Abstract
Differences by nativity status for cardiovascular disease (CVD) risk factors have been previously reported. Recent research has focused on understanding how other acculturation factors, such as length of residence, affect health behaviors and outcomes. This study examines the association between CVD risk factors and nativity/length of US residence. Using cross-sectional data from 15,965 adults in the 2011–2016 National Health and Nutrition Examination Surveys (analyzed in 2018), prevalence ratios and predicted marginals from logistic regression models are used to estimate associations of CVD risk factors (i.e., hypertension, hypercholesterolemia, diabetes, overweight/obesity and smoking) with nativity/length of residence (< 15 years, ≥15 years) in the US. In sex-, age-, education- and race and Hispanic origin- adjusted analyses, a higher percentage of US (50 states and District of Columbia) born adults (86.4%) had ≥1 CVD risk factor compared to non-US born residents in the US < 15 years (80.1%) but not ≥15 years (85.1%). Compared to US born counterparts, regardless of length of residence, hypertension overall and smoking among non-Hispanic white and Hispanic adults were lower among non-US born residents. Overweight/obesity overall and diabetes among Hispanic adults were lower among non-US born residents in the US < 15 years. In contrast, non-US born non-Hispanic Asian residents in the US < 15 years had higher prevalence of diabetes. Non-US born adults were less likely to have most CVD risk factors compared to US born adults regardless of length of residence, although, for smoking and diabetes this pattern differed by race and Hispanic origin.
Keywords: Nativity/length of residence, Cardiovascular disease risk factors, Hypertension, High cholesterol, Diabetes, Overweight/obesity, Cigarette smoking, NHANES
1. Introduction
Heart disease remains the leading cause of death in the United States (Kochanek et al., 2017). Many cardiovascular disease (CVD) risk factors, such as high blood pressure, high cholesterol, diabetes, overweight and obesity, and cigarette smoking are either preventable or modifiable (World Heart Federation, n.d.). Approximately 32% of US adults have hypertension (Fryar et al., 2017), 29% have hypercholesterolemia (National Center for Health Statistics, 2018), 14% have diabetes (Mendola et al., 2018), 72% are overweight or have obesity (National Center for Health Statistics, 2018), and 14% smoke cigarettes (Clarke and Schiller, 2019). The American Heart Association has projected that CVD prevalence and the resulting healthcare costs will increase substantially by 2030 (Heidenreich et al., 2011).
One of the Healthy People 2020 objectives is to achieve health equity, eliminate disparities, and improve the health of all groups (U. S. Department of Health and Human Services, 2010). By 2030, the US foreign-born population is projected to increase to 16%, up from 13% in 2014, representing a significant and increasing segment of the US population (Colby and Ortman, 2014). In addition to sex and race-ethnic origin (Ford, 2013; Fryar et al., 2010; Pool et al., 2017; Kurian and Cardarelli, 2007; Mosca et al., 2011), differences in CVD burden also have been reported by nativity status (Huh et al., 2008; Lariscy et al., 2013; Akbulut-Yuksel and Kugler, 2016; Ford et al., 2016). Several of these studies comparing US and non-US born adults, primarily in Hispanic or Asian populations, have found that birth in the US conveys greater risk of chronic conditions. Although studies of CVD risk factors and nativity status have been published, more recent research has focused on understanding how other acculturation factors, such as length of residence, affect health behaviors and outcomes (Rodriguez et al., 2012; Yi et al., 2014; Kershaw et al., 2016; Bharmal et al., 2015; Albrecht et al., 2013).
In this study, nationally representative data are used to examine the association between CVD risk factors and nativity status (US born in 50 states or District of Columbia vs non-US born) disaggregating non-US born residents by length of residence in the US, a commonly used proxy of acculturation. It examines whether these associations differ by race and Hispanic origin groups. The predicted prevalence of CVD risk factors (hypertension, hypercholesterolemia, diabetes, overweight or obesity, and cigarette smoking) by nativity/length of US residence is presented.
2. Methods
We analyzed data from the National Health and Nutrition Examination Survey (NHANES), a complex, multistage, probability survey conducted by the National Center for Health Statistics (NCHS). NHANES consists of nationally representative samples of the US civilian, non-institutionalized population. Participants in NHANES complete interviews in the home, and physical assessments, including collection of blood samples and measurement of blood pressure, weight, and height in a mobile examination center (MEC). NHANES was approved by the NCHS Research Ethics Review Board and written informed consent was obtained from adult participants. Interview and examination procedures have been previously described (Centers for Disease Control and Prevention. National Center for Health Statistics, 2019).
NHANES has been in the field continuously since 1999 and data are released in two-year cycles. Data from three 2-year cycles (2011–2012, 2013–2014 and 2015–2016) (Centers for Disease Control and Prevention. National Center for Health Statistics, 2019) were combined for this analysis in order to produce statistically reliable estimates for subgroups. In 2011–2016, oversampling was done for the non-Hispanic black, non-Hispanic Asian, and Hispanic population, as well as for other groups. The final cumulative examination response rate for adults aged ≥20 years was 64.5% in 2011–2012, 63.7% in 2013–2014, and 54.8% in 2015–2016.
This study was limited to adults aged ≥20 years (n = 15,965) who participated in both the home interview and MEC examination. We excluded pregnant women (n = 192), and persons with missing information on their place of birth (n = 10) or length of US residence (n = 205). An additional 9 persons with missing education were excluded.
2.1. Outcome variables
The outcome variables include five traditional CVD risk factors: hypertension, hypercholesterolemia, diabetes, overweight or obesity, and cigarette smoking.
