Abstract
Aims
As large population-based studies of aortic dissection are lacking, the incidence numbers and knowledge about time-trends and sex differences are uncertain. The objective was to describe incidence, temporal trends and outcome of aortic dissection with particular emphasis on sex differences.
Methods and results
During the study period 2002–2016, 8057 patients in Sweden were diagnosed with aortic dissection, identified from the National Patient Register and the Cause of Death Register. A total of 5757 (71%) patients were hospitalized, whereas 2300 (29%) patients were deceased without concurrent hospital stay. The annual incidence was 7.2 per 100 000 (9.1 in men and 5.4 in women), decreasing over time in men (P = 0.005). Mean age in the hospitalized patients was 68 years (SD 13), 2080 (36%) were women. Within the first 14 days after onset, 1807 patients (32%) underwent surgical repair. The proportion of surgically treated increased from the 5-year period 2002–2006 to 2012–2016 [27% vs. 35%, odds ratio (OR) 1.61, 95% confidence interval (CI) 1.39–1.86; P < 0.001]. In hospitalized patients, 30-day mortality decreased between the same periods (26% vs. 21%, OR 0.68, 95% CI 0.59–0.80; P < 0.001). Long-term mortality decreased as well (hazard ratio 0.74, 95% CI 0.67–0.82; P < 0.001). Women had higher 30-day mortality than men after acute repair, a sex difference that remained after age adjustment (17% vs. 12%, OR 1.38, 95% CI 1.04–1.82; P = 0.006).
Conclusion
This population-based study detected a higher incidence of aortic dissection than prior reports, but a decreasing incidence in men. Surgical therapy was increasingly used and with more favourable outcome but was less frequently offered to elderly patients. The sustained sex differences regarding both incidence and outcome require further attention.
Keywords: Aortic dissection, Population-based, Sex differences, Mortality, Treatment, Endovascular
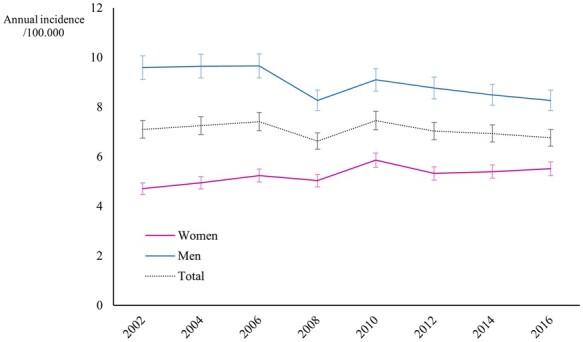
Graphical Abstract
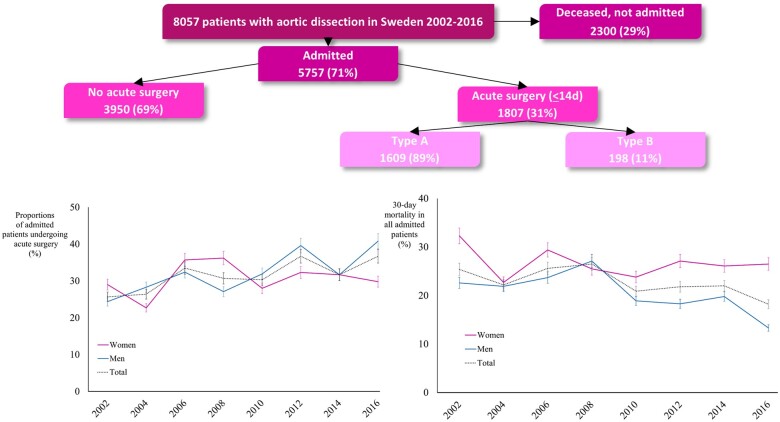
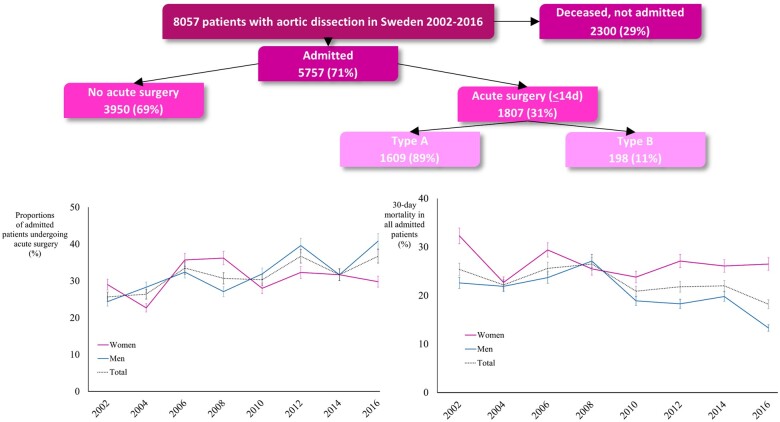
Graphical Abstract.
See page 2439 for the editorial comment on this article (doi: 10.1093/eurheartj/ehaa466)
Introduction
Acute aortic dissection is a potentially lethal condition. Many patients require emergency surgery but even with operative management, mortality is high. As stated in the European Society of Cardiology (ESC) guidelines, data on aortic dissection epidemiology are scarce and the true incidence is unknown.1 The incidence numbers presented in the ESC guidelines and the European Society for Vascular Surgery (ESVS) guidelines, respectively, were based on single population-based studies with an incidence of 3.5 per 100 000 per year in the Olmsted study and 6 per 100 000 per year in the Oxford vascular study, respectively.1–4 A national Swedish registry-based study found an increasing annual incidence of thoracic aortic disease (aneurysm and dissection) during the period 1987–2002.5 The ESC guidelines further emphasize the need for additional epidemiological studies on aortic dissection to analyse outcome in different treatment groups and to asses potential sex differences.1
Mortality in aortic dissection differs widely between subtypes and treatment groups, with the Stanford classification dividing aortic dissection patients into those with type A dissection (TAD) and type B dissection (TBD) being the most commonly used subdivision. A new classification of TBD was suggested very recently by the Society for Vascular Surgery and the Society of Thoracic Surgeons.6 In the above mentioned Swedish study, 30-day mortality in hospitalized patients with any acute aortic dissection was 37%.5 A recent report from the International Registry of Aortic Dissection (IRAD) demonstrated decreased in-hospital mortality in surgically treated patients with TAD from 25% to 18% during the years 1999 to 2014, whereas mortality in medically managed TAD patients remained at 56%.7 In patients with acute complicated TBD, IRAD reported in-hospital mortality of 11% in patients treated with thoracic endovascular aortic repair (TEVAR) vs. 34% in patients undergoing open surgical repair.7 , 8
The management of women with aortic disease is mostly based on evidence from studies including only or mainly men. According to previous studies, women with aortic dissection are older than men at presentation.2 , 9–12 The IRAD consortium stated that women diagnosed with aortic dissection present to the hospital later, have worse clinical status at presentation and have higher surgical and total mortality.9 Likewise, the Oxford vascular study demonstrated higher 30-day and 5-year mortality in women compared to men.2
The aim of the study was to describe the incidence of aortic dissection in the general population and to describe temporal trends and outcome of different treatment strategies, with particular emphasis on sex differences.
