Supplemental Digital Content is available in the text.
Keywords: children and adults, coronavirus disease 2019, pediatric intensive care units, quality
Objectives:
There are limited reports of the impact of the coronavirus disease 2019 pandemic focused on U.S. and Canadian PICUs. This hypothesis-generating report aims to identify the United States and Canadian trends of coronavirus disease 2019 in PICUs.
Design and Setting:
To better understand how the coronavirus disease 2019 pandemic was affecting U.S. and Canadian PICUs, an open voluntary daily data collection process of Canadian and U.S. PICUs was initiated by Virtual Pediatric Systems, LLC (Los Angeles, CA; http://www.myvps.org) in mid-March 2020. Information was made available online to all PICUs wishing to participate. A secondary data collection was performed to follow-up on patients discharged from those PICUs reporting coronavirus disease 2019 positive patients.
Measurements and Main Results:
To date, over 180 PICUs have responded detailing 530 PICU admissions requiring over 3,467 days of PICU care with 30 deaths. The preponderance of cases was in the eastern regions. Twenty-four percent of the patients admitted to the PICUs were over 18 years old. Fourteen percent of admissions were under 2 years old. Nearly 60% of children had comorbidities at admission with the average length of stay increasing by age and by severity of comorbidity. Advanced respiratory support was necessary during 67% of the current days of care, with 69% being conventional mechanical ventilation.
Conclusions:
PICUs have been significantly impacted by the pandemic. They have provided care not only for children but also adults. Patients with coronavirus disease 2019 have a high frequency of comorbidities, require longer stays, more ventilatory support than usual PICU admissions. These data suggest several avenues for further exploration.
The coronavirus disease 2019 (COVID-19) pandemic has had a significant impact on resource utilization in ICUs globally and across the United States and Canada. As many adult ICUs have reached capacity, the effect on PICUs has been less clear (1–3). PICUs have prepared for a surge in children, and, in many regions, have also prepared for and been used to provide care for adults.
Shekerdemian et al (4) evaluated the characteristics and outcomes of children with COVID-19 across 46 major children’s hospitals in North America. This report further expands this report by evaluating the geographic differences and resource use in PICUs across a broad range of large and small hospitals. It is not intended to be a comprehensive report of the natural history of COVID-19 in children. Even so, the effect on PICUs is important because there may still be a surge in pediatric cases and their management and resource preparation may be informed by these data. In addition, PICUs have been affected by the pressing needs of critically ill adults with practitioners and units serving adult patients.
This early hypothesis-generating report aims to: 1) summarize the reported national experience with COVID-19 in PICUs in the United States and also in Canada; 2) highlight the geographic variations in patterns of resource use in the PICUs with the greatest number of effected admissions; and 3) identify hypotheses that need urgent research to better understand the pediatric implications of COVID-19.
MATERIALS AND METHODS
In March 2020, to understand how the COVID-19 pandemic was affecting PICUs across North America, Virtual Pediatric Systems, LLC (VPS, Los Angeles, CA; http://www.myvps.org) expanded data collection related to COVID-19 for all Canadian and U.S. PICUs (regardless of VPS membership) to augment the existing VPS dataset and provide data for a near real-time dashboard. Concurrently, VPS launched a COVID-19 dedicated Listserv (now with over 1,300 participants) to enhance communication among pediatric intensivists concerning the pandemic and discuss patient management issues.
VPS is a national PICU data collaborative including data from more than 200 PICUs with over 1.5 million patient admissions over 20 years. The data collection was designed to be parsimonious to avoid imposing a data collecting burden on those PICUs managing COVID-19 patients and to assure rapid daily availability of results. Comorbidities were broadly defined as none, mild (single, minor comorbidity such as asthma, controlled diabetes), and moderate to severe (potentially life-threatening such as technology dependence, moderate to severe diabetes, immunosuppression, and cancer) as interpreted by individual PICUs. Data collection was focused on estimating the burden of the pandemic on PICUs and therefore reported as days of specific care provided by PICUs. Additionally, because many PICUs were required to admit adults beyond their usual age limits, all PICU admissions were counted regardless of age. Results were all individually reviewed several times a day; missing information was corrected, patient and data duplicates removed, obvious errors checked and corrected, and results verified. Data were also collected from reporting units providing more information about discharged COVID-19 positive patients. Existing data were analyzed to identify geographic variations in clinical presentations and outcomes for patients with COVID-19 in PICUs, and determined to be quality improvement, non-human Subjects research, by the institutional review board at Nicklaus Children’s Hospital.