Hypertension was defined using the 2017 ACC/AHA guidelines (Cifu and Davis, 2017) as having at least one of the following conditions: systolic blood pressure (BP) of 130 mmHg or greater, or a diastolic BP of 80 mmHg or greater, or self-reported current use of a hypertension medication based on an affirmative response to a question asking whether the participant was currently taking blood pressure medication because of a doctor’s diagnosis. A maximum of three BP readings collected on the same day were obtained by examiners: the mean of these recorded values was used to represent the participants’ systolic and diastolic BP.
Hypercholesterolemia (high cholesterol) was defined as serum total cholesterol ≥240 mg/dL or self-reported current use of cholesterol-lowering medication.
Diabetes was defined as having a measured blood glycohemoglobin (A1c) ≥6.5 mg/dL or a positive response to the question “Have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?” Women with gestational diabetes were excluded.
Overweight or Obesity was determined using body mass index (BMI) cutoffs. BMI is calculated as measured weight in kilograms divided by measured height in meters squared (kg/m2) rounded to the nearest tenth. Overweight or obesity was defined as a BMI ≥25.
Cigarette Smoking was defined as a positive response to the question “Have you smoked at least 100 cigarettes in your entire life? and also reported smoking every day or some days to the question “Do you now smoke cigarettes?”.
2.2. Independent variables
The key independent variable was nativity, which for non-US born was categorized by length of US residence. Nativity/length of US residence was defined based on self-report. US born was defined as being born in one of the 50 US states or the District of Columbia and all others, including those born in the US territories, were defined as non-US born. Those born in US territories (< 1% unweighted) are included in the “others” country of birth category (DMDBORN4) on the NHANES public release data files. Non-US born was categorized by length of residence in the US (i.e., the number of years non-US born participants have lived in the United States). NHANES computed years of residence for those who were born outside the U.S. based on their self-reported month and year when they came to the U.S. to live. Due to sample size constraints, length of residence was categorized as < 15 years and ≥15 years. Previous studies have used similar categories for length of residence with at least the ≥15 year cut point to study CVD risk factors (Bharmal et al., 2015; Koya and Egede, 2007; Krueger et al., 2014). Therefore, nativity/length of US residence was categorized as US born, non-US born < 15 years, and non-US born ≥15 years.
A sensitivity analysis in which a second acculturation variable, self-reported usual language spoken at home (other language vs English), added to the fully adjusted models was also conducted.
2.3. Covariates
Demographic characteristics were assessed as covariates. Age, sex, and race and Hispanic origin were included because previous studies have shown variation in CVD risk factors by these demographics (Ford, 2013; Kurian and Cardarelli, 2007; Mosca et al., 2011). Age in years was categorized into 3 groups: 20–39, 40–59, and 60 and over. Race and Hispanic origin was self-reported during the home interview and classified as non-Hispanic white, non-Hispanic black, non-Hispanic Asian, and Hispanic. Participants who reported other race (including multiple races) were included in total estimates but were not reported separately. Education, a measure of socioeconomic status, was also included as a covariate. Education was categorized into 3 groups: High school diploma or less, some college, and college graduate. Because of small sample sizes for some subgroup analyses and statistical power concerns, no additional covariates were added.
2.4. Statistical analyses
First, demographic characteristics of US and non-US born residents in the US ≥15 years or < 15 years were compared using chi-square tests for categorical variables and t-tests for continuous variables. Next, weighted logistic regression models were created for each CVD risk factor separately or for having one or more CVD risk factors. Because previous research has shown that the association between nativity status and health outcomes differs by race and Hispanic origin (Pool et al., 2017; Kurian and Cardarelli, 2007), an interaction term between nativity/length of residence and race and Hispanic origin was modeled for each outcome with age, sex, and race and Hispanic origin in the model. The interaction term was significant in the models for diabetes (p = 0.045) and smoking (p = 0.036). Consequently, the models and figures for these two outcomes are presented stratified by race and Hispanic origin. Age-, sex-, education- and race and Hispanic origin-adjusted prevalence estimates for hypertension, hypercholesterolemia, overweight/obesity and ≥1 CVD risk factor were obtained from predicted marginals. Age-, sex-, and education adjusted predicted prevalence estimates were obtained for race and Hispanic origin specific diabetes and smoking risk factors. Finally, adjusted prevalence ratios (Bieler et al., 2010) from the logistic regression models are presented to assess the relationship between nativity/length of US residence and each CVD risk factor.
Taylor series linearization was used to estimate standard errors (SE). Effective sample size, absolute and relative CI widths, and degrees of freedom were evaluated to determine the reliability of estimates (Parker et al., 2017). NHANES examination sample weights, which take into account unequal probabilities of selection resulting from the sample design, nonresponse (from screener to interview and from interview to examination), and noncoverage were used to obtain estimates (Chen et al., 2018). All statistical testing was performed using an α-level of 0.05, denoting significance. Analyses were conducted using SAS (version 9.4; SAS Institute) and SUDAAN (version 11.0; RTI International).
3. Results
This analysis includes data for 11,111 US born and 4854 non-US born adults from NHANES 2011–2016. Table 1 shows the sample sizes and weighted distribution of demographic characteristics among adults 20 years and over according to nativity/length of residence. There were differences in the distribution of age, race and Hispanic origin, and education. On average, non-US born adults in the US < 15 years were younger (37.9 years) than US born adults (48.4 years) and non-US born adults in the US ≥15 years (50.4 years). Non-US born adults in the US ≥15 or < 15 years were largely comprised of Hispanic (47.9%, SE 3.1; 48.4%, SE 3.7, respectively) and non-Hispanic Asian (25.3%, SE 2.6; 30.5%, SE 3.1) adults. Almost one-half of non-US born adults, regardless of length of residence, had a high diploma or less. US born adults were majority non-Hispanic white (76.8%, SE 1.9). There were no significant differences in the distribution of sex by nativity/length of residence.
