Abstract
Borderline personality disorder (BPD) involves instability in self-concept, emotions, and behavior. However, the dynamic, longitudinal relations among BPD symptoms and between these symptoms and other problematic emotional experiences are poorly understood. It is also unclear whether these dynamics are the same across persons (including across diagnostic boundaries), specific to individuals with BPD, or idiographic. The current study uses ecological momentary assessment and group iterative multiple model estimation, a novel, data-driven approach to identifying dynamic patterns in time-series data at group, subgroup, and individual levels, to investigate the dynamic connections among select features of BPD (anger, impulsivity, and identity disturbance) and anxiety-related experiences. Forty-two psychiatric outpatients diagnosed with BPD (n = 27) or with an anxiety disorder, but not BPD (n = 15), rated their anger, identity disturbance, impulsivity, anxiety, stress, and calmness states 6 times per day for 21 days, providing a total of 4,699 surveys. Only 1 dynamic link between symptoms was identified that applied at the group level, and group iterative multiple model estimation did not reveal stable subgroups of individuals with distinct symptom dynamics. Instead, these dynamics differed from individual to individual. These results suggest that connections among these BPD and anxiety symptoms do not depend on diagnosis and are somewhat idiographic. Case examples are used to illustrate the clinical utility of within-person symptom models as a supplement to traditional diagnostic information.
Keywords: person-specific modeling, borderline personality disorder, ecological momentary assessment, comorbidity, symptom networks
Borderline personality disorder (BPD) is a costly, debilitating, and common psychiatric disorder. Studies estimate its prevalence at about 2% of the general population (Lenzenweger, Lane, Loranger, & Kessler, 2007; Trull, Jahng, Tomko, Wood, & Sher, 2010). Individuals with BPD are common in clinical practice, making up about 10–20% of psychiatric outpatients (Korzekwa, Dell, Links, Thabane, & Webb, 2008; Zimmerman, Rothschild, & Chelminski, 2005). BPD is also highly comorbid with other disorders, particularly anxiety disorders, mood disorders, substance use disorders, and other personality disorders (Grant et al., 2008; Zanarini, Frankenburg, Hennen, Reich, & Silk, 2004; Zimmerman & Mattia, 1999).
One aspect of BPD that is particularly poorly understood is how different aspects of the disorder relate to one another and to features of other disorders. BPD consists of a diverse set of cognitive, affective, and behavioral experiences, suggesting a high degree of underlying complexity. Perhaps due to this complexity, many studies of the relations among different BPD symptoms have focused on a limited set of these features at a time, often in laboratory settings where researchers have induced a BPD-related experience and compared the outcomes between BPD and non-BPD groups. For example, several studies have examined links between negative emotionality (induced fear or anger, or measured negative affect) and impulsivity, and the ways in which these links depend on features of BPD or on the diagnosis itself (see Sebastian, Jacob, Lieb, & Tüscher, 2013, for a review). Findings from this literature are equivocal as to the connections between negative emotionality and impulsivity, with some studies showing positive links (Chapman, Dixon-Gordon, Layden, & Walters, 2010; Chapman, Leung, & Lynch, 2008; Silbersweig et al., 2007; Tomko et al., 2015) and some studies showing no such link (Domes et al., 2006; Jacob et al., 2013; Lawrence, Allen, & Chanen, 2010). The results of these studies also do not correspond as to the specificity of these links; some found that a BPD diagnosis, or an elevated score on a dimensional BPD measure, made connections between anger and impulsivity more likely in comparison with healthy control participants or those with other diagnoses (Chapman et al., 2008, 2010; Silbersweig et al., 2007), whereas others did not (Jacob et al., 2013; Tomko et al., 2015).
However, anger and impulsivity have rarely been studied in BPD samples in naturalistic contexts, meaning that there is a paucity of information about how these symptoms relate in everyday life. The literature relating BPD symptoms to one another has some other important limitations, as well. One shortcoming is that these studies have generally been confined only to BPD symptoms and do not consider links between BPD symptoms and features of other commonly comorbid disorders. However, researchers are increasingly conceptualizing symptoms of putatively discrete disorders as transdiagnostic entities, either within dimensional taxonomies of psychopathology (Kotov et al., 2017) or as “bridge symptoms” connecting networks of maladaptive experiences (Fried et al., 2017). Taking such a perspective may thus illuminate processes that underpin psychopathology more broadly and may help explain the high levels of comorbidity between BPD and other disorders.
A more fundamental limitation of prior studies on symptom relationships in BPD is that each is restricted to interindividual (i.e., between-person), groupwise analyses. However, structures uncovered from between-person analyses are conceptually (Borsboom, Mellenbergh, & van Heerden, 2003; Molenaar, 2004; Roche, Pincus, Rebar, Conroy, & Ram, 2014) and empirically (Beckmann, Wood, & Minbashian, 2010; Dowgwillo et al., 2019; Ram, Brinberg, Pincus, & Conroy, 2017; Roche, Pincus, Hyde, Conroy, & Ram, 2013; Yang et al., 2018) distinct from processes uncovered from within-subjects analyses. If theories of symptom interrelationships are meant to apply within subjects, cross-sectional analyses cannot test them directly. For models describing dynamics occurring within individuals, within-person analytic approaches are required (Hamaker & Wichers, 2017).
One important, additional implication of the divergence between intraindividual and interindividual variation is that dynamics among symptoms may be idiographic to some degree (Molenaar, 2004; Piccirillo & Rodebaugh, 2019). Due to the possibility of idiography in the structures and processes underlying BPD, we argue that it is prudent to base models of the dynamics among BPD symptoms on a within-person basis at the outset, rather than relying on an assumption of homogeneity in these processes (Molenaar & Campbell, 2009). Commonalities across individuals can then be derived empirically based on similarities in the person-specific models. In this way, generalizations to larger groups of individuals can be made. Group iterative multiple model estimation (GIMME), which was originally developed to model common, subgroup, and idiographic patterns in functional neuroimaging data, has recently been extended to ecological momentary assessment (EMA) data contexts (Lane, Gates, Pike, Beltz, & Wright, 2019). GIMME is a novel person-specific analytic approach that uncovers the contemporaneous and lagged dynamics in multivariate time series data and allows for individuals to be aggregated on the basis of patterns that they share (Gates, Lane, Varangis, Giovanello, & Guskiewicz, 2017). However, to date it has not been applied to symptom relationships in BPD.
Current Study
The primary aim of the current study was to use GIMME to characterize the dynamic connections among selected features of BPD and anxiety disorders, as the links among these features (both within and across disorder categories) are unclear from prior theory and research. Data were drawn from a larger study aimed at investigating the validity of EMA assessment in outpatients with BPD or with anxiety disorders. In this larger study, BPD features of anger, impulsivity, and identity disturbance were chosen to exemplify the emotional, behavioral, and identity-related features of this complex disorder. The larger study also included questions about experiences related to anxiety. The current study thus explores the dynamics among these features of BPD and these anxiety-related experiences.
