Abstract
Germline variants inactivating the mismatch repair (MMR) genes MLH1, MSH2, MSH6 and PMS2 cause Lynch syndrome that implies an increased cancer risk, where colon and endometrial cancer are the most frequent. Identification of these pathogenic variants is important to identify endometrial cancer patients with inherited increased risk of new cancers, in order to offer them lifesaving surveillance. However, several other genes are also part of the MMR pathway. It is therefore relevant to search for variants in additional genes that may be associated with cancer risk by including all known genes involved in the MMR pathway. Next-generation sequencing was used to screen 22 genes involved in the MMR pathway in constitutional DNA extracted from full blood from 199 unselected endometrial cancer patients. Bioinformatic pipelines were developed for identification and functional annotation of variants, using several different software tools and custom programs. This facilitated identification of 22 exonic, 4 UTR and 9 intronic variants that could be classified according to pathogenicity. This study has identified several germline variants in genes of the MMR pathway that potentially may be associated with an increased risk for cancer, in particular endometrial cancer, and therefore are relevant for further investigation. We have also developed bioinformatics strategies to analyse targeted sequencing data, including low quality data and genomic regions outside of the protein coding exons of the relevant genes.
Introduction
Cancer is a life-threatening disease, with 18.1 million new cancer cases and 9.6 million cancer deaths worldwide in 2018 [1]. There is an increasing number of cases every year, and it has become an enormous burden to society. With longer life span, increased population and changed lifestyle, we can expect to have even more cases of cancer in the future. Among many types of cancers, incidences of endometrial cancer (EC) have increased worldwide in recent years [2], and it is currently the most common gynecological disease in western world [3]. This is the sixth most commonly diagnosed cancer and the fourteenth leading cause of death for women worldwide, with 380,000 estimated new cases in 2018 [1]. In Europe around 88,000 women get affected with EC every year, making EC the fourth most common cancer in women and tenth most common cancer among cancer related deaths [4]. With these high rates, it is important to diagnose EC at early and treatable stages. Environmental factors, changed lifestyle, high BMI, hypertension, menstrual irregularities and hormonal imbalances can play important roles towards carcinogenesis [5].
Hereditary factors also contribute towards EC. Higher incidences of EC are common among close relatives of EC patients [6]. Micro-satellite instability (MSI), due to dysfunction of the DNA mismatch repair (MMR) pathway, has frequently been reported as an oncogenic mechanism in EC [7]. The MMR system corrects replication errors, in particular single nucleotide variants and insertion-deletion (INDEL) loops, and failure in this system can result in MSI. Around ~30% of EC patients have been found with hyper-mutable phenotype and MSI [7–9] induced by dysfunctional MMR. MMR dysfunction is the cause of Lynch syndrome (LS), an autosomal dominant inherited cancer susceptibility syndrome, also known as hereditary non-polyposis colon cancer (HNPCC). LS is characterized by early-onset epithelial cancers. Individuals affected with LS have high risk of colorectal cancer (CRC) and EC, in addition to an increased risk of other epithelial malignancies like bowel, stomach, ovary, bladder, or pancreas cancer to mention a few [10]. Life-time risk of LS-affected individuals for EC is 33–61% and for CRC 40–80% [11, 12]. Not all CRC and EC with MMR deficiency are due to germline mutation, rather, most of the cases are sporadic cancers occurring due to epigenetic silencing of the MMR gene MLH1 by DNA methylation [13–15]. It is important to identify EC cases with LS as they require regular surveillance, like colonoscopy. Given the high risk for developing new primary cancers, including CRC, this has been proven to reduce the overall mortality of the disease. If mutations in MMR genes are identified it will give the patient a diagnosis of LS and also enable at-risk relatives to be informed about their cancer risks. In addition, if pathogenic variants are identified in novel genes it could possibly explain why pathogenic variants are identified only in approximately 50% of families with a clinical diagnosis of LS (i.e. they fulfil the Amsterdam criteria) [16].
Since the rate of MSI tumours reported in EC cases is higher (30%) compared to other cancers (ie 15% in CRC), illustrating that an abnormal DNA MMR pathway plays a role in EC tumorigenesis, we decided to look into a more extended set of genes than those known to be involved in LS (MLH1, MSH2, MSH6, PMS2 and deletions in EPCAM1). In the present study, 22 genes (both coding and noncoding parts) involved in the MMR pathway were sequenced in DNA from 199 sporadic EC patients. Targeted next generation sequencing (NGS) was used, aiming to identify novel genetic variation like substitutions, insertions/deletions (indels) and structural alterations (e.g. copy number variations) that may lead to the multi-step process of carcinogenesis.
Materials and methods
The study was performed on DNA extracted from full blood from 199 patient samples from a study which included consecutively recruited women with histologically confirmed EC (sporadic cases) who presented for treatment at the Hunter Centre for Gynaecological Cancer, John Hunter Hospital, Newcastle, New South Wales, Australia between the years 1992 and 2005 [17]. Blood samples were taken in year 2005 for the present study. The study has been approved by Hunter New England (HNE) Human Research Ethics Committee (HNE HREC: 05/03/09/3.14). Written informed consent was obtained from all participants.
Targeted next generation sequencing (NGS)
Targeted NGS sequencing was performed on the 199 patient samples, using an Illumina MiSeq [18] instrument. Initially 12 runs were performed to sequence the samples; later 15 samples were re-sequenced due to low quality of the initial sequencing. The target regions (all introns, exons, 5’ and 3’ UTRs) of 22 MMR genes (MLH1, MSH2, MSH6, PMS2, MSH3, PMS1, MLH3, EXO1, RFC1, RFC2, RFC3, RFC4, RFC5, PCNA, LIG1, RPA1, RPA2, RPA3, POLD1, POLD2, POLD3 and POLD4) with a total size of 1.213 Mb were captured using 6961 probes and the Illumina Nextera Rapid Capture Enrichment Kit (custom, 96 samples). An overview of these 22 genes, their function and associated phenotypes are shown in Table 1. Sequencing was performed at the Medical Genetics Laboratory at Hunter Medical Research Institute (HMRI), University of Newcastle, Australia.
Table 1. List of genes in target panel.
| Gene | Gene function (Info source: NCBI-gene) | Phenotype (Info source: OMIM) | OMIM ID | |
|---|---|---|---|---|
| MLH | MLH1 | Encodes a protein which heterodimerizes with MMR endonuclease PMS2 to form MutL alpha. | Colorectal cancer, hereditary nonpolyposis, type 2; Muir-Torre syndrome; Mismatch repair cancer syndrome | 120436 |
| MLH3 | Member of the MutL-homolog (MLH) family, maintains genomic integrity during DNA replication and after meiotic recombination. | Colorectal cancer, hereditary nonpolyposis, type 7; Colorectal cancer, somatic; Susceptibility to Endometrial cancer | 604395 | |
| MSH | MSH2 | Forms 2 different heterodimers: MutS alpha (MSH2-MSH6 heterodimer) and MutS beta (MSH2-MSH3 heterodimer) which binds to DNA mismatches to initiate DNA repair | Colorectal cancer, hereditary nonpolyposis, type 1; Muir-Torre syndrome; Mismatch repair cancer syndrome | 609309 |
| MSH3 | Forms a hetero-dimer with MSH2 to form MutS beta which forms a complex with MutL alpha heterodimer and initiates mismatch repair by binding to a mismatch. | Endometrial carcinoma, somatic; Familial adenomatous polyposis 4 | 600887 | |