Table 1.
Weighted distribution of demographic characteristics for adults aged 20 years and over by nativity/length of residence in the US, NHANES 2011–2016.
| All | US born | Non-US born ≥ 15years | Non-US born < 15 years | p-Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | SE | n | % | SE | n | % | SE | n | % | SE | ||
| Age (years) | |||||||||||||
| Mean age Age group | 15,965 | 47.9 | 0.4 | 11,111 | 48.4 | 0.4 | 3044 | 50.4 | 0.4 | 1810 | 37.9 | 0.4 | <0.001 |
| 20–39 | 5369 | 35.5 | 1.0 | 3832 | 34.4 | 1.1 | 547 | 25.5 | 1.2 | 990 | 62.4 | 1.6 | <0.001 |
| 40–59 | 5376 | 37.2 | 0.7 | 3504 | 36.7 | 0.8 | 1316 | 46.7 | 1.2 | 556 | 29.5 | 1.6 | |
| 60 + | 5220 | 27.3 | 0.7 | 3775 | 28.9 | 0.8 | 1181 | 27.7 | 1.2 | 264 | 8.1 | 0.9 | |
| Sex | |||||||||||||
| Male | 7796 | 48.6 | 0.4 | 5440 | 48.5 | 0.4 | 1476 | 48.3 | 0.9 | 880 | 49.9 | 1.4 | 0.51 |
| Female | 8169 | 51.4 | 0.4 | 5671 | 51.5 | 0.4 | 1568 | 51.7 | 0.9 | 930 | 50.1 | 1.4 | |
| Race-Hispanic origin | |||||||||||||
| Non-Hispanic white | 6070 | 66.0 | 2.1 | 5813 | 76.8 | 1.9 | 178 | 17.1 | 1.7 | 79 | 10.8 | 1.2 | <0.001 |
| Non-Hispanic black | 3644 | 11.4 | 1.2 | 3215 | 12.2 | 1.4 | 260 | 7.2 | 1.1 | 169 | 7.9 | 1.2 | |
| Non-Hispanic Asian | 1999 | 5.5 | 0.6 | 253 | 0.9 | 0.1 | 984 | 25.3 | 2.6 | 762 | 30.5 | 3.1 | |
| Hispanic | 3747 | 14.2 | 1.4 | 1424 | 7.0 | 0.9 | 1560 | 47.9 | 3.1 | 763 | 48.4 | 3.7 | |
| Education | |||||||||||||
| ≤ High school diploma | 7088 | 36.2 | 1.4 | 4564 | 33.4 | 1.4 | 1643 | 49.7 | 2.1 | 881 | 49.1 | 2.5 | <0.001 |
| Some college | 4844 | 32.5 | 0.8 | 3857 | 34.9 | 0.8 | 630 | 22.0 | 1.2 | 357 | 20.7 | 1.6 | |
| College graduate | 4033 | 31.3 | 1.5 | 2690 | 31.8 | 1.5 | 771 | 28.3 | 2.1 | 572 | 30.2 | 2.5 | |
NHANES: National Health and Nutrition Examination Survey; n = sample size; % = percent; SE = standard error.
All values except (n) were weighted using NHANES examination weights. Column percentages may not sum to 100% due to rounding or missing observations. Race-Hispanic origin groups will not sum to 100% because other race groups are not shown in table but included in calculation of totals. p-values for categorical variables were based on chi-square test and t-test for the continuous age variable.
The unadjusted and adjusted predicted prevalence of hypertension, hypercholesterolemia, diabetes, overweight/obesity, cigarette smoking, and having ≥1 CVD risk factor by nativity/length of residence are shown in Table 2. During 2011–2016, the unadjusted prevalence of hypertension (27.4% vs. 48.9%), hypercholesterolemia (16.4% vs. 30.9%), overweight/obesity (60.6% vs. 71.5%) and having one or more of 5 CVD risk factors (72.8% vs. 86.8%) was lower among non-US born adults living in the US < 15 years than US born adults. When adjusted for age, sex, education, and race and Hispanic origin, the prevalence of hypertension (38.3%, 43.1% vs. 48.5%, respectively) and overweight/ obesity (65.6%, 67.8% vs. 71.1%) was lower among non-US born adults, regardless of length of residence, compared with US born adults. There were no significant differences observed between non-US born and US born adults in the adjusted prevalence of hypercholesterolemia. Overall, the adjusted prevalence of having one or more of the five CVD risk factors was lower among non-US born living in the US < 15 years(80.1%) than those born in the US (86.4%). There was no significant difference in having ≥1 CVD risk factors between US and non-US born adults living in the US ≥15 years (85.1%).
Table 2.
