INTRODUCTION
The transplant community is well-versed in ethical issues surrounding the allocation of scarce resources, but the COVID-19 pandemic has escalated moral dilemmas of transplantation far beyond simply allocation of limited donor organs. Emanuel et al1 were unfortunately prophetic in their recent NEJM article addressing the ethical principles guiding medical decisions during the COVID-19 pandemic and the associated depletion of resources. Hospital and intensive care resources are becoming severely limited in high-transmission areas, influencing decisions about who should be transplanted and affecting the availability of donated organs.2 The risk of COVID-19 transmission to donors and recipients further alters such risk considerations. Pre–COVID-19 organ allocation schemes, which are complex, transparent, and organ-specific, are by themselves insufficient to determine who should be transplanted under such conditions, particularly in resource-constrained areas.
Complex ethical considerations for transplantation during such a pandemic will inherently vary greatly by country, region, and culture—and be dynamic over time, and affected by both COVID-19 disease burden and trajectory. But the broad principles of nonmaleficence, beneficence, distributive justice, and respect for autonomy must continue to guide these difficult decisions. Nonmaleficence, for example, may dictate that living donor operations be held in heavily affected areas because of the potential risk of COVID-19 infection in donors. Indeed the same concern applies to transplant recipients, whose immunosuppression may put them at increased risk of infection posttransplant. Conversely, beneficence might suggest that successful kidney transplantation could, in addition to its other benefits, prevent the need for further dialysis center visits, potentially reducing the risk of nosocomial COVID-19 transmission. From a distributive justice perspective, by contrast, programs may need to curtail certain transplant activity simply as a result of resource constraints imposed by an overwhelming pandemic disease burden. Finally, autonomy dictates that programs communicate both the known and unknown risks of COVID-19 infection—and the policies we are each enacting as a result—to their transplant patients allowing them to make informed decisions about their care.
The urgent need to adapt rapidly during the COVID-19 pandemic has challenged traditional dependence on evidence-based data and peer-reviewed literature. Healthcare workers in transplantation are being asked to navigate our patients through a minefield in the absence of conventional pillars that usually guide clinical management and decisions. For treatment protocols, we traditionally rely on approaches that have undergone a thorough evaluation, testing, and review process. In the absence of such an opportunity for gradual and deliberate review, professional societies around the world have been quick to collaborate and share their global experiences,3 and the distribution of information has largely shifted to rapid, online platforms. In making decisions during this uncertain time, it is essential that our own uncertainty, lack of knowledge, and lack of prognostic ability about the pandemic disease course are recognized and factored into our risk-benefit analyses as well as our respect for the patient’s autonomy.
The availability of resources for transplantation is a moving target in the COVID-19 pandemic, dependent on the position of each region and country on the COVID incidence curve, and its baseline access to healthcare resources (Figure 1). While decisions must be based on available and expected resources, they must also be informed by underlying ethical values that have been and will continue to be the rationale for all our patient-care decisions.
FIGURE 1.
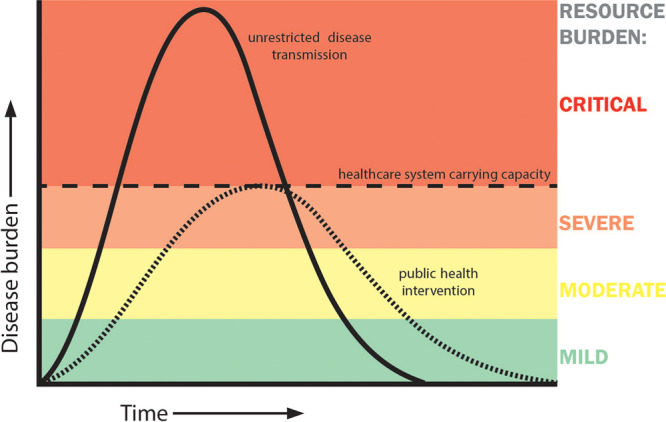
Responses on allocation, donor/recipient criteria, and transplant activities will largely depend on the position of centers on the slope of the incidence curve. Geographic and social characteristics will also determine the height of the curve, impacting risk-benefit assessments.