A key aim of the current study was to demonstrate the viability and utility of within-person analyses such as GIMME to examine intraindividual dynamics of psychopathology. In doing so, we specifically sought to determine the extent to which links among BPD and anxiety features were similar for every individual, were similar for subgroups of individuals, or were unique for each individual on an idiographic basis. For example, it may be the case that increases in anger increase the likelihood of impulsive urges, that increases in impulsivity make subsequent anger more likely, or both (as in a positive feedback loop). It is also possible that both of these dynamics operate, but separately and in different individuals. We therefore used GIMME to explore the nomothetic and idiographic relations among these experiences. A secondary aim of the study was to investigate whether any identified subgroup structure in these symptom dynamics related to Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnoses of BPD and anxiety disorders based on semistructured interviews.
Method
Participants
Participants were adult individuals participating in outpatient treatment at a community mental health center that is the primary training clinic for a doctoral program in clinical psychology. They were recruited for a broader study focused on the predictive validity of smartphone-based assessments (for more details, see Dowgwillo et al., 2019; Scala et al., 2018). To be eligible, participants had to be aged at least 18 years; could not be diagnosed with schizophrenia, schizoaffective disorder, delusional disorder, delirium, dementia, amnestic disorder, cognitive disorder not otherwise specified, mental retardation, or borderline intellectual disability; and had to self-report normal or corrected-to-normal vision (to read questionnaires on the smartphone’s LCD screen). Participants had to be diagnosed either with BPD or with an anxiety disorder (but not BPD). Fifty-five individuals met these criteria and began the smartphone portion of the protocol. Of these, 13 participants (n = 8 with BPD) discontinued the study before submitting at least 60 survey responses (range = 8–58 surveys) and were excluded. The remaining 42 participants, 27 with BPD and 15 without BPD, constitute the sample for the current study. Demographic and diagnostic information for the sample can be found in Table 1.
Table 1.
Demographic and Diagnostic Characteristics of the Current Sample (N = 42)
| Characteristic | N | % | M | SD |
|---|---|---|---|---|
| Age | 32.55 | 11.28 | ||
| Female | 38 | 90.5 | — | — |
| Primary ethnicity | ||||
| African American | 1 | 2.4 | — | — |
| Asian American | 1 | 2.4 | — | — |
| Caucasian | 37 | 88.1 | — | — |
| Other | 3 | 7.1 | — | — |
| Global assessment of functioning | 56.20 | 10.50 | ||
| Current DSM–IV Axis I diagnoses | ||||
| Major depressive disorder | 31 | 75.6 | — | — |
| Generalized anxiety disorder | 9 | 22.0 | — | — |
| Social phobia | 8 | 19.5 | — | — |
| Posttraumatic stress disorder | 6 | 14.6 | — | — |
| Alcohol abuse | 3 | 7.3 | — | — |
| Alcohol dependence | 3 | 7.3 | — | — |
| Anxiety disorder NOS | 3 | 7.3 | — | — |
| Somatization disorder | 3 | 7.3 | — | — |
| Current DSM–IV Axis II diagnoses | ||||
| Borderline personality disorder | 27 | 64.3 | — | — |
| Avoidant personality disorder | 4 | 9.8 | — | — |
| Antisocial personality disorder | 2 | 4.9 | — | — |
| Histrionic personality disorder | 2 | 4.9 | — | — |
| Obsessive–compulsive personality disorder | 2 | 4.9 | — | — |
| Paranoid personality disorder | 2 | 4.9 | — | — |
| Personality disorder NOS | 2 | 4.9 | — | — |
Note. DSM–IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; NOS = not otherwise specified.
Procedure
All procedures received approval from the university’s institutional review board. After being recruited and assessed for eligibility, participants received training in the use of the smartphone device. For 21 days following this laboratory session, they completed three kinds of smartphone surveys: in response to block-randomized auditory prompts from the device (“prompted surveys”), after interpersonal interactions lasting at least 3 min (“event-contingent surveys”), and at the end of each day. The three types of surveys varied in their content, and the current report only concerns the prompted surveys. Participants received six prompts per day to complete surveys, each of which occurred at a pseudorandom time within a 2-hr block during the overall 12-hr interval. Participants were compensated for completion of training and baseline assessments. Participants were also given a prorated amount for each day of study participation, with a bonus for returning surveys for at least 18 days; the maximum compensation for EMA surveys was $100.
Materials
Diagnostic interviews
Participants completed semistructured diagnostic interviews as part of their clinic intake or as part of previous institutional review board-approved research studies. Those recruited for the study from clinic intakes (n = 32) were diagnosed with Axis I disorders using an augmented version of the Anxiety Disorders Interview Schedule (Brown, DiNardo, & Barlow, 1994), a semistructured interview for the diagnosis of mood, eating, somatoform, psychotic, anxiety, and substance use disorders. Individuals recruited from previous research studies (n = 10) were diagnosed with Axis I disorders using the Structured Clinical Interview for DSM–IV Axis I Disorders, Clinician Version (First, Spitzer, Gibbon, & Williams, 1997), a semistructured interview covering mood, psychotic, substance use, anxiety, somatoform, and eating disorders. All individuals in the sample were diagnosed with personality disorders using the International Personality Disorders Examination (IPDE; Loranger, 1999), a semistructured interview for the DSM–IV/DSM–5 personality disorders.
All interviewers were advanced graduate students in clinical psychology who were trained to reliability in diagnostic interviewing as part of the core doctoral program. Interviews were videotaped. Taped interviews in the lab studies from which 10 participants were drawn were coded by a second rater, with substantial to excellent interrater reliability (κ = 0.67 to 1.0, with κ = 0.89 for a BPD diagnosis; Beeney, Hallquist, Ellison, & Levy, 2016). Although none of the interviews for individuals recruited from the clinic were double-rated, interrater reliability in the clinic, based on secondary coding of videotaped interviews, is generally substantial (κ = 0.62 on average, with κ = 0.66 for anxiety disorders and κ = 0.68 for BPD).
Prompted smartphone surveys
Participants completed six prompted smartphone surveys per day, which contained 46 questions and were designed to take about 5 min to complete. Prompts were block-pseudorandomized to occur at unpredictable occasions within separate 2-hr blocks, which were arranged according to each participant’s typical waking schedule. Questions queried about current affect, symptoms and functioning, repetitive thoughts, cravings to use substances, self-control capacity, values, thoughts of suicidality and self-harm, and self-concept. The current study concerns questions relating to three symptoms of BPD (anger, impulsivity, and identity disturbance) and three experiences related to anxiety: anxiety, stress, and calmness.
For each item, a visual analog scale on the touch-sensitive screen of the smartphone was used to record responses, which were encoded as an integer value from 0 to 100. Numerical values were not visible to participants. Anger was assessed with the prompt, “How angry do you feel right now?” with response anchors from not at all to extremely. Impulsivity was assessed with the prompt, “Please rate how you see yourself RIGHT NOW using the following scales” with response anchors from impulsive to in control. Identity disturbance was assessed with the prompt, “RIGHT NOW I have a clear sense of who I am and what I am” with response anchors of strongly disagree and strongly agree. For the latter two items, responses were reverse-scored so that higher scores represented more impulsivity and identity disturbance, respectively. Anxiety was assessed with the prompt, “Right now, my anxiety is” with response anchors from mild to severe. Stress was assessed with the prompt, “Right now, my stress is” with anchors low and high. Calmness was assessed with the prompt, “How calm do you feel right now?” with response anchors from not at all to extremely.