Unadjusted and adjusted predicted prevalence of CVD risk factors by nativity/length of residence in the US, 2011–2016. Source: National Health and Nutrition Examination Survey.
| CVD risk factor/race-Hispanic origin | Sample size | Unadjusted | Adjusted | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| US born | Non-US born ≥ 15 years | Non-US born < 15 years | US born | Non-US born ≥ 15years | Non-US born < 15 years | ||||||||
| Percent (95% confidence interval) | Percent (95% confidence interval) | ||||||||||||
| Hypertension | 15,554 | 48.9 | 47.4–50.4 | 46.9 | 44.8–49.0 | 27.4 | 24.5–30.5 | 48.5 | 47.0–49.9 | 43.1 | 39.9–46.3 | 38.3 | 34.6–42.2 |
| Hypercholesterolemia | 15,204 | 30.9 | 29.6–32.1 | 30.0 | 28.1–32.1 | 16.4 | 14.5–18.5 | 30.0 | 28.8–31.2 | 29.4 | 26.8–32.2 | 27.8 | 24.8–31.1 |
| Overweight/obesity | 15,757 | 71.5 | 70.0–73.0 | 68.4 | 64.8–71.9 | 60.6 | 56.7–64.3 | 71.1 | 69.5–72.7 | 67.8 | 64.3–71.2 | 65.6 | 62.4–68.6 |
| Diabetes | |||||||||||||
| Non-Hispanic white | 5895 | 11.2 | 10.3–12.2 | 7.4 | 4.4–12.0 | 2.9 | 1.0–8.6 | 11.2 | 10.2–12.2 | 6.9 | 4.3–10.9 | 5.5 | 2.0–13.9 |
| Non-Hispanic black | 3415 | 18.5 | 17.1–20.1 | 19.5 | 13.1–27.9 | 12.6 | 7.9–19.5 | 18.5 | 17.0–20.0 | 16.9 | 11.5–24.1 | 16.6 | 11.0–24.3 |
| Non-Hispanic Asian | 1893 | 6.0 | 3.7–9.5 | 18.9 | 16.3–21.8 | 11.4 | 9.0–14.2 | 9.4 | 6.0–14.6 | 14.5 | 12.4–16.8 | 15.4 | 12.4–18.9 |
| Hispanic | 3630 | 14.2 | 11.7–17.2 | 19.6 | 17.4–22.0 | 8.1 | 6.1–10.6 | 16.7 | 14.2–19.5 | 14.5 | 12.7–16.5 | 11.1 | 8.6–14.2 |
| Smoking | |||||||||||||
| Non-Hispanic white | 6066 | 19.9 | 18.0–21.9 | 13.5 | 8.2–21.3 | 21.9 | 13.2–34.1 | 19.8 | 18.0–21.7 | 16.7 | 10.7–25.1 | 20.7 | 11.8–33.8 |
| Non-Hispanic black | 3636 | 26.8 | 24.9–28.7 | 9.8 | 6.3–15.1 | 6.3 | 3.4–11.3 | 26.5 | 24.7–28.4 | 11.2 | 7.2–17.1 | 6.6 | 3.5–12.1 |
| Non-Hispanic Asian | 1997 | 12.5 | 9.5–16.4 | 9.2 | 7.2–11.8 | 8.8 | 6.6–11.8 | 10.6 | 7.7–14.5 | 10.3 | 7.9–13.5 | 8.2 | 6.3–10.7 |
| Hispanic | 3744 | 20.3 | 18.1–22.7 | 12.4 | 10.3–14.9 | 13.1 | 10.7–16.0 | 21.5 | 19.2–24.0 | 12.0 | 9.8–14.6 | 12.5 | 10.1–15.3 |
| ≥ 1 CVD risk factor | 15,965 | 86.8 | 85.4–88.0 | 86.4 | 84.3–88.3 | 72.8 | 69.3–76.0 | 86.4 | 85.1–87.7 | 85.1 | 82.4–87.4 | 80.1 | 77.4–82.6 |
CVD indicates cardiovascular disease.
NOTE: Prevalence estimates are from predicted marginals from logistic regression. Hypertension, hypercholesterolemia, overweight/obesity and ≥ 1 CVD risk factor adjusted for age, sex, education, and race and Hispanic origin. Diabetes and smoking adjusted for age, sex and education. Covariate reference groups in models were age (20–39 years), sex (female), education (college graduate) and race and Hispanic origin (non-Hispanic white).
The nativity/length of residence and race and Hispanic origin interaction term was significant for diabetes and cigarette smoking, suggesting that these findings vary by race and Hispanic origin. Table 2 and the figure panels show the age-, sex-, and education- adjusted predicted prevalence of diabetes and smoking by nativity/length of residence, stratified by race and Hispanic origin. Among non-Hispanic white and Hispanic adults, the prevalence of diabetes decreased as acculturation decreased. In contrast, among non-Hispanic Asian adults, the prevalence of diabetes increased as acculturation decreased. Non-US born Asian adults had similar prevalence of diabetes regardless of length of residence (14.5%, 15.4%). Among non-US born non-Hispanic black and Hispanic adults the prevalence of cigarette smoking decreased as acculturation decreased. Among non-Hispanic white and Asian adults, no significant difference was observed between US born and non-US born in cigarette smoking (Fig. 1).
Fig. 1.