RESULTS
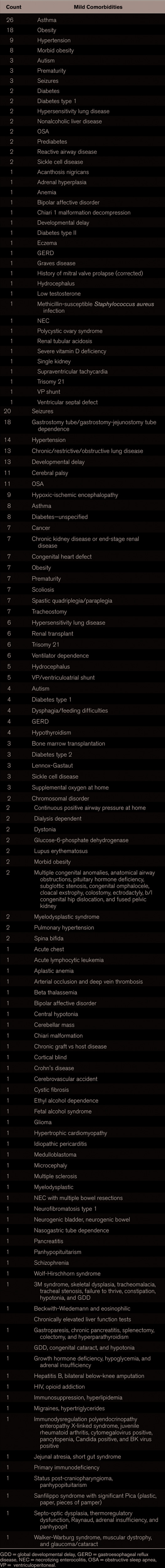
Data collection was started on March 14, 2020. To date (May 26, 2020, 10 wk), the following data were reported to VPS: 530 COVID-19 positive patients have been admitted to 183 reporting Canadian and U.S. ICUs with 30 deaths (5.7% case mortality rate) requiring over 3,467 days of ICU care (average length of stay [LOS] 6.5 d). These patients were identified among 9,186 tested patients. Although the VPS is an established national network of PICUs, these results reflect responses from 99 VPS members and 84 nonmembers self-reporting PICUs, with an estimated total of 3,228 PICU bed-capacity reported, representing the majority of PICU beds in the United States. The reporting hospitals were quite diverse including 74 freestanding children’s hospitals, 107 children’s hospitals within adult hospitals, and two specialty children’s hospitals. COVID-19 patient characteristics are shown in Table 1.
Table 1.
Admission Characteristics of 530 Coronavirus Disease 2019 Admissions to Date
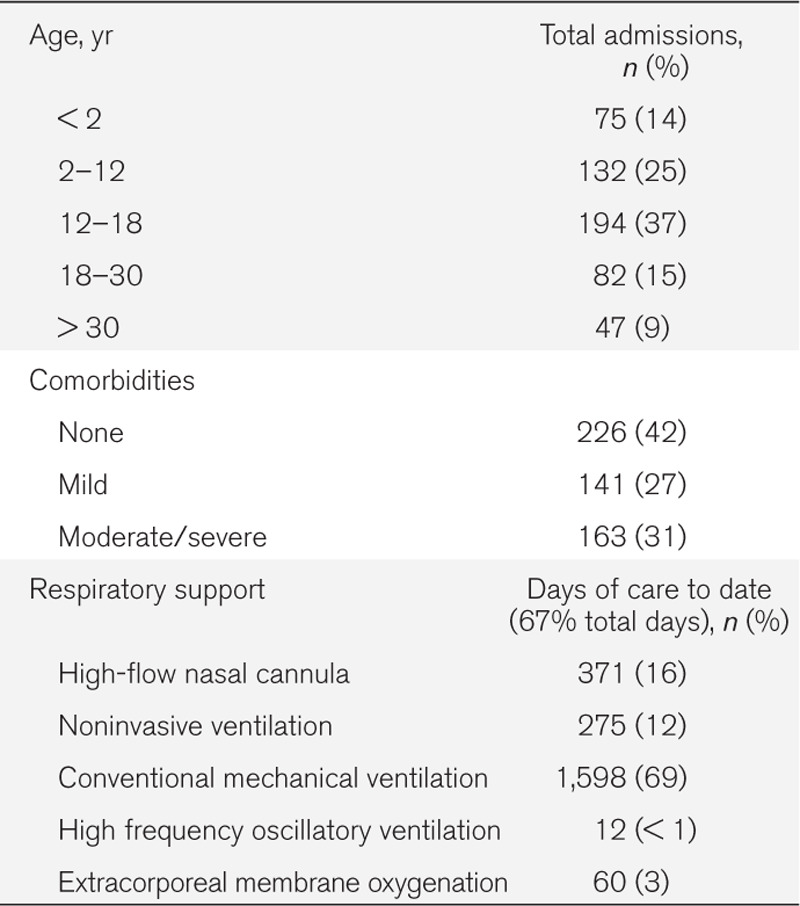
A significant number of admitted patients were greater than 18 years old (24%), although this has shown a decrease over time (40% at peak). The majority (65%) of adults (> 18 yr) were admitted to children’s hospitals part of adult hospitals, mostly in New York and New Jersey. Comorbidities were common in admitted patients (57% of admissions), with over half of these patients having moderate to severe comorbidities (a detailed list of the comorbidities in the discharged patients is shown in the Appendix). The most common mild comorbidities were obesity, asthma, and hypertension. The most common moderate to severe comorbidities were seizure disorder, cerebral