Data Analysis
Group iterative multiple model estimation
Model fitting was conducted in R software, Version 3.5.0, using the GIMME package (Lane et al., 2018). GIMME works within a structural equation modeling framework to identify group, subgroup, and person-specific patterns in time-series data, including EMA data (Lane et al., 2019). Importantly for EMA applications, estimation in GIMME occurs using full information maximum likelihood and thus is relatively robust to data missingness (Enders & Bandalos, 2001; Lane & Gates, 2017). Because participants did not complete surveys at night, leading to unequal intervals in the time series, missing-data rows were added between days to constrain estimation to within-day effects. Importantly, individuals were only considered if they had returned at least 60 surveys, as recommended by Lane and Gates (2017).
Model elements (contemporaneous regression parameters and parameters with a lag of one occasion) were assigned to the overall group if they were statistically significant for at least 75% of the time series of individuals in the sample. Subgroups (distinct clusters of individuals) were sought via the Walktrap algorithm, an approach to community detection in networks based on random walks (Pons & Latapy, 2005). In GIMME, paths within subgroups are estimated uniquely for each individual but must improve the majority of individuals’ models within the subgroup (Gates et al., 2017; Lane et al., 2019). Individual models were estimated containing group-level and subgroup-level parameters, along with person-specific elements derived from each individual’s multivariate time series.
Evaluation of cluster stability
Two methods were used to evaluate the robustness of cluster solutions. First, the modularity index (Q; Newman & Girvan, 2004) was examined, which ranges from 0 (random community structure) to 1 (strongest community structure). Values for networks with strong community structure typically fall in the range of 0.3 to 0.7 (Newman & Girvan, 2004). Second, the perturbR package (Gates, Fisher, & Arizmendi, 2018) was used to incrementally change the values of the “edges” in the subgroup networks’ matrices. The variation of information (VI; Meilă, 2007) resulting from this network perturbation was compared with the VI obtained from randomly altering nodes (rather than edges) in the original matrix. Strong community structure is shown when about as many edges as nodes must be perturbed to achieve a given VI (Karrer, Levina, & Newman, 2008). A recent article using simulations and empirical examples supports the utility of this second method of evaluating cluster stability (Gates et al., 2019).
Results
Compliance With Prompted Surveys
Compliance was measured as the percentage of the expected 126 prompted surveys (21 days with six surveys per day) completed. Participants who began the smartphone portion of the study returned 74% of the expected surveys, on average (M = 92.7 surveys, SD = 39.21, Mdn = 109). Excluding dropouts, participants returned an average of 89% of the expected surveys (M = 111.8 surveys, SD = 15.60, Mdn = 115). There was no relation between diagnostic group and dropout, χ2(1) = 0.115, p = .73, nor was there a difference in overall compliance between those with BPD (M = 113.9, SD = 12.74) and those with an anxiety disorder (ANX; M = 107.6, SD = 20.06), t(40) = 1.23, p = .23, d = 0.37, 95% CI [−6.08, 18.58].
Results of GIMME
The GIMME procedure produced a convergent solution for all 42 participants. However, one individual in the ANX group showed poor fit on all fit indices, and an examination of this individual’s data suggested that this individual’s time series contained very low variability (e.g., out of 86 surveys, 85 had values of 0 for identity disturbance, and 84 had values of 0 for impulsivity). Therefore, this individual was removed from further analyses, leaving a sample of 41 in the final analysis for GIMME.
Group parameters
Only one parameter was identified that applied at the group level: After controlling for its lagged influence on itself, stress level was predicted by the amount of anxiety reported in the same survey (average β = 0.47; p values < .05 for 36 out of 41 participants, or 88%). After the groupwise link between anxiety and stress, the most common connection was a contemporaneous link between identity disturbance and impulsivity, with 27 individuals (66%; n = 20 with BPD) showing a significant positive regression β in either direction (average value = 0.49) and one person showing a significant negative link (β = −0.42). The remaining 14 individuals had a nonsignificant connection between these two values in contemporaneous surveys.
Subgroups
Four subgroups were identified by GIMME on the basis of dynamic relations among symptoms. These subgroups contained 17, 13, two, and four members, respectively. An additional two individuals in the sample were not identified as belonging to any subgroup. Importantly, subgroups did not differ in terms of the mean level of identity disturbance, anger, impulsivity, anxiety, stress, or calmness in EMA ratings (all p values > 0.2), highlighting that GIMME groups individuals on the basis of the time series’ covariation, not the elevation of these symptoms. However, the modularity of the subgroup solution was very low (Q = 0.02). In addition, perturbing only 3% of the edges in these networks resulted in a VI that exceeded that obtained by altering group membership for 20% of the individuals in the sample. These results both indicate that the clusters of individuals identified by GIMME were unreliable and should not be interpreted as evidence of the existence of any natural clusters in the dynamics of the EMA data. Because of the instability of the community structure, we did not proceed to compare the clusters identified by GIMME and the diagnostic groups delineated by the semistructured interviews, because this comparison would not be meaningful.
Individual results
In contrast to the subgroup structure, the individual within-person models identified by GIMME were robust, showing good fit for all individuals (see Table 2). These models showed a high degree of heterogeneity: contemporaneous and lagged relationships among features of BPD and anxiety varied from individual to individual. Figure 1 shows a summary of the parameters contained in the within-person models across individuals. To illustrate the diversity of the dynamic links among anger, impulsivity, identity disturbance, anxiety, stress, and calmness for different individuals, and to highlight the potential for these models to aid in case conceptualization and clinical intervention for individuals on a person-specific basis, we describe three individuals and their models in the following text.
Table 2.
