Abstract
Infection is a leading cause of death worldwide in babies under one month of age who are more susceptible to sepsis due to immature host defence mechanisms. Usually, babies may become acutely unwell from infective pathogens due to specific differences in their respiratory and immune systems. However, with the COVID-19 virus, the focus of this paper, it appears that the neonatal population is not significantly affected in the same way as adults. That said, knowledge about this novel virus is rapidly emerging. Therefore, it is vital that neonatal nurses, midwives and other healthcare professionals are adequately informed and educated about the potential impact on neonatal practice. This review paper draws upon key findings and themes from a selection of recent literature to provide an overview of current knowledge on COVID-19 and the implications for care within the neonatal field. The discussion focuses on the nature of COVID-19, its pathophysiology and transmission relevant to maternal and neonatal care. This is followed by implications for practice; namely, maternal issues, the importance of human breast milk, neonatal care relating to parenting and specific management before a final review of the current World Health Organization guidance.
Keywords: COVID-19, Neonate, Pathophysiology, Transmission, Care implications
1. Introduction
The emergence and transmission of new viral diseases represents a major threat to worldwide public health, particularly high-impact animal viruses such as COVID-19 that have switched hosts and are able to be transmitted within human populations. Infection is a leading cause of death worldwide in babies under one month of age who are more susceptible to sepsis due to immature host defence mechanisms. COVID-19 is a respiratory infection, and under normal circumstances babies who acquire pathogens may become acutely unwell due to the anatomical differences in their immune and respiratory systems. In COVID-19 however, it appears that the naivete of the neonatal immune system may have afforded protection against the ‘cytokine storm’ experienced by adults and so the incidence in the neonatal population remains low (Knight et al., 2020).
Nonetheless, due to rapidly emerging knowledge about this novel virus and the need to adapt care environments to prevent cross-infection in babies, parents and staff, it is vital that neonatal nurses, midwives and other healthcare professionals are adequately informed and educated about important areas that will impact on the care of babies and families. This review paper provides an overview of the current knowledge on COVID-19 and the implications for maternal and neonatal nursing care. Firstly, a background to the pandemic will be given followed by a review of a selection of current literature from which key areas of interest are discussed. These areas of interest focus on the nature of COVID-19, related pathophysiology and transmission with specific application to maternal and neonatal care. Implications for practice comprise maternal issues, the importance of human breast milk, parental and neonatal care such as the impact on early attachment and neonatal management including the use of dexamethasone. Finally, the current World Health Organization (WHO) guidance will be outlined, essential for a global perspective.
2. Background
COVID-19. a clinical syndrome caused by the coronavirus (SARS-CoV-2) became a pandemic following an outbreak of viral pneumonitis, first identified in Wuhan, Hubei, China. The disease manifests with a spectrum of symptoms ranging from mild upper respiratory tract infection to severe pneumonitis, acute respiratory distress syndrome (ARDS) and death. Evidence from previous viral outbreaks suggest potentially a higher risk of unfavourable maternal and neonatal outcomes in this population (Alfaraj et al., 2019). While not initially identified as a population at risk, pregnant woman may be more vulnerable to severe infection (Favre et al., 2020). Relatively few cases have occurred in children and neonates who seem to have a more favourable clinical course than other age groups (De Rose et al., 2020). Moreover, the associated policies developed as a result of the pandemic relating to social distancing and prevention of cross infection have led to important considerations specific to the field of maternal and neonatal health, and a necessity to consider unintended consequences for both the mother and baby (Buekens et al., 2020).
As a consequence of COVID-19, countries are faced with a rapidly developing clinical situation. While more definitive evidence is required on short and long term maternal, fetal and neonatal outcomes to ascertain impact in the neonatal population, the number of confirmed cases of COVID-19 has increased globally (Kimberlin and Stagno, 2020). At this stage it is not possible to gauge an accurate account of the number of neonates infected by COVID-19. Many reviews are reports on case studies and anecdotal experiences. In one American study however, COVID-19 positive infants had a much higher hospitalisation rate than any other child age group. Of 95 infants, 62 percent were hospitalised (Center for Disease Control-CDC, 2020). The outcomes of these babies are not currently known. This has necessitated the need for the global neonatal community to prepare for a potential impact, but also for the development of policies to protect neonates, parents and staff. Concern for the vulnerable, high-risk neonatal population goes beyond vertical transmission with the acknowledgement of risk to both mothers and neonates who may acquire COVID-19 through close contact with those infected or carrying the virus (Wang et al., 2020a).
Given such uncertainty, therefore, this virus must be taken seriously in view of the potential impact, not only on disease transmission itself but on the ramifications of social distancing policies on families and health professionals. Moreover, in the light of the current lack of literature on COVID-19 in midwifery and nursing fields, there is a need to address these significant issues that are faced globally and contribute a neonatal nursing and midwifery perspective to the emerging body of evidence during this pandemic.
3. Aims and objectives
The aim of this paper is to address the current and emerging literature, largely medical in nature, and draw on essential implications for neonatal nursing and midwifery practice relating to the babies and families in our care.
The key objectives of the paper are:
-
•
To collate and analyse key literature on the incidence and implications of COVID-19 within maternal and neonatal care.
-
•
To draw on key themes from the literature to inform practice.
-
•
To contribute a neonatal nursing perspective to the emerging body of literature in this unprecedented time of the COVID-19 pandemic.
4. Methodology and search strategy
An integrative review methodology was utilised for this paper as it enables a broad review and facilitates a comprehensive understanding of COVID-19 infection in babies. The literature was gathered using a framework outlined as Arksey and O'Malley's (2005) 5 step framework, and more recently Levac et al.'s. (2010) method of synthesising health evidence. COVID-19 has only been seen in 2019 and 2020. Therefore, relevant and recent literature was easily identified using the terms;
-
•
COVID-19 in babies/neonates AND outcomes (1670)
-
•
COVID-19 in pregnancy AND outcomes (8410)
It is noteworthy that publishers (Elsevier; PubMed) have made their peer-reviewed publications regarding COVID-19 available in full-text for researchers. The search was then limited to the criteria outlined in Box 1 .
Box 1. Selection criteria.
