreased by 48% and inpatient exams declined by 31%. Mammograms and nuclear medicine scans were the most affected modalities, decreasing by 93% and 61%, respectively. The main campus hospital experienced less relative imaging volume loss compared to the other smaller and outpatient-driven hospitals. At its lowest point, the technical component revenue from main campus imaging services demonstrated a 49% negative variance from normal practice.
Conclusion
The trends and magnitude of the actual imaging utilization data presented will help inform evidence-based decisions for more accurate volume predictions, policy changes, and institutional preparedness for current and future pandemics.
Key Words: Imaging Utilization, COVID-19, Multimodality
Introduction
The COVID-19 pandemic has had an unprecedented effect on radiology practices nationwide. Since the World Health Organization officially labeled COVID-19 a global pandemic on March 11, 2020, both US federal and state policies rapidly evolved to curtail the spread of the virus (1,2). In addition to these policies, healthcare systems implemented further restrictions limiting the number of patients they serve to decrease risk of exposures. These restrictions, in combination with stay-at-home orders and a broader developing economic recession, resulted in a sharp and precipitous decline in demand for imaging services (3). Predictive models and anecdotal articles suggested that practices lost up to 50%-70% of their normal imaging volume during the surge phase of the pandemic; however, minimal real-world data have been published to confirm these figures (4,5).
The purpose of this study is to provide actual data for future evidence-based decisions regarding similar public health crises by quantifying the change in imaging utilization at our institution during an 8-week span amidst the COVID-19 pandemic.
Methods
Setting
This study was exempted by the Institutional Review Board and patient consent was waived. Our healthcare institution serves northeast Ohio including the Cleveland metropolitan area and its surrounding counties. It is an integrated healthcare system of over 150 locations, including 18 hospitals, more than 40 outpatient health centers, 11 urgent care centers, and numerous physician offices across the region (6). It serves a total of nine counties containing a population of nearly 3 million people, which makes up approximately 25% of the population of Ohio (7). Roughly 1.5 million people are concentrated within two major counties that contain the system's three largest hospitals. The West hospital serves the less populous Lorain county, while the Central and East hospitals both serve the more populous Cuyahoga county. The West hospital has 232 beds, the Central main campus hospital has 1032 beds, and the East hospital has 157 beds (6). In 2019, 1.3 million imaging exams were performed throughout the entire institution. Approximately 35% of these scans were performed at these three main hospitals, which were chosen as a representative sample of the general characteristics in imaging utilization throughout the system.
COVID-19
As of June 15, 2020, the number of confirmed cases in the United States has surpassed 2.2 million. This has led to 120,000 deaths with greater than 150,000 deaths predicted before the virus ultimately clears (8). In Ohio, over 43,000 COVID-19 cases have been confirmed resulting in over 7000 hospitalizations, 1800 intensive care unit admissions, and 2600 confirmed deaths. Compared to other states in the United States, Ohio has the 16th highest number of cases overall, 39th highest number of cases per capita, and the 19th highest number of COVID-related deaths. The nine counties served by our institution have seen over 9800 of these cases. Cuyahoga county, which makes up 57% of the population of this nine-county fingerprint, reported 55% of these cases and contains the second highest number of COVID-19 cases of any county in the state of Ohio (8,9).
The major events and policy changes used to anchor the relative chronology of imaging utilization change include:
-
1.
March 9, 2020, when Ohio was officially placed into a state of emergency after the first three positive cases of COVID-19 were confirmed.
-
2.
March 15, 2020, when restaurants and bars were ordered closed.
-
3.
March 17, when elective and nonessential procedures were to be postponed in an effort to conserve personal protective equipment (PPE).
-
4.
March 22, 2020, when the official stay-at-home order was implemented.
-
5
May 1, 2020, when healthcare services were permitted to resume operations with the exception of those requiring overnight hospitals stays (2).
Imaging Utilization
Data were obtained from a business intelligence and analytics platform that aggregates data primarily from the Radiology Information System and Picture Archiving and Communication System to construct performance statistics by analyzing all radiologist-generated reports (3M M*Modal Scout, Pittsburgh, PA) (10). The absolute number of accession numbers created was used to estimate the total number of exams performed. The platform aggregated a list of all accession numbers associated with diagnostic radiologist reports completed between January 1, 2020 and April 30, 2020 throughout the institution. This list of over 350,000 accession numbers were exported and organized by exams completed per day. Approximately 3% of the exams were excluded since they were not categorized as completed in inpatient, outpatient or emergency department (ED) settings. An aggregated 7-day total was used as a measure of weekly imaging volume due to the large variance between the number of exams performed during weekdays versus weekends. This value was used as the main basis of image utilization volume tracking and comparison.