| MSH6 | A component of the post-replicative DNA MMR system. Heterodimerizes with MSH2 to form MutS alpha, which binds to DNA mismatches to initiate DNA repair. | Colorectal cancer, hereditary nonpolyposis, type 5; Endometrial cancer, familial; Mismatch repair cancer syndrome | 600678 | |
| PMS | PMS1 | Forms heterodimers with MLH1. Encoded protein belongs to the DNA MMR mutL/hexB family. | Hereditary nonpolyposis colorectal cancer type 3 (HNPCC3); Lynch syndrome | 600258 |
| PMS2 | Forms MutL-alpha heterodimer (MLH1-PMS2 hetetrodimer) which activates endonucleolytic activity following recognition of mismatches and insertion/deletion loops by the MutS-alpha and MutS-beta heterodimers. | Colorectal cancer, hereditary nonpolyposis, type 4; Mismatch repair cancer syndrome | 600259 | |
| EXO1 | Encodes a protein with 5' to 3' exonuclease and RNase H activities. Similar to the Saccharomyces cerevisiae protein Exo1 which interacts with Msh2 for MMR. | 606063 | ||
| RFC | RFC1 | Encodes large subunit of replication factor C, a 5 subunit DNA polymerase accessory protein (DNA-dependent ATPase required for eukaryotic DNA replication and repair). | 102579 | |
| RFC2 | Encodes 40-kD subunit, responsible for binding ATP and may help promote cell survival | Disruption of this gene is associated with Williams syndrome | 600404 | |
| RFC3 | Encodes 38-kD subunit, responsible for binding ATP and may help promote cell survival | 600405 | ||
| RFC4 | Encodes 37-kD subunit, responsible for binding ATP and may help promote cell survival | 102577 | ||
| RFC5 | Encodes 36.5-kD subunit, responsible for binding ATP and may help promote cell survival | 600407 | ||
| PCNA | Encodes a protein which acts as a homotrimer and helps increase the process of leading strand synthesis during DNA replication, also involved in the RAD6-dependent DNA repair pathway | ataxia-telangiectasia-like disorder-2 (ATLD2) | 176740 | |
| LIG1 | Encodes a member of the ATP-dependent DNA ligase protein family, which functions in DNA replication, recombination, and the base excision repair process. | Mutations in gene leads to ligase-I deficiency resulting in immunodeficiency and increased sensitivity to DNA-damaging agents associated with variety of cancers | 126391 | |
| RPA | RPA1 | Encodes the subunit of heterotrimeric Replication Protein A (RPA) complex, which binds to single-stranded DNA, forming a nucleoprotein complex. Complex is involved in DNA metabolism, replication, repair, recombination, telomere maintenance. | knockdown of RPA1 in HeLa cells caused accumulation of cells in S and G2/M phases, followed by cell death | 179835 |
| RPA2 | Same as above | 179836 | ||
| RPA3 | Same as above | 179837 | ||
| POLD | POLD1 | Encodes a catalytic subunit of DNA polymerase delta, which possesses both polymerase and 3' to 5' exonuclease activity, important for DNA replication and repair. | Colorectal cancer, Susceptibility to, CRC-10; CRCS10; Mandibular hypoplasia, deafness, progeroid features, and lipodystrophy syndrome | 174761 |
| POLD2 | Encodes 50-kDa catalytic subunit of DNA polymerase delta which possesses both polymerase and 3' to 5' exonuclease activity and plays a critical role in DNA replication and repair. | Expression of this gene may be a marker for ovarian carcinomas | 600815 | |
| POLD3 | Encodes the 66-kDa subunit of DNA polymerase delta. | 611415 | ||
| POLD4 | Encodes the smallest subunit of DNA polymerase delta POLDS-P12. | 611525 | ||
Bioinformatic analysis
Raw reads (.fastq files) generated by the sequencer were processed by the following three major steps:
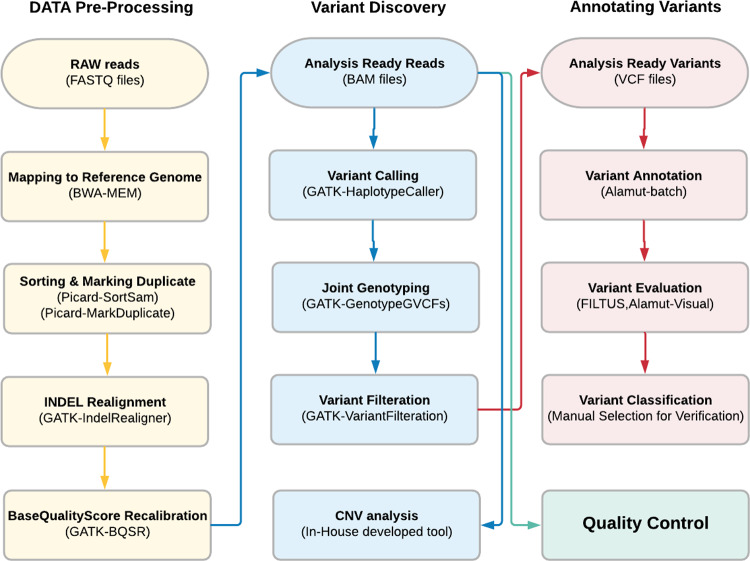
Data pre-processing: Raw reads were aligned to the reference genome (version hg19), and sequence alignment maps were generated. These alignment maps were used for read visualization and to call variants.
Variants discovery: The alignment maps generated from previous steps were compared against the reference genome to generate a list of nucleotide variants.
Variants annotation: Variants were annotated using different databases and tools.
A pipeline was constructed to perform the above-mentioned steps of analysis. Detailed overview of pipeline and tools used can be found as S1 File. Schematic overview of the pipeline is shown in Fig 1.
Fig 1. Schematic overview of the bioinformatics pipeline.
Filtration of variants
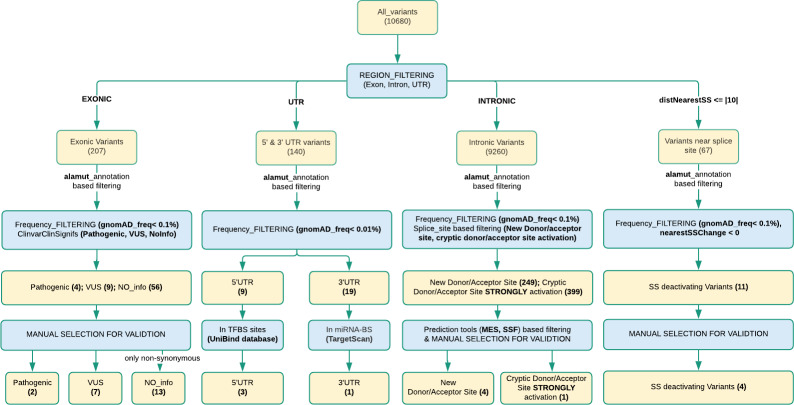
All called variants were annotated by using Alamut-batch [19] before filtering. Filtus [20] was used for filtering variants. All variants were classified into 4 region-wise categories; exons, UTRs, introns, and splice sites (variant distance ≤ 10 nucleotides from nearest splice site). In the first stage of filtering, variants from all these four regions were filtered based on frequencies of variants in the gnomAD database [21]. Exonic variants, intronic variants, and variants near splice sites were filtered-in for frequencies less than 0.1% (or no frequency). UTR variants were filtered-in for frequencies less than 0.01% (or no frequency). In further stages of filtering, different strategies were adopted for every region. See Fig 2 for the workflow. Detailed filtering steps can be found in S2 File.
Fig 2. Filtering workflow and number of genetic variants detected.
Validation of variants
Sanger sequencing was performed for validation of selected variants. The fragments were amplified using AmpliTaq Gold® 360 MasterMix and 360 GC Enhancer (Life Technologies). Cycle sequencing reaction was performed with BigDye® Terminator v3.1 (Life Technologies) and subsequent capillary electrophoresis was performed on the ABI 3130xl or ABI 3730 (Life Technologies). List of primer sequences can be provided upon request. Sanger sequencing data was analysed using SeqScape Software v3.0 (Life Technologies). Some variants have not been verified by Sanger sequencing, partly due to unavailability of primers for some of these gene, but also due to logistic issues. But variants were thoroughly inspected in BAM files to assure they were likely to be true positive variants (enough coverage and an allele fraction of about 50%, between 30 and 75%).
Interpretation and classification of DNA variants
The remaining variants after filtering were classified into 5 classes according to the American College of Medical genetics (ACMG) guidelines [22]. To determine whether these variants had been detected before, literature and databases including LOVD/InSIGHT (https://www.insight-group.org/variants/databases/) and ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/) were searched. Potential pathogenicity of missense variants was interpreted using Alamut batch (annotation) [19] and Alamut Visual (interpretation) [23].
Results and discussion
From all 199 samples, on average 99.8% of reads (per run) could be aligned to the reference genome (hg19) using BWA for alignment (see S1 File). Coverage depth of reads for samples and mean coverage depth for runs varied a lot among the 12 runs. Only 23 samples had a coverage of more than 100X (maximum 169X), and 50 samples had coverage of less than 30X (minimum 1X) (see S1 Table). Despite having multiple samples with low quality, the strategy for variant calling was uniformly applied to all samples. This was done to investigate the potential for identifying true variants even from target regions with low coverage depth. However, these low-quality data were not suitable for identification of copy number variants, and therefore CNV calling was not included in the final analysis.
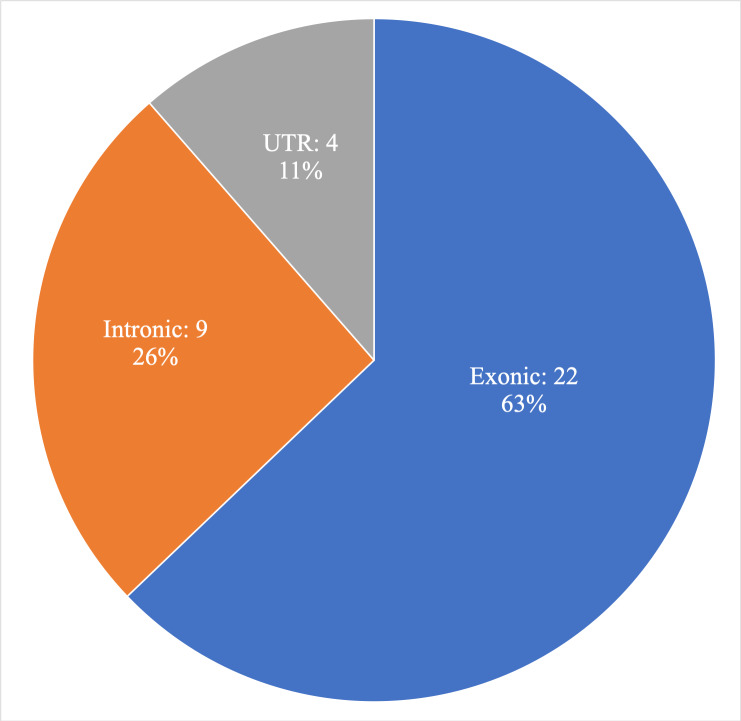
In total 10,680 unique variants (substitutions and INDELs) were called using the GATK toolkit. These variants could be classified into four categories according to genomic region; exonic, intronic, UTRs and splice-site neighbourhood (≤ |10|bp). See Fig 2 for the workflow. After filtering and annotation, 22 exonic, 9 intronic (4 variants in splice-site neighbourhood) and 4 UTR variants (Fig 3) were selected for further investigation for pathogenicity as potential cancer risk variants, and these variants are described below. See Table 2 for an aggregate list. Sanger verification was performed for 21 of these 35 variants. Remaining 14 variants are not Sanger validated. These 14 variants were designated as true variants by observing BAM files.