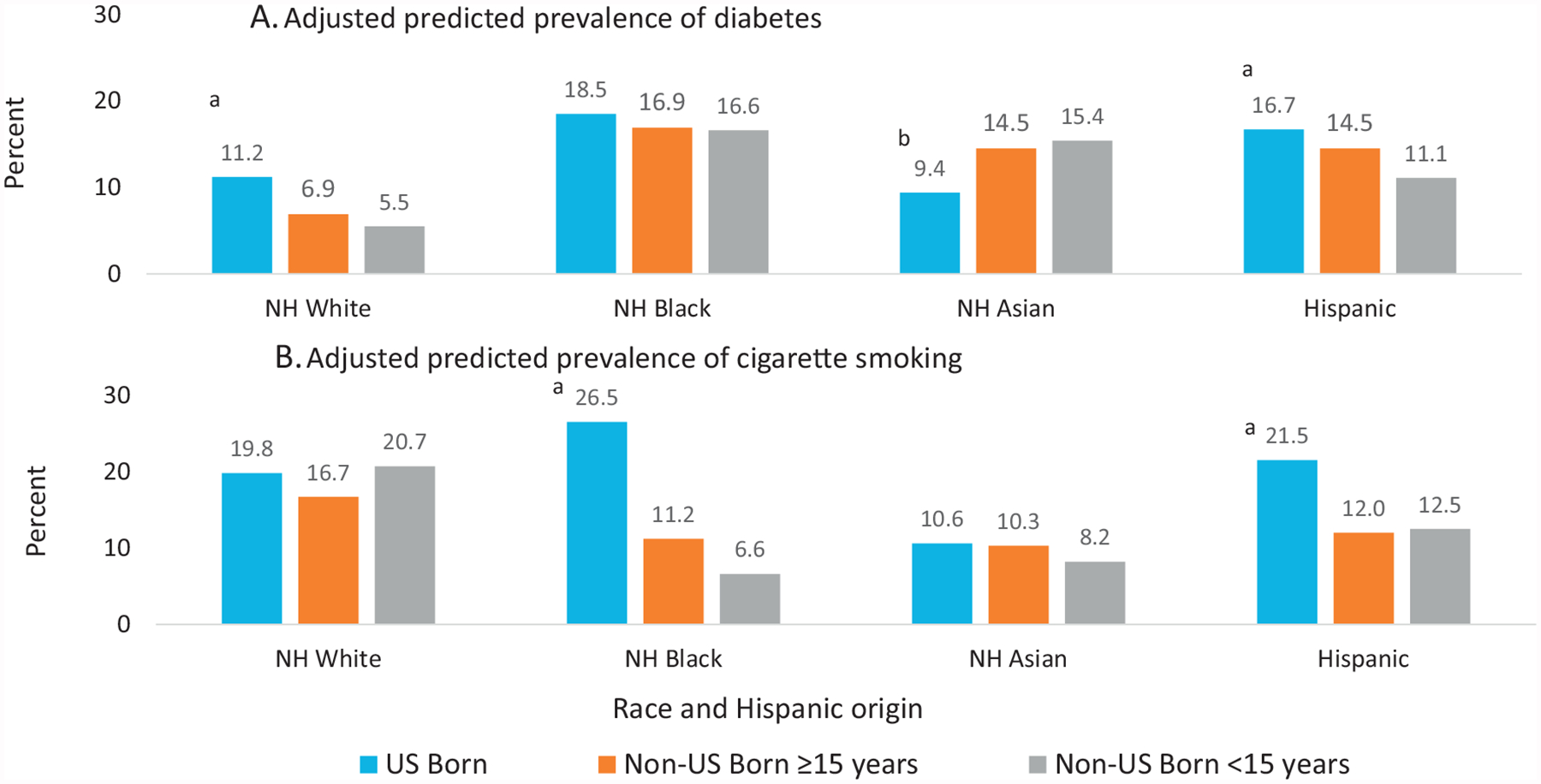
Adjusted predicted prevalence of diabetes (panel A) and cigarette smoking (panel B) among adults 20 years and over by nativity/length of US residence and race and Hispanic origin, United States, 2011–2016.
Diabetes is defined as a self-reported physician’s diagnosis of diabetes or having a measured blood glycohemoglobin (A1c) ≥6.5 mg/dL. Cigarette Smoking is defined as self-reported ever smoking at least 100 cigarettes and currently smoking every day or some days.
aSignificant decreasing trend from most acculturated (US born) to least acculturated (non-US born < 15 years). p < 0.05.
bSignificant increasing trend from most acculturated (US born) to least acculturated (non-US born < 15 years). p < 0.05.
Note: NH indicates non-Hispanic; prevalence estimates are from age, sex and education adjusted predicted marginals from logistic regression. Covariate reference groups in models were age (20–39 years), sex (female), and education (college graduate).
Source: National Health and Nutrition Examination Survey
Table 3 provides unadjusted and adjusted prevalence ratios for having each CVD risk factor by nativity/length of residence. Compared to US born adults, the unadjusted prevalence ratio of hypertension was lower for non-US born adults living in the US < 15 years (PR = 0.56, 95% CI 0.50–0.62). In models adjusted for sex, age, education, and race and Hispanic origin, non-US born adults had a lower prevalence ratio of hypertension regardless of length of residence in the US [≥15 years (PR = 0.89, 95% CI 0.83–0.96); < 15 years (PR = 0.79, 95% CI0.72–0.87)].
Table 3.