The system-wide number of completed exams for all modalities (X-ray, CT, Mammography, MRI, Nuclear Medicine/PET, US) was then tracked and charted chronologically. A normalized average weekly volume was derived using the 7-day aggregate from January 2020 to mid-March 2020. This weekly system-wide total utilization was superimposed on the aforementioned timeline of major events and policy decisions to qualitatively and quantitatively evaluate the connection between policy changes and imaging utilization. The COVID-19 confirmed cases data timeline was juxtaposed on this chart.
Subsequently, the overall imaging utilization was categorized by patient type, which exhibited exams completed in the inpatient, outpatient, and ED settings. The imaging utilization trends from each of these three main patient groups were charted chronologically. Separately, the overall utilization was also categorized by imaging modality. Exams that were not classified into these imaging modalities were excluded from this portion of the analysis (Angiograms, Fluoroscopy, and accession numbers without images). For trend comparison, the 7-day aggregate volume data from January 2019 to mid-March 2019 were similarly extracted and graphed chronologically by total utilization and by patient type.
Finally, the West, Central, and East hospitals, as the three largest medical centers spread out over two adjacent counties, were analyzed by total imaging utilization, patient type, and modality as above.
Results
Total Volume
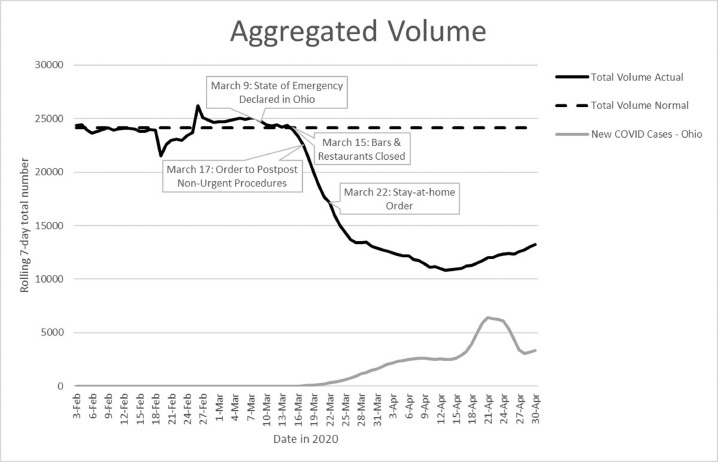
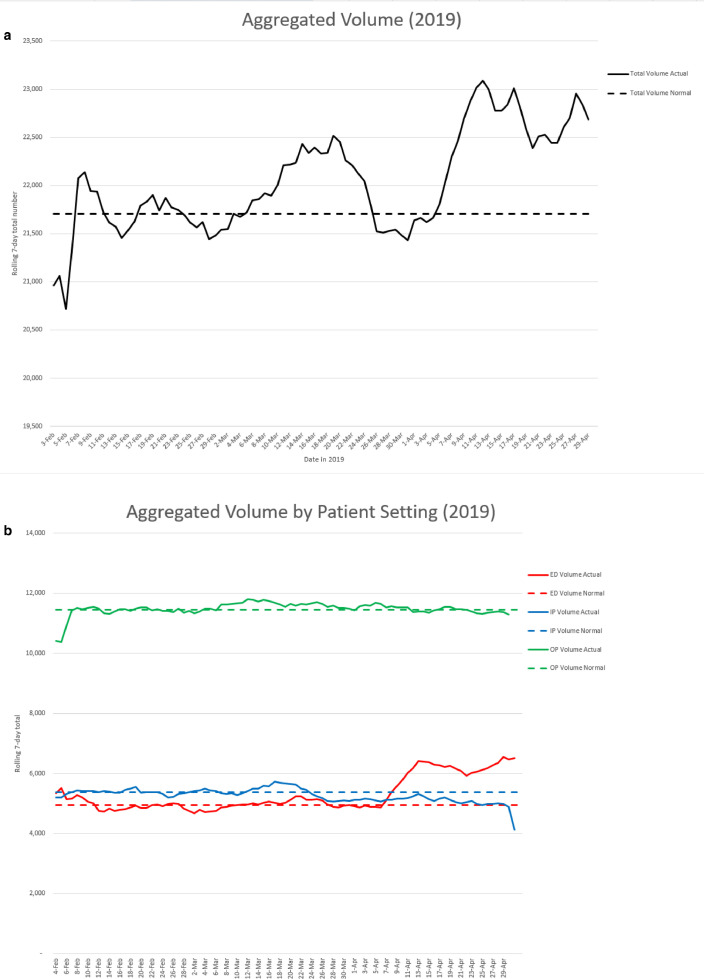