Demographic and Diagnostic Information and Fit Statistics
| ID | Age | Gender | Group | χ2 | df | p | CFI | NNFI | RMSEA | SRMR |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 52 | F | BPD | 43.81 | 41 | .35 | 0.995 | 0.992 | 0.0233 | 0.067 |
| 2 | 48 | F | BPD | 53.40 | 40 | .08 | 0.965 | 0.941 | 0.0477 | 0.0639 |
| 3 | 44 | F | BPD | 40.93 | 33 | .16 | 0.978 | 0.956 | 0.0427 | 0.0546 |
| 4 | 50 | F | BPD | 66.97 | 40 | .005 | 0.973 | 0.956 | 0.0696 | 0.0713 |
| 5 | 39 | F | BPD | 48.37 | 38 | .12 | 0.954 | 0.920 | 0.0441 | 0.0623 |
| 6 | 25 | F | BPD | 48.02 | 36 | .09 | 0.974 | 0.953 | 0.0517 | 0.1029 |
| 7 | 48 | F | BPD | 57.20 | 39 | .03 | 0.979 | 0.965 | 0.0577 | 0.0611 |
| 8 | 38 | F | BPD | 45.49 | 38 | .19 | 0.985 | 0.975 | 0.0381 | 0.0601 |
| 9 | 40 | F | BPD | 48.44 | 39 | .14 | 0.975 | 0.958 | 0.0400 | 0.0604 |
| 10 | 46 | F | BPD | 54.19 | 31 | .01 | 0.978 | 0.954 | 0.0723 | 0.1101 |
| 11 | 34 | F | BPD | 48.28 | 36 | .08 | 0.979 | 0.962 | 0.0494 | 0.0457 |
| 12 | 60 | M | BPD | 57.36 | 40 | .04 | 0.975 | 0.959 | 0.0533 | 0.0857 |
| 13 | 27 | F | BPD | 54.52 | 42 | .09 | 0.955 | 0.929 | 0.0444 | 0.0609 |
| 14 | 21 | F | BPD | 41.93 | 38 | .30 | 0.961 | 0.932 | 0.0276 | 0.069 |
| 15 | 21 | F | BPD | 47.29 | 37 | .12 | 0.977 | 0.959 | 0.0461 | 0.0636 |
| 16 | 21 | F | BPD | 42.86 | 36 | .20 | 0.977 | 0.958 | 0.0409 | 0.0748 |
| 17 | 29 | F | BPD | 54.19 | 40 | .07 | 0.965 | 0.942 | 0.0488 | 0.0707 |
| 18 | 19 | F | BPD | 41.57 | 40 | .40 | 0.995 | 0.992 | 0.0194 | 0.0715 |
| 19 | 28 | F | BPD | 54.16 | 40 | .07 | 0.973 | 0.956 | 0.0489 | 0.0902 |
| 20 | 24 | F | BPD | 62.94 | 38 | .007 | 0.978 | 0.962 | 0.0673 | 0.0454 |
| 21 | 47 | F | BPD | 46.67 | 40 | .22 | 0.978 | 0.964 | 0.0381 | 0.0739 |
| 22 | 40 | F | BPD | 45.37 | 40 | .26 | 0.990 | 0.983 | 0.0319 | 0.0699 |
| 23 | 39 | M | BPD | 51.79 | 40 | .10 | 0.981 | 0.968 | 0.0473 | 0.0668 |
| 24 | 48 | F | BPD | 55.47 | 38 | .03 | 0.978 | 0.962 | 0.0575 | 0.0557 |
| 25 | 19 | F | BPD | 47.62 | 39 | .16 | 0.977 | 0.962 | 0.044 | 0.0585 |
| 26 | 21 | F | BPD | 52.73 | 41 | .10 | 0.954 | 0.926 | 0.0469 | 0.0685 |
| 27 | 21 | F | BPD | 49.56 | 37 | .08 | 0.972 | 0.951 | 0.05 | 0.0631 |
| 28 | 32 | F | ANX | 45.40 | 38 | .19 | 0.986 | 0.975 | 0.0408 | 0.05 |
| 29 | 21 | F | ANX | 45.52 | 38 | .19 | 0.984 | 0.972 | 0.0408 | 0.0624 |
| 30 | 32 | M | ANX | 47.12 | 41 | .24 | 0.968 | 0.949 | 0.0316 | 0.1005 |
| 31 | 20 | F | ANX | 43.48 | 39 | .29 | 0.978 | 0.963 | 0.0339 | 0.1044 |
| 32 | 30 | F | ANX | 53.32 | 41 | .09 | 0.958 | 0.932 | 0.0457 | 0.0741 |
| 33 | 36 | F | ANX | 50.13 | 37 | .07 | 0.968 | 0.943 | 0.0483 | 0.07 |
| 34 | 21 | F | ANX | 51.18 | 39 | .09 | 0.987 | 0.977 | 0.0492 | 0.0446 |
| 35 | 45 | F | ANX | 51.24 | 37 | .06 | 0.977 | 0.959 | 0.0571 | 0.0518 |
| 36 | 20 | F | ANX | 48.66 | 40 | .16 | 0.959 | 0.933 | 0.0396 | 0.0862 |
| 37 | 21 | M | ANX | 46.43 | 37 | .14 | 0.959 | 0.926 | 0.0497 | 0.0770 |
| 38 | 22 | F | ANX | 49.67 | 41 | .17 | 0.972 | 0.955 | 0.0384 | 0.0665 |
| 39 | 25 | F | ANX | 54.32 | 37 | .03 | 0.967 | 0.941 | 0.0562 | 0.0452 |
| 40 | 27 | F | ANX | 39.63 | 39 | .44 | 0.997 | 0.995 | 0.0139 | 0.0715 |
| 41 | 32 | F | ANX | 47.92 | 41 | .21 | 0.988 | 0.981 | 0.0348 | 0.0720 |
Note. CFI = comparative fit index; NNFI = nonnormed fit index; RMSEA = root mean square error of approximation; SRMR = standardized root mean square residual; BPD = borderline personality disorder; ANX = anxiety disorder.
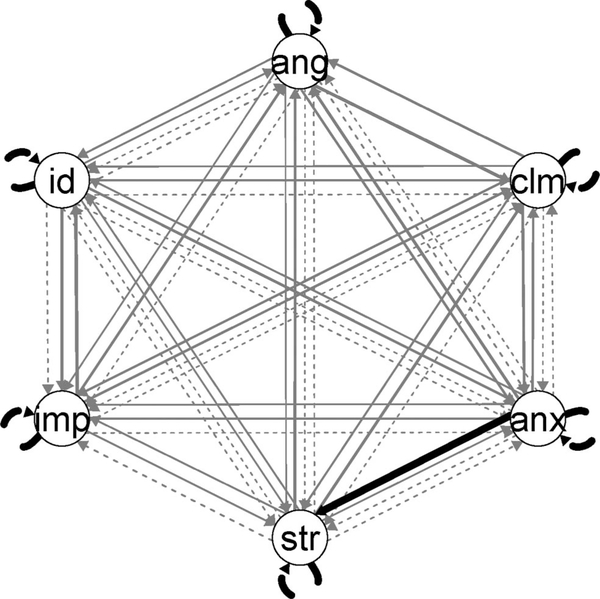
Figure 1.
Path diagram summarizing the contemporaneous (solid lines) and lagged (dashed lines) connections among items across participants. Black lines indicate parameters assigned to the group; gray lines indicate parameters assigned to individual models. The thickness of gray lines corresponds to the number of individual models containing the parameter. ang = anger; clm = calmness; anx = anxiety; str = stress; imp = impulsivity; id = identity disturbance.
Participant 32
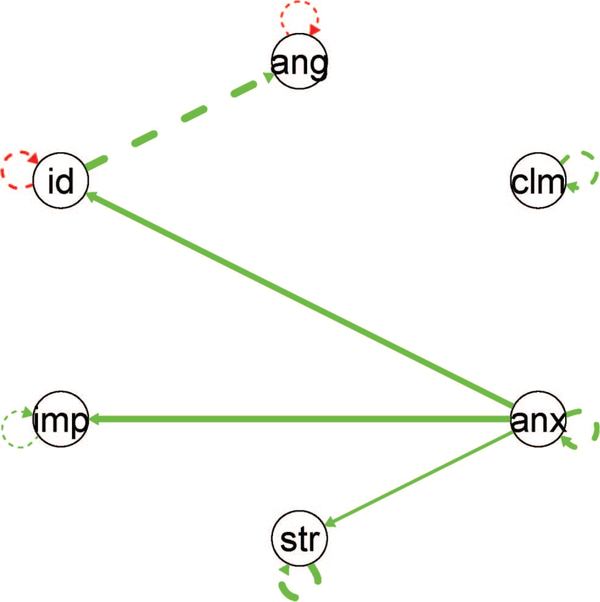
Participant 32 was a 30-year-old married White woman diagnosed with major depressive disorder, social phobia, and generalized anxiety disorder. She did meet two BPD criteria: affective instability and nonsuicidal self-injury. Notably, she was diagnosed with personality disorder not otherwise specified. In line with her diagnosis of social phobia and generalized anxiety disorder, Participant 32’s model suggests that moment-tomoment anxiety experiences played an important role in the fluctuation of other symptoms (see Figure 2). The more anxious she was, the more she felt stressed, b = 0.18, Z = 2.57, p = .01, impulsive, b = 0.54, Z = 7.98, p < .001, and unsure of who she was, b = 0.44, Z = 5.80, p < .001, controlling for the lagged influences these latter experiences had on themselves. In addition, Participant 32’s level of identity disturbance predicted her level of anger approximately 2 hr later, b = 0.65, Z = 11.91, p < .001.