Materials and methods
National registers
All Swedish inhabitants are assigned a unique 12-digit personal registration number based on date of birth adding a 4-digit control number. Through this number, all individuals are identifiable in all medical registers maintained by the Swedish Board of Health and Welfare. The National Patient Register (NPR) holds individual data for each hospitalization and visits to specialist outpatient clinics including diagnostic codes from the International Classification of Disease (ICD-10) and procedures according to the Nomesco Classification of Surgical Procedures (NCSP) as well as date of admission. The Cause of Death Register (CDR) holds data on all individuals that die in Sweden, both in and outside of hospital care, including autopsy information. Reporting the main cause of death (ICD-10) to the CDR is mandatory by Swedish law. Statistics Sweden holds demographic data on the Swedish population including the total population each year.
Study design and population
This was a retrospective population-based register study. Data on all individuals diagnosed with aortic dissection (ICD-10 code I71.0) in the NPR or in the CDR during a 17-year period (2000–2016) were extracted. The date of the first-time diagnosis of aortic dissection was defined as the index event. All registered data on relevant concomitant diseases for all patients with dissection were extracted from the NPR 2 years prior to the index event in addition to all diagnoses at discharge including any diagnoses up to 90 days after the index event. Operations for aortic dissection were extracted from NPR based on specific NCSP codes. Patients under the age of 18 were excluded. As patients with aortic dissection have a relatively high degree of readmission following the acute index event and since the aim of our study was to include only new cases, we excluded patients diagnosed during 2000–2001, thereby securing that patients included in 2002–2016 had not been diagnosed with dissection prior to the index event. Thus, the study period was 15 years (2002–2016). The extracted dataset from the national registers was delivered on a patient-specific level but anonymized. Therefore, medical and surgical notes, imaging studies or autopsy reports could not be retrieved for included patients.
Surgically treated patients were divided into TAD and TBD based on typical treatment differences. Type A dissection is most commonly treated with open surgical repair of the ascending aorta. Thus, patients undergoing resection and graft replacement of the ascending aorta were categorized as TAD. In case of need of intervention, TBD is most commonly managed through TEVAR or open surgical repair of the descending aorta. Since medical notes and imaging studies could not be retrieved, the type of dissection could not be assessed in medically managed patients.
Surgery within 14 days was defined as acute and any later surgery was defined as delayed. In patients with TBD, surgery from Day 15 to Day 90 was defined as subacute. Dates of death were registered from the CDR. Last follow-up was 31 December 2016. Minimum follow-up was 30 days.
The STROBE statement was used in the preparation of the manuscript.13 The data underlying this article will be shared on reasonable request to the corresponding author. Ethical approval was obtained from the Regional Board of Ethical Approval in Stockholm, DNR 2014/957-31 and DNR 2017/127-32.
Statistical analysis
Continuous variables are presented as means with standard deviation (SD). Annual incidence was calculated as proportions of the total adult population of Sweden and presented as individuals per 100 000. Incidence trends were analysed through binary logistic regression model with aggregated data. The study period was divided into three 5-year time periods, 2002–2006, 2007–2011, and 2012–2016, and the patients were categorized in five different age groups, 18–49, 50–59, 60–69, 70–79, and 80–99 years old. Factors associated with acute surgery or TEVAR, and 30-day mortality were analysed with multiple logistic regression models adjusting for time period, sex, age, and comorbidity. For time trend analyses, the latter two 5-year time periods were compared with the first period. For age analyses, the latter four groups were compared to the first age group. Sex differences and time trends in long-term survival were analysed using Cox regression models adjusting for index year, sex, age, and comorbidity. Results are presented with odds ratios (ORs) for multiple logistic regression models and hazard ratios (HRs) for Cox regression models, respectively, with 95% confidence intervals (CIs). P-values below 0.05 were considered statistically significant. Statistical analysis was done using the Statistical Package for the Social Science (SPSS) 25.0 for Windows.
Results
Patient characteristics and general management
Overall, 8057 individuals with the diagnosis of aortic dissection were identified and included in the study. Of these individuals, 5757 (71%) had been hospitalized, whereas 2300 (29%) were deceased without concurrent hospital stay, only identified through the CDR and with an autopsy frequency of 76% (Figure 1, Take home figure). In total, 3035 (38%) were women. The proportions of women were higher among patients deceased without hospital admission than in hospitalized patients (42% vs. 36%, P = 0.001) (Supplementary material online, Table S1). Mean age in admitted patients was 68 years (SD 13). The admitted women were older than the men (71 vs. 66 years, P < 0.001). Mean age increased from 67 years in the first 5-year time period to 69 years in the last time period. In women mean age increased from 70 to 72 years, whereas it remained unchanged at 66 years in men. Age distributions in men and women of each 5-year time period are presented in Supplementary material online, Table S2. The occurrence of comorbid conditions diagnosed prior to the diagnosis of dissection was lower than after discharge from hospital. For example, at discharge 747 patients (36%) had the diagnosis of hypertension (ICD-10 code I10.9), whereas this was the case in only 126 patients (2%) prior to the onset of dissection (Table 1). At discharge, men were more frequently diagnosed with hypertension and kidney failure than women (Table 1). The majority (n = 3950, 69%) of the patients admitted with aortic dissection did not undergo surgical repair during the initial hospitalization. A total of 1807 (31%) patients underwent open or endovascular repair within 14 days (Figure 1). Acute surgically treated patients were younger than medically managed patients, mean age 62 vs. 70 years, P < 0.001. The 2300 individuals who were deceased but not hospitalized were older, had more comorbidity and a larger proportion were women (Supplementary material online, Table S1).