RECIPIENT SELECTION AND PROGRAMMATIC POLICIES
In the current global snapshot,3 programs in affected areas have been remarkably consistent in distributive justice-based decisions about which patients to transplant. Their approaches begin with practical accounting for availability of essential resources such as ventilators, ICU beds, or blood products required for successful transplantation, availability of COVID-19 free facilities for the immediate posttransplant recovery period, and availability of personal protective equipment (PPE). Of course, the prepandemic starting point of available resources in each region will impact the threshold for transplantation, and there are many places that cannot consider transplantation with any additional strain on the system. After determining who can be transplanted, programs have generally addressed the question of who should be transplanted using the principle of distributive justice to maximize benefits, minimize resource utilization, and treat the highest-need patients first. Programs are also making new risk-benefit calculations by trying to best evaluate how to apply the principles of beneficence and nonmaleficence in the setting of COVID-19. Finally, allocation decisions that are made at the programmatic level often do not account for the individual patient’s desire to be transplanted despite the risk of COVID-19, and therefore, risk placing autonomy behind the overriding principles of distributive justice, beneficence, and nonmaleficence. The relative weight of these factors may be influenced by the estimated position of each center and region on the COVID-19 incidence curve and relative to the available healthcare resources (Figure 1).
For regions early on the ascending portion of the COVID-19 incidence curve, representing mild to moderate resource constraints, transplantation decisions are guided by anticipating future resource limitations and infectious risks and are weighted toward autonomy, nonmaleficence, and beneficence. For kidney transplantation, for example, many centers are selecting recipients with fewer comorbidities who are unlikely to require prolonged hospitalization or the need for ICU beds. This resource-distribution strategy favors patients likely to benefit from transplantation while utilizing fewer resources and minimizing the risk of nosocomial recipient COVID-19 infection.
Other programs have favored reliance on nonmaleficence as the driving principle of kidney transplant allocation because precise risks and benefits of kidney transplantation in this setting remain both highly dynamic and poorly characterized. Patients with end-stage renal disease, for example, may survive for many years on dialysis, albeit with less quality of life and longevity than following successful transplantation. Given the alternative of dialysis, many programs globally have suspended kidney transplantation based on this principle, reasoning that transplantation in the midst of the COVID-19 pandemic may do more harm than good. Several assumptions underpin this decision: that harms may indeed be great if COVID-19 infection is transmitted by an infected donor or acquired by the recipient in hospital or community during maximal infection, and that the incidence and outcomes of COVID-19 infection are less frequent and less lethal among dialysis patients than kidney transplant recipients. Given the potential for the pandemic to run a protracted and potentially recurrent course, testing the validity of these assumptions through research will be a priority.
Similarly, using the considerations of maximizing benefit, minimizing risk and limiting resource use, simultaneous pancreas/kidney transplants have been suspended by many programs, based on the length of anticipated hospitalization and the likelihood of readmission in hospitals that may be filled to capacity, with high potential risk for COVID-19 exposure. Programs suspending simultaneous pancreas/kidney transplants have decided that the risks of infection and resource utilization outweigh the potential benefits of transplantation, making a decision based on both distributive justice and nonmaleficence.
A unique consideration focused on beneficence and nonmaleficence is an assessment of whether the intended recipient can effectively quarantine after discharge. This makes social considerations all the more pressing in transplant selection, but importantly, while such postdischarge social distancing and quarantine considerations are critical in selection, it is essential that these considerations do not disadvantage certain categories of patients who are already vulnerable. During this challenging COVID-19 era of decreased medical resources, we must maintain a particular focus on disadvantaged populations to ensure equal access to medical care. Programs should also strive to help support social distancing, whether by reducing clinic visits or blood draws, promoting telehealth opportunities where available, or coordinating social and community support mechanisms.
As COVID-19 disease burden increases (moderate-severe resource burden, Figure 1), many centers have shifted their ethical framework toward distributive justice considerations, focusing on more urgent patients in greatest need. For example, some programs have limited liver transplantation to candidates with Model for End-Stage Liver Disease (MELD) scores reflective of poor 3-month survival without transplantation, heart transplantation for intermediate- and high-risk patients, and lung transplantation for unstable patients. Of note, some regions have also seen the beneficial effects of public health interventions with flattening the disease incidence curve (dotted line, Figure 1). In these regions, decisions about which patients to transplant may differ from those in regions at a similar level of resource-deprivation but on a different trajectory. Thus, real-time assessment, not just of resources on hand but also estimated disease trajectory, is essential in appropriate planning for all such ethically guided considerations.
As the incidence for COVID-19 increases and the resource burden from infectious disease alone approaches the critical threshold of consuming the entire capacity of the system (Figure 1, critical burden), programs shift their distributive justice considerations from urgent to only emergent transplants. At this point, transplantation is limited to only the most emergent cases (ie, fulminant liver failure, highest acuity heart transplantation, and decompensated patients for lung transplantation), and above this threshold, all transplantation is held based on an absolute lack of resources including ventilators, blood products, and PPE.2 At this point care systems are forced to make the most difficult decisions about which patients have claim to limited resources. While it might seem natural to shift all resources to COVID-19, this strategy disadvantages other patients with equally life-threatening conditions, such as end-organ failure. It is, therefore, essential that the sickest transplant patients continue to be considered in resource-allocation schemes because of their equal need for medical care as compared to critically ill COVID-19 patients.