palsy, gastric or jejunal permanent feeding tube, hypertension, chronic lung disease, and developmental delay. Figure 1 shows the case distribution in North America with a clear preponderance of cases in the east. Figure 2 shows the average daily census in the reporting ICUs showing a likely plateau in case numbers. Although the most recent day’s apparent drop in cases is due to reporting lag, it does appear that the new cases have certainly plateaued and apparently peaked in early May. As noted in Supplemental Table 1 (Supplemental Digital Content 1, http://links.lww.com/PCC/B427), despite the differences in the number of cases admitted to PICUs, there was no apparent trend between the timing of state interventions and the geographic differences in PICU admissions.
Figure 1.

Canada and the United States reported pediatric coronavirus disease 2019 (COVID-19) case distribution by state/province.
Figure 2.
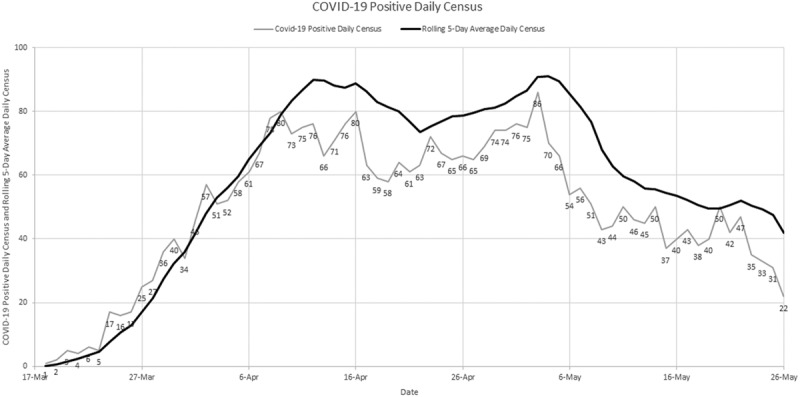
Canadian and the United States reporting ICUs daily coronavirus disease 2019 (COVID-19) patient census. A steady increase in patients being admitted to PICUs over time which seems to have plateaued.
Approximately 70% of the patients’ care days to date required treatment with more than supplemental oxygen. These therapies were high-flow nasal cannula (HFNC) (11% of all patient care days), noninvasive ventilation (NIV) (8%), conventional mechanical ventilation (46%), extracorporeal membrane oxygenation (ECMO) (2%), and high frequency oscillatory ventilation (HFOV) (< 1%). Conventional ventilation was modestly more frequent than in routine PICU admissions in whom 43% of patient care days require conventional mechanical ventilation, less than 1% oscillation, and 2% ECMO (VPS data).