Figure 1 shows our system-wide imaging volume hit a 7-day total trough of 55% decrease from expected average between April 7 and April 13. Key policy dates are displayed on the actual volume series and show that volume began to decline rapidly immediately after the state of Ohio declared a state of emergency. The superimposed graph of the new COVID-19 cases shows a peak rolling 7-day total of 6445 new cases on April 21, which occurred about a week after the aforementioned imaging volume trough. To compare utilization trends, Figure 2 a demonstrates the aggregate 2019 volume. Imaging utilization in the system actually increased during this same 2019 timeframe transitioning from winter to spring, thus supporting the idea that the 2020 volume loss was due entirely due to the COVID-19 pandemic.
Figure 1.
The rolling 7-day total number of imaging exams performed in the Northeast Ohio healthcare institution between February 3, 2020 and April 30, 2020. The dashed horizontal line represents the normalized/average number of total exams performed over a 7-day period between February 3, 2020 and March 14, 2020. The rolling 7-day total of new COVID cases in the State of Ohio is also shown.
Figure 2.
The rolling 7-day total number of imaging exams performed cumulatively in the Northeast Ohio health system between February 3, 2019 and April 30, 2019 (a) cumulatively, and (b) by each patient setting of ED, inpatient, and outpatient. The dashed horizontal line represents the normalized/average number of total exams performed over a 7-day period between February 3, 2019 and March 14, 2019.
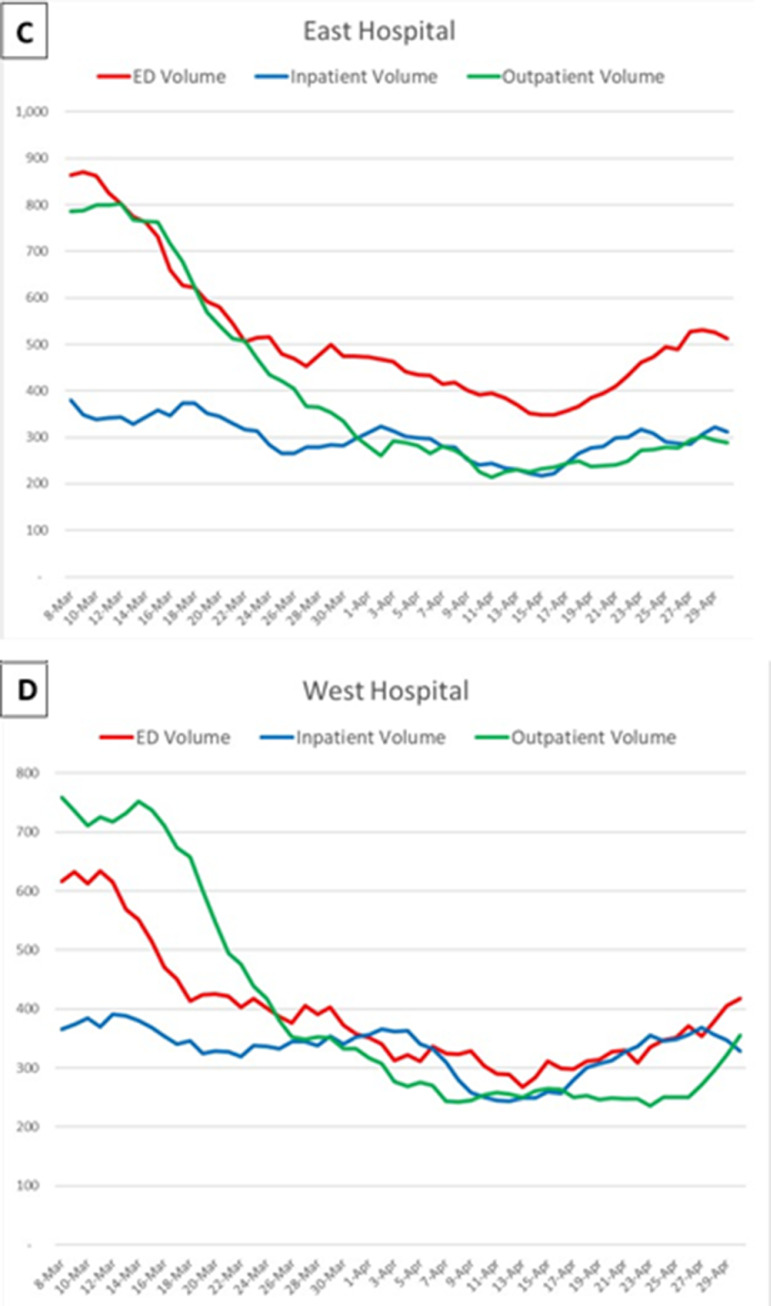
Volume by Patient Type
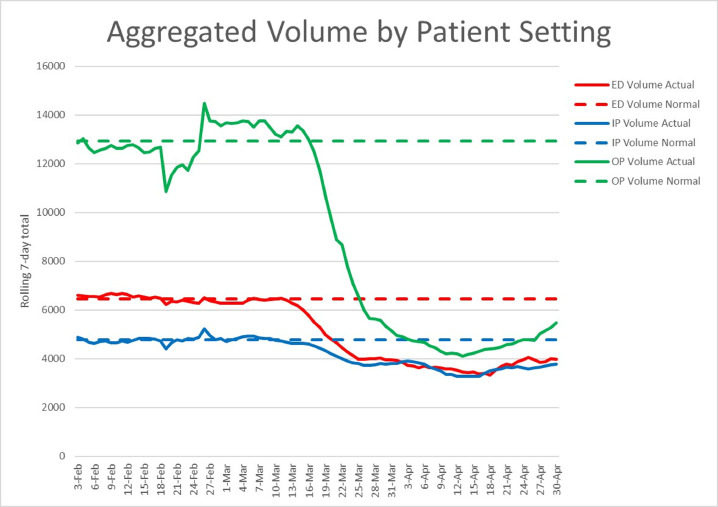