Take home figure.
This large population-based register study of over 8000 patients with aortic dissection demonstrates a higher incidence than earlier described, an increase in surgical management and improved outcome.
Figure 1.
Overview of all adult individuals with aortic dissection in Sweden 2002–2016 divided into different groups. Individuals identified from the Cause of Death Register are defined as deceased, not admitted. Aortic surgery is defined as acute the first 14 days and delayed after 14 days. Surgically treated patients are further divided into type A and type B dissections. Surgery for type B dissection is divided into open surgery and thoracic endovascular aortic repair.
Table 1.
Prevalence of concomitant disorders in all the 5757 patients, and separately in men (n = 3677) and in women (n = 2080), admitted with aortic dissection in Sweden 2002–2016 prior to the first event and within 90 days from the index event
| Prior to index event |
At discharge or within 90 days from index event |
|||||||
|---|---|---|---|---|---|---|---|---|
| Total, N (%) | Women, N (%) | Men, N (%) | P-value | Total, N (%) | Women, N (%) | Men, N (%) | P-value | |
| Hypertension | 126 (2%) | 38 (2%) | 88 (2%) | 0.158 | 2184 (38%) | 747 (36%) | 1437 (39%) | 0.017 |
| Ischaemic heart disease | 24 (0.4%) | 10 (1%) | 14 (0%) | 0.572 | 207 (4%) | 74 (4%) | 133 (4%) | 0.907 |
| Heart failure | 27 (1%) | 7 (0%) | 20 (1%) | 0.269 | 246 (4%) | 87 (4%) | 159 (4%) | 0.799 |
| Atrial fibrillation | 44 (1%) | 15 (1%) | 29 (1%) | 0.777 | 766 (13%) | 272 (13%) | 494 (13%) | 0.701 |
| Any heart disease | 146 (3%) | 46 (2%) | 100 (3%) | 0.239 | 2604 (46%) | 888 (43%) | 1726 (47%) | 0.004 |
| Stroke/TIA | 9 (0.2%) | 2 (0%) | 7 (0%) | 0.385 | 367 (6%) | 121 (6%) | 246 (7%) | 0.193 |
| Kidney failure | 12 (0.2%) | 2 (0%) | 10 (0%) | 0.160 | 284 (5%) | 79 (4%) | 205 (6%) | 0.003 |
| Diabetes | 19 (0.3%) | 19 (0%) | 1 (0%) | 0.005 | 194 (3%) | 64 (3%) | 130 (4%) | 0.354 |
Concomitant disorders in all hospitalized patients with aortic dissection in Sweden prior to admission as well as at discharge combined with data from within 90 days from the admission date. Proportions are described for men and women separately and compared with the χ2 test, presented with P-value.
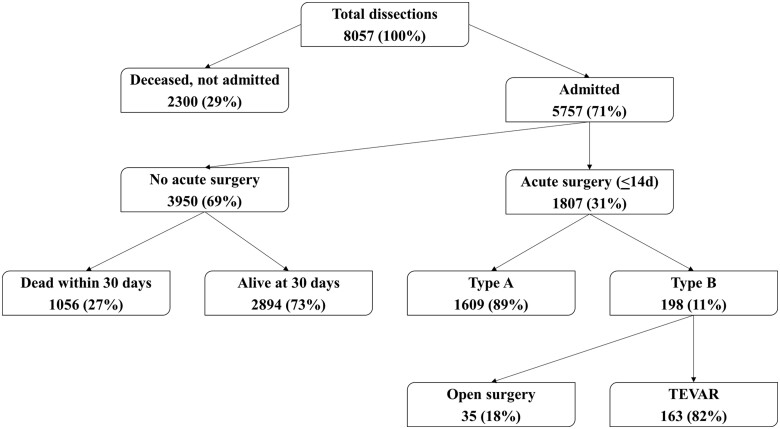
Incidence
The number of diagnosed individuals was 497 in 2002 and 535 in 2016. During the same period, the Swedish population grew from 8.9 to 10.0 million people. The mean annual incidence was 7.2/100 000. The incidence was higher in men than in women (9.1 per 100 000 vs. 5.4 per 100 000, P < 0.001). The mean annual incidence in men was 9.8 in the first 5-year time period and 8.8 in the last time period. Trend analysis showed a decreased in the incidence in men over time (P = 0.005), whereas no change was seen in women (P = 0.105) (Figure 2).
Figure 2.
Incidence of aortic dissection in the adult population of Sweden (men and women) 2002–2016. 95% confidential intervals for each year are presented.
Surgical management
The majority of surgically managed patients were treated in the acute phase, 87% (n = 1807/2067). Most patients undergoing acute repair had TAD, n = 1609 (89%). Few TBD patients were treated by means of surgical or endovascular repair in the acute phase, n = 198 (Table 2). The majority underwent TEVAR, n = 163 (82%), 22 (11%) open surgical repair of the descending aorta and 13 (7%) open thoracoabdominal surgical repair.
Table 2.