Figure 2.
Path diagram of the contemporaneous (solid lines) and lagged (dashed lines) connections among items for Participant 32. Green (light gray) lines represent positive links, and red (dark gray) lines are negative links. The thickness of lines corresponds to the strength of the connection. ang = anger; clm = calmness; anx = anxiety; str = stress; imp = impulsivity; id = identity disturbance. See the online article for the color version of this figure.
Participant 19
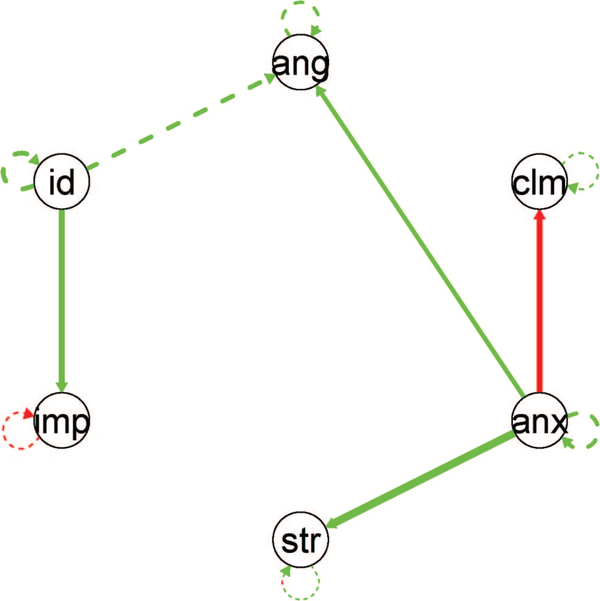
Participant 19 was a 28-year-old single White woman diagnosed with somatoform disorder and with BPD. She met six criteria for BPD via the IPDE (identity disturbance, impulsivity, suicidality, affective instability, emptiness, and transient paranoia/dissociation). Figure 3 shows this person’s individual solution. For her, identity disturbance predicted later increases in anger, b = 0.35, Z = 4.30, p < .001. In addition, after controlling for its lagged influence on itself, impulsivity was predicted by the level of identity disturbance at the same occasion, b = 0.54, Z = 8.46, p < .001. A contemporaneous link was also uncovered between anxiety and anger, b = 0.34, Z = 4.84, p < .001. That is, controlling for the autoregressive relationship of anger between surveys, Participant 19 tended to be angrier if she also reported higher anxiety at that survey.
Figure 3.
Path diagram of the contemporaneous (solid lines) and lagged (dashed lines) connections among items for Participant 19. Green (light gray) lines represent positive links, and red (dark gray) lines are negative links. The thickness of lines corresponds to the strength of the connection. ang = anger; clm = calmness; anx = anxiety; str = stress; imp = impulsivity; id = identity disturbance. See the online article for the color version of this figure.
Participant 10
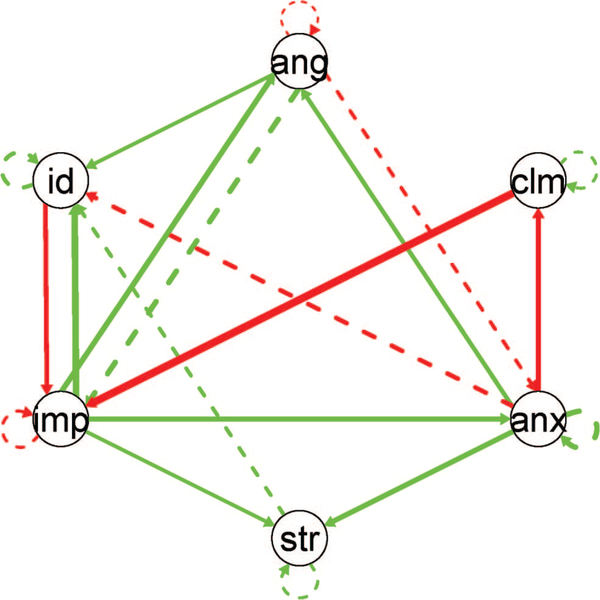
Participant 10 was a 46-year-old married White woman diagnosed with BPD, having met six criteria for the disorder on the IPDE: unstable relationships, identity disturbance, chronic suicidal ideation/behavior, affective instability, chronic emptiness, and anger. In contrast to many individuals with BPD, she did not meet criteria for any other DSM–IV disorders. For Participant 10, dysregulated emotional experiences served as predictors of behavioral dysregulation and identity disturbance 2 hr later (i.e., at a lag of one survey). In particular, stress predicted identity disturbance 2 hr later, b = 0.28, Z = 2.62, p = .009, and anger predicted the participant’s level of impulsivity across this lag, b = 0.49, Z = 3.98, p < .001. Contemporaneous connections within this individual’s symptom network also suggested that her experience of negative affect is imbued with impulsive urges, as indicated by the strong connections between feelings of anxiety (b = 0.48, Z = 6.18, p < .001), calmness (b = −0.51, Z = 7.02, p < .001), anger (b = 0.50, Z = 5.32, p < .001), and stress (b = 0.47, Z = 5.96, p < .001) and impulsive states. Interestingly, for Participant 10, anxiety negatively predicted momentary identity disturbance 2 hr later, b = − 0.40, Z = 3.45, p < .001. Figure 4 shows this participant’s model.
Figure 4.
Path diagram of the contemporaneous (solid lines) and lagged (dashed lines) connections among items for Participant 10. Green (light gray) lines represent positive links, and red (dark gray) lines are negative links. The thickness of lines corresponds to the strength of the connection. ang = anger; clm = calmness; anx = anxiety; str = stress; imp = impulsivity; id = identity disturbance. See the online article for the color version of this figure.
Discussion
Results from the current study provide preliminary evidence that naturally occurring dynamic links among identity disturbance, anger, impulsivity, anxiety, stress, and calmness are not the same for every individual. There was only one “nomothetic” connection between these experiences (in the sense of applying to the general case). Moreover, these connections did not differ systematically between BPD and anxiety-disordered groups, and no robust community structure was identified in these models. Instead, connections among these six experiences differed from individual to individual in terms of their presence, strength, direction, and speed (i.e., contemporaneous or lagged).
These results provide important qualifications to existing studies of interrelationships among BPD symptoms. Not only do within-person processes differ from the structures identified in cross-sectional analyses, but the dynamics among BPD symptoms may differ from person to person as well. For both of these reasons, the apparent importance of a particular BPD symptom in a study of nomothetic (i.e., groupwise or between-subjects) relationships should not be understood to mean that this symptom is causally relevant for any particular individual. This general result may help to explain why studies of the links between individual symptoms (such as impulsivity and emotion dysregulation) are inconsistent: It may be that these dynamics are fundamentally and meaningfully different across individuals, and the average result of any given study depends on the frequency with which individuals with different processes appear in different samples.