Similarly, Figure 2b demonstrates 2019 imaging utilization by patient setting; it is evident that imaging utilization did not significantly change from early February to the end of April in all three settings. Figure 3 then separates exams completed based on the inpatient, outpatient, and ED settings in 2020. In a normal practice, outpatient scans drive the majority of imaging volume, accounting for 54% of total exams. Inpatient and ED exams account for 20% and 27% of normal practice imaging volume, respectively. Outpatient volumes dropped most significantly by 68% during the April 7 to April 13 timeframe. Inpatient exams decreased the least by 31% compared to normal practice. Exams in the ED setting hit their lowest point during April 12 to April 18 with a decrease of 48% compared to normal practice. Figure 3 shows that the during the weeks encompassing the volume trough, imaging utilization from all three settings fell to a seven-day total between 3000 and 4000 exams.
Figure 3.
The rolling 7-day total number of imaging exams performed in each patient setting of ED, inpatient, and outpatient. The dashed horizontal lines represent the normalized/average number of total exams performed over a 7-day period for each patient setting.
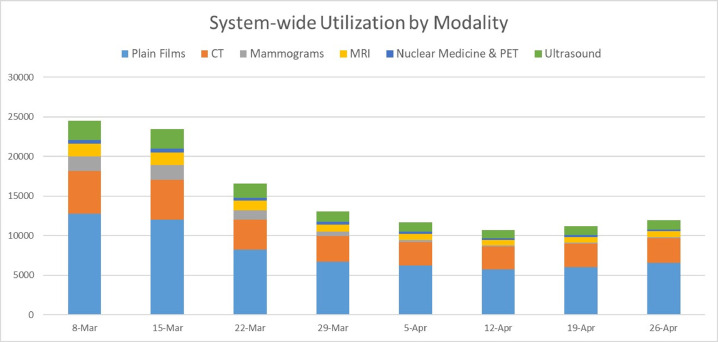
Volume by Modality
Figure 4 shows a consolidated aggregate of chronological change in imaging volume distributed by modality. Mammograms were most affected with imaging volume dropping by 93% between April 10 and April 16 relative to normal practice. Nuclear Medicine exams, which included PET, dropped by 61% relative to normal practice. Relative to normal practice, at their lowest point during the 8-week period, US exams decreased by 58%, MRI decreased by 56%, plain films decreased by 53%, and CT decreased by 47%.