Acute and delayed surgical management, in total and in three different 5-year time periods
| Surgical management | Total (n = 5757) | 2002–2006 (n = 1767) | 2007–2011 (n = 1917) | 2012–2016 (n = 2073) | P-value |
|---|---|---|---|---|---|
| Acute aortic surgery | 1807 (31%) | 478 (27%) | 603 (31%) | 726 (35%) | <0.001 |
| Type A—acute surgery | 1609 (28%) | 438 (25%) | 544 (28%) | 627 (30%) | 0.001 |
| Type B—acute surgery | 198 (3%) | 40 (2%) | 59 (3%) | 99 (5%) | <0.001 |
| Delayed aortic surgery | 260 (5%) | 93 (5%) | 83 (4%) | 84 (4%) | 0.176 |
| Type A—delayed surgery | 100 (2%) | 27 (2%) | 28 (2%) | 45 (2%) | 0.116 |
| Type B—delayed surgery | 160 (3%) | 66 (4%) | 55 (3%) | 39 (2%) | 0.002 |
Proportions of hospitalized patients that were treated with surgery during the three 5-year time periods. Acute is defined as surgery within 14 days from admission and any later surgery is defined as delayed. The proportion of patients with type B dissection treated with endovascular repair was 82% for acute surgery and 76% for delayed surgery. P-values refer to differences between the time groups, trends, analysed with the χ2 test.
The proportion receiving an acute procedure increased during the study period (27% in 2002–2006 vs. 35% in 2012–2016, OR 1.61, 95% CI 1.39–1.86; P < 0.001) (Table 3, Figure 3, Take home figure). An increase was seen in acute TEVAR for TBD as well (Table 3). Fewer women were treated with acute TEVAR for TBD compared to men (2% vs. 3%, OR 0.69, 95% CI 0.49–0.99; P = 0.006) (Table 3). The mean age in acute surgically treated patients increased from 62 years in the first time period to 64 in the last period. The sex-specific increase was 60–63 years in men and 65–67 years in women.
Table 3.
Chance of being subjected to operative management, defined as any acute aortic surgery (A) and TEVAR (B), respectively, and the association to index year, sex, and age in all hospitalized patients (n = 5757)
| A | Mean age (SD) | Crude results (n = 1807) | Adjusted results OR (CI 95%) |
|---|---|---|---|
| Men (n = 3677) | 61 (12) | 1195 (33%) | 1 |
| Women (n = 2080) | 65 (11) | 612 (29%) | 1.09 (0.96–1.23) |
| 5-year time groups | |||
| 2002–2006 | 62 (12) | 478 (27%) | 1 |
| 2007–2011 | 62 (12) | 603 (31%) | 1.31 (1.13–1.52) |
| 2012–2016 | 64 (12) | 726 (35%) | 1.61 (1.40–1.87) |
| Age categories | |||
| 18–49 (n = 511) | 246 (48%) | 1 | |
| 50–59 (n = 922) | 409 (44%) | 0.87 (0.70–1.08) | |
| 60–69 (n = 1541) | 594 (39%) | 0.67 (0.55–0.82) | |
| 70–79 (n = 1650) | 481 (29%) | 0.43 (0.35–0.53) | |
| 80–99 (n = 1133) | 77 (9%) | 0.08 (0.06–0.10) | |
|
| |||
| B | Mean age (SD) | Crude results (n = 163) | Adjusted results OR (CI 95%) |
|
| |||
| Men (n = 3677) | 65 (11) | 118 (3%) | 1 |
| Women (n = 2080) | 67 (14) | 45 (2%) | 0.69 (0.48–0.98) |
| 5-year time groups | |||
| 2002–2006 | 65 (14) | 25 (1%) | 1 |
| 2007–2011 | 64 (11) | 53 (3%) | 2.11 (1.31–3.43) |
| 2012–2016 | 67 (12) | 85 (4%) | 3.08 (1.96–4.85) |
| Age categories | |||
| 18–49 (n = 511) | 14 (3%) | 1 | |
| 50–59 (n = 922) | 36 (4%) | 1.51 (0.81–2.85) | |
| 60–69 (n = 1541) | 45 (3%) | 1.06 (0.57–1.95) | |
| 70–79 (n = 1650) | 51 (3%) | 1.15 (0.63–2.12) | |
| 80–99 (n = 1133) | 17 (2%) | 0.69 (0.48–0.98) | |
The association between index year, sex, and age, respectively, and acute surgical management analysed with multiple logistic regression models. Index year was divided into three 5-year time periods, comparing the latter two periods to the first (reference). The patients were divided into five different age strata analysing the first age category as reference. Mean age is shown for men and women as well as mean patient age of each time period. Models are adjusted for index year, sex, and age, respectively, as well as for concomitant disorders.
Figure 3.
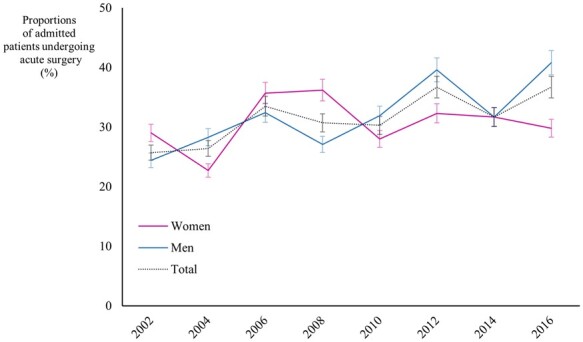
Proportions of admitted patients with aortic dissection treated with acute surgery of the aorta per year in total, in men and in women. 95% confidential intervals for each year are presented.
Out of the 2894 medically managed patients alive at 30 days, 160 patients with TBD were treated with TEVAR or open surgical repair during follow-up. Out of these patients, 32 (20%) were treated in the subacute phase and 128 (80%) in the chronic phase. One hundred patients with TAD were treated with open surgical repair after the acute phase.
Short-term mortality
Overall 30-day mortality in admitted patients was 23% (n = 1307/5757), 26% in women and 21% in men (P < 0.001) (Table 4). During the first period, 30-day mortality was 25%, it decreased to 21% in the last 5-year period (P < 0.001) (Table 4, Figure 4, Take home figure). Out of the medically managed patients, 27% (n = 1056/3950) died within 30 days. Mean time to death in these individuals was 2 days (SD 4).
Table 4.