Fig 3. Investigated variants in different genomic regions.
Table 2. Aggregate list of variants and their classification according to the ACMG system.
| Sample ID | Other Cancersc | Family history of Cancerd | Genea | gNomen, cNomen, pNomen, rsID | Variant allele fraction | ClinVar / gnomAD | Class | Commentsb | References |
|---|---|---|---|---|---|---|---|---|---|
| 051783 | BC | 2nd° BC | MLH1 | Chr3:g.37042548A>G, NM_000249.3:c.306+4A>G, p.(?), rs267607733 | 0.35 | 6 x VUS /0.0012% | Class 3 | Activation of a cryptic donor site and the skipping of exon 3 in an ex vivo splicing minigene assay | [24] |
| 060337 | BC | NO | MLH1 | Chr3:g.37090414A>G, NM_000249.3:c.2009A>G, p.(Lys670Arg), rs905983196 | 0.49 | 3 x VUS / NIL | Class 3 | SS: Helix | |
| 051456 | NO | NO | MSH6* | Chr2:g.48010297:G>T, NM_000179.2:c.-76G>T, p.(?) | 0.64 | NIL/ NIL | Class 3 | No frequency, highly conserved | |
| 051026 | SC | NO | MSH6 | Chr2:g.48018140A>G, NM_000179.2:c.335A>G, p.(Asn112Ser), rs587779934 | 0.44 | 6 X VUS /0.0025% | Class 3 | New acceptor site predicted SS: Turn | |
| 051408 | NO | 2nd° CRC | MSH6 | Chr2:g.48025743C>A, NM_000179.2:c.628-7C>A, p.(?), rs373129248 | 0.41 | 6 x VUS /0.0093% | Class 3 | ||
| 051476 | NO | 1st° EC | MSH6 | Chr2:g.48026531C>G, NM_000179.2:c.1409C>G, p.(Ser470*) | 0.48 | NIL/ NIL | Class 5 | SS: Helix | |
| 051791 | NO | 1st° EC | MSH6 | Chr2:g.48027325C>A, NM_000179.2:c.2203C>A, p.(Leu735Ile), rs786204071 | 0.4 | 6 X VUS / NIL | Class 3 | ||
| 051280 | NO | NO | MSH6 | Chr2:g.48032048G>T, NM_000179.2:c.3439-1G>T, p.(?), rs587779263 | 0.5 | 8 X Pathogenic / NIL | Class 5 | ||
| 060162 | NO | 2nd° OC | MSH6 | Chr2:g.48033587_48033614dup, NM_000179.2:c.3802-4_3825dup, p.(Glu1276*) | 0.46 | NIL/ NIL | Class 5 | [25] | |
| 051233 | NO | 1st° BC | MSH2 | Chr2:g.47630427A>C, NM_000251.2:c.97A>C, p.(Thr33Pro), rs63751107 | 0.75 | 6 X VUS / 0.0056% | Class 3 | SS: Beta strand | [26, 27, 28–35, 36] |
| MSH3* | Chr5:g.79968115C>T, NM_002439.4:c.845C>T, p.(Thr282Ile), rs202184623 | 0.67 | NIL// 0.0053% | Class 3 | SS: Beta strand | ||||
| 051872 | 3 Melanomas | NO | MSH2 | Chr2:g.47657032G>T, NM_000251.2:c.1228G>T, p.(Gly410Cys), rs587782242 | 0.47 | 1 X VUS/ NIL | Class 3 | SS: Helix | |
| 051107 | Melanoma | NO | MSH2 | Chr2:g.47672680C>A, NM_000251.2:c.1277-7C>A, p.(?), rs375437307 | 0.57 | 3 X VUS/ 0.0037% | Class 3 | ||
| 051271 | BC | 1st° BC & PC, 2nd° CRC | MSH2 | Chr2:g.47710015T>G, NM_000251.2:c.2732T>G, p.(Leu911Arg), rs41295182 | 1 | 1 X VUS gnomAD: 0.0062% | Class 3 | SS: Helix | [34, 37–39] |
| 051179 | SKIN SPOTS | 1st° CRC | PMS2 | Chr7:g.6045549C>A, NM_001322014.1:c.137G>T, p.(Ser46Ile), rs121434629 | 0.44 | 12 X VUS:/ 0.0169% | Class 4 | Associated with diagnosis of CMMRD syndrome, SS: Helix | [40–47] |
| 051300 | NO | 1st° CRC & PC | 0.47 | ||||||
| 051657 | NO | 1st° OC | MSH3 | Chr5:g.80021325A>G, NM_002439.4:c.1394A>G, p.(Tyr465Cys), rs35009542 | 0.58 | NIL/ 0.0202% | Class 3 | SS: Helix | |
| 051172 | NO | NO | MSH3* | Chr5:g.79974804G>A, NM_002439.4:c.1232G>A, p.(Arg411His), rs764885728 | 0.49 | NIL/ 0.0012% | Class 3 | ||
| 051469 | PCOS | 2nd° UC | MSH3* | Chr5:g.80021327A>G, NM_002439.4:c.1396A>G, p.(Ser466Gly), rs766948921 | 0.51 | NIL/ 0.0025% | Class 3 | SS: Helix | |
| 060161 | NO | NO | MSH3* | Chr5:g.80063896C>T, NM_002439.4:c.2041C>T, p.(Pro681Ser), rs115198722 | 0.48 | NIL/ 0.0787% | Class 3 | SS: Helix | |
| 051330 | BC, SpC, LC, KC AND LiC | NO | 0.55 | ||||||
| 051610 | BrT | NO | POLD1 | Chr19:g.50905980G>A, NM_001308632.1:c.952G>A, p.(Glu318Lys), rs775232133 | 0.63 | 1 X VUS / NIL | Class 3 | highly conserved DIE | |
| 051406 | BC | 1st° BC | RFC1 | Chr4:g.39290383A>T, NM_001204747.1:c.3445T>A, p.(*1149Argext*15), rs149767968 | 0.59 | NIL/ 0.0065% | Class 3 | Altered stop codon, extension of protein with 15 aa | |
| RPA3 | Chr7:g.7676702A>G, NM_002947.4:c.295T>C, p.(Tyr99His) | 0.62 | NIL/ 0.0004% | Class 3 | SS: Helix | ||||
| 051663 | NO | 1st° BC | RFC1* | Chr4:g.39306530C>A, NM_001204747.1:c.2017G>T, p.(Val673Leu), rs28903096 | 0.33 | NIL/ 0.057% | Class 3 | ||
| 051400 | NO | 1st° Unknown CANCER | RFC1* | Chr4:g.39346049A>CNM_001204747.1:c.208+972T>G, p.(?) | 0.63 | NIL/ NIL | Class 3 | ||
| 051471 | NO | NO | RFC3 | Chr13:g.34392210:A>G, NM_002915.3:c.-106A>G, p.(?), rs554574193 | 0.57 | NIL/ 0.0064% | Class 3 | highly conserved | |
| 051640 | NO | 2nd° CRC | RFC4 | Chr3:g.186524157:G>A, NM_002916.3:c.-90C>T, p.(?) | 0.52 | NIL/ NIL | Class 3 | not conserved | |
| 051439 | NO | NO | RFC4* | Chr3:g.186518351T>C,NM_002916.3:c.210+555A>G, p.(?), rs781729102 | 0.55 | NIL/ 0.0387% | Class 3 | ||
| 051802 | UC | 1st° EC | LIG1 | Chr19:g.48640874G>A, NM_000234.2:c.1159C>T, p.(Arg387Cys), rs749929415 | 0.48 | NIL/ 0.0018% | Class 3 | SS: Beta strand | |
| 051133 | BC & OC | 1st° BC | LIG1* | Chr19:g.48653350A>C, NM_002439.4:c.692T>G, p.(Phe231Cys), rs767343361 | 0.37 | NIL/ 0.0079% | Class 3 | SS: Turn | |
| 051166 | BC & OC | 1st° BC | MLH1 | Chr3:g.37048554G>A, NM_000249.3:c.453G>A, p.(Thr151 =), rs369521379 | 0.51 | 9 x VUS /0.0011% | Class 3 | Last nucleotide of exon 5. ClinVar Miner: damage the nearby splice donor site (at -1 distance) and cause abnormal splicing. SS: Beta strand | |
| EXO1* | Chr1:g.242020650G>T, NM_006027.4:c.409G>T, p.(Ala137Ser), rs147663824 | 0.55 | NIL/ 0.0094% | Class 3 | SS: Helix | [48] | |||
| RPA3* | Chr7:g.7753847G>T, NM_002947.4:c.-1028+959C>A, p.(?) | 0.51 | NIL/ NIL | Class 3 | |||||
| 051267 | NO | 1st° PCOS | EXO1* | Chr1:g.242052986T>G, NM_130398.3:c.*84T>G, p.(?) | 0.5 | NIL/ NIL | Class3 | Can affect miRNA binding, for miR-370-3p and miR-93-3p | |
| 051007 | NO | NO | RPA1* | Chr17:g.1785509A>G,NM_002945.4:c.1241+1524A>G, p.(?), rs536796524 | 0.43 | NIL/ 0.0323% | Class 3 | It is within 1000 bp of a region that may be important for chromatin folding (Insulator / CTCF / SMC3 / RAD21) | |
| 051291 | NO | NO | RPA3* | Chr7:g.7695875T>C,NM_002947.4:c.-757-15069A>G, p.(?), rs946965390 | 0.54 | NIL/ NIL | Class 3 | It is within 2500 bp of a region that may be important for chromatin folding (Insulator / CTCF / SMC3 / RAD21) |
aVariants with
* not yet verified by Sanger sequencing;
bSS: Variant lies in Secondary Structure (UniProt)
cOther cancers: BC: Breast Cancer, CRC: Colorectal Cancer, PCOS: Polycystic Ovary Syndrome, PC: Prostate Cancer, UC: Uterine Cancer, EC: Endometerial Cancer,OC: Ovarian Cancer, SC: Skin Cancer, SpC: Spine Cancer, LC: Lung Cancer, KC: Kidney Cancer, LiC:Liver Cancer, BrT: Brain Tumor
dFamily history of cancer: 1st° & 2nd°: 1st & 2nd Degree relatives with cancer-type
Exonic variants
A total of 207 variants were called in exonic regions of the target panel, over all samples. The variants were filtered by removing cases according to their frequency in gnomAD (> 0.1%) and annotation in ClinVar (benign/likely-benign) [49]. Of the 22 exonic variants (S3 File) that remained after filtering, there were 2 putative pathogenic variants, 7 variants of unknown significance (VUS) and 13 variants without any information (NO_Info) according to ClinVar (only non-synonymous variants).