Table 2 shows the results of discharged patients by age group received by VPS to date (May 26, 2020). The characteristics of the 284 reported discharged patients, 21 of whom died, include LOS, case fatality rate, need for ventilation, and frequency of comorbidities, all of which tended to increase with increasing age. Less than one-third of the reported mortalities were less than 18 years old. Multiple organ systems were involved during the patients ICU stays, often with several in a given patient, respiratory in 204 (72% of all discharges) patients, 120 (42%) had circulatory involvement, 93 (33%) gastro-intestinal disease, 83 (29%) had hematologic abnormalities, 58 (20%) with significant renal disease, 45 (16%) with nervous system involvement, and 41 (14%) endocrine involvement. Interestingly, there have been 47 cases reported (9% of all reports) with pediatric inflammatory multisystem syndrome temporally associated with severe acute respiratory syndrome coronavirus 2 (PIM-TS). Other systems involved included immunologic deficits, skin, and muscular. Smoking and vaping were only reported in 11 cases. There was no relationship between blood type and COVID-19 reporting.
Table 2.
Characteristics of 284 Discharged Coronavirus Disease 2019 Patients
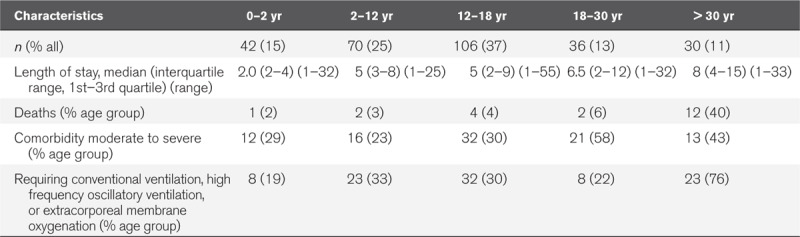
Further analyses to identify specific trends in children (< 18 yr) in the 284 reported discharged patients showed that there were 218 children (77%) with the following reported characteristics: 31% African American, 32% Hispanic/Latino 18% white, and 5% Asian. Most of the children remained in room air or low flow nasal cannula support (44%). Conventional ventilation was used in 25% of children, 8% received HFNC and 6% NIV. HFOV was used in only 1% of children and ECMO in 3% of children.
DISCUSSION
Although there are emerging studies of the experience of COVID-19 in pediatrics (1, 2), estimates of the potential impact of COVID-19 in children in ICUs were based on the early experience in China (5). A recent study by Shekerdemian et al (4) evaluated patient characteristics and outcomes of patients in large PICUs in North America. This is an important study evaluating the clinical course of children in PICUs. Nevertheless, a large proportion of the care for children is provided in smaller PICUs in addition to the larger PICUs in traditional freestanding children’s hospitals, and many of these PICUs in adult-based health systems may be flexed up to care for adult critically ill patients in an overflow situation. This study captured the recent experience of all types of PICUs in the United States and Canada, not only in large academic freestanding children’s hospitals. This is particularly relevant from a resource use and planning perspective for meeting the surge capacity for adult ICUs.
Recently (late April), the peak of adult COVID-19 patients admitted to PICUs reached approximately 40% over 18 years old with approximately 12% over 30 years. Currently, 24% are over 18 years old. This is in contrast to approximately 4% of patients older than 18 years and 0.2% over 30 years typically admitted to PICUs over the past 10 years (VPS data). It would appear that several PICUs have increased the age limits of patients cared for and admitted adult age patients.
Sixty-five percent of patients older than 18 years were admitted to PICUs in hospitals part of caring for both children and adults, mostly in the New Jersey and New York. Although some of these adults may represent former PICU patients or adults with pediatric disease often cared for in PICUs, the significantly greater number in this population indicates that it is most likely due to overflow from adult ICUs. Thus, PICUs appear to be providing important reserve support for adult ICUs, particularly in PICUs that are part of adult healthcare systems. Clearly, this has implications for future training, staffing, and supply needs. Respiratory support is shown as days of care delivered to date as opposed to patients receiving a particular therapy to more clearly reflect the impact on PICU resources rather than individual patients.
The findings noted in Supplemental Table 1 (Supplemental Digital Content 1, http://links.lww.com/PCC/B427) do not show a trend between state interventions and PICU admissions. This may be because PICUs with the greatest number of COVID-19 admissions were used for adult patients once the adult ICUs were at capacity. Of interest, from the 14 of Canada’s 16 PICUs that have participated in the ongoing VPS COVID-19 data collection, only eight patients tested positive, all within Quebec and Alberta provinces, with three deaths being reported.