-
•
Full text in English (many of the earlier publications report results of women and babies in China because this is where COVID-19 is believed to have started)
-
•
Pregnancy in women with COVID-19 and the disease process
-
•
Guidelines for women with suspected COVID-19 infection
-
•
Articles about possible intrauterine transmission
-
•
Articles about possible transmission during labour and delivery
-
•
Neonatal COVID-19 case reports
-
•
Caring for the neonate with COVID-19
Alt-text: Box 1
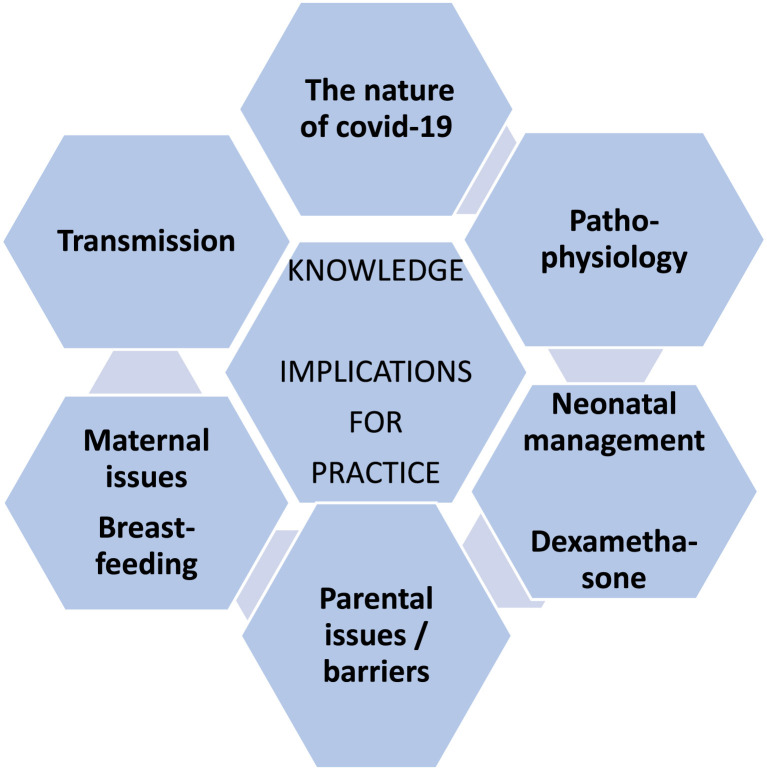
Other resources have been used to form the background such as the neonatal immune response and the developmental characteristics of the neonatal respiratory system. Updates from the World Health Organization and the CDC have been utilised to ensure that any recommendations comply with current best evidence and practice. The emerging themes for discussion are outlined in Fig. 1 .
Fig. 1.
Emerging themes.
5. The nature of coronavirus
Coronaviruses are a large family of viruses that can cause a range of illnesses. These illnesses include the common cold, Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). Coronaviruses have been around for many years; therefore, humans have built an immunity to them (Parrish et al., 2008). This is demonstrated by a common cold generally not being severe. When a new strain of coronavirus is discovered, it is called a ‘novel' coronavirus because it is new and has not been previously identified. (CDC, 2020). The International Committee on Taxonomy of Viruses (ICTV) formally named the virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2 or SARS-CoV-2 due to its genetic similarity to the virus that caused the SARS outbreak in 2003. While related, however, the two viruses are different (WHO, 2020a).
Animals can also have coronavirus related illnesses which can mutate and be passed on to humans (Parrish et al., 2008), referred to as 'zoonotic spillover' (Johnson et al., 2015). When this happens, the disease can be more severe because humans have not had to fight the illness before, with SARS and MERS as examples. What makes this situation even more problematic is that the animal to human 'spillover' of a new virus, signals diseases that have a high pandemic potential (Johnson et al., 2015). This is because they are able to amplify by human-to-human transmission with spread on a global scale.
The first reported cases of COVID-19 appeared to be potentially from an animal source. Subsequent cases, however, were because of person to person transmission (Wu et al., 2020). The virus is now known to be extremely contagious, particularly where there is close contact between people (Liu et al., 2020a). From its original source, COVID-19 rapidly spread to other countries due to this high transmission rate. In February 2020, the World Health Organization (WHO) officially named the coronavirus as COVID-19 (WHOb, WHOc, 2020; Karimi-Zarchi et al., 2020) and a pandemic was subsequently confirmed.
6. Transmission of COVID-19 in babies
How COVID-19 is spread is also an important area of knowledge about which the world is still learning, particularly in the field of maternal and neonatal care. It is evident that symptomatic people with coronavirus disease are the main disseminators, but there is also emerging evidence that asymptomatic people should not be underestimated (Heneghan et al., 2020). The major transmission routes are droplet, contact and aerosol. Faecal-oral transmission cannot be ignored, because the virus was detected in the faecal samples of patients in the United States and China (Zheng et al., 2020). The evidence on maternal-infant vertical transmission is still unclear. Favre et al. (2020) suggested that pregnant women may be more susceptible to the virus. Alfaraj et al. (2019) , however, analysed evidence from previous viral outbreaks; namely SARS-CoV and MERS-CoV and put forward a suggestion of a greater risk of adverse maternal and neonatal outcomes. To date, emerging evidence to support vertical transmission of COVID-19 during pregnancy remains low (Knight et al., 2020). According to existing data, amniotic fluid, cord blood, neonatal throat swab, placental tissue and breastmilk samples show low incidence (Yang et al., 2020a, 2020b). One study tested samples for SARS-CoV-2 from six newborn babies delivered to infected mothers; all samples tested negative for the virus (Lu and Shi, 2020).
7. Pathophysiology of COVID-19 in babies
The pathophysiology of the virus and how it affects the human body is now starting to be known. The COVID-19 virus appears to directly infect cells via the ACE2 Receptor (Sriram et al., 2020). This is expressed in various organs, including the lung. Cells in children's lungs express this receptor less than those in adult lungs. This may be one reason why the infection affects children less severely.
There are some specific areas of concern in relation to neonates and COVID-19 infection. The respiratory physiology in neonates is immature and different to that of older children and adults (Saikia and Mahanta, 2019). It is this difference that is responsible for why neonates can become acutely ill when they have a respiratory illness. Neonates are also preferential nose breathers; however, their nasal passages are small and prone to be easily obstructed by thick secretions, causing difficulty in breathing and an increase in the work of ventilation. The small diameter of the airways causes higher resistance to airflow in both term and preterm neonates. In addition, neonates, especially premature ones, have fewer alveoli. The alveoli they possess lack interalveolar communications and are at risk of collapse and atelectasis in dependent areas of the lung (Saikia and Mahanta, 2019; Neumann and von Ungern-Sternberg, 2014; Mercer and Skovgaard, 2002).
Furthermore, intercostal muscles of neonates are poorly developed and lack the ability to be the accessory muscles of respiration. The unfavourable rib configuration of ribs being horizontally aligned from the vertebral column, means that the size of the thorax cannot be increased during inspiration. In neonates, the diaphragm is responsible for the workload of breathing; however, it is prone to be easily fatigued. To maintain minute volume, babies breathe faster with smaller tidal volumes (Saikia and Mahanta, 2019; Mercer and Skovgaard, 2002).
Neonates also have low total lung capacity and functional residual capacity. They have a highly compliant thoracic wall and poorly compliant lung tissue, which causes air trapping in the alveoli. Neonates attempt to modify the airflow to the small airways by creating a positive end inspiratory pressure (Saikia and Mahanta, 2019; Neumann and von Ungern-Sternberg, 2014). Moreover, neonates have a higher basal metabolic requirement of oxygen, and this requirement increases when they are sick.
Another area of concern is the immune system which is relatively immature at birth with neonatal complications being potentially high when exposed to pathogens. During fetal life the development of the immune system is initiated by a highly complex process mediated by the expression of cytokines. Fetal cytokines play a role to protect the fetus against rejection; placental and fetal cytokines also protect against infection (Erić, 2019). The transplacental transferal of maternal antibodies contributes to the early defence against pathogens, however this passive protection only lasts until the child is six months of age (Basha et al., 2014).