The diversity of links among features of BPD and anxiety disorders implies that there may be subpopulations of individuals who meet DSM–5 criteria for BPD and who nonetheless are not well described by the same model of the disorder’s mechanisms. Whereas the current study did not uncover direct evidence of subgroups, we think it is likely that distinct clusters may be uncovered eventually, because only a subset of all possible causal relations among BPD symptoms is psychologically plausible. For example, frantic efforts to avoid abandonment are probably more likely to result from relationship instability, abandonment fears, or alternating between idealizing and devaluing close others than from impulsivity. Future studies with a broader palette of BPD-relevant experiences and larger sample sizes will be needed to test these propositions, however. Moreover, we expect that diverse explanations of comorbidity between BPD and anxiety disorders may be required, as the “bridge symptoms” between syndromes may also differ from person to person.
The largely idiographic nature of the links uncovered in the current analyses highlights the immediate clinical relevance of within-person analyses of symptom covariation. As opposed to diagnoses, which are based on levels or counts of symptoms, it may be important to distinguish individuals by the dynamic covariation of their symptoms as well. Such analyses have several potential applications within clinical work. For example, analyses of dynamic covariation could be used to provide prescriptive, individualized recommendations for one therapy over another, depending on the processes that are targeted by different interventions (Fisher, 2015; Fisher & Boswell, 2016; Roche et al., 2014). This application has been referred to as “precision diagnosis” (van Os, Delespaul, Wigman, Myin-Germeys, & Wichers, 2013), “precision assessment” (Roche & Pincus, 2016), and “personalized network modeling” (Epskamp et al., 2018). For example, a treatment that focuses on emotion regulation, such as dialectical behavior therapy (DBT; Linehan, 1993), might be a good treatment for Participant 10, because it is more likely that her self-concept disturbance and impulsive behaviors are the result of affective instability and anger than the other way around, given her individual model. If DBT were successfully used to reduce her anger and emotion dysregulation, it is possible that changes in identity disturbance and impulsivity would follow. On the other hand, for Participant 19, the current results might suggest prescribing a treatment focused on identity disturbance (such as transferencefocused psychotherapy; Yeomans, Clarkin, & Kernberg, 2015), because bolstering this participant’s identity might lead to decreases in her levels of anger. Participant 32 did not have BPD, but she did meet two criteria for the disorder and had significant personality pathology (as indicated by her personality disorder not otherwise specified diagnosis); nonetheless, her model suggests that a therapy targeting anxiety might be most helpful, as it might ameliorate not only her core complaint (pathological anxiety) but also these personality problems. In general, if individuals do not exhibit the same pathological processes, clinicians should pay attention to each client’s particular symptom dynamics rather than relying on nomothetically derived models of pathology (Hopwood et al., 2016), as treatments based on these general models are unlikely to be relevant for some people. The current findings thus bolster the perspective of researchers who have advocated for a person-specific approach to diagnosis and psychological assessment, based on reciprocal interactions between affective states and behaviors instead of solely on symptom checklists or evaluations of mean symptom levels (Hopwood, 2018; Hopwood, Pincus, & Wright, 2019; Pincus & Hopwood, 2012; Roche et al., 2014; van Os et al., 2013).
In addition to treatment prescription, the use of within-person modeling has the potential to augment existing clinical practices within empirically supported treatments. For example, DBT already has therapists and clients monitor different phenomena as they unfold over time, using diary cards. However, the process of gathering these data can be lengthy. Using data-collection and data-analytic procedures such as the ones in the present article could lend statistical rigor to behavioral chain analyses in DBT and improve their efficiency. In general, a personalized approach may aid in case formulation, allowing therapists to prioritize certain interventions over others. For example, Participant 10’s results suggest that two potentially fruitful therapeutic goals for this individual would be to reduce negative affect (so as to promote adaptive behavior regulation and a coherent sense of self) and to work to decouple impulsivity from anger and anxiety. These goals presumably could be accommodated within several existing treatments for BPD. In other words, the most effective interventions might not simply focus on the most problematic or elevated symptoms; they might also target the phenomena that give rise to (or maintain) them for that person. Thus, within-person models of symptom covariation might profitably be used as supplements to traditional diagnostic information (e.g., Wright & Zimmermann, 2019; Zimmermann et al., 2019).
A few limitations of the current study deserve mention. One potential limitation is the frequency and scope of the observations taken during the EMA sampling period. To accurately model processes of interest, data must be collected at an adequate frequency (Collins, 2006). The 2-hr interval between observations in the current study may mean that important processes that occurred at a greater frequency were not captured. Additionally, symptoms were sampled over a limited time (21 days), raising the possibility that some rare but clinically significant events (and thus dynamics of potential interest) may not have occurred in this timespan. That is, whereas self-report measures can rely on an individual’s memory for important events and their contexts, EMA with random sampling intervals does not. It is thus possible that longer sampling periods, or protocols with higher frequency sampling, might identify different patterns than those obtained here and may indeed allow meaningful subgroups to be identified as a result. Second, the sample size of the current study was small (in terms of individuals, if not in terms of overall observations). This also may have made it more difficult to detect meaningful subgroups in the dynamic patterns here. The fact that the current analyses only used three BPD symptoms and three anxiety symptoms may have also contributed to the lack of identifiable community structure; future research with an expanded list of items may be more successful in detecting robust subgroups in BPD/anxiety dynamics. It is also possible that more distinct subgroups may emerge from samples with different diagnostic characteristics (e.g., a BPD group and a group with major depression). For all these reasons, the current results with respect to subgroups should be considered preliminary. A third limitation of the current study is that GIMME assumes “weak stationarity” of the processes of interest (Lane & Gates, 2017), or stability of item means and covariances. This may be problematic given that the individuals in the sample were in active treatment, which may have affected the means and covariances of these symptoms over the 3-week EMA period. Finally, measurement in the EMA portion of the study, as in many EMA studies, was confined to self-report and to one item per construct. These measurement limitations may have hampered the reliability and validity of the current findings, to some degree.
Given the prevalence of BPD as well as its debilitating nature and its direct and indirect costs, it is vital to understand it properly and to treat it effectively. The current study is, to our knowledge, the first to apply within-subject modeling to BPD symptom data gathered through EMA. As such, it presents a statistically rigorous method for modeling dynamic processes of the disorder and exemplifies methods that may be useful in clinical research and practice. Future research will be needed to extend the current models to other BPD symptoms and symptoms of other disorders and to evaluate their clinical utility.
Acknowledgments
This research was supported in part by grants from the Pennsylvania State University Social Sciences Research Institute, the Pennsylvania State University Research and Graduate Studies Office, the American Psychoanalytic Association, and the International Psychoanalytical Association. We thank J. Wesley Scala and Emily A. Dowgwillo for their assistance in developing training material and coordinating the collection of data; Benjamin N. Johnson for coordinating the collection of data; Kathleen Bohomey, Colin Carey, Caroline Curran, Wendi Falk, Sarah Forsythe, Laura Frey, Caroline Gooch, Jessica Grom, Brittani Hollern, Lauren Lipner, Kristin McLaughlin, Megan Moyer, Joanna Pantelides, Megan Parker, Jacqueline Proczynski, Carolina Ribo, Silvia Rizkallah, Aimee Sohnleitner, and Alyssa Spaw for their assistance in data collection; and Jennifer Fox and Allison Clark for their assistance in the recruitment of participants. We also thank Kathleen M. Gates for her assistance with the data analytic method.