Unadjusted and adjusted prevalence ratios (95% confidence intervals) for CVD risk factors and nativity/length of residence in the US, 2011–2016. Source: National Health and Nutrition Examination Survey.
| Unadjusted model | Adjusted model | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| US born | Non-US born ≥ 15years | Non-US born < 15 years | US born | Non-US born ≥ 15years | Non-US born < 15 years | |||||
| Hypertension | 1.00 | 0.96 | 0.92–1.00 | 0.56 | 0.50–0.62 | 1.00 | 0.89 | 0.83–0.96 | 0.79 | 0.72–0.87 |
| Hypercholesterolemia | 1.00 | 0.97 | 0.91–1.04 | 0.53 | 0.47–0.60 | 1.00 | 0.98 | 0.90–1.07 | 0.93 | 0.83–1.04 |
| Overweight/obesity | 1.00 | 0.96 | 0.91–1.00 | 0.85 | 0.80–0.90 | 1.00 | 0.95 | 0.91–1.00 | 0.92 | 0.88–0.97 |
| Diabetes | ||||||||||
| Non-Hispanic white | 1.00 | 0.66 | 0.40–1.09 | 0.26 | 0.09–0.78 | 1.00 | 0.62 | 0.39–0.98 | 0.49 | 0.19–1.28 |
| Non-Hispanic black | 1.00 | 1.05 | 0.73–1.52 | 0.68 | 0.44–1.07 | 1.00 | 0.91 | 0.64–1.31 | 0.90 | 0.60–1.33 |
| Non-Hispanic Asian | 1.00 | 3.18 | 1.93–5.22 | 1.91 | 1.17–3.11 | 1.00 | 1.55 | 0.97–2.43 | 1.63 | 1.06–2.51 |
| Hispanic | 1.00 | 1.38 | 1.16–1.64 | 0.57 | 0.40–0.79 | 1.00 | 0.87 | 0.74–1.02 | 0.67 | 0.50–0.89 |
| Smoking | ||||||||||
| Non-Hispanic white | 1.00 | 0.68 | 0.41–1.11 | 1.10 | 0.68–1.78 | 1.00 | 0.84 | 0.55–1.30 | 1.05 | 0.62–1.76 |
| Non-Hispanic black | 1.00 | 0.37 | 0.23–0.58 | 0.23 | 0.13–0.42 | 1.00 | 0.42 | 0.27–0.66 | 0.25 | 0.14–0.46 |
| Non-Hispanic Asian | 1.00 | 0.74 | 0.50–1.09 | 0.70 | 0.45–1.10 | 1.00 | 0.97 | 0.63–1.50 | 0.77 | 0.52–1.16 |
| Hispanic | 1.00 | 0.61 | 0.49–0.76 | 0.65 | 0.52–0.80 | 1.00 | 0.56 | 0.44–0.70 | 0.58 | 0.46–0.74 |
| ≥ 1 CVD risk factor | 1.00 | 1.00 | 0.97–1.02 | 0.84 | 0.80–0.88 | 1.00 | 0.98 | 0.96–1.01 | 0.93 | 0.90–0.96 |
CVD indicates cardiovascular disease.
NOTE: Prevalence ratios are from logistic regression models. Hypertension, hypercholesterolemia, overweight/obesity and ≥1 CVD risk factor adjusted for age, sex, education, and race and Hispanic origin. Diabetes and smoking adjusted for age, sex and education. Covariate reference groups in models were age (20–39 years), sex (female), education (college graduate) and race and Hispanic origin (non-Hispanic white).
Compared to US born adults, the unadjusted prevalence ratio of hypercholesterolemia was lower for non-US born adults living in the US < 15 years (PR = 0.53, 95% CI 0.47–0.60). In models adjusted for sex, age, education, and race and Hispanic origin, no significant difference was observed between non-US born adults, regardless of US length of residence, and their US born counterparts.
The unadjusted prevalence ratio of being overweight or having obesity was lower among non-US born adults living in the US < 15 years (PR = 0.85, 95% CI 0.80–0.90) compared to those born in the US. In models adjusted for sex, age, education, and race and Hispanic origin, non-US born adults living in the US < 15 years had a lower prevalence ratio of being overweight or having obesity (PR = 0.92, 95% CI 0.88–0.97) compared to US born adults.
The unadjusted prevalence ratio of having one or more CVD risk factors was lower among non-US born adults living in the US < 15 years (PR = 0.84, 95% CI 0.80–0.88) compared to those born in the US. In models adjusted for sex, age, education, and race and Hispanic origin, only non-US born adults living in the US < 15 years had a lower prevalence ratio of having one or more CVD risk factors (PR = 0.93, 95% CI 0.90–0.96) compared to US born adults.
Compared to their US born counterparts, the unadjusted prevalence ratio of diabetes was lower for non-US born non-Hispanic white (PR = 0.26, 95% CI 0.09–0.78) and Hispanic (PR = 0.57, 95% CI0.40–0.79) adults living in the US < 15 years. In contrast, the unadjusted prevalence was higher for non-US born Asian adults, regardless of length of US residence [≥15 years (PR = 3.18, 95% CI1.93–5.22); < 15 years (PR = 1.91, 95% CI 1.17–3.11)]. The unadjusted prevalence also was higher in non-US born Hispanic adults living in the US ≥15 years (PR = 1.38, 95% CI 1.16–1.64). In models adjusted for sex, age, and education only non-US born non-Hispanic white adults (PR = 0.62, 95% CI 0.39–0.98) in the US ≥15 years and non-US born Hispanics adults (PR = 0.67, 95% CI 0.50–0.89) in the US < 15 years had a lower prevalence ratio of diabetes. Non-Hispanic Asian adults living in the US < 15 years had a higher prevalence ratio of diabetes (PR = 1.63, 95% CI 1.06–2.51).
Both the unadjusted and adjusted prevalence ratios for cigarette smoking were lower among non-US born non-Hispanic black and Hispanic adults regardless of length of time in the US, compared to their US born counterparts. No significant difference for cigarette smoking was observed between non-US born non-Hispanic white and Asian adults, regardless of length of residence in the US, and their US born counterparts.