Newborns also do not have fully developed innate or adaptive immune responses (Strauss-Albee et al. 2015). The innate immune system provides the first line of defence against invading pathogens in neonates. The cells in the innate immune system include neutrophils, monocytes, macrophages and dendritic cells; however the functions of all of the components of innate immunity are weak in newborns (Simon et al., 2015). Despite being mature, neonatal neutrophils show weak bactericidal functions, poor responses to inflammatory stimuli, reduced adhesion to endothelial cells and diminished chemotaxis (Neumann and von Ungern-Sternberg, 2014). Coupled with immaturity of monocytes and macrophages, impairment in neutrophil functions puts the baby at risk of significant viral infection.
The adaptive immunity in the newborn consists of B cell and T cell lymphocytes (Basha et al., 2014). Both B and T cell lymphocytes originate in the bone marrow, however only B lymphocytes mature in the bone marrow. T lymphocytes migrate to the thymus for maturation. Following maturation, both types of lymphocytes enter the bloodstream and migrate to peripheral lymphoid organs (Basha et al., 2014). One of the major roles that B-cells play in an immune response is the production of antibodies, that specifically recognise and bind to proteins on the invading bacteria or virus particles (Basha et al., 2014). However, neonatal B-cells are naïve, lack specific antigenic exposure and have only a partially developed surface immunoglobulin (Ig) repertoire (Basha et al., 2014).
The three independent pathways that activate the complement system in the newborn are critical to host defence and inflammation. Complement components facilitate opsonization, are chemo-attractants for innate cells, mediate cell lysis and influence antibody production (Merle et al., 2015). Almost all of the concentrations of circulating immune components in neonates are 10–80percent lower than in adults. Complement levels increase after birth, with some serum factors reaching adult concentration within a month; however others evolve more slowly (Merle et al., 2015). Newborns have low immunoglobulin concentration, making the newborn, and particularly the premature baby, susceptible to bacterial and viral infections (Simon et al., 2015).
Furthermore, in neonates, the secretion of inflammatory mediators is deficient (Erić, 2019). Inflammation is a protective response to infection or injury, and the inflammatory response is controlled primarily by cytokines. Cytokines are endogenous mediators of the immune system and are directly involved in the activation of cells at the inflammatory site (Erić, 2019). It has been proposed that the balance of proinflammatory and anti-inflammatory cytokines may ultimately determine the outcome with sepsis in newborn infants (Machado et al., 2014). To reiterate, this inflammatory response may have its origins during the fetal period.
One proposed disease mechanism in severe cases is a ‘cytokine storm’. This describes a cascade process whereby the immune system over-reacts to an infection. In COVID-19 the virus leads to an overproduction of immune cells and their activating compounds, cytokines, that are associated with a surge of activated immune cells into the lungs (Jose and Manuel, 2020). The resulting lung inflammation (alveolar macrophage activation) causes direct tissue damage, recruitment of neutrophils to tissues, and other pro-inflammatory effects. This damage can lead to ARDS (Mehta et al., 2020). It is noteworthy that the cytokine storm is particularly relevant in new influenza variants such as the H1N1 'swine flu' and H5N1 'bird flu' of recent years (Saunders-Hastings and Krewski, 2016).
Not much is known about the link between the naïve newborn immune system and the decreased risk of a cytokine storm in COVID-19. Mature immune response encompasses the ability to produce inflammatory cytokines and to regulate those responses. It is suggested that neonates are profoundly reliant on the innate immune system; this inflammation may help improve their chances of clearing pathogens at the risk of excessive activation and death (Zhao et al., 2008). A sufficient number of T-cells could be vital for protecting neonates from the lethal inflammatory response of innate cells.
Natural killer (NK) cells are granular lymphocytes and a component of the adaptive immune system and are among the earliest cellular responders and defence against most viral infections (Strauss-Albee et al. 2017; Bashe et al., 2014). NK cells serve as a bridge between innate immunity and adaptive immunity and release a variety of cytokines (Lee and Lin, 2013). It is noteworthy that severe acute respiratory infection with the influenza virus in neonates has shown a decrease in NK cells in the blood, and that the influenza virus directly infects the NK cells causing apoptosis (Lee and Lin, 2013).
Concern has been raised that a cytokine storm and hyperinflammation may increase the risk for poor neurodevelopmental outcomes in the neonate (Martins-Filho and Tanajura, 2020). This is because there is growing evidence that infection during pregnancy and enhanced expression of cytokines are associated with an increased risk of autism spectrum disorder and schizophrenia in the offspring (Estes and McAllister, 2016). There is a need for longitudinal research to evaluate this issue further with COVID-19 positive women and their children.
8. Implications for practice
8.1. Maternal issues
Current evidence suggests that pregnant women are not at greater risk then other adults for contracting COVID-19 (Rasmussen et al., 2020). This is despite the fact that pregnant women are more susceptible to respiratory illness due to the physiological changes to the immune and cardiopulmonary systems that occur during pregnancy (Yan et al. 2020). The immune system of a newborn is the product of the immune environment during pregnancy. While responding to allo-antigens, the maternal immune system must be tolerant to the fetus (Yu et al., 2018, Yu et al., 2020). The placental immune response for specific viruses and pathogens affects the outcome of the pregnant woman's susceptibility to, and severity of, certain infectious diseases (Simon et al., 2015).
COVID-19 infection is not thought to be more severe in pregnant women despite the pre-existing physiological factors that predispose the women to more poorer outcomes during respiratory infections, that is, basal atelectasis from gravid uterus, lower lung reserves and increased oxygen consumption (Qiao, 2020; Zaigham and Andersson, 2020). Reviews have mostly reported, however, short intervals of time from COVID-19 diagnosis to caesarean deliveries (Chen et al., 2020). Therefore, the true impact has not been determined. Evaluation of 147 pregnant women reported up to 8percent severely ill and 1percent critically ill which was less than that observed during the H1N1 pandemic (Ashokka et al., 2020). Current evidence with pregnant women with COVID-19 pneumonia indicate that conditions are similar to non-pregnant adults (Chen et al., 2020; Yan et al., 2020). While there is insufficient data, it is suggested that fetal growth restriction rates are increased highlighting a need for fetal growth surveillance after previous occurence and recovery from COVID-19 (Di Mascio et al., 2020).
There is concern about the spread of infection during labour and birth because of the possibility of droplet contamination when women are forcefully exhaling during active labour. It has been suggested there is a need to consider early epidural analgesia, and that unmedicated natural labour be discouraged (Ashokka et al., 2020). Infection control precautions includes restrictions on number of people in the room to minimise movement between care locations, and the number of external visitors and care providers (Ashokka et al., 2020). This resulted in women not having partner or support people with them during labour.
The caesarean section rate is reported to be high 86–100percent (Della Gatta et al., 2020; Di Mascio et al., 2020; Yan et al., 2020; Zaigham and Andersson, 2020). Early on in the history of the pandemic, the reason for caesarean section was the uncertainty regarding the risk of intrapartum vertical transmission (Chen et al., 2020). Generally, indications are not well reported and have included the possibility of COVID-19 pneumonia (Della Gatta et al., 2020; Yan et al., 2020), fetal distress (Zaigham and Andersson, 2020), as well as anxiety toward potential consequences of new viral infection (Della Gatta et al., 2020). There appears to be no risk of transmission during vaginal delivery as vaginal swabs of COVID-19 positive women are shown to be negative (Yan et al., 2020). It has been suggested that the threshold for caesarean delivery be lower than usual to ensure infection control procedures are adhered to. Based on evidence, COVID-19 infection cannot be considered as the indication for delivery and should be determined by individual factors such as worsening maternal health (Di Mascio et al., 2020; Ashokka et al., 2020).