Contributor Information
William D. Ellison, Department of Psychology, Trinity University
Kenneth N. Levy, Department of Psychology, Pennsylvania State University
Michelle G. Newman, Department of Psychology, Pennsylvania State University
Aaron L. Pincus, Department of Psychology, Pennsylvania State University
Stephen J. Wilson, Department of Psychology, Pennsylvania State University
Peter C. M. Molenaar, Department of Human Development and Family Studies, Pennsylvania State University
References
- Beckmann N, Wood RE, & Minbashian A (2010). It depends how you look at it: On the relationship between neuroticism and conscientiousness at the within- and between-person levels of analysis. Journal of Research in Personality, 44, 593–601. 10.1016/j.jrp.2010.07.004 [DOI] [Google Scholar]
- Beeney JE, Hallquist MN, Ellison WD, & Levy KN (2016). Self-other disturbance in borderline personality disorder: Neural, selfreport, and performance-based evidence. Personality Disorders, 7, 28–39. 10.1037/per0000127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Mellenbergh GJ, & van Heerden J (2003). The theoretical status of latent variables. Psychological Review, 110, 203–219. 10.1037/0033-295X.110.2.203 [DOI] [PubMed] [Google Scholar]
- Brown T, DiNardo P, & Barlow D (1994). Anxiety Disorders Interview Schedule, Adult Version. Oxford, UK: Oxford University Press. [Google Scholar]
- Chapman AL, Dixon-Gordon KL, Layden BK, & Walters KN (2010). Borderline personality features moderate the effect of a fear induction on impulsivity. Personality Disorders, 1, 139–152. 10.1037/a0019226 [DOI] [PubMed] [Google Scholar]
- Chapman AL, Leung DW, & Lynch TR (2008). Impulsivity and emotion dysregulation in borderline personality disorder. Journal of Personality Disorders, 22, 148–164. 10.1521/pedi.2008.22.2.148 [DOI] [PubMed] [Google Scholar]
- Collins LM (2006). Analysis of longitudinal data: The integration of theoretical model, temporal design, and statistical model. Annual Review of Psychology, 57, 505–528. 10.1146/annurev.psych.57.102904.190146 [DOI] [PubMed] [Google Scholar]
- Domes G, Winter B, Schnell K, Vohs K, Fast K, & Herpertz SC (2006). The influence of emotions on inhibitory functioning in borderline personality disorder. Psychological Medicine, 36, 1163–1172. 10.1017/S0033291706007756 [DOI] [PubMed] [Google Scholar]
- Dowgwillo EA, Pincus AL, Newman MG, Wilson SJ, Molenaar PCM, & Levy KN (2019). Two methods for operationalizing the interpersonal situation to investigate personality pathology and interpersonal perception in daily life In Truslow LI & Rahmaan JM (Eds.), Personality disorders: What we know and future directions for research (pp. 31–106). Hauppauge, NY: Nova Science Publishers. [Google Scholar]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8, 430–457. 10.1207/S15328007SEM0803_5 [DOI] [PubMed] [Google Scholar]
- Epskamp S, van Borkulo CD, van der Veen DC, Servaas MN, Isvoranu A-M, Riese H, . . . Cramer AOJ (2018). Personalized network modeling in psychopathology: The importance of contemporaneous and temporal connections. Clinical Psychological Science, 6, 416–427. 10.1177/2167702617744325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1997). Structured Clinical Interview for DSM–IV Axis I Disorders: Clinician version. Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Fisher AJ (2015). Toward a dynamic model of psychological assessment: Implications for personalized care. Journal of Consulting and Clinical Psychology, 83, 825–836. 10.1037/ccp0000026 [DOI] [PubMed] [Google Scholar]
- Fisher AJ, & Boswell JF (2016). Enhancing the personalization of psychotherapy with dynamic assessment and modeling. Assessment, 23, 496–506. 10.1177/1073191116638735 [DOI] [PubMed] [Google Scholar]
- Fried EI, van Borkulo CD, Cramer AOJ, Boschloo L, Schoevers RA, & Borsboom D (2017). Mental disorders as networks of problems: A review of recent insights. Social Psychiatry and Psychiatric Epidemiology, 52, 1–10. 10.1007/s00127-016-1319-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates KM, Fisher Z, & Arizmendi C (2018). Package ‘perturbR’ (Version 0.1.2) [Computer software]. Retrieved from https://cran.r-project.org/web/packages/perturbR/index.html
- Gates KM, Fisher ZF, Arizmendi C, Henry TR, Duffy KA, & Mucha PJ (2019). Assessing the robustness of cluster solutions obtained from sparse count matrices. Psychological Methods. Advance online publication. 10.1037/met0000204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates KM, Lane ST, Varangis E, Giovanello K, & Guskiewicz K (2017). Unsupervised classification during time-series model building. Multivariate Behavioral Research, 52, 129–148. 10.1080/00273171.2016.1256187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, . . . Ruan WJ (2008). Prevalence, correlates, disability, and comorbidity of DSM–IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 69, 533–545. 10.4088/JCP.v69n0404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamaker EL, & Wichers M (2017). No time like the present: Discovering the hidden dynamics in intensive longitudinal data. Current Directions in Psychological Science, 26, 10–15. 10.1177/0963721416666518 [DOI] [Google Scholar]
- Hopwood CJ (2018). Interpersonal dynamics in personality and personality disorders. European Journal of Personality, 32, 499–524. 10.1002/per.2155 [DOI] [Google Scholar]
- Hopwood CJ, Pincus AL, & Wright AGC (2019). The interpersonal situation: Integrating personality assessment, case formulation, and intervention In Samuel D & Lynam D (Eds.), Using basic personality research to inform personality pathology (pp. 94–121). New York, NY: Oxford University Press. [Google Scholar]
- Hopwood CJ, Thomas KM, Luo X, Bernard N, Lin Y, & Levendosky AA (2016). Implementing dynamic assessments in psychotherapy. Assessment, 23, 507–517. 10.1177/1073191116649658 [DOI] [PubMed] [Google Scholar]
- Jacob GA, Zvonik K, Kamphausen S, Sebastian A, Maier S, Philipsen A, . . . Tüscher O (2013). Emotional modulation of motor response inhibition in women with borderline personality disorder: An fMRI study. Journal of Psychiatry and Neuroscience, 38, 164–172. 10.1503/jpn.120029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karrer B, Levina E, & Newman MEJ (2008). Robustness of community structure in networks. Physical Review E, 77, Article ID 046119. 10.1103/PhysRevE.77.046119 [DOI] [PubMed] [Google Scholar]
- Korzekwa MI, Dell PF, Links PS, Thabane L, & Webb SP (2008). Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Comprehensive Psychiatry, 49, 380–386. 10.1016/j.comppsych.2008.01.007 [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, . . . Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. 10.31234/osf.io/zaadn [DOI] [PubMed] [Google Scholar]
- Lane S, Gates K, Molenaar P, Hallquist M, Pike H, Fisher Z, . . . Henry T (2018). Package ‘gimme’ (Version 0.4–2) [Computer software]. Retrieved from https://cran.r-project.org/web/packages/gimme/index.html
- Lane ST, & Gates KM (2017). Automated selection of robust individual-level structural equation models for time series data. Structural Equation Modeling, 24, 768–782. 10.1080/10705511.2017.1309978 [DOI] [Google Scholar]