Among these 22 variants there were 2 variants in MLH1 (NM_000249.3). Both MLH1 variants were classified as class 3 in pathogenicity, according to ACMG guidelines [22]. The variant c.453G>A p.(Thr151 =) is found in the last nucleotide of exon 5. It may alter the ligation of adjacent exons 5 and 6 and is predicted to be splice site deactivating by prediction tools (SSF [50], MES [51]) (nearest-SS-change score: -0.29). The first and the last three positions of the exon are an integral part of the 3’ and 5’splice site consensus sequences [52], the variant position is highly conserved (PhastCons score: 0.99), and predicted as pathogenic by UMD-predictor [53]. According to ClinVar it is classified as a likely pathogenic / VUS variant, with multiple submissions in ClinVar where many of them has a HNPCC/Lynch syndrome phenotype. With strong evidences for being a pathogenic variant, it is a candidate for further RNA/functional studies. The variant c.2009A>G p.(Lys670Arg) has no frequency in the gnomAD database, but has recently been reported in ClinVar (as VUS) and in other databases. This variant has been associated with a HNPCC phenotype and hereditary cancer-predisposing syndrome, according to ClinVar. The variant position is highly conserved (PhastCons: 1, phyloP: 4.6) and lies in a helix secondary structure of the protein. It has been predicted as pathogenic (UMD-prediction, MutationTaster).
There were also four exonic variants in MSH6 (NM_000179.2). Two of the variants, c.335A>G p.(Asn112Ser) and c.2203C>A (p.Leu735Ile), have been classified as VUS by ClinVar. These two variants have previously been associated with Lynch syndrome, HNPCC and hereditary cancer-predisposing syndrome-like phenotype according to ClinVar and other databases. Both variants are at highly conserved positions and both have been predicted as damaging by prediction tools. We classified these two variants as class 3. Variants c.1409C>G p.(Ser470*) and c.3802-4_3825dup p.(Glu1276*) both code for “STOP gain” and are disease causing. None of these variants have entries in ClinVar or frequency in gnomAD. We classify these as class 5 variants.
Three exonic variants in MSH2 was identified (NM_000251.2), c.97A>C p.(Thr33Pro), c.1228G>T p.(Gly410Cys) and c.2732T>G p.(Leu911Arg), with all three classified as VUS by ClinVar. All three have phenotypic association to Lynch syndrome/HNPCC and hereditary cancer-predisposing syndrome and have been predicted as pathogenic/disease-causing by many prediction tools (UMD-prediction, PolyPhen, SIFT and MutationTaster). All three variant positions are highly conserved (with high scores in PhastCons and phyloP). Variant c.97A>C p.(Thr33Pro) was identified from a low quality sample (coverage depth at variant position 4X and sample coverage 7X), but was verified as a true variant by Sanger sequencing. It has been scored with a high value for decreasing protein stability (SNPs3D [54] score: -1.08) and has been suggested as a cause of reduced mismatch binding/release efficiency compared to wild-type protein in previous studies by Ollila et al. [26, 27]. Variant c.1228G>T p.(Gly410Cys) has no frequency in gnomAD, but has been reported to ClinVar and is located in a helix secondary structure of the protein. It has a high score for structural change (Grantham-Distance: 159), but it is predicted not to alter protein stability (SNPs3D: +3.43). Variant c.2732T>G p.(Leu911Arg) was also identified in a low quality sample (coverage depth at variant position 5X, sample 10X). It lies in a helix secondary structure, has high score for structural change (Grantham-Distance: 102) and for decreased protein stability (SNPs3D: -1.08). These three MSH2 variants have been classified as class 3.
A missense exonic variant in PMS2 was also detected (NM_001322014.), c.137G>T p.(Ser46Ile), which was found in two samples. It was classified as likely pathogenic according to ClinVar, and is reported to be a founder mutation [55]. The protein region has helix-like secondary structure (UniProt [56]), and the position is highly conserved (PhastCons [57] score:1; phyloP [58] score: 6.178). It has been classified as pathogenic by several prediction tools (UMD-predictor, PolyPhen [59], SIFT [60], and MutationTaster [61], the variant has been referred to in many previous studies, and it has been considered for strongly decreased DNA mismatch repair activity. This variant was classified as class 4.
One exonic variant in POLD1 was identified (NM_001308632.1), c.952G>A p.(Glu318Lys), was classified as VUS according to ClinVar. It was called in a low-quality sample (coverage depth at variant position 11X, sample’s mean coverage depth 22X). The position is highly conserved (PhastCons: 1, phyloP:3.9). The variant is in the DNA binding cleft of the exonuclease active domain of POLD1, it has a high score for decreased protein stability (SNPs3D: -2.68), and is predicted as damaging by prediction tools. A previous study has predicted it to be disease causing [62]. However, functional studies are needed to confirm pathogenicity, and therefore it was classified as class 3.
Exonic variants were also found in five other genes; MSH3, LIG1, RFC1, EXO1 and RPA3. All these variants were classified as class 3. In MSH3 (NM_002439.4) variants were c.1394A>G p.(Tyr465Cys), c.845C>T p.(Thr282Ile), c.1232G>A p.(Arg411His), c.1396A>G p.(Ser466Gly), c.2041C>T p.(Pro681Ser). In LIG1 (NM_000234.2) variants were c.1159C>T p.(Arg387Cys) and c.692T>G p.(Phe231Cys). In RFC1 (NM_001204747.1) this was c.3445T>A p.(*1149Argext*15), which introduces a “STOP loss” and extension of 15 amino acids in the product protein and c.2017G>T p.(Val673Leu); in EXO1 (NM_006027.4) c.409G>T p.(Ala137Ser); In RPA3 (NM_002947.4) it was c.295T>C p.(Tyr99His).
Intronic variants
Among all detected variants, 9,260 were identified as intronic, which was ~97% of all variants. Intronic regions of human DNA, being extraordinarily larger in comparison to other regions, it is expected to find most of the variants in these non-coding regions. After frequency-based filtering (< 0.1%), this list was reduced to 4,197 variants, which was further reduced by splice site related filtering, using strict filtering criteria to reduce the large number of variants. These variants were filtered for two categories, first for “New Donor/Acceptor site” and then for “Cryptic Donor/Acceptor Site STRONG activation” (see S2 File for filtering details). We found in total five variants, with four variants in the first category and one in the second (see S3 File). Two of these variants were in RPA1 and RPA3, and have been predicted as new acceptor site, two were in RFC1 and RFC4 and have been predicted as new donor sites, and one was in RPA3 and has been predicted to give strong activation of a cryptic donor site.