The number of premature births during COVID-19 has been documented between 42 and 56percent (Di Mascio et al., 2020; Yan et al., 2020; Zaigham and Andersson, 2020); however the risk of spontaneous miscarriage and spontaneous preterm birth do not appear to be increased (Yan et al., 2020). It would appear that the high preterm birth rate is related to the consequences of elective intervention and are therefore iatrogenic in nature (Di Mascio et al., 2020; Della Gatta et al., 2020; Yan et al., 2020). At this stage, the outcome of pregnant women with no or mild symptoms of COVID-19 infection is yet unknown.
To re-iterate, there is no evidence of vertical transmission when the infection manifests during the third trimester of COVID-19 positive pregnant women. Amniotic fluid and cord blood samples were found to be negative (Di Mascio et al., 2020; Yan et al., 2020), as were neonatal throat swabs and breastmilk samples (Chen et al., 2020). There has been reported, however, one case of suspected vertical transmission from COVID-19 positive women who had a caesarean section and the neonate separated from mother 10 minutes after birth was found to be COVID-19 positive. It is believed therefore that vertical transmission cannot be excluded (Wang et al., 2020b).
8.2. The importance of human breast milk
Human milk contains a variety of soluble and cellular antimicrobial substances which are believed to facilitate immune development and maturation in infants (Field, 2005). Substances that modulate the inflammatory response have been identified in human milk and these could be beneficial to the newborn during COVID-19. A balance needs to exist between the protective inflammation and the modulation of inflammation that naturally exists in breast milk to protect the newborn against infection (Cacho and Lawrence, 2017). Human milk has both anti-inflammatory and pro-inflammatory cytokines; however anti-inflammatory cytokines dampen the T-helper cells’ 1 (Th1) cytokine response, thereby inhibiting pro-inflammatory cytokine release (Cacho and Lawrence, 2017; Field, 2005). Osteoprotegerin, a member of the tumour necrosis factor (TNF) superfamily has been suggested to prevent TNF-induced inhibition of T cell proliferation, thereby enabling T cells to dampen an inflammatory response. Lactoferrin has been demonstrated to inhibit the production of proinflammatory cytokines (Field, 2005). Epidermal growth Factor (EGF) also has anti-inflammatory properties and is higher in preterm milk compared to full-term milk. Care issues and guidance relating to breast-feeding is covered later.
8.3. Parental issues
The impact of social distancing must not be under-estimated. When the pandemic took hold, neonatal units across the globe began to implement revised visiting policies to restrict the presence of parents and extended family, in an attempt to protect hospitalised neonates. The policy was also introduced to minimise potential sickness in the number of healthcare professionals available to care for mothers and neonates, should they need to self-isolate for a minimum of 7–14 days. The unfortunate consequence of such a policy has resulted in potentially long periods where parents are unable to see or touch their baby.
Consequently, neonatal nurses and midwives around the globe are prevented in their ability to provide true family integrated care. Given what is known about the impact of early separation on attachment between parent and baby and parental mental health (Petty et al., 2018; Fowler et al., 2019) and the practices that positively influence infant development and breastfeeding rates, such as skin-to-skin contact and family integrated care (O'Brien et al., 2018), the implementation of these are now more challenging. The concern is that preventing such beneficial strategies may therefore increase parental stress, depression and anxiety due to parent-infant separation and being unable to participate in their baby's care and develop their parenting role. Another concern is the potential disruption to communication with healthcare professionals, which is so essential (Gallagher et al., 2018). Midwives, neonatal nurses and health professionals have had to quickly adapt to this challenge and engage in the balancing act of providing optimum care to families whilst at the same time, ensuring the safety of all neonates and parents under their care as well as their colleagues, their own families and the wider public. This is a situation that has not been faced in recent healthcare.
8.4. Neonatal COVID-19 and management
The cases of neonatal COVID-19 have been limited to date. It would appear neonates with COVID-19 have a mild course with favourable outcomes.
Possible causes for the neonate becoming COVID-19 positive is through vertical transmission from the mother or cross-infection from carers. Understandably, many of the initial reports have come from China (Luo and Yin, 2020; Li et al., 2020; Yang et al., 2020b; Liu et al., 2020b; Yan et al., 2020). There is only a relatively small number of cases of neonatal COVID-19 and each study presents limited evidence of vertical transmission. In fact, the recent WHO (2020d) guidelines (as of June 25th, 2020) state there has been no confirmed mother-to-child transmission (WHO clinical management in COVID-19 interim guidance) supported by a review by Zimmerman and Curtis (2020). Despite this, there are studies emerging where the findings leave this open to further interpretation.
Arecent systematic review by Smith et al. (2020) found one case of neonatal COVID-19. Zaigham and Andersson's (2020) systematic review concluded that vertical transmission of the COVID-19 cannot be ruled out for neonatal infection. There was a case in Iran where a COVID-19 positive mother delivered a large-for-gestational-age (LGA) baby at 32 weeks gestation. The neonate had a positive nasal swab at 24 hours old. All PCR tests were negative for COVID-19 apart from the amniotic fluid. The neonate had initial fever but was well. All precautions for droplet infection were undertaken and only the amniotic fluid was positive; the authors concluded that the neonate developed the infection in-utero (Zamaniyan et al., 2020).
A recent French case study further questions the vertical transmission hypothesis. Abasse et al. (2020) describe a 33-week male neonate with a positive nasopharyngeal (NA) swab at 24 hours of age for COVID-19 who developed early mild respiratory distress. He was successfully managed with non-invasive ventilation (NIV) for 24 hours and continuous positive airway pressure (CPAP) for 48 hours. Chest Xray (CXR) showed normal lung aeration without pneumonia. However, on day 7–14, some respiratory distress returned with fever. The neonate was again tested with a NP swab which was COVID-19 positive. He was managed with high flow nasal canula for his respiratory distress. The authors concluded the preterm labour was due to COVID-19, as there were no other indications for the preterm delivery. They also suggested a vertical transmission of COVID-19 could not be excluded as the baby was continually nursed in isolation with droplet and contact precautions (Abasse et al., 2020).
Community transmission acquisition has been recorded in the literature, but the course is usually mild. Dumpa et al. (2020) highlighted a case of a 22-day old male infant presenting at a New York emergency department with fever, tachycardia and decreased oral intake. The neonate had an uncomplicated term vaginal delivery, and was exclusively breastfed. He was not in any acute distress; however given the risk of community-acquired COVID-19, he was investigated for sepsis and a NP swab was performed. As a precaution, the neonate was cared for in a negative pressure room with strict droplet infection control precautions. The NP swab returned positive the day after admission. There was no indication of bacterial infection and his condition was stable. He was discharged home after two days with advice for parents to self-quarantine at home and continue meticulous hand hygiene, particularly with feeding and nappy changes. The neonate continued to be well and thriving at the four-week follow-up appointment (Dumpa et al., 2020).