Short-term mortality and association with index year, sex, and age
| All admitted (n = 5757) |
Acute surgically treated (n = 1807) |
|||||
|---|---|---|---|---|---|---|
| Age, mean (SD) | 30-day mortality | Adjusted OR (95% CI) | Age, mean (SD) | 30-day mortality | Adjusted OR (95% CI) | |
| Men | 66 (13) | 759 (21%) | 1 | 61 (12) | 144 (12%) | 1 |
| Women | 71 (12) | 548 (26%) | 1.11 (0.97–1.27) | 65 (11) | 111 (17%) | 1.38 (1.04–1.82) |
| 5-year time groups | ||||||
| 2002–2006 | 67 (13) | 455 (26%) | 1 | 62 (12) | 81 (17%) | 1 |
| 2007–2011 | 68 (13) | 426 (22%) | 0.78 (0.67–0.91) | 62 (12) | 80 (13%) | 0.74 (0.52–1.03) |
| 2012–2016 | 69 (13) | 426 (21%) | 0.68 (0.59–0.80) | 64 (12) | 89 (12%) | 0.64 (0.46–0.88) |
| Age categories | ||||||
| 18–49 | 62 (12%) | 1 | 25 (10%) | 1 | ||
| 50–59 | 119 (13%) | 1.06 (0.76–1.47) | 43 (11%) | 1.00 (0.59–1.69) | ||
| 60–69 | 240 (16%) | 1.34 (0.99–1.81) | 75 (13%) | 1.22 (0.75–1.97) | ||
| 70–79 | 404 (25%) | 2.31 (1.73–3.09) | 85 (18%) | 1.84 (1.13–2.97) | ||
| 80–99 | 482 (43%) | 5.34 (3.98–7.16) | 22 (29%) | 3.33 (1.73–6.41) | ||
Multiple logistic regression models analysing 30-day mortality and the association between index year, sex, and age for all admitted patients and in acute surgically treated, respectively. The 15-year study period was divided into three 5-year time groups where the latter two time groups were compared with the first time group. Patients were divided into five different age groups and the latter four were compared to the first age group. Mean age is presented for each time period and for men and women, respectively. Models are adjusted for index year, sex, and age, respectively as well as for concomitant disorders.
Figure 4.
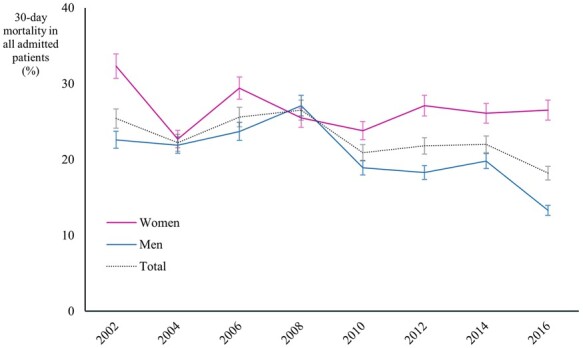
Thirty-day mortality in patients admitted with aortic dissection presented in total, in men and in women. 95% confidential intervals for each year are presented.
In acute surgically treated patients, 30-day mortality was 14% (n = 250/1807), decreasing from the first to the last 5-year period (Table 4). Female sex was associated with higher 30-day mortality after acute repair (Table 4). In patients with TAD treated with acute surgery, 30-day mortality was 14% (n = 231/1609). In individuals with TBD, 30-day mortality after acute TEVAR was 10% (n = 17/163) and after acute open surgical repair 6% (n = 2/35). Including out of hospital deaths, 30-day mortality in the entire cohort was 46% (n = 3657/8057).
Long-term survival
In all hospitalized patients, 1-year mortality was 27% (n = 1575/5757), 17% in acute surgically treated TAD (n = 278/1609), and 14% in acute surgically treated TBD (n = 27/198). Overall, 5-year survival was 63% (n = 3629/5757), mean follow-up was 38 months. Long-term mortality decreased during the study period, HR 0.74 (95% CI 0.67–0.82; P < 0.001). Female sex was not associated with higher long-term mortality, HR 1.002 (95% CI 0.925–1.084; P = 0.982).
Discussion
This nationwide population-based study of more than 8000 patients with aortic dissection, demonstrated a higher incidence than previously described, an increase in acute operative management and, in addition, improved survival. Some apparent sex differences were identified such as unchanged incidence in women compared to a decrease in men, a lower proportion of women admitted, fewer TEVAR-treated and a higher postoperative mortality in women.
To our knowledge, this is one of the largest population-based studies of aortic dissection to date and one of only a few modern studies focusing on sex differences. Population-based studies are likely to reflect the reality more accurately than hospital-based studies or randomized controlled trials, since also non-admitted patients dying outside of hospital are included. Hospital-based studies, such as analyses from IRAD, suffer from potential selection bias, often including a core of healthier subjects with lower morbidity and mortality, which may decrease the generalizability of the findings to larger populations.
The age and sex distribution of the identified cases were comparable to other population-based aortic dissection cohorts with mean age between 66 and 72 years and the proportions of women ranging from 36% to 40% (Table 5).2 , 4 , 14 , 15 However, compared to single- and multicentre studies and investigations on surgically treated patients alone, the population in our study was older, with mean age of 68 years compared to 63 years in IRAD and 58 years in the STABLE study (Table 5).7 , 8 , 16 , 17 Women were 5 years older than men at presentation, a finding coherent with other reports.2 , 9–12 Notably, a higher proportion of the patients deceased without concomitant hospital stay were women compared to hospitalized patients. The same difference was reported for TAD patients in the Oxford Vascular Study where the proportion of women in out-of-hospital deaths was even higher.2 The higher mean age in women may contribute to such a sex difference, but a bias in referral patterns and clinicians failing to treat women per protocol has been reported to remain even after adjustment for age and comorbidity in other patient groups such as with chest pain and patients with abdominal aortic aneurysms.18 , 19 A recent meta-analysis of sex-specific differences in association with repair of descending thoracic aortic aneurysms identified higher 30-day mortality in women, a finding unrelated to age.20 Any possible biological sex differences in eligibility for repair of the thoracic aorta and the reason behind the sex-specific mortality differences remain to be identified.
Table 5.