According to the Human Gene Mutation Database (HGMD) more than 10% of all disease-causing hereditary mutations are splice site altering [63–65]. Variants in vicinity of exon-intron junctions were therefore studied. After filtering (see Supporting Material), we found four variants of interest in the vicinity of splice sites (see S3 File). Two of these were in MSH6 (NM_000179.2). The variant c.628-7C>A has been classified as VUS by us and ClinVar, The variant c.3439-1G>T, at the last nucleotide of 5th intron, has been classified as pathogenic by ClinVar, it has been linked to LS/HNPCC phenotype, and has a maximum score (-1) for splice-site deactivation. We classified it as class 5 and hence disease causing.
An intronic variant in MLH1 (NM_000249.3: c.306+4A>G) is found close to a splicing junction and was predicted for splice site deactivation. It is in a highly conserved position (PhastCons:1, phyloP:4.2), and has been classified as VUS in ClinVar. Experimental studies have shown that this variant results in the activation of a cryptic donor site and skipping of exon 3 in an ex-vivo splicing minigene assay [24], but as no studies have verified this in patient samples, we classified it as class 3 variant. An intronic variant in MSH2 (NM_000251.2:c.1277-7C>A), previously classified as likely benign, we classified as a class 3 variant.
UTR variants
There were 140 variants identified in UTR regions. Due to limitations of annotation tools and databases, any effects of most mutations in these regions are hard to predict. Hence, a relatively strict filtering compared to standard (for diagnostics) [66] was used for variants in these regions, to reduce the number of variants to a manageable size. After frequency-based filtering (< 0.01%) this list reduced to 28 variants, of which 9 variants were in 5’ and 19 variants were in 3’ UTR.
Variants in 5’ UTR were annotated for transcription factor binding sites (TFBSs), using the UniBind database [67]. Among the 9 variants in 5’ UTR, three had significant hits in the database, where each of these three variants was found inside a potential binding site for at least one transcription factor (TF) according to UniBind data (see S2 Table). One variant in MSH6 (NM_000179.2: c.-76G>T) had overlap with potential binding sites for the TFs CTCF, STAT3, E2F7 and E2F1. For CTCF there is a high frequency of the reference allele (G) compared to the alternate allele (T) at the variant position, which can indicate a strong preference for the reference variant, and possibly a significant effect of the alternate variant on TFBS specificity (frequency matrices from the JASPAR database [68, 69] were used for this analysis). According to ChIP-seq data visualized with the UCSC genome browser [70] there are relatively strong signals for CTCF at this position (see S1 Fig) compared to other potential TFs. Mutations in CTCF binding sites have for example been associated with chromosomal instability and aberration and have been found in gastric and colorectal cancer [71], which strengthens the possibility that this variant may have an effect through altered binding of CTCF. A variant in RFC3 (NM_002915.3: c.-106A>G) had hits for the TFs GABPA, JUN, CREM, JUND, ATF1, MITF, NR3C1, ATF7 and CREB1. Among these hits, 6 TFs (JUN, CREM, JUND, R3C1, ATF7 and CREB1) had a very high frequency of the reference allele (A) compared to the alternate allele (G) at the variant position. ChIP-seq data shows strong signals for CREB1 (see S2 Fig.), which may indicate a potential for significant effects due to alteration in the binding site. A variant in RFC4 (NM_002916.3: c.-90C>T) had a hit for the TF AR.
Nineteen variants in 3’UTR were annotated using TargetScan v6.2 [72] and a two-step SVM prediction of micro-RNA (miRNA) target sites [73]. A SVM score normalization method [74] was used to normalize the score and miRNA data were taken from MirBase v22 [75]. Only a variant in gene EXO1 (NM_130398.3:c.*84T>G) was predicted as a likely true candidate for affecting miRNA binding, for miR-370-3p and miR-93-3p (see S3 Table). Several studies have shown the importance of EXO1 in replication, DNA repair pathways, cell cycle checkpoints and its association to cancer [76], and GWAS studies have identified specific mutations in EXO1 gene as risk alleles for different types of cancer [77, 78]. SNPs in miRNA binding sites have been associated with CRC [79]. For the two miRNAs predicted to be affected by variation in their binding site, miR-370-3p has been identified as a tumour suppressor in EC via endoglin regulation [80]. The miR-93-3p can be considered as an important factor for CRC suppression and inhibition of tumorigenesis [81], as a previous study has associated the down-regulation of miR-93 with unfavourable clinicopathologic features and short overall survival of CRC patients [82].
Implications of the study
In this study we found 35 significant variants (22 exonic, 4 UTR, 9 intronic), with 15 variants in the 4 MMR genes known to cause LS (MLH1, MSH2, MSH6, PMS2) and 20 in the additional MMR genes included in this study (MSH3, POLD1, RFC1, RFC3, RFC4, LIG1, EXO1, RPA1, RPA3). This helped in identification of variants in less studied genes, as well as polygenic variations (although none of the 199 samples in this particular study showed polygenic variants of interest for further investigations). This study also used the complete genomic regions of the genes, which very few previous studies have done [83, 84].
Though all known genes in the MMR pathway were studied, there will always be a possibility of additional genes and associated variants with similar disease effects, e.g., POLE mutations in EC cases contributing towards Polymerase Proofreading Associated Polyposis (PPAP) [85, 86], or germline deletions in another gene (EPCAM1) leading to silencing of the MSH2 gene, causing Lynch syndrome [87]. These limitations can only be removed by expanding the panel by including more genes, up to the extent of the whole genome. However, this will also increase the potential of noise and complexity of the analysis, by including more genes and variants that are less likely to be relevant in a given study. Another limitation is associated with the PMS2 gene in this panel, which has a pseudo-gene (PMS2CL), and where 6 exons (exon 9, 11, 12, 13, 14 & 15) are highly similar to PMS2CL. This creates challenges in alignment of correct reads at these exons and creates artefacts during variant calling. This limitation has also been mentioned in a pilot study [83]. This makes it important to manually check reads and coverage in a genomic viewer, and to do Sanger verification of variants, as we did for the PMS2 gene.
The current study emphasises the importance of including non-coding intronic regions. These regions will often have splice site variants, which may contribute to 10% of all disease-causing hereditary mutations according to HGMD [63–65], and deep intronic variants (e.g., in branch-point sequences, U2 type introns) which also contribute towards disease, most frequently by creating new pseudo-exons by activating non-trivial splice sites or by changing splicing regulatory elements. Intronic variants can also disrupt transcription regulatory motifs and non-coding RNA genes [88]. However, it is challenging to annotate these intronic variants due to limitations of annotation databases and tools. In a clinical setting, these variants can easily be missed unless RNA studies are performed to check for exon skipping, generation of new donor sites or cryptic site activation. Considering the potential importance of such variants, the current study included all intronic regions in order to search for this type of variant. Among 10 significant intronic variants we found four in the splice site vicinity and six in deep intronic regions.
NGS was performed, aiming at a data quality greater than 100X (average read coverage depth) for all samples. However, only 23 samples achieved this coverage (highest among them 169X), whereas 50 samples had coverage of less than 30X. These low-quality samples were included in the study, with the aim of exploring the value of low-quality data when searching for true positive (TP) variants. Using low quality data (i.e., with low coverage) led to a higher fraction of false positive (FP) variants, as 16 variants identified from the data analysis were subsequently identified as false positive variants by Sanger sequencing. Most of them had low coverage at the variant position (between 14X to 6X coverage), whereas others were in repeat regions. FP variants in MLH1, MSH6 & PMS2 genes were in repeat regions, and had low coverage (except a PMS2 variant with 84X coverage), which possibly led to their false SNV call. On the other hand, we cannot rule out that some were not verified due to SNPs in the primer binding site (allelic dropout). However, we also found many true positive variants in low coverage regions, as we found and confirmed 6 true positive variants in regions with low coverage (between 16X and 4X). Among these were two class 3 variants (MSH2), one class 3+ variant (POLD1) and a class 5 variant (MSH6). This shows the potential for finding true variants of significance even in low-quality samples, given that the variants can be verified.
Our initial aim also included identification of CNVs. CNVs can occur in both exonic and intronic regions of protein coding genes, with intronic CNVs being more frequent [89], and both types can contribute towards disease. However, due to the limitations of data quality (non-uniform and low coverage depth), it was not possible to do reliable CNV calling. Also, there is no availability of MLPA kits (MRC-Holland) for detecting CNVs for many genes in this panel.
To associate variants with possible effects we utilized in silico resources and tools, in addition to published literature. Effect prediction and annotation of all variants was done using multiple tools as mentioned in the methods section. Also, multiple potential factors and effects, like conservation in variant position or structural changes at protein level, were checked for each variant. This consensus-like approach (multiple tools, multiple potential effects) increases the robustness of predictions and annotations of the variants, although we also had cases of contradictory predictions, which illustrates the challenge of using in silico prediction tools.