In sensitivity analyses with usual language spoken in the home in the model (English vs. non-English), results did not change for hypercholesterolemia, hypertension, overweight/obesity and smoking. For diabetes among non-US born Hispanics residing in the US ≥15 years, results became significant (change in PR from 0.87, 95% CI0.74–1.02 to 0.80, 95% CI 0.66–0.96) (data not shown).
4. Discussion
In 2011–2016, non-US born adults were less likely to have individual CVD risk factors compared to their US born counterparts. The one exception, non-US born Asian adults in the US < 15 years were more likely to have diabetes than their US born counterparts. Length of residence in the US impacted the likelihood of having 1 or more CVD risk factors; non-US born adults in the US ≥15 years had the same risk as those born in the US while those in the US < 15 years were less likely to have 1 or more risk factors. Adjustment for age, sex, education, and race and Hispanic origin impacted the prevalence of hypercholesterolemia, where there was no longer a difference between non-US and US born adults. Adjustment for demographic characteristics also resulted in differences in hypertension between US and non-US born adults who lived in the US ≥15 years that were not observed before adjustment.
Demographic differences by age, sex, and race/ethnicity, and nativity status exist in CVD outcomes.(Pool et al., 2017; Kurian and Cardarelli, 2007; Mosca et al., 2011; Huh et al., 2008; Lariscy et al., 2013; Akbulut-Yuksel and Kugler, 2016; Ford et al., 2016) We show that non-US born adults in the US < 15 years tend to be younger than US born adults. The distribution of the US population by nativity/length of US residence also varied by race-Hispanic origin. There are more non-Hispanic white and black US born adults and more non-Hispanic Asian and Hispanic non-US born adults. Hispanic and Asian Americans are two of the fastest growing racial-ethnic groups in the US. While the increase in the Hispanic population has been primarily attributed to an increased birth rate in the US, the growth in the Asian American population has been primarily from immigration (Brown, 2014). Nevertheless, the interaction between nativity/length of US residence and race-Hispanic origin was only significant in models for diabetes and smoking, suggesting that the relationship between nativity/length of US residence and hypertension, hypercholesterolemia, and overweight/obesity does not vary by race-Hispanic origin.
Our results are generally consistent with other studies that have reported that non-US born persons are less likely to have most cardiovascular risk factors compared to their US counterparts (Wade et al., 2013; Echeverria et al., 2017; Baluja et al., 2003). However, previous studies of nativity/length of residence and some CVD risk factors have focused on one race/ethnic group (Rodriguez et al., 2012; Kershaw et al., 2016; Echeverria et al., 2017; O’Brien et al., 2014). For example, a previous study using NHANES 2011–2014 data examined diabetes, obesity, and smoking among US born and non-US born non-Hispanic Asian adults compared to non-Hispanic white adults. In that study, diabetes and obesity increased with longer length of residence in the US. However, that study only focused on three CVD risks among non-US born and US born Asians compared to US born whites only (Echeverria et al., 2017). Another study using NHANES 2007–2010 data examined nativity, language spoken at home, and duration of US residence and concluded that those measures were associated with higher risk of diabetes among US Latinos (O’Brien et al., 2014). Our study reports on more recent data, includes five CVD risk factors, and includes the entire US civilian, non-institutionalized adult population adjusting for or stratifying by race and Hispanic origin.
There are limitations of our study. First, the data are cross-sectional and inferences cannot be made about causal associations. Second, there were not enough data to examine individual countries or regions among those who were non-US born. Finally, sample sizes may not have been large enough to determine differences in subgroup comparisons when one indeed did exist.
In conclusion, non-US born adults were less likely to have most CVD risk factors compared to US born counterparts, regardless of length of US residence, although for smoking and diabetes this pattern differed by race and Hispanic origin.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Financial disclosure
None of the authors of this paper has any financial disclosures to report.
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The findings and conclusions in this report are those of the authors and not necessarily of the official position of the Centers for Disease Control and Prevention.
Declaration of competing interest
None of the authors of this paper has any conflicts of interest.