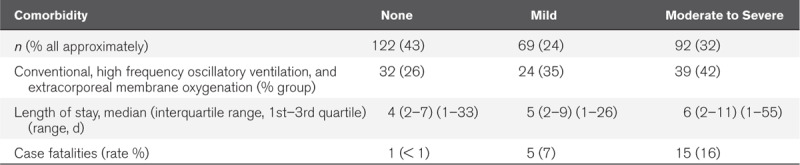
Sixty-seven percent of all reported COVID-19 patient care days to date (3,467) in this sample required conventional mechanical ventilation, NIV, HFNC, ECMO, or HFOV. Interestingly, over time there has been a shift away from conventional ventilation toward more HFNC and NIV. This is similar to their use in all PICU admissions during 2018–2019 (VPS data). This observation likely reflects appropriate utilization of PICU resources with the majority of care being provided for patients requiring advanced respiratory support. The distribution of age and comorbidities in discharged patients (284) (Tables 2 and 3) shows increasing ventilatory support, LOS, and mortality with both comorbidities and age. The LOS, increased support, and increased mortality in adults do not suggest either higher early mortality or a triage effect resulting from selecting adults less severely ill for admission to PICUs.
Table 3.
Length of Stay, Ventilation, and Case Fatality Rate by Comorbidity of 284 Discharged Patients
Our observations demonstrate a departure from the traditional experience in PICUs due to the COVID-19 pandemic. Most currently available data reports and predictive models do not differentiate between the experience of adult and PICUs. This difference is important from a clinical and resource utilization standpoint as well as policy development.
Limitations of this report include those inherent to early brief reports, convenience samples with potential reporting biases, and incomplete data on all cases as well as insufficient information about the denominator, with limitations to perform formal statistical analyses. The volunteer nature of the reporting clearly does not capture the full impact of COVID-19 in PICUs in the United States and Canada including the limitations of not capturing the presence of defined protocols for admitting adult patients to PICUs, physicians, and nurse staffing which could impact outcomes. A recent report from the Society of Critical Care Medicine highlights the importance and current availability of beds in the United States and a tiered staffing strategy during pandemic situations such as COVID-19 (6). This report indicates that there are 5,137 PICU beds, 22,901 neonatal ICU beds with a total of 96,596 ICU beds (2018 American Hospital Association data) (6).
Despite these limitations, this brief early report evaluates the experience and resource use implications of those reporting PICUs representing both large and small units in the COVID-19 pandemic, including the observation of PICUs being used for adult patients particularly in PICUs that are part of adult systems in contrast to PICUs in freestanding children’s hospitals. This early information may guide the PICU response to further care for critically ill children with COVID-19 and identify areas for future research given the unclear epidemiology surrounding COVID-19 (3).
Based on these data, the following hypothesis and questions emerge to guide better understanding of the epidemiologic differences of COVID-19 in adults and children. These need urgent research to allow developing policies for utilization of PICUs during the pandemic:
-
Contrary to the typical PICU demographics, children less than 2 years comprised of only 14.2% of the population. Important implications:
Why are younger children spared?
What are the determinants for younger children not needing PICU care?
Are, in fact, younger patients less severely affected than older patients?
What are the differences in severity of illness and implications for risk-adjusted outcomes using the Pediatric Risk of Mortality scoring system (7)?
Important comorbidities include obesity, asthma, and hypertension along with developmental delay. These at-risk populations require further consideration and the relationship between predisposition to COVID-19 and these comorbidities requires further elucidation.
-
Sixty-seven percent of patients required advanced respiratory support. Preparing for this surge number of ventilator cases and their safe management is crucial.
Is the high incidence of mechanical ventilation due to the higher severity of illness in COVID-19 patients?
Or is the high incidence of mechanical ventilation a function of differences in practice with early intubation in these patients?
Important questions concerning how care was provided in these unexpected circumstances, emergency staffing patterns, physician and other caregiver staffing models, resource sharing within hospitals, regions and communities, cohorting practices, the use of trainees such as residents and fellows, and resource rationing were not addressed in this report. Understanding how to optimize staffing and what protocols were most beneficial would be of considerable importance to guiding individual PICU planning.