Chacón-Aguilar et al. (2020) also discuss a presentation to a Spanish Emergency Department of a 26-day old male neonate with fever and neurological manifestations. The neonate had been living in close contact with multiple symptomatic family members with COVID-19. He had a history of two episodes of seizure activity and on presentation had a fever with nasal discharge and vomiting. He had been exclusively breastfed since birth. Septic workup for bacterial infection was undertaken, as well as NP swab for COVID-19, which was positive. The neonate was admitted and isolated for droplet precautions in negative pressure room. The fever resolved after two days and septic workup was negative for bacterial infection. He was hospitalised for six days with no further seizure activity. Neurological examination was normal, he was discharged home with parents to home-isolate with instructions for strict hand hygiene for feeding and nappy changing (Chacón-Aguilar et al., 2020).
Another concern for the transmission of a COVID-19 was through the breast milk of a positive mother and breast feeding initially was not advised. However, to date there has been no evidence of presence of the virus in breastmilk of COVID-19 mothers and these mothers may continue to breastfeed using strict hand hygiene and droplet precautions (Velasco-Aro and Sanchez-Mostiero, 2020).
There was also some concern that a COVID-19 positive mother may infect her neonate in the postnatal period, and it was advised to separate and isolate mothers from their babies. This also been shown to be unnecessary (Stuebe, 2020). Lowe and Bopp (2020) describe a case in Queensland of a 40+2 week uncomplicated vaginal birth, COVID-19 positive mother who roomed in with her COVID-19 negative neonate after birth. Both parents tested positive for the virus. As the neonate was well and breast feeding, no further COVID-19 testing was indicated. This neonate continued rooming in with their parents and was discharged on day four following birth. The parents were advised to continue home isolation and use viral droplet precautions. Follow-up indicated the neonate was healthy and thriving (Lowe and Bopp, 2020).
The WHO (2020d) has concluded that COVID-19 mothers and their babies should not be separated, and skin-to-skin contact and breastfeeding encouraged, because the benefits outweigh any potential risks. WHO (2020d) recommend careful monitoring of pregnancies with COVID-19 with measures to prevent neonatal infection. Most common investigations include amniotic fluid, cord blood, placental swabs, genital swabs, with neonatal throat and nasopharyngeal swabs (Kallem and Sharma, 2020). Isolation with negative pressure rooms in NICU within a closed incubator is required only for symptomatic neonates (Zaigham and Andersson, 2020).
The studies so far suggest neonates can develop COVID-19; however, it is still not clear the route of transmission. It is therefore recommended that all newborns delivered from positive mothers are thoroughly investigated for the virus. If both mother and baby are well, there is no need to separate a positive mother from her baby. Likewise, if the mother and baby are well, skin-to-skin and breast feeding should be encouraged, as the benefits outweigh any potential harms. If a neonate becomes unwell and requires intensive care, they should be nursed with droplet precautions in a closed incubator. The management is dictated by the presenting signs and symptoms. It would appear the presenting symptoms in the neonate are mild, with low-grade fever and gastrointestinal signs such as poor feeding and vomiting. The respiratory symptoms are also limited to mild tachypnoea and/or tachycardia. However, as there has been a presentation of seizure activity with fever a neurological examination should be part of the investigations.
8.5. Treatment with dexamethasone
As of writing this paper, there has been a preliminary study published in the general media from the University of Oxford on the use of dexamethasone in COVID-19 infections. The RECOVERY (Randomised Evaluation of COVID-19 thERapY) trial enrolled over 11,500 patients in a randomised controlled trial (RCT) in over 175 NHS hospitals in the UK. The trial randomised 2104 patients to receive dexamethasone 6 mg in one daily dose for ten days and compared that with 4321 patients who received usual care. The study results showed dexamethasone had significantly reduced mortality by one-third in ventilated patients and by one-fifth in patients receiving oxygen (Nuffield Department of Health, 2020).
Although the findings from this study have not been published in any peer reviewed paper, the consensus globally among the medical profession is that this research group have a scrupulous reputation and would not publish to the wider public if they were not confident of these results. Given these findings, the national medical director for the NHS and the chief medical officers of Wales, Scotland, Northern Ireland and England published a Therapeutic Alert on June 16th, 2020 recommending an immediate change of practice.
‘’Normally we would advise waiting for the full paper before changing practice, to ensure final analysis and peer review do not lead to different conclusions. However, given this clear mortality advantage, with good significance, and with a well-known medicine which is safe under these circumstances, we consider it is reasonable for practice to change in advance of the final paper’’ (Medicines & Healthcare products Regulatory Agency (MHRA), 2020).
The WHO has also welcomed these preliminary results and state it is “looking forward to a full data analysis” (WHO, 2020e).
Dexamethasone is a steroid used in many respiratory conditions associated with the inflammatory response. It is effective in suppressing the cytokine storm, which is the key factor in the severity of COVID-19 infections. Dexamethasone is also given to the mother in preterm labour to help mature the lungs and lessens the incidence of Respiratory Distress Syndrome in the premature neonate. To date, there have been no studies on antenatal dexamethasone and severity of COVID-19 in the preterm neonate; however the results from the RECOVERY trial do raise the question of whether this could be beneficial in neonatal COVID-19 infections.
It is important to acknowledge that the current studies have focused on babies exposed in late pregnancy and the postnatal period. At this stage, there is no research that has explored whether there are any effects with exposure in early pregnancy, and whether COVID-19 is indeed teratogenic. It is recommended that future studies investigate this possibility. In addition, there is a need for longitudinal studies of neonates from COVID-19 positive mothers to ascertain the potential for neurodevelopmental issues.
An interesting and positive outcome of the COVID-19 virus has been reported from Ireland as an unprecedented fall in preterm births from University Hospital, Limerick. There has been a 73 percent reduction in the number of very low birth-weight babies born in the hospital, when compared to the average for the same first four months of the year in the preceding two decades. The reduction has been credited to the effect of positive lifestyle influences during isolation and COVID-19 restrictions, and reduced exposure to ordinary stressors (Cullen, 2020). The stressors that were reduced include work and commuting along with, increased family support, better infection avoidance, improved sleep, nutrition and exercise, and reduced exposure to tobacco and illegal drugs (Cullen, 2020).
8.6. The World Health Organization recommendations
The World Health Organization Health Emergencies programme has an essential role to play in providing contemporary data in pandemics from the initial prevention to helping countries recover (https://www.who.int/emergencies/en/). While neonatal clinicians and researchers publish their experiences in countries with COVID-19, the WHO experts have been collating data from countries and are providing guidance for countries on best practice and evidence during COVID-19 using a traffic light system with green, red and yellow symbols. Green denotes data which is recommended and based on the best evidence, red denotes practices which are not recommended and yellow, practices which are conditionally recommended (WHO, 2020d: Clinical management of COVID-19 – interim guidance 27th May 2020).
The pertinent recommendations for countries for mothers who are COVID-19 positive and their babies are that the mother should not be separated from her baby, and breastfeeding should be encouraged as well as implementing increased hygiene practices. Specific recommendations on breastfeeding resulted from analysis of seventeen studies reporting the outcomes for 115 positive mothers which found of 13 COVID-19 positive babies, only four were breastfed and a further two mix-fed. Thus, with low potential transmission, the health benefits of breastfeeding outweigh the risks and the WHO recommends the initiation and continuation of breastfeeding for all mothers with suspected or confirmed COVID-19.