Figure 4.
The 7-day total number of radiology exams performed in the health system broken down by the selected modalities of plain films, CT, mammograms, MRI, Nuclear Medicine (including PET) and Ultrasound. The modality proportions and total volume change is seen chronologically between March 8 and April 26.
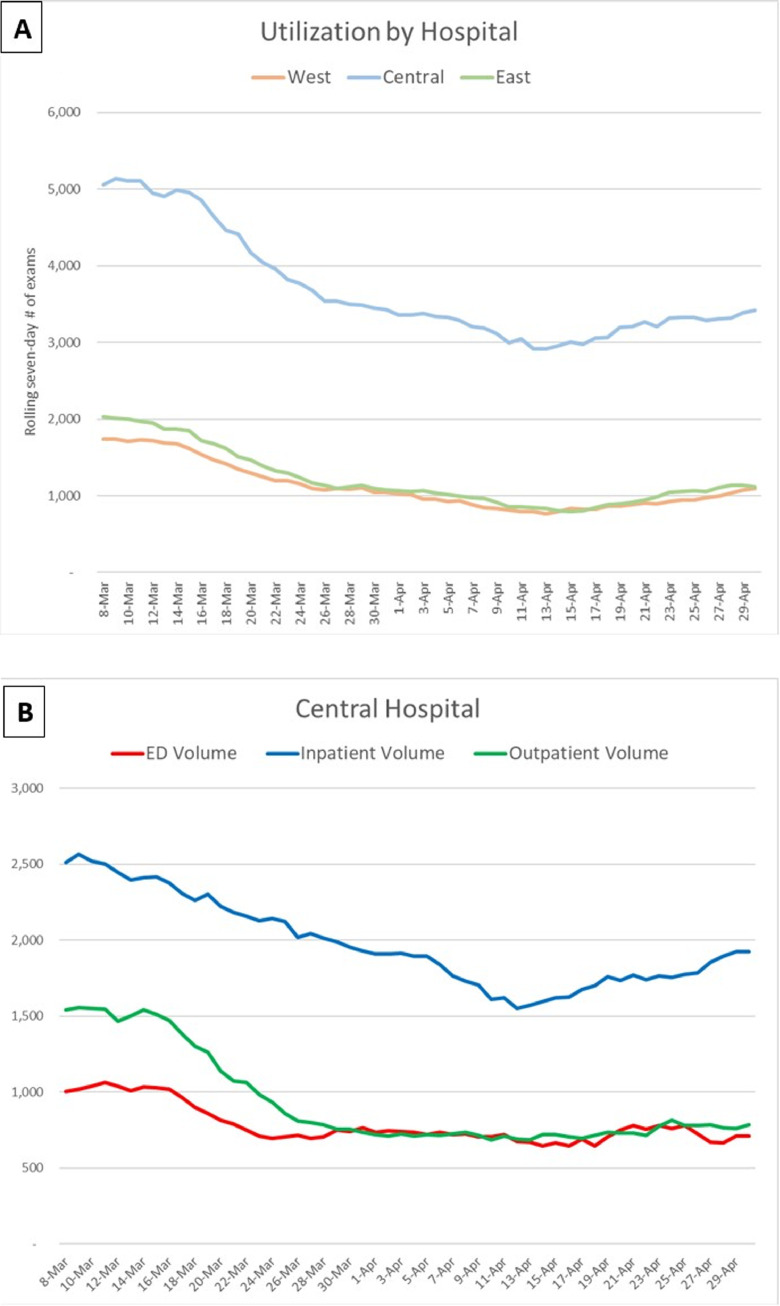
Volume by Site
When evaluated by hospital location, the Central main campus sees higher imaging volume compared to the other two regional East and West sites combined on a normal practice basis (Fig 5 ). Both of the smaller East and West hospitals dropped to approximately 800 exams per week whereas the main campus dropped to approximately 3000 per week. At its lowest point relative to normal practice, the Central main campus total volume decreased by 42%, inpatient imaging volume decreased by 36%, outpatient imaging volume decreased by 56%, and ED imaging volume decreased by 38%. At the East hospital relative to normal practice, total imaging volume decreased by 60%, inpatient imaging volume decreased by 46%, outpatient imaging volume decreased by 71%, and ED imaging volume decreased by 58%. At West hospital relative to normal practice, the total imaging volume decreased by 54%, inpatient imaging volume dropped by 39%, outpatient imaging volume dropped by 67%, and ED imaging volume dropped by 53%. In aggregate, the three largest hospitals in the institution combined experienced a 48% decrease in imaging volume.