The incidence of cardiogenic shock and multiple organ system failure with patients presenting with PIM-TS, Kawasaki like illness of which over 40 have been reported to VPS.
Incidence of short- and long-term neurologic complications during and after infection with COVID-19.
Differences in mechanical ventilation patterns between COVID-19 patients and other patients with specific viral illnesses (e.g., respiratory syncytial virus) after severity of illness adjustment.
-
Patients presenting with COVID-19 have a significant proportion of comorbidity, 27% mild morbidity and 31% moderate/severe morbidity. Interestingly, this is less than usual for PICU patients with 53% having some complex chronic conditions. Increasing comorbidities, severity is associated with greater mortality and prolonged LOS (8).
What are the factors underlying this and the long-term outcomes of these patients?
Can their risk be minimized?
What is it about asthma, hypertension, and obesity that cause patients with these conditions to appear at risk?
ACKNOWLEDGMENTS
We thank Dr. Theresa Mikhailov, Dr. Sheila Hanson, Dr. Curtis Kennedy, Dr. Steven Shein, Jamie Palumbo, and Gerardo Soto-Campos, PhD, for assistance with design and analysis.
Supplementary Material
APPENDIX: COMORBIDITIES REPORTED ON ICU ADMISSION
Many patients had more than one comorbidity.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/pccmjournal).
Dr. Sachdeva institution received funding from American Academy of Pediatrics—Health Resources & Service Administration Maternal Child Health Bureau grant: “Awareness and Access to Care for Children and Youth (CYE) with Epilepsy” (Medical Director, American Academy of Pediatrics CYE Project ECHO [Extension for Community Healthcare Outcomes]); New York State Department of Health, Office of Quality and Patient Safety—Health Research Incorporated—grant “Health innovation plan/state innovation model” (co-principal investigator) (2018) Agency for Healthcare Research and Quality grant “Pediatric Measurement Center for Excellence.” Children's Health Insurance Program Reauthorization Act Pediatric Quality Measurement Program (Principal Investigator) (2011–2017). Dr. Sachdeva is uncompensated for his role as Chief Scientific Officer for Virtual Pediatric Systems (VPS), LLC; however, his travel expenses for VPS related meetings were paid by VPS, LLC. Drs. Rice, Reisner, Brundage, Hulbert, Kaminski, and Wetzel received funding from VPS, LLC (employee).
REFERENCES
- 1.Cruz AT, Zeichner SL. Covid-19 in children: Initial characterization of the pediatric disease. Pediatrics 2020; 145:e20200834. [DOI] [PubMed] [Google Scholar]
- 2.Liu W, Zhang Q, Chen J, et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med 2020; 382:1370–1371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fauci AS, Lane HC, Redfield RR. Covid-19 – Navigating the uncharted. N Engl J Med 2020; 382:1268–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shekerdemian LS, Mahmood NR, Wolfe KK, et al. International COVID-19 PICU Collaborative: Characteristics and outcomes of children with coronavirus disease 2019 (COVD-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr 2020. May 11. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pathak EB, Salemi JL, Sobers N, et al. COVID-19 in children in the United States. Intensive care admissions, estimated total infected, and projected numbers of severe pediatric cases in 2020. J Public Health Manag Prac 2020; 26:325–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halpern NA, Tan KS.United States Resource Availability for COVID-19. Society of Critical Care Medicine: version 3 (5/12/2020). 2020. Available at: https://www.sccm.org/getattachment/Blog/March-2020/United-States-Resource-Availability-for-COVID-19/United-States-Resource-Availability-for-COVID-19.pdf. Accessed May 25, 2020.
- 7.Pollack MM, Patel KM, Ruttimann UE. PRISM III: An updated Pediatric Risk of Mortality score. Crit Care Med 1996; 24:743–752 [DOI] [PubMed] [Google Scholar]
- 8.Edwards JD, Houtrow AJ, Vasilevskis EE, et al. Chronic conditions among children admitted to U.S. pediatric intensive care units: Their prevalence and impact on risk for mortality and prolonged length of stay*. Crit Care Med 2012; 40:2196–2203 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.