Maternal and newborn health is not just directly impacted by illness in the mother or baby, the indirect costs through the impact on services could be substantial (Robertson et al., 2020). Riley et al. (2020) predict that with only a 10 percent decline in maternal and newborn care, an estimated 28,000 maternal and 16,800 newborn deaths could result, and with the disruption to family planning services, there could be many more unplanned pregnancies. Therefore, one of the key objectives for the WHO is to provide guidance to minimise the health systems impact of this pandemic across the lifespan.
9. Conclusion
The COVID-19 pandemic has presented neonatal nurses and midwives with challenges when caring for babies and families. This review has presented what is currently known about COVID-19 and neonatal health. Further information and research as they are generated will add to a complete picture of the health outcomes. While babies have been infected, the naivete of the neonatal immune system in relation to the inflammatory response would appear to be protective, with further responses achieved with the consumption of human milk. The WHO has made clear recommendations about the benefits of breastfeeding, even if the mother and baby dyad is COVID-19 positive, if they remain well. The mother and baby should not be separated, and the mother needs to be able to participate in her baby's care and develop her mothering role. The complexities of not being able to access usual and adequate support means that the mother's mental health should be a priority during isolation and social distancing along with the emotional needs of the father and / or partner.
Understandably, the research related to neonatal COVID-19 infection is limited and in very early stages, and unfortunately much of the literature is vague and contradictory. For example, there is still no clear consensus on vertical transmission of the virus. Also, some case studies suggest COVID-19 in the neonate is less severe but this requires much more robust research. Furthermore, future research needs to focus on maternal infection in early pregnancy and whether the virus is teratogenic. Finally, the most recent and promising research related to dexamethasone in reducing mortality, needs to be extended to antenatal dexamethasone use in preterm labour and the potential positive impact on neonatal COVID-19 infection.
Undoubtedly, more information, knowledge and research findings will emerge in this significant event in global healthcare. We will continue to learn, disseminate and share knowledge generated in the name of global, collaborative learning for the collective good of babies, families and the staff who care for them.
Authorship
All authors meet the criteria for authorship, have approved the final article and all those entitled to authorship are listed as authors.
Funding
No external funding
Ethical statement
Ethical approval was not required.
Declaration of competing interest
None.
References
- Abasse S., Essabar L., Costin T., Mahistra V., Kaci M., Braconnier A., Serhal R., Collet L., Fayssoil A. 2020. Neonatal COVID 19 Pneumonia: Report of the First Case in a Preterm Neonate in Mayotte, an Overseas Department of France. Pre Prints.https://www.preprints.org/manuscript/202005.0482/v1 (viewed 10 June 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfaraj S.H., Al-Tawfiq J.A., Memish Z.A. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection during pregnancy: report of two cases & review of the literature. J. Microbiol. Immunol. Infect. 2019;52(3):501–503. doi: 10.1016/j.jmii.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8(1):19–32. [Google Scholar]
- Ashokka B., Loh M., Tan C.H., Su L.L., Young B.E., Lye D.C., Biswas A., Illanes S.E., Choolani M. Care of the pregnant women with coronavirus disease of 2019 in labor and delivery: anaesthesia, emergency caesarean delivery, differential diagnosis of the acutely ill parturient, care of the newborn, and protection of the healthcare personnel. Am. J. Obstetr. Gynaecol. 2020 doi: 10.1016/j.ajog.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basha S., Surendran N., Pichichero M. Immune responses in neonates. Expet Rev. Clin. Immunol. 2014;10(9):1171–1184. doi: 10.1586/1744666X.2014.942288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buekens P., Alger J., Bréart G., Cafferata M.L., Harville E., Tomasso G. A call for action for COVID-19 surveillance and research during pregnancy. Lancet Glob. Health. 2020;8(7):e877–e878. doi: 10.1016/S2214-109X(20)30206-0. Apr 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacho N.T., Lawrence R.M. Innate immunity and breast milk. Front. Immunol. 2017;8:584. doi: 10.3389/fimmu.2017.00584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, CDC Coronavirus disease 2019 (Covid-19). Frequently asked questions. 2020. https://www.cdc.gov/coronavirus/2019-ncov/faq.html#Coronavirus-Disease-2019-Basics (accessed 10 June 2020)
- Chacón-Aguilar R., Osorio-Cámara J.M., Sanjurjo-Jimenez I., González-González C., López-Carnero J., Pérez-Moneo-Agapito B. COVID-19: fever syndrome and neurological symptoms in a neonate, COVID-19: Síndrome febril y clínica neurológicaen neonato. An . Pediatr. (Barc) 2020 doi: 10.1016/j.anpedi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., Li D., Xu D., Gong Q., Liao J., Yang H., Hou W., Zhang Y. Clinical characteristics and intrapartum vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical record. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen P. Positive lockdown influence credited with fall in pre-term births. Ir. Times. 2020 https://www.irishtimes.com/news/health/positive-lockdown-influence-credited-with-fall-in-pre-term-births-1.4275968 June 11. (viewed 17 June 2020) [Google Scholar]
- De Rose D.U., Piersigilli F., Ronchetti M.P., Santisi A., Bersani I., Dotta A., Danhaive O., Auriti C., Study Group of Neonatal Infectious Diseases of The Italian Society of Neonatology (SIN) Novel Coronavirus disease (COVID-19) in newborns and infants: what we know so far. Ital. J. Pediatr. 2020;46(1):56. doi: 10.1186/s13052-020-0820-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Della Gatta A.N., Rizzo R., Pilu G., Simonazzi G. COVID19 during pregnancy: a systematic review of reported cases. Am. J. Obstet. Gynecol. 2020 doi: 10.1016/j.ajog.2020.04.013. https://www.sciencedirect.com/science/article/pii/S0002937820304385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Mascio D., Khalil A., Saccome G., Rizzo G., Buca D., Liberati M., Vecchiet J., Nappi L., Scmbia G., Berghella V., D'Antonio F. Outcomes of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: a systematic review and meta-analysis. Am. J. Obstetr. Gynaecol. 2020 doi: 10.1016/j.ajogmf.2020.100107. MFM:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumpa V., Kamity R., Vinci A.N., Noyola E., Noor A. Neonatal coronavirus 2019 (COVID-19) infection: a case report and review of literature. Cureus. 2020;12:5. doi: 10.7759/cureus.8165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erić Ž. Proinflammatory cytokines in a newborn: a literature review. Signa Vitae-A J. Intensive Care And Emerg. Med. 2019;15:2. http://www.signavitae.com/2017/06/proinflammatory-cytokines-in-a-newborn-a-literature-review/ Accessed 17/6/2020. [Google Scholar]