Figure 5.
The three largest hospitals in the healthcare institution. (a) The rolling 7-day total number of imaging exams performed in each hospital is shown. (b–d) The Central, East, and West hospital imaging volumes are further separated by the three major patient settings, respectively.
When organized by modality, plain films and CTs continued to drive imaging volume at all three sites (Table 1 ). Studies such as nuclear medicine and mammograms dramatically decreased, especially in the predominantly outpatient-driven West hospital site.
Table 1.
West, Central, and East Rolling 7-Day Total Raw Hospital Volumes Are Compared During Each Week Between March 8 and April 26
| March 8 | March 15 | March 22 | March 29 | April 5 | April 12 | April 19 | April 26 | |
|---|---|---|---|---|---|---|---|---|
| West hospital | ||||||||
| CR | 786 | 709 | 569 | 546 | 450 | 364 | 429 | 520 |
| CT | 464 | 363 | 259 | 288 | 237 | 212 | 222 | 236 |
| MG | 99 | 83 | 67 | 39 | 13 | 4 | 10 | 9 |
| MR | 93 | 122 | 84 | 61 | 66 | 51 | 46 | 44 |
| NM + PET | 15 | 28 | 18 | 23 | 15 | 12 | 18 | 5 |
| US | 225 | 262 | 154 | 133 | 125 | 103 | 116 | 134 |
| Central hospital | ||||||||
| CR | 2757 | 2737 | 2112 | 1948 | 1774 | 1622 | 1690 | 1806 |
| CT | 1005 | 953 | 754 | 725 | 718 | 661 | 798 | 705 |
| MG | 123 | 119 | 71 | 18 | 13 | 17 | 10 | 9 |
| MR | 357 | 342 | 268 | 206 | 204 | 191 | 231 | 227 |
| NM + PET | 93 | 104 | 89 | 66 | 64 | 61 | 73 | 44 |
| US | 476 | 462 | 338 | 301 | 260 | 213 | 244 | 293 |
| East hospital | ||||||||
| CR | 864 | 772 | 532 | 464 | 431 | 378 | 403 | 435 |
| CT | 529 | 474 | 341 | 341 | 287 | 252 | 283 | 341 |
| MG | 142 | 114 | 72 | 53 | 39 | 17 | 11 | 17 |
| MR | 154 | 167 | 115 | 88 | 75 | 70 | 68 | 87 |
| NM +PET | 61 | 41 | 32 | 31 | 14 | 13 | 21 | 20 |
| US | 205 | 196 | 168 | 112 | 97 | 79 | 101 | 119 |
CR, plain films; MG, mammograms; NM, nuclear medicine; PET, positron emission tomography CT scans.
The most significant drop off is seen between March 15 and March 22 at each hospital within all modalities.
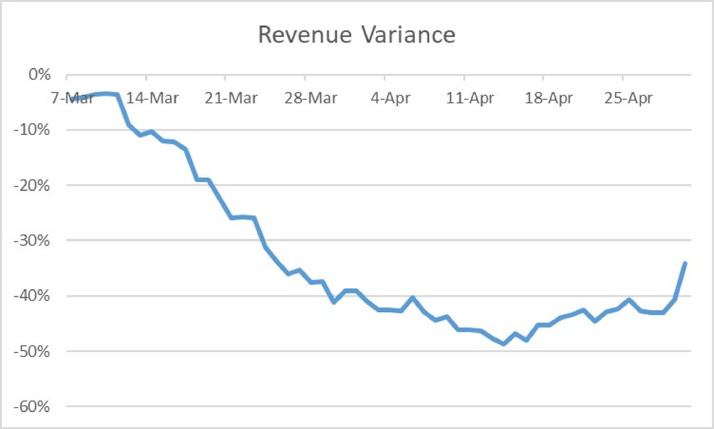
Revenue Loss
Figure 6 encapsulates the increasing revenue losses incurred by the system by showing the variance of actual technical component revenue compared to normal practice during the COVID-19 healthcare crisis. At its lowest point on April 14, the Central hospital had 49% revenue decreased from its technical component compared to normal practice prior to the COVID-19 healthcare crisis. This coincided with the imaging volume decrease seen around April 13.