Among the 199 EC patient samples, we identified variants of interest (for further investigations) in 34 patients. Among these, we found 3 patients with class 5 variants (in MSH6 gene) and two patients with the same class 4 variant (in PMS2 gene); ~2,5% of patients had pathogenic variants representing a very likely cause of cancer in these five patients. This is in accordance with other studies. One meta-analysis of 53 studies concluded the prevalence of LS in EC patients to be approximately 3% [90]. These studies have only looked into the coding part of the four MMR genes MLH1, MSH2, MSH6 and PMS2. We found class 3 variants in another 29 patients, some of which are highly suspicious of being pathogenic variants. This indicates potential causes of their disease, although further studies are required to confirm their actual significance. It is an important limitation for further interpretation of these class 3 variants that we lack information about the patients debut age of cancer, and results from tumour analyses (MSI status and immunohistochemistry of MMR genes). For the remaining 164 patients, we did not find any significant variant to explain their disease. Expansion of panel size with more genes, improved annotation (particularly of variants in non-protein-coding regions), and improved data quality may help in explanation of some of these cases. However, since the study cohort consist of consecutive EC patients, most of the cancers will be sporadic with no underlying high penetrant genetic cause.
Conclusions
Including all genes of the MMR pathway in a gene panel provides opportunity to discover variants in additional genes that potentially can be associated with a risk for EC, and hence are relevant for further investigation towards a better understanding of the development of EC. Including non-coding parts provides chances of identifying gene regulation or splice site alteration variants, although this will lead to a larger number of unknown variants which is challenging to study and annotate. In silico tools can be useful to find some leads in this situation, although their predictions can be ambiguous and noisy. Hence in silico tools should not be used in identifying pathogenicity by themselves. In addition, although low-quality data should be avoided, such data can still support identification of informative variants. But such data will also lead to increased noise in the analysis, and experimental verification of such variants is essential. We identified pathogenic MMR variants in the same order of magnitude as earlier reported. In addition, we identified 31 class-3 (VUS) variants some of which may be disease causing. This supports that screening for LS among EC patients should be recommended. However, to determine whether the use of an extended panel of MMR genes (beyond MLH1, MSH2, MSH6 and PMS2) has clinical value needs further investigation.
Supporting information
(TIF)
(TIF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(XLSX)
Data Availability
Data contain confidential information and cannot be shared publicly as per guidelines from Hunter New England Human Research Ethics Committee. Data may be made available by request to Rodney Scott (rodney.scott@health.nsw.gov.au) for researchers who meet the criteria for access to this confidential data.
Funding Statement
This research grant was awarded to BTP by Cancer Institute NSW (https://www.cancer.nsw.gov.au/), (Grant number: 12/ECF/2-34). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018. November 1;68(6):394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2.Lortet-Tieulent J, Ferlay J, Bray F, Jemal A. International Patterns and Trends in Endometrial Cancer Incidence, 1978–2013. JNCI J Natl Cancer Inst. 2017. October 16;110(4):354–61. [DOI] [PubMed] [Google Scholar]
- 3.Jemal A, Siegel R, Xu J, Ward E. Cancer Statistics, 2010. CA Cancer J Clin. 2010. September 1;60(5):277–300. 10.3322/caac.20073 [DOI] [PubMed] [Google Scholar]
- 4.Colombo N, Preti E, Landoni F, Carinelli S, Colombo A, Marini C, et al. Endometrial cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013. October 1;24(suppl 6):vi33–8. [DOI] [PubMed] [Google Scholar]
- 5.Jenabi E, Poorolajal J. The effect of body mass index on endometrial cancer: a meta-analysis. Public Health. 2015. July 1;129(7):872–80. 10.1016/j.puhe.2015.04.017 [DOI] [PubMed] [Google Scholar]
- 6.Banno K, Yanokura M, Kobayashi Y, Kawaguchi M, Nomura H, Hirasawa A, et al. Endometrial cancer as a familial tumor: pathology and molecular carcinogenesis (review). Curr Genomics. 2009. April;10(2):127–32. 10.2174/138920209787847069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kunitomi H, Banno K, Yanokura M, Takeda T, Iijima M, Nakamura K, et al. New use of microsatellite instability analysis in endometrial cancer. Oncol Lett. 2017;14(3):3297 10.3892/ol.2017.6640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Resnick KE, Frankel WL, Morrison CD, Fowler JM, Copeland LJ, Stephens J, et al. Mismatch repair status and outcomes after adjuvant therapy in patients with surgically staged endometrial cancer ☆. Gynecol Oncol. 2010;117:234–8. 10.1016/j.ygyno.2009.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kawaguchi M, Banno K, Yanokura M, Kobayashi Y, Kishimi A, Ogawa S, et al. Analysis of candidate target genes for mononucleotide repeat mutation in microsatellite instability-high (MSI-H) endometrial cancer. Int J Oncol. 2009. September 15;35(05):977–82. [DOI] [PubMed] [Google Scholar]
- 10.Bansidhar BJ. Extracolonic Manifestations of Lynch Syndrome. Clin Colon Rectal Surg. 2012;25:103–10. 10.1055/s-0032-1313781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barrow E, Hill J, Evans DG. Cancer risk in Lynch Syndrome. Fam Cancer. 2013. June 21;12(2):229–40. 10.1007/s10689-013-9615-1 [DOI] [PubMed] [Google Scholar]
- 12.Ferguson SE, Aronson M, Pollett A, Eiriksson LR, Oza AM, Gallinger S, et al. Performance characteristics of screening strategies for Lynch syndrome in unselected women with newly diagnosed endometrial cancer who have undergone universal germline mutation testing. Cancer. 2014. December 15;120(24):3932–9. 10.1002/cncr.28933 [DOI] [PubMed] [Google Scholar]
- 13.Cunningham JM, Christensen ER, Tester DJ, Kim CY, Roche PC, Burgart LJ, et al. Hypermethylation of the hMLH1 promoter in colon cancer with microsatellite instability. Cancer Res. 1998. August 1;58(15):3455–60. [PubMed] [Google Scholar]
- 14.Herman JG, Umar A, Polyak K, Graff JR, Ahuja N, Issa JP, et al. Incidence and functional consequences of hMLH1 promoter hypermethylation in colorectal carcinoma. Proc Natl Acad Sci U S A. 1998. June 9;95(12):6870–5. 10.1073/pnas.95.12.6870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haraldsdottir S, Hampel H, Tomsic J, Frankel WL, Pearlman R, de la Chapelle A, et al. Colon and Endometrial Cancers With Mismatch Repair Deficiency Can Arise From Somatic, Rather Than Germline, Mutations. Gastroenterology. 2014. December 1;147(6):1308-1316.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonis PA, Trikalinos TA, Chung M, Chew P, Ip S, Devine DA, et al. Hereditary Nonpolyposis Colorectal Cancer: Diagnostic Strategies and Their Implications [Internet]. 2007. [cited 2018 Sep 3]. [PMC free article] [PubMed] [Google Scholar]
- 17.Ashton KA, Proietto A, Otton G, Symonds I, McEvoy M, Attia J, et al. The influence of the Cyclin D1 870 G>A polymorphism as an endometrial cancer risk factor. BMC Cancer. 2008. September 29;8:272 10.1186/1471-2407-8-272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Illumina. Illimina MiSeq.