Presentation of contemporary reports on aortic dissection including epidemiological studies and studies focusing on sex differences
| Reference | Study design | Number of patients | Mean age | Percentage of women | Incidence per 100 000 |
|---|---|---|---|---|---|
| Howard et al., 20132 | Population based | 155 | 72 | 40% | 6.0 |
| Clouse et al., 20044 | Population based | 39 | 67 | 36% | 3.5 |
| McClure et al., 201814 | Population based | 5966 | 66 | 39% | 4.6 |
| Melvinsdottir et al., 201615 | Population based | 153 | 67 | 39% | 2.5 |
| Nienaber et al., 20049 | IRAD | 1078 | 62 | 32% | — |
| Sex differences | |||||
| Conway et al., 201510 | Multicentre | 251 | 67 | 31% | — |
| Sex differences | |||||
| Liang et al., 201711 | Population based | 9855 | 66 | 43% | — |
| Sex differences | |||||
| Maitusong et al., 201612 | Multicentre | 400 | 51 | 24% | — |
| Sex differences | |||||
| Pape et al., 201517 | IRAD | 4428 | 63 | 37% | — |
| Lombardi et al., 201216 | STABLE | 40 | 58 | 30% | — |
| Smedberg et al., (present study) | Population based | 8057 | 68 | 36% | 7.2 |
Important studies on aortic dissection including number of patients as well as sex- and age distribution. In epidemiological studies, incidence is presented.
The frequency of previously documented comorbid conditions prior to onset of dissection was unexpectedly low in contrast to the more prevalent disease distribution found at or after discharge. Moreover, it has been reported that diagnoses other than the main diagnosis are more poorly documented in the NPR.21 Most importantly, after the index event the patients have a vast increase of registered comorbid conditions, which would have been missed if only the diagnosis codes on admission had been included.
The true incidence of aortic dissection has been hard to determine due to lack of large population-based studies, which was addressed in the ESC guidelines as a gap in evidence.1 The incidence reported in guidelines and earlier population-based studies span from 2.5 to 6 per 100 000 per year (Table 5).1–4 , 14 , 15 In the Oxford Vascular Study, the incidence of aortic dissection was 6 per 100 000 per year, a study identifying 155 cases (admitted and out-of-hospital deaths) in a population-based setting in a county with 93 000 inhabitants. In the present study, the incidence of aortic dissection was found to be 7.2 per 100 000 per year in Sweden with a population of 10 million. The inclusion of out-of-hospital deaths, combined with the high autopsy rate among individuals dying outside of hospital markedly strengthens the findings. This implies that the true incidence of aortic dissection is higher than indicated in a number of previous reports. Actually, since 29% of diagnosed patients were not admitted, only reporting the incidence of hospitalized patients would introduce a serious underestimation of the incidence. From the high autopsy frequency, 76%, compared to the general Swedish autopsy frequency of 11% (www.socialstyrelsen.se; 2016), the validity of the dissection diagnoses in the 2300 out-of-hospital deaths can be considered to be very high. The Swedish law on autopsy do not mandate autopsy other than when a forensic autopsy is indicated and there are no specific regulations regarding out of hospital deaths. In a recent German study, an annual incidence of TAD as high as 11.9 per 100 000 was reported.22 However, that figure was an estimation based on exploration rather than a true finding.22 An increase in the incidence of aortic dissection and aneurysm was presented in a population-based study from Ontario, Canada, during the period 2002–2014.14 Conversely, the present dataset rather confirms an unchanged incidence in women and a decrease in the incidence in men. In a study from Iceland, no change in the incidence was reported during 1992–2013.15 The general development of incidence rates in other cardiovascular disease groups is similar. The ESC recently published cardiovascular disease statistics from 2019 reporting a decrease in the incidence of coronary heart disease and stroke as well as a decrease in cardiovascular risk factors such as hypertension and smoking.23 , 24 Statistics on aortic dissection is not included in the report.24 Survival in coronary heart disease and stroke in men is improving, but a less pronounced improvement is seen in women.25 , 26
In contrast to the incidence rates, the proportions of surgically treated patients increased markedly during the study period. An increase in acute operative management was also shown in IRAD.17 It could have been suspected that the wide introduction of TEVAR would have contributed greatly to the increase, but actually, the increase was mainly due to a rise in acute open surgical repair for TAD shown both in actual numbers and as proportions treated in the population. Older age was associated with a decreased chance of getting aortic surgery, whereas sex did not influence the chance of surgical management other than the chance for TEVAR in TBD.
The outcome in patients with aortic dissection is improving. Thirty-day mortality in admitted patients was 23% in our study compared to 37% in Sweden 1987–2002.5 This improvement continued during our study, both overall and in surgically treated individuals, which is coherent with other modern epidemiological studies.7 , 14 , 15 In crude numbers, among all admitted patients, women had higher 30-day mortality. Women also had higher 30-day mortality than men among acute surgically treated patients. Age-adjusted analysis revealed that female sex per se was associated with increased 30-day mortality after acute surgical procedures, whereas such an association did not exist in the whole group of admitted patients. Our results are consistent with results presented in the Oxford vascular study and by the IRAD-group, but differs from modern, albeit small, studies on patients with TBD and surgically managed patients with TAD where no sex differences in mortality were seen.2 , 9–12 Postoperative mortality after TEVAR for descending thoracic aortic aneurysm has been reported to be higher in women.20 The same review conclude that the reason for the sex differences in mortality is unknown but speculates that sex differences in aortic morphology and hidden coronary heart disease in women are possible reasons.20 Another possible explanation to the sex differences in mortality could be that clinicians fail to adhere to guidelines when treating women, as reported for coronary heart disease and abdominal aortic aneurysms.18 , 19 Our results show higher 30-day mortality in medically managed patients compared to acute surgically treated patients (27% vs. 14%). It is plausible that the group of medically managed patients dying within 30 days mostly included patients with TAD that had been denied surgical repair.2 , 14 , 15 , 27 , 28 Not surprisingly, older age was associated with increased 30-day mortality. Interestingly, no difference was seen in the three youngest age groups, whereas patients over 70 years had markedly higher mortality, both overall and in surgically treated patients alone.