Encouragingly, as COVID-19 incidence has begun to decline in some geographic areas, transplant centers in these regions appear to be cautiously resuming practices from the pre–COVID-19 era. Centers and regions emerging from the pandemic will have to determine how to gradually resume transplants in a graded fashion based on capacity, resources, and considerations of other patient needs—as well as factoring in the possibility of COVID-19 recurrence, with bimodal or even multimodal incidence curves. We expect that overall operative volumes will also increase given the backlog of elective and urgent procedures, so the needs of transplant patients will have to be balanced with other patients requiring time-sensitive intervention (eg, cancer, cardiac, or vascular patients). Thus, there will likely be continuing constraints on operating room capacity. In turn, this will influence when and how full transplant activity, and living donation in particular, can be reinstated.
It is becoming increasingly clear that resumption of transplant practices (and all medical practices) will be contingent on availability of COVID-19 testing for donors, recipients, and healthcare practitioners. While the availability for testing that includes a detection of COVID-19 nucleic acid or antibodies has improved in some but not all geographic areas, the sensitivity and specificity of these tests still vary. Programs will have to apply distributive justice principles for scaling up volume, determining whether to focus on maximizing benefit while minimizing resource use. They will also have to continue to evaluate the risk of COVID-19 infection in recipients as new data emerges on therapeutics, outcomes in transplant patients, and testing capabilities to make accurate judgments based on beneficence and nonmaleficence.
DONOR ACCEPTANCE AND CONSIDERATIONS
Decisions to accept organs from deceased donors have also been significantly affected by the COVID-19 pandemic. Many centers have been hesitant to use marginal/extended criteria grafts, believing these transplants are more likely to result in delayed function and increased resource utilization. Many centers also require donor and recipient testing for COVID-19 before organ offer acceptance.3 In addition, donor procurement operations are frequently being done by local surgeons rather than travel teams when possible to decrease the risks of exposure. As a result, some programs, particularly those that commonly perform their own donor operations, may be hesitant to accept offers because of the inability to assess the donor organs in person. The risks of prolonged hospitalization and increased resource utilization associated with extended criteria grafts are taking precedence over the risk of organ failure.
Further, where resources are constrained at recipient hospitals, it is likely that the same will be true at donor hospitals. In this setting, centers and healthcare systems need to determine if those resources being used for donor care—ICU beds, nursing care, PPE, medications, and operating room time—are needed for the care of other patients. If so, their use for donor care may be in conflict. Donors are normally prioritized for such resources because a single donor can save multiple lives, and the donor often occupies those ICU resources for only a short time. As recipient operations are curtailed to only those in greatest need during this pandemic, the ability of a single donor to acutely save multiple lives becomes all the more evident.
Thus, if resources permit the continued transplantation of recipients in acute need, donor care should be prioritized wherever possible because of the potential to maximize lives saved during the pandemic. Allocation of organs should be done as expeditiously as possible to minimize the burden of donor care on the system. Similarly, as resources become constrained, procurement organizations may need to become more selective in donor workup, and prioritize only those donors healthy enough to provide multiorgan donation. Ultimately, as resource constraints become critical, difficult decisions may need to be made by each center, including even halting deceased-donor care and procurement—but knowing that this also means losing the supply of life-saving organs and recognizing that critically ill transplant patients have an equally legitimate claim to scarce resources when compared to critically ill COVID-19 patients.1
Living donation is also being evaluated differently in COVID-19 affected regions. As the regional incidence of COVID-19 increases and resources necessary for safe transplantation are depleted, many centers have stopped living donation related to the risks of exposing healthy donors to COVID-19 during their hospitalizations, and due to the potential risk for asymptomatic donor disease transmission to recipients. In these decisions, nonmaleficence is taking precedence over autonomy, meaning that the risk of harm is perceived to be too great to offer the option of living donation to individual potential donors. To decrease the risk of harm, donor and recipient COVID-19 testing are necessary for any center continuing to perform living donation in this era. In areas of high prevalence, even these measures may be insufficient for harm mitigation, given the nonzero risk of nosocomial infection and the nonzero false-negative rate of testing.
TRANSPARENCY AND COMMUNICATION
Organ supply has run behind demand for decades. Allocation has thus traditionally been based on transparent and clear communication providing patients, providers, and the community with a framework on how to deal with fair distribution of a scarce resource. While the current crisis has not changed national allocation systems, the allocation decisions about which patients to transplant have shifted to regional and program levels. These decisions utilize different material principles of distributive justice, depending on the status of that region and its position on the COVID-19 incidence curve. Because programs are constantly adapting to the changing environment, decisions about which patients will be considered for transplantation will continue to evolve, making it all the more important to assure continuing public and patient confidence in the system with transparency and consistency. For those centers that decide to systematically pause or alter the transplantation patterns of certain waitlisted patients, centers should officially notify their patients. This approach has been selected by some institutions particularly for simultaneous kidney/pancreas, pancreas after kidney, or pancreas alone transplants.