Figure 6.
The percent variance of the technical component of hospital revenues. Data are based on a rolling 7-day actual total that is compared to the 7-day normalized projected total for 2020.
Discussion
The results from our study demonstrated a 55% imaging volume loss during an 8-week timespan of the COVID-19 pandemic. Although these results do align with early predictive models, which suggested radiology practices would face 50%-70% volume loss during this crisis, the value of this study lies in its comparison to other real-world data compiled in different locales. Ohio has thus far experienced a prevalence of COVID-19 cases that place it within the middle 50% of all states. Several characteristics, such as population demographics and the aforementioned policy changes, have contributed to this status and are ultimately reflected in the degree of imaging utilization change experienced by our institution.
In contrast, a study conducted in the state of New York, where the highest number of cases and deaths related to COVID-19 in the country were seen, demonstrated a 28% overall decline in imaging volume during a similar timeframe (5). On the surface, a large discrepancy exists between imaging utilization in that study compared to our own; however, further comparison of patient setting and modalities reveal important commonalities. Both studies show the largest decline in the outpatient setting, followed by the ED and inpatient. In terms of modality, both studies demonstrated that the primarily outpatient-driven mammography and nuclear medicine studies experienced the highest volumes decreases, whereas the primarily inpatient-driven plain films and CTs experienced smaller volume decreases. Thus, from the limited data available at this time, similar trends in imaging utilization have been seen at various institutions despite the regional differences in COVID-19 prevalence. However, the magnitude of these trends expectedly differs.
From a revenue standpoint, outpatient imaging has a favorable revenue profile as patients tend to be more commercially insured with a lower average disease acuity relative to their inpatient or ED counterparts (4). Losing this imaging volume significantly contributed to the nearly 50% net revenue loss for the health system during this span (Fig 6). Fewer outpatient screening exams also led to fewer downstream diagnostic exams. For example, mammograms, which are an entirely outpatient-driven service, lost up to 93% of normal imaging volume as a consequence of the state order. This eventually led to a decrease in related downstream studies including diagnostic mammograms, ultrasounds, and breast biopsies.
Having quantified and trended the impact of the COVID-19 pandemic on imaging utilization, this study sets the stage for an introspective assessment of current radiology operations. Our institution has taken several measures to address the volume loss and the associated impending recovery phase as hospitals open up. First, the post-COVID-19 patient surge is estimated by the sum of COVID-19-related cancellations, held electives, and the normal demand. Over 4000 screening exams were postponed during this timeframe. These patients are being rescheduled alongside previously scheduled exams over the next 12 months to more evenly and predictably distribute demand. Patient scheduling calls have been extended to the evenings and weekends and precertification processes have begun earlier. To handle this endeavor, the radiology department established a new strategy for staff re-purposing. An expediated formal training program was created to educate over 200 technologists and nurses employed at low-volume departments to help with patient re-scheduling. This process directed efforts to the more acutely important job functions while also preventing furloughs. Creating this new infrastructure of expedited training and bolstering a culture of adaptability will help to not only establish a blueprint for responding to pandemics but also improve our normal operations moving forward.
From a safety standpoint, new partnerships with software companies have been created to maintain social distancing practices by utilizing tools such as the virtual waiting room (11). Workforce strategies such as telehealth and remote Picture Archiving and Communication System use from home workstations will continue to minimize the number of people in the reading room (12). Universal masking mandates have been implemented for all staff and patients. Screening staff and patients at the point of entry for fever and COVID-19 symptoms has been ongoing. Disinfection practices have been further optimized and staff PPE has been reallocated to highest risk and highest traffic areas within the heath system.