This study is limited by its register-based design as well as the flawed ICD coding of dissection, not separating TAD and TBD. The distinction of surgically treated TAD and TBD can be made by applying the treatment codes, but medically managed can only with caution and interpretation of common clinical care be divided into TAD and TBD. By excluding patients diagnosed with aortic dissection during the 2 years preceding the study period the risk of including patients with already diagnosed dissection should have been minimized, albeit that some patients could have had a diagnosed hospital episode more than two years prior to 2000, which would then be misclassified as ‘new dissection’ rather than progression of disease. A large validating study in 2011 concluded that the validity of the NPR for cardiac diagnoses was over 90% and for cardiac surgery, 98% but no validating study for aortic dissection has been conducted.21 The majority of comorbid conditions, such as hyperlipidaemia and hypertension, are managed by general practitioners, whose diagnostic coding is not included in the NPR. This introduces an underestimation of comorbid conditions prior to hospital or specialist outpatient care, which was clearly shown in our results.
The strengths of the study are the population-based nature and the inclusion of a large number of patients over many years. Patient inclusion not limited to hospitalized individuals but also taking into account those deceased from aortic dissection without hospitalization should be of great importance in describing the true incidence of aortic dissection. An autopsy frequency in not admitted patients of 75% in our study confirms the reliability of diagnoses in this group. Reporting to the NPR and the CDR is mandatory and the possibility to cross-link these registers are limited to few countries. Given that, these registers are good for describing incidence and trends in treatment and mortality.
In summary, the present population-based study detected a higher incidence of aortic dissection than prior reports, but a decrease in the incidence in men over time. The trend, including an increasing volume of surgically treated patients and with more favourable outcome, mirrors the tendencies found in other cardiovascular diseases with increasing treatment rates and improved survival. The lower chance for elderly patients to be subjected to surgical treatment also mimics what has been described for other patient groups. The findings imply that one can foresee an increasing number of patients admitted for open and endovascular repair, considering the improving results also in elderly, even though the incidence is not increasing. The sustained sex differences identified also in this cardiovascular patient group regarding both incidence and outcome require further attention in future studies.
Supplementary Material
Acknowledgements
We thank Max Vikström, statistician at the Institute of Environmental medicine, Karolinska Institutet, and Mikael Andersson-Franko, statistician at the Department of Clinical Science and Education, Karolinska Institutet, Södersjukhuset, for their statistical aid.
Funding
Researchers conducting the study were supported with financial aid from the Department of Clinical Science and Education, Karolinska Institutet, Södersjukhuset, the Department of Surgery, Södersjukhuset, as well as from the Swedish Heart-Lung Foundation (Hultgren 20180506).
Conflict of interest: none declared.
Contributor Information
Christian Smedberg, Department of Clinical Science and Education, Karolinska Institutet, Södersjukhuset, Sjukhusbacken 10, SE-11883 Stockholm, Sweden; Department of Surgery, Södersjukhuset, Sjukhusbacken 10, SE-11883 Stockholm, Sweden.
Johnny Steuer, Department of Clinical Science and Education, Karolinska Institutet, Södersjukhuset, Sjukhusbacken 10, SE-11883 Stockholm, Sweden; Department of Surgery, Södersjukhuset, Sjukhusbacken 10, SE-11883 Stockholm, Sweden.
Karin Leander, Institute of Environmental Medicine, Karolinska Institutet, Box 210, SE-17177 Stockholm, Sweden.
Rebecka Hultgren, Department of Molecular Medicine and Surgery, Karolinska Institutet, Stockholm S301 SE-17176, Sweden; Department of Vascular Surgery, Karolinska University Hospital, Stockholm S301 SE-17176, Sweden.
References
- 1. Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwoger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ; ESC Committee for Practice Guidelines. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2015;36:2779–2926. [DOI] [PubMed] [Google Scholar]
- 2. Howard DP, Banerjee A, Fairhead JF, Perkins J, Silver LE, Rothwell PM. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford Vascular Study. Circulation 2013;127:2031–2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Riambau V, Bockler D, Brunkwall J, Cao P, Chiesa R, Coppi G, Czerny M, Fraedrich G, Haulon S, Jacobs MJ, Lachat ML, Moll FL, Setacci C, Taylor PR, Thompson M, Trimarchi S, Verhagen HJ, Verhoeven ELESVS Guidelines CommitteeKolh P, de Borst GJ, Chakfe N, Debus ES, Hinchliffe RJ, Kakkos S, Koncar I, Lindholt JS, Vega de Ceniga M, Vermassen F, Verzini F, Document R, Kolh P, Black JH 3rd, Busund R, Bjorck M, Dake M, Dick F, Eggebrecht H, Evangelista A, Grabenwoger M, Milner R, Naylor AR, Ricco JB, Rousseau H, Schmidli J. Editor’s Choice—management of descending thoracic aorta diseases: clinical practice guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 2017;53:4–52. [DOI] [PubMed] [Google Scholar]
- 4. Clouse WD, Hallett JW Jr, Schaff HV, Spittell PC, Rowland CM, Ilstrup DM, Melton LJ 3rd. Acute aortic dissection: population-based incidence compared with degenerative aortic aneurysm rupture. Mayo Clin Proc 2004;79:176–180. [DOI] [PubMed] [Google Scholar]
- 5. Olsson C, Thelin S, StaåHle E, Ekbom A, Granath F. Thoracic aortic aneurysm and dissection: increasing prevalence and improved outcomes reported in a nationwide population-based study of more than 14,000 cases from. Circulation 2006;114:2611–2618. [DOI] [PubMed] [Google Scholar]