- Lane ST, Gates KM, Pike HK, Beltz AM, & Wright AGC (2019). Uncovering general, shared, and unique temporal patterns in ambulatory assessment data. Psychological Methods, 24, 54–69. 10.1037/met0000192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence KA, Allen JS, & Chanen AM (2010). Impulsivity in borderline personality disorder: Reward-based decision-making and its relationship to emotional distress. Journal of Personality Disorders, 24, 786–799. 10.1521/pedi.2010.24.6.785 [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Lane MC, Loranger AW, & Kessler RC (2007). DSM–IV personality disorders in the National Comorbidity Survey replication. Biological Psychiatry, 62, 553–564. 10.1016/j.biopsych.2006.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM (1993). Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- Loranger AW (1999). International personality disorder examination. Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Meilă M (2007). Comparing clusterings—An information based distance. Journal of Multivariate Analysis, 98, 873–895. 10.1016/j.jmva.2006.11.013 [DOI] [Google Scholar]
- Molenaar PCM (2004). A manifesto on psychology as an idiographic science: Bringing the person back into scientific psychology, this time forever. Measurement, 2, 201–218. [Google Scholar]
- Molenaar PCM, & Campbell CG (2009). The new person-specific paradigm in psychology. Current Directions in Psychological Science, 18, 112–117. 10.1111/j.1467-8721.2009.01619.x [DOI] [Google Scholar]
- Newman MEJ, & Girvan M (2004). Finding and evaluating community structure in networks. Physical Review E, 69, Article ID 026113. 10.1103/PhysRevE.69.026113 [DOI] [PubMed] [Google Scholar]
- Piccirillo ML, & Rodebaugh TL (2019). Foundations of idiographic methods in psychology and applications for psychotherapy. Clinical Psychology Review, 71, 90–100. 10.1016/j.cpr.2019.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincus AL, & Hopwood CJ (2012). A contemporary interpersonal model of personality pathology and personality disorder In Widiger TA (Ed.), Oxford handbook of personality disorders (2nd ed., pp. 372–398). New York, NY: Oxford University Press. [Google Scholar]
- Pons P, & Latapy M (2005). Computing communities in large networks using random walks In Yolum P, Güngör T, Gürgen F, & Özturan C (Eds.), Computer and information sciences: ISCIS 2005 (pp. 284–293). Berlin, Germany: Springer; 10.1007/11569596_31 [DOI] [Google Scholar]
- Ram N, Brinberg M, Pincus AL, & Conroy DE (2017). The questionable ecological validity of ecological momentary assessment: Considerations for design and analysis. Research in Human Development, 14, 253–270. 10.1080/15427609.2017.1340052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche MJ, & Pincus AL (2016). Precision assessment: An individualized and temporally dynamic approach to understanding patients in their daily lives In Kumar U (Ed.), The Wiley handbook of personality assessment (pp. 192–204). Hoboken, NJ: Wiley Blackwell; 10.1002/9781119173489.ch14 [DOI] [Google Scholar]
- Roche MJ, Pincus AL, Hyde AL, Conroy DE, & Ram N (2013). Within-person covariation of agentic and communal perceptions: Implications for interpersonal theory and assessment. Journal of Research in Personality, 47, 445–452. 10.1016/j.jrp.2013.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche MJ, Pincus AL, Rebar AL, Conroy DE, & Ram N (2014). Enriching psychological assessment using a person-specific analysis of interpersonal processes in daily life. Assessment, 21, 515–528. 10.1177/1073191114540320 [DOI] [PubMed] [Google Scholar]
- Scala JW, Levy KN, Johnson BN, Kivity Y, Ellison WD, Pincus AL, . . . Newman MG (2018). The role of negative affect and self-concept clarity in predicting self-injurious urges in borderline personality disorder using ecological momentary assessment. Journal of Personality Disorders, 32, 36–57. 10.1521/pedi.2018.32.supp.36 [DOI] [PubMed] [Google Scholar]
- Sebastian A, Jacob G, Lieb K, & Tüscher O (2013). Impulsivity in borderline personality disorder: A matter of disturbed impulse control or a facet of emotional dysregulation? Current Psychiatry Reports, 15, 339 10.1007/s11920-012-0339-y [DOI] [PubMed] [Google Scholar]
- Silbersweig D, Clarkin JF, Goldstein M, Kernberg OF, Tuescher O, Levy KN, . . . Stern E (2007). Failure of frontolimbic inhibitory function in the context of negative emotion in borderline personality disorder. The American Journal of Psychiatry, 164, 1832–1841. 10.1176/appi.ajp.2007.06010126 [DOI] [PubMed] [Google Scholar]
- Tomko RL, Lane SP, Pronove LM, Treloar HR, Brown WC, Solhan MB, . . . Trull TJ (2015). Undifferentiated negative affect and impulsivity in borderline personality and depressive disorders: A momentary perspective. Journal of Abnormal Psychology, 124, 740–753. 10.1037/abn0000064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Jahng S, Tomko RL, Wood PK, & Sher KJ (2010). Revised NESARC personality disorder diagnoses: Gender, prevalence, and comorbidity with substance dependence disorders. Journal of Personality Disorders, 24, 412–426. 10.1521/pedi.2010.24.4.412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J, Delespaul P, Wigman J, Myin-Germeys I, & Wichers M (2013). Beyond DSM and ICD: Introducing “precision diagnosis” for psychiatry using momentary assessment technology. World Psychiatry, 12, 113–117. 10.1002/wps.20046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, & Zimmermann J (2019). Applied ambulatory assessment: Integrating idiographic and nomothetic principles of measurement. Psychological Assessment. Advance online publication. 10.1037/pas0000685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X, Ram N, Gest SD, Lydon-Staley DM, Conroy DE, Pincus AL, & Molenaar PCM (2018). Socioemotional dynamics of emotion regulation and depressive symptoms: A person-specific network approach. Complexity, 2018, Article ID 5094179. 10.1155/2018/5094179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeomans FE, Clarkin JF, & Kernberg OF (2015). Transference-focused psychotherapy for borderline personality disorder: A clinical guide. Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, & Silk KR (2004). Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. The American Journal of Psychiatry, 161, 2108–2114. 10.1176/appi.ajp.161.11.2108 [DOI] [PubMed] [Google Scholar]
- Zimmerman M, & Mattia JI (1999). Axis I diagnostic comorbidity and borderline personality disorder. Comprehensive Psychiatry, 40, 245–252. 10.1016/S0010-440X(99)90123-2 [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Rothschild L, & Chelminski I (2005). The prevalence of DSM–IV personality disorders in psychiatric outpatients. The American Journal of Psychiatry, 162, 1911–1918. 10.1176/appi.ajp.162.10.1911 [DOI] [PubMed] [Google Scholar]
- Zimmermann J, Woods WC, Ritter S, Happel M, Masuhr O, Jaeger U, . . . Wright AGC (2019). Integrating structure and dynamics in personality assessment: First steps toward the development and validation of a personality dynamics diary. Psychological Assessment, 31, 516–531. 10.1037/pas0000625 [DOI] [PubMed] [Google Scholar]