- 19.Alamut. Alamut-batch [Internet]. Interactive Biosoftware, Rouen, France;
- 20.Vigeland MD, Gjøtterud KS, Selmer KK. FILTUS: a desktop GUI for fast and efficient detection of disease-causing variants, including a novel autozygosity detector. Bioinformatics. 2016. January 27;32(10):1592–4. 10.1093/bioinformatics/btw046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alföldi J, Wang Q, et al. Variation across 141,456 human exomes and genomes reveals the spectrum of loss-of-function intolerance across human protein-coding genes. bioRxiv. 2019. January 30;531210. [Google Scholar]
- 22.Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–23. 10.1038/gim.2015.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alamut. Alamut-visual [Internet]. Interactive Biosoftware, Rouen, France;
- 24.Tournier I, Vezain M, Martins A, Charbonnier F, Baert-Desurmont S, Olschwang S, et al. A large fraction of unclassified variants of the mismatch repair genes MLH1 and MSH2 is associated with splicing defects. Hum Mutat. 2008. December 1;29(12):1412–24. 10.1002/humu.20796 [DOI] [PubMed] [Google Scholar]
- 25.Lo SM, Choi M, Liu J, Jain D, Boot RG, Kallemeijn WW, et al. Phenotype diversity in type 1 Gaucher disease: discovering the genetic basis of Gaucher disease/hematologic malignancy phenotype by individual genome analysis. Blood. 2012. May 17;119(20):4731 10.1182/blood-2011-10-386862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ollila S, Sarantaus L, Kariola R, Chan P, Hampel H, Holinski–Feder E, et al. Pathogenicity of MSH2 Missense Mutations Is Typically Associated With Impaired Repair Capability of the Mutated Protein. Gastroenterology. 2006. November 1;131(5):1408–17. 10.1053/j.gastro.2006.08.044 [DOI] [PubMed] [Google Scholar]
- 27.Ollila S, Bebek DD, Jiricny J, Nyström M. Mechanisms of pathogenicity in human MSH2 missense mutants. Hum Mutat. 2008;29(11):1355–63. 10.1002/humu.20893 [DOI] [PubMed] [Google Scholar]
- 28.Hegde M, Blazo M, Chong B, Prior T, Richards C. Assay validation for identification of hereditary nonpolyposis colon cancer-causing mutations in mismatch repair genes MLH1, MSH2, and MSH6. J Mol Diagnostics. 2005;7(4):525–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hampel H, Frankel W, Panescu J, Lockman J, Sotamaa K, Fix D, et al. Screening for Lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients. Cancer Res. 2006. August 1;66(15):7810–7. 10.1158/0008-5472.CAN-06-1114 [DOI] [PubMed] [Google Scholar]
- 30.Ou J, Niessen RC, Lützen A, Sijmons RH, Kleibeuker JH, de Wind N, et al. Functional analysis helps to clarify the clinical importance of unclassified variants in DNA mismatch repair genes. Hum Mutat. 2007. November;28(11):1047–54. 10.1002/humu.20580 [DOI] [PubMed] [Google Scholar]
- 31.Chao EC, Velasquez JL, Witherspoon MSL, Rozek LS, Peel D, Ng P, et al. Accurate classification of MLH1/MSH2 missense variants with Multivariate Analysis of Protein Polymorphisms-Mismatch Repair (MAPP-MMR). Hum Mutat. 2008. June;29(6):852–60. 10.1002/humu.20735 [DOI] [PubMed] [Google Scholar]
- 32.Martinez SL, Kolodner RD. Functional analysis of human mismatch repair gene mutations identifies weak alleles and polymorphisms capable of polygenic interactions. Proc Natl Acad Sci U S A. 2010. March 16;107(11):5070–5. 10.1073/pnas.1000798107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kansikas M, Kariola R, Nyström M. Verification of the three-step model in assessing the pathogenicity of mismatch repair gene variants. Hum Mutat. 2011. January;32(1):107–15. 10.1002/humu.21409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thompson BA, Greenblatt MS, Vallee MP, Herkert JC, Tessereau C, Young EL, et al. Calibration of Multiple In Silico Tools for Predicting Pathogenicity of Mismatch Repair Gene Missense Substitutions. Hum Mutat. 2013. January;34(1):255–65. 10.1002/humu.22214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chubb D, Broderick P, Frampton M, Kinnersley B, Sherborne A, Penegar S, et al. Genetic diagnosis of high-penetrance susceptibility for colorectal cancer (CRC) is achievable for a high proportion of familial CRC by exome sequencing. J Clin Oncol. 2015. February 10;33(5):426–32. 10.1200/JCO.2014.56.5689 [DOI] [PubMed] [Google Scholar]
- 36.Houlleberghs H, Dekker M, Lantermans H, Kleinendorst R, Dubbink HJ, Hofstra RMW, et al. Oligonucleotide-directed mutagenesis screen to identify pathogenic Lynch syndrome-associated MSH2 DNA mismatch repair gene variants. Proc Natl Acad Sci U S A. 2016. April 12;113(15):4128–33. 10.1073/pnas.1520813113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pal T, Akbari MR, Sun P, Lee J-H, Fulp J, Thompson Z, et al. Frequency of mutations in mismatch repair genes in a population-based study of women with ovarian cancer. Br J Cancer. 2012. November 6;107(10):1783–90. 10.1038/bjc.2012.452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barnetson RA, Cartwright N, van Vliet A, Haq N, Drew K, Farrington S, et al. Classification of ambiguous mutations in DNA mismatch repair genes identified in a population-based study of colorectal cancer. Hum Mutat. 2008. March;29(3):367–74. 10.1002/humu.20635 [DOI] [PubMed] [Google Scholar]
- 39.Karageorgos I, Mizzi C, Giannopoulou E, Pavlidis C, Peters BA, Zagoriti Z, et al. Identification of cancer predisposition variants in apparently healthy individuals using a next-generation sequencing-based family genomics approach. Hum Genomics. 2015. December 20;9(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drost M, Koppejan H, de Wind N. Inactivation of DNA mismatch repair by variants of uncertain significance in the PMS2 gene. Hum Mutat. 2013. November;34(11):1477–80. 10.1002/humu.22426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Senter L, Clendenning M, Sotamaa K, Hampel H, Green J, Potter JD, et al. The Clinical Phenotype of Lynch Syndrome Due to Germ-Line PMS2 Mutations. Gastroenterology. 2008. August 1;135(2):419–428.e1. 10.1053/j.gastro.2008.04.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van der Klift HM, Mensenkamp AR, Drost M, Bik EC, Vos YJ, Gille HJJP, et al. Comprehensive Mutation Analysis of PMS2 in a Large Cohort of Probands Suspected of Lynch Syndrome or Constitutional Mismatch Repair Deficiency Syndrome. Hum Mutat. 2016. November 1;37(11):1162–79. 10.1002/humu.23052 [DOI] [PubMed] [Google Scholar]
- 43.Borràs E, Pineda M, Cadiñanos J, Del Valle J, Brieger A, Hinrichsen I, et al. Refining the role of PMS2 in Lynch syndrome: germline mutational analysis improved by comprehensive assessment of variants. J Med Genet. 2013. August 1;50(8):552–63. 10.1136/jmedgenet-2012-101511 [DOI] [PubMed] [Google Scholar]
- 44.Auclair J, Leroux D, Desseigne F, Lasset C, Saurin JC, Joly MO, et al. Novel biallelic mutations inMSH6 andPMS2 genes: gene conversion as a likely cause ofPMS2 gene inactivation. Hum Mutat. 2007. November 1;28(11):1084–90. 10.1002/humu.20569 [DOI] [PubMed] [Google Scholar]
- 45.Brohl AS, Patidar R, Turner CE, Wen X, Song YK, Wei JS, et al. Frequent inactivating germline mutations in DNA repair genes in patients with Ewing sarcoma. Genet Med. 2017. August 1;19(8):955–8. 10.1038/gim.2016.206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nowak JA, Yurgelun MB, Bruce JL, Rojas-Rudilla V, Hall DL, Shivdasani P, et al. Detection of Mismatch Repair Deficiency and Microsatellite Instability in Colorectal Adenocarcinoma by Targeted Next-Generation Sequencing. J Mol Diagnostics. 2017. January 1;19(1):84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rengifo-Cam W, Jasperson K, Garrido-Laguna I, Colman H, Scaife C, Samowitz W, et al. A 30-Year-Old Man with Three Primary Malignancies: A Case of Constitutional Mismatch Repair Deficiency. ACG Case Reports J. 2017;4(1):e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jagmohan-Changur S, Poikonen T, Vilkki S, Launonen V, Wikman F, Orntoft TF, et al. EXO1 variants occur commonly in normal population: evidence against a role in hereditary nonpolyposis colorectal cancer. Cancer Res. 2003. January 1;63(1):154–8. [PubMed] [Google Scholar]
- 49.Landrum MJ, Lee JM, Riley GR, Jang W, Rubinstein WS, Church DM, et al. ClinVar: public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res. 2013. November 14;42(D1):D980–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shapiro MB, Senapathy P. RNA splice junctions of different classes of eukaryotes: sequence statistics and functional implications in gene expression. Nucleic Acids Res. 1987. September 11;15(17):7155–74. 10.1093/nar/15.17.7155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yeo G, Burge CB. Maximum Entropy Modeling of Short Sequence Motifs with Applications to RNA Splicing Signals. J Comput Biol. 2004. March;11(2–3):377–94. 10.1089/1066527041410418 [DOI] [PubMed] [Google Scholar]
- 52.Soukarieh O, Gaildrat P, Hamieh M, Drouet A, Baert-Desurmont S, Frébourg T, et al. Exonic Splicing Mutations Are More Prevalent than Currently Estimated and Can Be Predicted by Using In Silico Tools. Aretz S, editor. PLOS Genet. 2016. January 13;12(1):e1005756 10.1371/journal.pgen.1005756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Salgado D, Desvignes J-P, Rai G, Blanchard A, Miltgen M, Pinard A, et al. UMD-Predictor: A High-Throughput Sequencing Compliant System for Pathogenicity Prediction of any Human cDNA Substitution. Hum Mutat. 2016. May;37(5):439–46. 10.1002/humu.22965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yue P, Melamud E, Moult J. SNPs3D: candidate gene and SNP selection for association studies. BMC Bioinformatics. 2006. March 22;7(1):166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tomsic J, Senter L, Liyanarachchi S, Clendenning M, Vaughn CP, Jenkins MA, et al. Recurrent and founder mutations in the PMS2 gene. Clin Genet. 2013. March 1;83(3):238–43. 10.1111/j.1399-0004.2012.01898.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bateman A, Martin MJ, O’Donovan C, Magrane M, Alpi E, Antunes R, et al. UniProt: the universal protein knowledgebase. Nucleic Acids Res. 2017. January 4;45(D1):D158–69. 10.1093/nar/gkw1099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Siepel A, Bejerano G, Pedersen JS, Hinrichs AS, Hou M, Rosenbloom K, et al. Evolutionarily conserved elements in vertebrate, insect, worm, and yeast genomes. Genome Res. 2005. August 1;15(8):1034–50. 10.1101/gr.3715005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pollard KS, Hubisz MJ, Rosenbloom KR, Siepel A. Detection of nonneutral substitution rates on mammalian phylogenies. Genome Res. 2010. January 1;20(1):110–21. 10.1101/gr.097857.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Adzhubei I, Jordan DM, Sunyaev SR. Predicting functional effect of human missense mutations using PolyPhen-2. Curr Protoc Hum Genet. 2013. January;Chapter 7:Unit7.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ng PC, Henikoff S. SIFT: Predicting amino acid changes that affect protein function. Nucleic Acids Res. 2003. July 1;31(13):3812–4. 10.1093/nar/gkg509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schwarz JM, Cooper DN, Schuelke M, Seelow D. MutationTaster2: mutation prediction for the deep-sequencing age. Nat Methods. 2014. April 1;11(4):361–2. 10.1038/nmeth.2890 [DOI] [PubMed] [Google Scholar]
- 62.Haradhvala NJ, Kim J, Maruvka YE, Polak P, Rosebrock D, Livitz D, et al. Distinct mutational signatures characterize concurrent loss of polymerase proofreading and mismatch repair. Nat Commun. 2018. Dec 1;9(1):1746 10.1038/s41467-018-04002-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Krawczak M, Thomas NST, Hundrieser B, Mort M, Wittig M, Hampe J, et al. Single base-pair substitutions in exon-intron junctions of human genes: nature, distribution, and consequences for mRNA splicing. Hum Mutat. 2007. February 1;28(2):150–8. 10.1002/humu.20400 [DOI] [PubMed] [Google Scholar]
- 64.Stenson PD, Mort M, Ball E V, Howells K, Phillips AD, Thomas NS, et al. The Human Gene Mutation Database: 2008 update. Genome Med. 2009. January 22;1(1):13 10.1186/gm13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cooper DN. Functional intronic polymorphisms: Buried treasure awaiting discovery within our genes. Hum Genomics. 2010. June;4(5):284–8. 10.1186/1479-7364-4-5-284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.InSiGHT Variant Interpretation Committee: Mismatch Repair Gene Variant Classification Criteria Rules for Variant Classification [Internet]. 2018 [cited 2019 Nov 15].