- 6. Lombardi JV, Hughes GC, Appoo JJ, Bavaria JE, Beck AW, Cambria RP, Charlton-Ouw K, Eslami MH, Kim KM, Leshnower BG, Maldonado T, Reece TB, Wang GJ. Society for Vascular Surgery (SVS) and Society of Thoracic Surgeons (STS) reporting standards for type B aortic dissections. J Vasc Surg 2020;71:723–747. [DOI] [PubMed] [Google Scholar]
- 7. Evangelista A, Isselbacher EM, Bossone E, Gleason TG, Eusanio MD, Sechtem U, Ehrlich MP, Trimarchi S, Braverman AC, Myrmel T, Harris KM, Hutchinson S, O’Gara P, Suzuki T, Nienaber CA, Eagle KA. Insights from the International Registry of Acute Aortic Dissection: a 20-year experience of collaborative clinical research. Circulation 2018;137:1846–1860. [DOI] [PubMed] [Google Scholar]
- 8. Tsai TT, Trimarchi S, Nienaber CA. Acute aortic dissection: perspectives from the International Registry of Acute Aortic Dissection (IRAD). Eur J Vasc Endovasc Surg 2009;37:149–159. [DOI] [PubMed] [Google Scholar]
- 9. Nienaber CA, Fattori R, Mehta RH, Richartz BM, Evangelista A, Petzsch M, Cooper JV, Januzzi JL, Ince H, Sechtem U, Bossone E, Fang J, Smith DE, Isselbacher EM, Pape LA, Eagle KA. Gender-related differences in acute aortic dissection. Circulation 2004;109:3014–3021. [DOI] [PubMed] [Google Scholar]
- 10. Conway BD, Stamou SC, Kouchoukos NT, Lobdell KW, Hagberg RC. Effects of gender on outcomes and survival following repair of acute type A aortic dissection. Int J Angiol 2014;24: 93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liang NL, Genovese EA, Al-Khoury GE, Hager ES, Makaroun MS, Singh MJ. Effects of gender differences on short-term outcomes in patients with type B aortic dissection. Ann Vasc Surg 2017;38:78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Maitusong B, Sun HP, Xielifu D, Mahemuti M, Ma X, Liu F, Xie X, Azhati A, Zhou XR, Ma YT. Sex-related differences between patients with symptomatic acute aortic dissection. Medicine 2016;95:e3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453–1457. [DOI] [PubMed] [Google Scholar]
- 14. McClure RS, Brogly SB, Lajkosz K, Payne D, Hall SF, Johnson AP. Epidemiology and management of thoracic aortic dissections and thoracic aortic aneurysms in Ontario, Canada: a population-based study. J Thorac Cardiovasc Surg 2018;155:2254–2264.e4. [DOI] [PubMed] [Google Scholar]
- 15. Melvinsdottir IH, Lund SH, Agnarsson BA, Sigvaldason K, Gudbjartsson T, Geirsson A. The incidence and mortality of acute thoracic aortic dissection: results from a whole nation study. Eur J Cardiothorac Surg 2016;50:1111–1117. [DOI] [PubMed] [Google Scholar]
- 16. Lombardi JV, Cambria RP, Nienaber CA, Chiesa R, Teebken O, Lee A, Mossop P, Bharadwaj P. Prospective multicenter clinical trial (STABLE) on the endovascular treatment of complicated type B aortic dissection using a composite device design. J Vasc Surg 2012;55:629–640.e2. [DOI] [PubMed] [Google Scholar]
- 17. Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S, Evangelista A, Myrmel T, Larsen M, Harris KM, Greason K, Di Eusanio M, Bossone E, Montgomery DG, Eagle KA, Nienaber CA, Isselbacher EM, O'Gara P. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the international registry of acute aortic dissection. J Am Coll Cardiol 2015;66:350–358. [DOI] [PubMed] [Google Scholar]
- 18. Alabas OA, Gale CP, Hall M, Rutherford MJ, Szummer K, Lawesson SS, Alfredsson J, Lindahl B, Jernberg T. Sex differences in treatments, relative survival, and excess mortality following acute myocardial infarction: national cohort study using the SWEDEHEART registry. J Am Heart Assoc 2017;6:e007123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zommorodi S, Bottai M, Hultgren R. Sex differences in repair rates and outcomes of patients with ruptured abdominal aortic aneurysm. Br J Surg 2019;106:1480–1487. [DOI] [PubMed] [Google Scholar]
- 20. Ulug P, Powell JT, Warschkow R, von Allmen RS. Editor’s choice—sex specific differences in the management of descending thoracic aortic aneurysms: systematic review with meta-analysis. Eur J Vasc Endovasc Surg 2019;58:503–511. [DOI] [PubMed] [Google Scholar]
- 21. Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO. External review and validation of the Swedish national inpatient register. BMC Public Health 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kurz SD, Falk V, Kempfert J, Gieb M, Ruschinski TM, Kukucka M, Tsokos M, Grubitzsch H, Herbst H, Semmler J, Buschmann C. Insight into the incidence of acute aortic dissection in the German region of Berlin and Brandenburg. Int J Cardiol 2017;241:326–329. [DOI] [PubMed] [Google Scholar]
- 23. Dalen JE, Alpert JS, Goldberg RJ, Weinstein RS. The epidemic of the 20(th) century: coronary heart disease. Am J Med 2014;127:807–812. [DOI] [PubMed] [Google Scholar]
- 24. Timmis A, Townsend N, Gale CP, Torbica A, Lettino M, Petersen SE, Mossialos EA, Maggioni AP, Kazakiewicz D, May HT, De Smedt D, Flather M, Zuhlke L, Beltrame JF, Huculeci R, Tavazzi L, Hindricks G, Bax J, Casadei B, Achenbach S, Wright L, Vardas P; European Society of Cardiology. European Society of Cardiology: Cardiovascular Disease Statistics 2019. Eur Heart J 2020;41:12–85. [DOI] [PubMed] [Google Scholar]
- 25. Arciero TJ, Jacobsen SJ, Reeder GS, Frye RL, Weston SA, Killian JM, Roger VéL. Temporal trends in the incidence of coronary disease. Am J Med 2004;117:228–233. [DOI] [PubMed] [Google Scholar]
- 26. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation 2014;129:e28–e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chiappini B, Schepens M, Tan E, Amore AD, Morshuis W, Dossche K, Bergonzini M, Camurri N, Reggiani LB, Marinelli G, Bartolomeo RD. Early and late outcomes of acute type A aortic dissection: analysis of risk factors in 487 consecutive patients. Eur Heart J 2005;26:180–186. [DOI] [PubMed] [Google Scholar]
- 28. Trimarchi S, Nienaber CA, Rampoldi V, Myrmel T, Suzuki T, Mehta RH, Bossone E, Cooper JV, Smith DE, Menicanti L, Frigiola A, Oh JK, Deeb MG, Isselbacher EM, Eagle KA. Contemporary results of surgery in acute type A aortic dissection: the International Registry of Acute Aortic Dissection experience. J Thorac Cardiovasc Surg 2005;129:112–122. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.