As most centers have applied more nuanced center-specific modifications to donor and recipient criteria, it is also important to update patients and providers on these developments as they occur. Such communication should provide clear information on temporary changes to selection and allocation approaches, in a language facilitating general insight on the reasons behind these decisions. Moreover, programs must determine the best way to communicate both the known and unknown risks of COVID-19 infection with patients who are being considered for a transplant so that patients can make informed decisions consistent with their personal goals and values. Clear communication with waitlisted patients about programmatic changes during the shifting risk-landscape of the COVID-19 pandemic will allow transplant programs to maintain respect for patient autonomy as well as patient trust during this critical time.
Transparency in communication is not only critical for the trust and effective flow of information between providers and patients but also between government healthcare agencies and transplant providers. Accurate reporting of the incidence of COVID-19, real-time and realistic appraisals of the current and expected availability of resources, and effective strategies to alter the course of the pandemic should be shared across regions within and between countries. COVID-19 does not recognize borders or discriminate between countries and continents, and this pandemic has demonstrated unequivocally that global cooperation is imperative to blunt its devastating impact. As one such mechanism for facilitating international collaboration and coordination, The Transplantation Society is currently providing an online dashboard of up-to-date global information and experience in response to the crisis (https://tts.org/covid-19).
CONCLUSIONS
The same ethical principles that have always been used to guide transplant practices continue to apply during the COVID-19 era, but the balance between autonomy, beneficence, nonmaleficence, and justice will be inherently fluid, dependent on baseline resources, local practices, and where a given region resides—and is headed—on the COVID-19 incidence curve (Figure 1).4 Programmatic decisions about transplantation will weigh more heavily on distributive justice, beneficence and nonmaleficence than respect for autonomy. The overriding material principle of distributive justice will change, and be weighted more or less heavily, throughout the stages of the incidence curve based on available resources. Beneficence and nonmaleficence calculations must be continually reassessed as more data become available regarding the risk of COVID-19 infections in transplant patients, the availability and accuracy of testing, and the efficacy of new therapeutic modalities. While the complexity, threats, and consequences of COVID-19 are immense, it is reassuring to see the transplant and medical communities rallying together in such a time, and to see, as a result, such thoughtful and consistent responses to dealing with this situation around the globe. Putting aside the jargon of classical medical ethics, these global responses reflect the straightforward principles of doing the right thing for our patients, at the right time, for the right reasons.
APPENDIX
Rudolf Garcia-Gallont: Hospital San Juan de Dios Guatemala, Guatemala City, Guatemala. Kristof Van Assche: University of Antwerp, Antwerp, Belgium, Riadh Abdul Sattar Fadhil: Qatar Organ Donation Center-Hiba, Doha, Qatar. Elizabeth A. Pomfret: University of Colorado School of Medicine and UC Health, Denver, United States. Adibul Hasan Rizvi: Sindh Institute of Urology and Transplantation (SIUT), Karachi, Pakistan. Adisorn Lumpaopong: Bangkok Hospital, Bangkok, Thailand. Patrizia Burra: Universita Degli Studi Di Padova, Padova, Italy. Alejandro Niño-Murcia: Colombiana de Trasplantes, Bogota, Colombia. Ifeoma Ulasi: University of Nigeria Teaching Hospital, Ituku-Ozalla, Nigeria. Haibo Wang: Peking University, China. Richard Allen: University of Sydney, Sydney, Australia.
Footnotes
A list of all the TTS Ethics Committee participants is given in the Appendix.
The authors declare no funding or conflicts of interest.
REFERENCES
- 1.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Eng J Med. 2020; 382:2049–2055. doi:10.1056/NEJMsb2005114 [DOI] [PubMed] [Google Scholar]
- 2.Kumar D, Manuel O, Natori Y, et al. COVID-19: a global transplant perspective on successfully navigating a pandemic. Am J Transplant. [Epub ahead of print March 23, 2020]. doi:10.1111/ajt.15876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahn C, Amer H, Anglicheau D, et al. Global transplantation COVID report March 2020. Transplantation. [Epub ahead of print April 1, 2020]. doi:10.1097/TP.0000000000003258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Organ Procurement and Transplantation Network. Ethical principles in the allocation of human organs. 2018 Available at https://optn.transplant.hrsa.govresourcesethicsethical-principles-in-the-allocation-of-human-organs. Accessed March 27, 2020.