- Estes M., McAllister A.K. Maternal immune activation: implications for neuropsychiatric disorders. Science. 2016;353:722–727. doi: 10.1126/science.aag3194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favre G., Pomar L., Musso D., Baud D. 2019-nCoV epidemic: what about pregnancies? Lancet. 2020;395:10224. doi: 10.1016/S0140-6736(20)30311-1. e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field C.J. The immunological components of human milk and their effect on immune development in infants. J. Nutr. 2005;135(1):1–4. doi: 10.1093/jn/135.1.1. [DOI] [PubMed] [Google Scholar]
- Fowler C., Green J., Whiting L., Petty J., Rossiter C., Elliott D. The forgotten mothers of extremely preterm babies: need for increased psychosocial support. J. Clin. Nurs. 2019;8(11–12):2124–2134. doi: 10.1111/jocn.14820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher K., Shaw C., Aladangady N., Marlow N. Parental experience of interaction with healthcare professionals during their infant's stay in the neonatal intensive care unit. Arch. Dis. Child. Fetal Neonatal Ed. 2018;103(4):F343–F348. doi: 10.1136/archdischild-2016-312278. [DOI] [PubMed] [Google Scholar]
- Heneghan C., Brassey J., Jefferson T. COVID-19: What proportion are asymptomatic? The Centre for Evidence-Based Medicine. 2020. https://www.cebm.net/Covid-19/Covid-19-what-proportion-are-asymptomatic/ April 6, 2020. (viewed 19 June 2020)
- Johnson C.K., Hitchens P.L., Evans T.S., Goldstein T., Thomas K., Clements A., Joly D.O., Wolfe N.D., Daszak P., Karesh W.B., Mazet J.K. Spillover and pandemic properties of zoonotic viruses with high host plasticity. Sci. Rep. 2015;5:14830. doi: 10.1038/srep14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jose R.J., Manuel A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir. Med. 2020 doi: 10.1016/S2213-2600(20)30216-2. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30216-2/fulltext April 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kallem V.R., Sharma D. COVID 19 in neonates. J. Matern. Fetal Neonatal Med. 2020:1–9. doi: 10.1080/14767058.2020.1759542. [DOI] [PubMed] [Google Scholar]
- Karimi-Zarchi M., Neamatzadeh H., Dastgheib S.A., Abbasi H., Mirjalili S.R., Behforouz A., Ferdosian F., Bahrami R. Vertical transmission of coronavirus disease 19 (COVID-19) from infected pregnant mothers to neonates: a review. Fetal Pediatr. Pathol. 2020:1–5. doi: 10.1080/15513815.2020.1747120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimberlin DW, Stagno S. Can SARS-CoV-2 infection be acquired in utero? More definitive evidence is needed. JAMA. 2020;323(18):1788–1789. doi: 10.1001/jama.2020.4868. [DOI] [PubMed] [Google Scholar]
- Knight M., Bunch K., Vousden N., Morris E., Simpson N., Gale C., et al. Characteristics and outcomes of pregnant women hospitalised with confirmed SARS-CoV-2 infection in the UK: a national cohort study using the UK Obstetric Surveillance System (UKOSS) 2020. https://www.npeu.ox.ac.uk/ukoss
- Lee Y.C., Lin S.J. Neonatal natural killer cell function: relevance to antiviral immune defense. Clin. Dev. Immunol. 2013:427696. doi: 10.1155/2013/427696. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac D., Colquhoun H., O'Brien K.K. Scoping studies: advancing the methodology. Implement. Sci. 2010;5(1):69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li N., Han L., Peng M., Lv Y., Ouyang Y., Liu K., Yue L., Li Q., Sun G., Chen L., Yang L. Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case-control study. Clin. Infect. Dis. 2020 doi: 10.1101/2020.03.10.20033605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Trav. Med. 2020;27:2. doi: 10.1093/jtm/taaa021. Mar 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Wang J., Li W., Zhou Z., Liu S., Rong Z. Clinical characteristics of 19 neonates born to mothers with COVID-19. Front. Med. 2020;14(2):193–198. doi: 10.1007/s11684-020-0772-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe B., Bopp B. COVID-19 vaginal delivery – a case report. Aust. N. Z. J. Obstet. Gynaecol. 2020:1–2. doi: 10.1111/ajo.13173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Q., Shi Y. Coronavirus disease (COVID‐19) and neonate: what neonatologist need to know. J. Med. Virol. 2020;92(6):564–567. doi: 10.1002/jmv.25740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., Yin K. Management of pregnant women infected with COVID-19. Lancet Infect. Dis. 2020;20(5):513–514. doi: 10.1016/S1473-3099(20)30191-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machado J.R., Soave D.F., da Silva M.V., de Menezes L.B., Etchebehere R.M., Monteiro M.L., dos Reis M.A., Corrêa R.R., Celes M.R. Neonatal sepsis and inflammatory mediators. Mediat. Inflamm. 2014:269681. doi: 10.1155/2014/269681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins-Filho P.R., Tanajura D.M. COVID-19 during pregnancy: potential risk for neurodevelopmental disorder in neonates. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020 doi: 10.1016/j.ejogrb.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicines & Healthcare Products Regulatory Agency (MHRA) June 2020. https://www.rpharms.com/Portals/0/RPS%20document%20library/Support%20alert/CMO%20-dexa%20letter.pdf?ver=2020-06-17-092605-187 (viewed 21 June, 2020)
- Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020 doi: 10.1016/S0140-6736(20)30628-0. S0140673620306280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercer J.S., Skovgaard R.L. Neonatal transitional physiology: a new paradigm. J. Perinat. Neonatal Nurs. 2002;15(4):56–75. doi: 10.1097/00005237-200203000-00007. [DOI] [PubMed] [Google Scholar]
- Merle N.S., Noe R., Halbwachs-Mecarelli L., Fremeaux-Bacchi V., Roumenina L.T. Complement system part II: role in immunity. Front. Immunol. 2015;6:257. doi: 10.3389/fimmu.2015.00257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann R.P., von Ungern-Sternberg B.S. The neonatal lung–physiology and ventilation. Pediatr. Anesth. 2014;24(1):10–21. doi: 10.1111/pan.12280. [DOI] [PubMed] [Google Scholar]
- Nuffield Department of Health Low-cost dexamethasone reduces death by up to one third in hospitalised patients with severe respiratory complications of COVID-19. 2020. https://www.recoverytrial.net/news/low-cost-dexamethasone-reduces-death-by-up-to-one-third-in-hospitalised-patients-with-severe-respiratory-complications-of-covid-19 June 16 2020. (viewed 6 July 2020)
- O'Brien K., Robson K., Bracht M., Cruz M., Lui K., Alvaro R., da Silva O., Monterrosa L., Narvey M., Ng E., Soraisham A. Effectiveness of Family Integrated Care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. Lancet Child Adolesc. Health. 2018;2(4):245–254. doi: 10.1016/S2352-4642(18)30039-7. [DOI] [PubMed] [Google Scholar]
- Parrish C.R., Holmes E.C., Morens D.M., Park E.C., Burke D.S., Calisher C.H., Laughlin C.A., Saif L.J., Daszak P. Cross-species virus transmission and the emergence of new epidemic diseases. Microbiol. Mol. Biol. Rev. 2008;72(3):457–470. doi: 10.1128/MMBR.00004-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petty J., Whiting L., Green J., Fowler C. Parents' views on preparation to care for extremely premature infants at home. Nurs. Child. Young People. 2018;30(4):22–27. doi: 10.7748/ncyp.2018.e1084. [DOI] [PubMed] [Google Scholar]
- Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet. 2020;395(10226):760–762. doi: 10.1016/S0140-6736(20)30365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus Disease 2019 (COVID-19) and Pregnancy: What obstetricians need to know. American Journal of Obstetrics and Gynecology. 2020 doi: 10.1016/j.ajog.2020.02.017. https://www.sciencedirect.com/science/article/pii/S0002937820301976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley T., Sully E., Ahmed Z., Biddlecom A. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low- and middle-income countries. Int. Perspect. Sex. Reprod. Health. 2020;46:73–76. doi: 10.1363/46e9020. [DOI] [PubMed] [Google Scholar]
- Roberton T., Carter E.D., Chou V.B., Stegmuller A.R., Jackson B.D., Tam Y., et al. Sawadogo-Lewis T., Walker N. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob. Health. 2020 doi: 10.1016/S2214-109X(20)30229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saikia D., Mahanta B. Cardiovascular and respiratory physiology in children. Indian J. Anaesth. 2019;63(9):690–697. doi: 10.4103/ija.IJA_490_19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6761775/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders-Hastings P.R., Krewski D. Reviewing the history of pandemic influenza: understanding patterns of emergence and transmission. Pathogens. 2016;5(4):66. doi: 10.3390/pathogens5040066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon A.K., Hollander G.A., McMichael A. Evolution of the immune system in humans from infancy to old age. Proc. Biol. Sci. 2015;282:1821. doi: 10.1098/rspb.2014.3085. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4707740/ 20143085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith V., Seo D., Warty R., Payne O., Salih M., Chin K.L., Ofori-Asenso R., Krishnan S., da Silva Costa F., Vollenhoven B., Wallace E. Maternal and neonatal outcomes associated with COVID-19 infection: a systematic review. PloS One. 2020;15(6) doi: 10.1371/journal.pone.0234187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sriram K., Insel E., Loomba R. What is the ACE2 receptor, how is it connected to coronavirus and why might it be key to treating COVID-19? The experts explain. The Conversation. 2020 https://theconversation.com/what-is-the-ace2-receptor-how-is-it-connected-to-coronavirus-and-why-might-it-be-key-to-treating-Covid-19-the-experts-explain-136928 [Google Scholar]
- Strauss-Albee D.M., Liang E.C., Ranganath T., Aziz N., Blish C.A. The newborn human NK cell repertoire is phenotypically formed but functionally reduced. Cytometry B Clin. Cytometry. 2017;92(1):33–41. doi: 10.1002/cyto.b.21485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuebe A. Should infants be separated from mothers with COVID-19? First, do no harm. Breastfeed. Med. 2020;15:5. doi: 10.1089/bfm.2020.29153.ams. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velasco-Aro S.J.G., Sanchez-Mostiero D.O. Should suspected or proven COVID-19 mothers continue to breastfeed their babies? UNICEF. 2020. https://www.unicef.org.uk/babyfriendly/Covid-19/
- Wang S., Guo L., Chen L., Liu W., Cao Y., Zhang J., Feng L. A case report of neonatal COVID-19 infection in China. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 2020 doi: 10.1093/cid/ciaa225. ciaa225. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Qi H., Bao L., Li F., Shi Y. A contingency plan for the management of the 2019 novel coronavirus outbreak in neonatal intensive care units. Lancet Child Adolesc. Health. 2020;4(4):258–259. doi: 10.1016/S2352-4642(20)30040-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Naming the coronavirus disease (COVID-19) and the virus that causes it. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(Covid-2019)-and-the-virus-that-causes-it (viewed 16 June 2020)
- World Health Organization Rolling updates on Coronavirus Disease (COVID-19) 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (viewed 17 June 2020)
- World Health Organization Coronavirus disease (COVID-2019) situation reports. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (viewed 20 June 2020)
- World Health Organisation Clinical management of COVID-19 – interim guidance 27th May 2020 WHO/2019-nCoV/clinical/2020.5. 2020. https://apps.who.int/iris/handle/10665/332196 (viewed 2June 2020)
- World Health Organisation WHO welcomes preliminary results about dexamethasone use in treating critically ill COVID-19 patients. 2020. https://www.who.int/news-room/detail/16-06-2020-who-welcomes-preliminary-results-about-dexamethasone-use-in-treating-critically-ill-covid-19-patients (viewed 21 June 2020)
- Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.2648. https://jamanetwork.com/journals/jama/fullarticle/2762130 [DOI] [PubMed] [Google Scholar]
- Yan J., Guo J., Fan C., Juan J., Yu X., Li J., Feng L., Li C., Chen H., Qiao Y., Lei D. Coronavirus disease 2019 (COVID-19) in pregnant women: a report based on 116 cases. Am. J. Obstet. Gynecol. 2020 doi: 10.1016/j.ajog.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Wang M., Zhu Z., Liu Y. Coronavirus disease 2019a. (COVID-19) and pregnancy: a systematic review. J. Matern. Fetal Neonatal Med. 2020:1–4. doi: 10.1080/14767058.2020.1759541. [DOI] [PubMed] [Google Scholar]
- Yang P., Wang X., Liu P., Wei C., He B., Zheng J., Zhao D. Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. J. Clin. Virol. 2020:104356. doi: 10.1016/j.jcv.2020.104356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J.C., Khodadadi H., Malik A., Davidson B., Salles É.D.S.L., Bhatia J., Hale V.L., Baban B. Innate immunity of neonates and infants. Front. Immunol. 2018;9:1759. doi: 10.3389/fimmu.2018.01759. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6077196/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu N., Li W., Kang Q., Xiong Z., Wang S., Lin X., Liu Y., Xiao J., Liu H., Deng D., Chen S. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaigham M., Andersson O. Maternal and perinatal outcomes with COVID‐19: a systematic review of 108 pregnancies. Acta Obstet. Gynecol. Scand. 2020:1–7. doi: 10.1111/aogs.13867. 00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamaniyan M., Ebadi A., Mir S.A., Rahmani Z., Haghshenas M., Azizi S. Preterm delivery in pregnant woman with critical COVID‐19 pneumonia and vertical transmission. Prenat. Diagn. 2020 doi: 10.1002/pd.5713. https://penta-id.org/Covid-19-publications/preterm-delivery-in-pregnant-women-with-critical-Covid-19-pneumonia-and-vertical-transmission/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, Kim KD, Yang X, Auh S, Fu YX, Tang H. Hyper innate responses in neonates lead to increased morbidity and mortality after infection. Proceedings of the National Academy of Sciences. 2008;105(21):7528–7533. doi: 10.1073/pnas.0800152105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng S., Fan J., Yu F., Feng B., Lou B., Zou Q., Xie G., Lin S., Wang R., Yang X., Chen W. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study. BMJ. 2020;369 doi: 10.1136/bmj.m1443. https://www.bmj.com/content/369/bmj.m1443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman P, Curtis N. COVID-19 in children, pregnancy and neonates: a review of epidemiologic and clinical features. The Pediatric Infectious Disease Journal. 2020;39(6):469–477. doi: 10.1097/INF.0000000000002700. [DOI] [PMC free article] [PubMed] [Google Scholar]