References
- Akbulut-Yuksel M, Kugler AD, 2016. Intergenerational persistence of health: do immigrants get healthier as they remain in the U.S. for more generations? Economics & Human Biology 23, 136–148. [DOI] [PubMed] [Google Scholar]
- Albrecht SS, Diez Roux AV, Aiello AE, Schulz AJ, Abraido-Lanza AF, 2013. Secular trends in the association between nativity/length of US residence with body mass index and waist circumference among Mexican-Americans, 1988–2008. Int J Public Health 58 (4), 573–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baluja KF, Park J, Myers D, 2003. Inclusion of immigrant status in smoking prevalence statistics. Am. J. Public Health 93 (4), 642–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharmal N, Kaplan RM, Shapiro MF, et al. , 2015. The association of duration of residence in the United States with cardiovascular disease risk factors among South Asian immigrants. J. Immigr. Minor. Health 17 (3), 781–790. [DOI] [PubMed] [Google Scholar]
- Bieler GS, Brown GG, Williams RL, Brogan DJ, 2010. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am. J. Epidemiol 171 (5), 618–623. [DOI] [PubMed] [Google Scholar]
- Brown A, 2014. U.S. Hispanic and Asian populations growing, but for different reasons Pew Research Center; http://www.pewresearch.org/fact-tank/2014/06/26/u-s-hispanic-and-asian-populations-growing-but-for-different-reasons/. [Google Scholar]
- Centers for Disease Control and Prevention. National Center for Health Statistics, 2019. Centers for Disease Control and Prevention. National Center for Health Statistics. National Health and Nutrition Examination Survey https://wwwn.cdc.gov/nchs/nhanes/default.aspx Accessed 2019. [Google Scholar]
- Chen TC, Parker JD, Clark J, Shin HC, Rammon JR, Burt VL, 2018. National Health and nutrition examination survey: estimation procedures, 2011–2014. Vital Health Stat. 2 (177), 1–26. [PubMed] [Google Scholar]
- Cifu AS, Davis AM, 2017. Prevention, detection, evaluation, and management of high blood pressure in adults. JAMA 318 (21), 2132–2134. 10.1001/jama.2017.18706. [DOI] [PubMed] [Google Scholar]
- Clarke TCNT, Schiller JS, 2019. Early Release of Selected Estimates Based on Data from the National Health Interview Survey. National Center for Health Statistics. [Google Scholar]
- Colby S, Ortman JM, 2014. Projections of the size and composition of the U.S. population: 2014 to 2060 In: Current Population Reports. U.S. Census Bureau, Washington, DC. [Google Scholar]
- Echeverria SE, Mustafa M, Pentakota SR, et al. , 2017. Social and clinically-relevant cardiovascular risk factors in Asian Americans adults: NHANES 2011–2014. Prev. Med 99 (Supplement C), 222–227. [DOI] [PubMed] [Google Scholar]
- Ford ES, 2013. Trends in predicted 10-year risk of coronary heart disease and cardiovascular disease among U.S. adults from 1999 to 2010. J. Am. Coll. Cardiol 61 (22), 2249–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ND, Narayan KM, Mehta NK, 2016. Diabetes among US- and foreign-born blacks in the USA. Ethn Health 21 (1), 71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD, 2010. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in U.S. adults, 1999–2006. NCHS Data Brief 36, 1–8. [PubMed] [Google Scholar]
- Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D, 2017. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS Data Brief 289, 1–8. [PubMed] [Google Scholar]
- Heidenreich PA, Trogdon JG, Khavjou OA, et al. , 2011. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 123 (8), 933–944. [DOI] [PubMed] [Google Scholar]
- Huh J, Prause J, Dooley CD, 2008. The impact of nativity on chronic diseases, self-rated health and comorbidity status of Asian and Hispanic immigrants. J. Immigr. Minor. Health 10 (2), 103–118. [DOI] [PubMed] [Google Scholar]
- Kershaw KN, Giacinto RE, Gonzalez F, et al. , 2016. Relationships of nativity and length of residence in the U.S. with favorable cardiovascular health among Hispanics/Latinos: The Hispanic Community Health Study/Study of Latinos (HCHS/ SOL). Prev. Med 89, 84–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek KD, Murphy S, Xu J, Arias E, 2017. Mortality in the United States, 2016. NCHS Data Brief. 293 pp. 1–8. [PubMed] [Google Scholar]
- Koya DL, Egede LE, 2007. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J. Gen. Intern. Med 22 (6), 841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger PM, Coleman-Minahan K, Rooks RN, 2014. Race/ethnicity, nativity and trends in BMI among U.S. adults. Obesity 22 (7), 1739–1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurian AK, Cardarelli KM, 2007. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis 17 (1), 143–152. [PubMed] [Google Scholar]
- Lariscy JT, Hummer RA, Rath JM, Villanti AC, Hayward MD, Vallone DM, 2013. Race/ethnicity, nativity, and tobacco use among US young adults: results from a nationally representative survey. Nicotine Tob. Res 15 (8), 1417–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendola ND, Chen T-C, Gu Q, Eberhardt MS, Saydah S, 2018. Prevalence of total, diagnosed, and undiagnosed diabetes among adults: United States, 2013–2016. NCHS Data Brief 319, 1–8. [PubMed] [Google Scholar]
- Mosca L, Barrett-Connor E, Wenger NK, 2011. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation 124 (19), 2145–2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics, 2018. Health, United States, 2017: With SpecialFeature on Mortality. Hyattsville, Maryland. [Google Scholar]
- O’Brien MJ, Alos VA, Davey A, Bueno A, Whitaker RC. Acculturation and the prevalence of diabetes in US Latino adults, national health and nutrition examination survey 2007–2010. Prev. Chronic Dis 2014;11:E176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker JDTM, Malec DJ, et al. , 2017. National Center for Health Statistics data presentation standards for proportions. Vital Health Stat 2 (175). [PubMed] [Google Scholar]
- Pool LR, Ning H, Lloyd-Jones DM, Allen NB, 2017. Trends in racial/ethnic disparities in cardiovascular health among US adults from 1999–2012. J. Am. Heart Assoc 6 (9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez F, Hicks LS, López L, 2012. Association of acculturation and country of origin with self-reported hypertension and diabetes in a heterogeneous Hispanic population. BMC Public Health 12 (1), 768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. S. Department of Health and Human Services, 2010. Healthy people 2020. https://www.cdc.gov/nchs/healthy_people/hp2020.htm.
- Wade B, Lariscy JT, Hummer RA, 2013. Racial/ethnic and nativity patterns of U.S. adolescent and young adult smoking. Popul. Res. Policy Rev 32 (3), 353–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Heart Federation Cardiovascular disease risk factors. Press release. http://www.world-heart-federation.org/press/fact-sheets/cardiovascular-disease-risk-factors/.
- Yi S, Elfassy T, Gupta L, Myers C, Kerker B, 2014. Nativity, language spoken at home, length of time in the United States, and race/ethnicity: associations with self-reported hypertension. Am. J. Hypertens 27 (2), 237–244. [DOI] [PMC free article] [PubMed] [Google Scholar]