From an expense perspective, faculty incentive payments including overtime and internal moonlighting has been reduced or eliminated while maintaining base compensation (12). This is a practice similar to other academic practices across the country. Many top administrators in the healthcare institutions across the country have taken salary cuts up to 20% (13).
There are several limitations to this study. First, there is approximately a 3%-10% error rate in the accuracy of calculating actual imaging volume from the accession numbers in the centralized software system. Studies not categorized as inpatient, outpatient or ED were excluded. Additionally, a small sample of exams have multiple accession numbers for a single study or a single accession number for multiple studies. This is an inherent variability within the coding system. The early 2019 data used for comparison have similar limitations. Due to its proprietary and confidential nature, specific values were not reported for accounts receivable based on imaging services provided and we therefore extrapolated an estimate for revenue for purposes of publication. This study captures the tip of the iceberg in telling the story of volume loss during the COVID-19 crisis and data trends may continue to change. Varying institutional experiences in differential parts of the United States should be aggregated to gain an even more accurate illustration of how radiology practices were affected during this pandemic. Further studies of this format can delve into radiology subspecialty-specific changes in volume.
In conclusion, the actual data provided in this study will be useful in comparing how different regions within the country experienced variable changes in imaging utilization during the respective COVID-19 time period. We recommend large and small institutions to continue publicizing their actual data to create an accurate picture of how the pandemic has affected different types of radiology practices. As health systems continue to navigate the uncertainty of the pandemic while the country progressively opens up, these studies will help inform evidence-based decisions for more accurate volume predictions, policy changes, and staff reorganization. These results will also be helpful in preparing applications for federal and state funding relief as part of institutional recovery plans.
Acknowledgments
Funding
None.
Conflicts of Interest
The author(s) declare(s) no conflict of interest.
References
- 1.Sohrabi C., Alsafi Z., O'Neill N. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Public Health Orders. Ohio Department of Health. Available at:https://coronavirus.ohio.gov/wps/portal/gov/covid-19/resources/public-health-orders/public-health-orders. 2020. Accessed May 10, 2020.
- 3.Stempniak M. Imaging volume dipped upward of 60% at Mednax radiology practices in April. Healthcare Economics & Policy. Radiol Bus. 2020 https://www.radiologybusiness.com/topics/healthcare-economics/mednax-imaging-volume-dip-first-quarter-earnings-covid-19#:~:text=Radiology%20provider%20Mednax%20revealed%20Thursday,decrease%20of%20upward%20of%2035%25 Available at: Accessed May 14, 2020. [Google Scholar]
- 4.Cavallo J.J., Forman H.P. The economic impact of the COVID-19 pandemic on radiology practices. Radiology. 2020 doi: 10.1148/radiol.2020201495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naidich J.J., Boltyenkov A., Wang J.J. Impact of the COVID-19 pandemic on imaging case volumes. J Am Coll Radiol. 2020 doi: 10.1016/j.jacr.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radiology Services 2020 . University Hospitals Health System; 2020. System UHH. [Google Scholar]
- 7.QuickFacts Ohio. United States Census Bureau. Available at: https://www.census.gov/quickfacts/fact/table/OH/LFE305218. Accessed May 10, 2020.
- 8.Cases of Coronavirus Disease (COVID-19) in the U.S. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. 2020. Accessed May 14, 2020.
- 9.Coronavirus (COVID-19). Ohio Department of Health. Available at: https://coronavirus.ohio.gov/wps/portal/gov/covid-19/home. 2020. Accessed May 14, 2020.
- 10.M*Modal Company Overview. 3M. Available at: https://mmodal.com/resources/product-brochures/mmodal-company-overview/. Accessed May 10, 2020.
- 11.Rosipko B. University Hospitals Health System; Cleveland, Ohio: 2020. Radiology Recovery Plan; p. 21. [Google Scholar]
- 12.Lee C.I., Raoof S., Patel S.B. Coronavirus disease 2019 (COVID-19) and your radiology practice: case triage, staffing strategies, and addressing revenue concerns. J Am Coll Radiol. 2020 doi: 10.1016/j.jacr.2020.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haefner M. Hospital CEOs, execs forgo pay amid COVID-19. Becker's Hospital Review. ASC Communications. 2020 www.beckershospitalreview.com/hospital-management-administration/hospital-ceos-execs-forgo-pay-amid-covid-19-7-updates.html Available at: Accessed May 14, 2020. [Google Scholar]