- 67.Gheorghe M, Sandve GK, Khan A, Cheneby J, Ballester B, Mathelier A. A map of direct TF-DNA interactions in the human genome. bioRxiv. 2018. August 17;394205. [Google Scholar]
- 68.Sandelin A, Alkema W, Engström P, Wasserman WW, Lenhard B. JASPAR: an open-access database for eukaryotic transcription factor binding profiles. Nucleic Acids Res. 2004. January 1;32(90001):91D – 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Khan A, Fornes O, Stigliani A, Gheorghe M, Castro-Mondragon JA, van der Lee R, et al. JASPAR 2018: update of the open-access database of transcription factor binding profiles and its web framework. Nucleic Acids Res. 2018. January 4;46(D1):D260–6. 10.1093/nar/gkx1126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kent WJ, Sugnet CW, Furey TS, Roskin KM, Pringle TH, Zahler AM, et al. The human genome browser at UCSC. Genome Res. 2002. June;12(6):996–1006. 10.1101/gr.229102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guo YA, Chang MM, Huang W, Ooi WF, Xing M, Tan P, et al. Mutation hotspots at CTCF binding sites coupled to chromosomal instability in gastrointestinal cancers. Nat Commun. 2018. December 18;9(1):1520 10.1038/s41467-018-03828-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Garcia DM, Baek D, Shin C, Bell GW, Grimson A, Bartel DP. Weak seed-pairing stability and high target-site abundance decrease the proficiency of lsy-6 and other microRNAs. Nat Struct Mol Biol. 2011. October 11;18(10):1139–46. 10.1038/nsmb.2115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saito T, Sætrom P. A two-step site and mRNA-level model for predicting microRNA targets. BMC Bioinformatics. 2010. December 31;11(1):612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Thomas LF, Saito T, Sætrom P. Inferring causative variants in microRNA target sites. Nucleic Acids Res. 2011. September 1;39(16):e109–e109. 10.1093/nar/gkr414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kozomara A, Griffiths-Jones S. miRBase: integrating microRNA annotation and deep-sequencing data. Nucleic Acids Res. 2011. January 1;39(Database):D152–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Keijzers G, Bakula D, Petr M, Madsen N, Teklu A, Mkrtchyan G, et al. Human Exonuclease 1 (EXO1) Regulatory Functions in DNA Replication with Putative Roles in Cancer. Int J Mol Sci. 2018. December 25;20(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhang M, Zhao D, Yan C, Zhang L, Liang C. Associations between Nine Polymorphisms in EXO1 and Cancer Susceptibility: A Systematic Review and Meta-Analysis of 39 Case-control Studies. Sci Rep. 2016. September 8;6(1):29270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Michailidou K, Beesley J, Lindstrom S, Canisius S, Dennis J, Lush MJ, et al. Genome-wide association analysis of more than 120,000 individuals identifies 15 new susceptibility loci for breast cancer. Nat Genet. 2015. April 9;47(4):373–80. 10.1038/ng.3242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kang BW, Jeon H-S, Chae YS, Lee SJ, Park JS, Choi GS, et al. Impact of Genetic Variation in MicroRNA-binding Site on Susceptibility to Colorectal Cancer. Anticancer Res. 2016. July 1;36(7):3353–61. [PubMed] [Google Scholar]
- 80.Chen X-P, Chen Y-G, Lan J-Y, Shen Z-J. MicroRNA-370 suppresses proliferation and promotes endometrioid ovarian cancer chemosensitivity to cDDP by negatively regulating ENG. Cancer Lett. 2014. October 28;353(2):201–10. 10.1016/j.canlet.2014.07.026 [DOI] [PubMed] [Google Scholar]
- 81.Yang I-P, Tsai H-L, Hou M-F, Chen K-C, Tsai P-C, Huang S-W, et al. MicroRNA-93 inhibits tumor growth and early relapse of human colorectal cancer by affecting genes involved in the cell cycle. Carcinogenesis. 2012. August 1;33(8):1522–30. 10.1093/carcin/bgs166 [DOI] [PubMed] [Google Scholar]
- 82.Xiao Z-G, Deng Z-S, Zhang Y-D, Zhang Y, Huang Z-C. Clinical significance of microRNA-93 downregulation in human colon cancer. Eur J Gastroenterol Hepatol. 2013. March;25(3):296–301. 10.1097/MEG.0b013e32835c077a [DOI] [PubMed] [Google Scholar]
- 83.Talseth-Palmer BA, Bauer DC, Sjursen W, Evans TJ, Mcphillips M, Proietto A, et al. Targeted next-generation sequencing of 22 mismatch repair genes identifies Lynch syndrome families. Cancer Med. 2016;5(5):929–41. 10.1002/cam4.628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Xavier A, Olsen MF, Lavik LA, Johansen J, Singh AK, Sjursen W, et al. Comprehensive mismatch repair gene panel identifies variants in patients with Lynch-like syndrome. Mol Genet Genomic Med. 2019. August 1;7(8):e850 10.1002/mgg3.850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Billingsley CC, Cohn DE, Mutch DG, Stephens JA, Suarez AA, Goodfellow PJ. Polymerase ɛ (POLE) mutations in endometrial cancer: clinical outcomes and implications for Lynch syndrome testing. Cancer. 2015. February 1;121(3):386–94. 10.1002/cncr.29046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Konstantinopoulos PA, Matulonis UA. POLE mutations as an alternative pathway for microsatellite instability in endometrial cancer: Implications for Lynch syndrome testing. Cancer. 2015. February 1;121(3):331–4. 10.1002/cncr.29057 [DOI] [PubMed] [Google Scholar]
- 87.Huth C, Kloor M, Voigt AY, Bozukova G, Evers C, Gaspar H, et al. The molecular basis of EPCAM expression loss in Lynch syndrome-associated tumors. Mod Pathol. 2012;25(6):911–6. 10.1038/modpathol.2012.30 [DOI] [PubMed] [Google Scholar]
- 88.Vaz-Drago R, Custódio N, Carmo-Fonseca M. Deep intronic mutations and human disease. Hum Genet. 2017. September 12;136(9):1093–111. 10.1007/s00439-017-1809-4 [DOI] [PubMed] [Google Scholar]
- 89.Rigau M, Juan D, Valencia A, Rico D. Intronic CNVs and gene expression variation in human populations. Semple C, editor. PLOS Genet. 2019. January 24;15(1):e1007902 10.1371/journal.pgen.1007902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ryan NAJ, Glaire MA, Blake D, Cabrera-Dandy M, Evans DG, Crosbie EJ. The proportion of endometrial cancers associated with Lynch syndrome: a systematic review of the literature and meta-analysis. Genet Med. 2019;21(10):2167–80. 10.1038/s41436-019-0536-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(XLSX)
Data Availability Statement
Data contain confidential information and cannot be shared publicly as per guidelines from Hunter New England Human Research Ethics Committee. Data may be made available by request to Rodney Scott (rodney.scott@health.nsw.gov.au) for researchers who meet the criteria for access to this confidential data.