Abstract
Diaphragm disease is a rare condition associated with the long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) and can lead to severe complications. Most strictures occur in the small bowel, and occurrence in the colon is rare. We report a case of an asymptomatic patient with colonic diaphragm disease secondary to NSAID use.
Keywords: Colonic diaphragm disease, nonsteroidal anti-inflammatory drugs, stricture
Diaphragm disease is a rare condition associated with the long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) and can lead to severe complications.1,2 Diaphragm-like strictures occur mostly in the small bowel and rarely in the colon. The most common occurrence in the colon is in the ascending colon.2 Patients with colonic diaphragm disease (CDD) can present with a wide array of symptoms and presentations, such as lower gastrointestinal bleeding, anemia, abdominal pain, constipation, and colonic obstruction/perforation.1 Although the adverse effects of NSAIDs on the upper gastrointestinal tract are well known, it is important to highlight NSAID-induced stricture formation in the colon from inflammation, ulceration, and formation of a diaphragm, which can cause obstruction.3,4 Due to the increased frequency of NSAID use in the general population, it is important to consider CDD as a possible diagnosis in such patients.
CASE REPORT
A 70-year-old black woman with a past medical history of gastroesophageal reflux disease, congestive heart failure, and osteoarthritis presented for a screening colonoscopy. She denied nausea, vomiting, abdominal pain, loss of appetite, constipation, diarrhea, melena, and hematochezia. She was taking omeprazole 40 mg daily, furosemide 40 mg daily, and naproxen 500 mg twice a day. She had been taking naproxen for the past 15 years. She had no symptoms or history suggestive of inflammatory bowel disease. Her past surgical, social, and family histories were unremarkable.
The patient’s body mass index was 21 kg/m2, and physical examination showed a soft abdomen with no distention or tenderness. Laboratory testing from 2 weeks prior revealed a hematocrit of 34.4% and a normal leukocyte count. A metabolic panel showed a potassium of 3.8 mEq/L; chloride, 93 mEq/L; bicarbonate, 29 mEq/L; blood urea nitrogen, 28 mg/dL; and creatinine, 1.1 mEq/L.
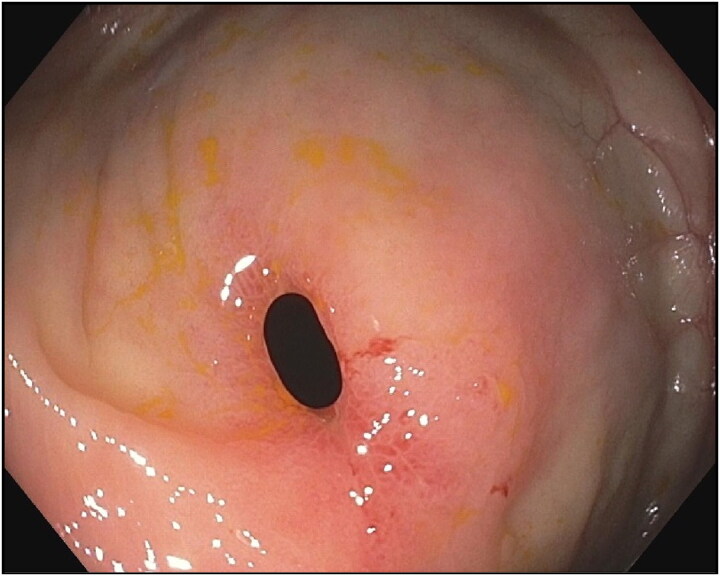
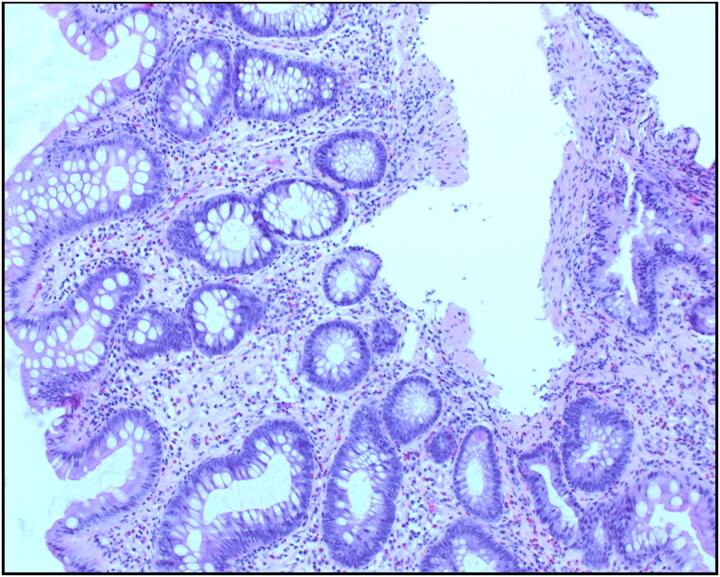
Colonoscopy to the proximal ascending colon was normal with no mucosal abnormality, but the cecum could not be reached as the lumen appeared to close off, posing difficulty to advance the endoscope. Further manipulation of the colonoscope revealed a tight stricture with fibrotic edges and mildly erythematous mucosa (Figure 1). The stricture could not be traversed with the adult colonoscope. Multiple biopsies were obtained from the stricture margins. Histology was negative for malignancy and showed chronic active colitis with focal surface erosion, inflamed granulation tissue, fibrosis of the lamina propria, and minimal architecture disarray (Figure 2).
Figure 1.
An endoscopic view of NSAID-induced colonic diaphragm showing tight stricture in the ascending colon with fibrotic edges and mildly erythematous mucosa. The stricture resulted in significant narrowing of the colonic mucosa.
Figure 2.
Biopsy showing chronic active colitis with focal surface erosion, inflamed granulation tissue, and fibrosis of the lamina propria.
Based on the typical histological features, a diagnosis of CDD secondary to naproxen, an NSAID, was made. Taking into consideration the patient’s age, lack of abdominal symptoms, and other medical comorbidities, the patient was managed conservatively with close monitoring. Naproxen was discontinued, and she was counseled to avoid all types of NSAIDs. She remained asymptomatic at 3-month follow-up.
DISCUSSION
In contrast to other well-known gastrointestinal side effects of NSAIDs, diaphragm disease is a rare complication, and only one-third of all such cases are found in the colon. It is reported that CDD has a higher incidence in the seventh decade of life and occurs predominantly in women.1 The most common presenting symptoms include anemia and mechanical obstruction. This contrasts with our patient, who was asymptomatic at presentation. The duration of NSAID use is an important factor in the formation of the diaphragm and varies widely in the literature—from 2 months to 25 years.2 Chronic NSAID use increases the likelihood of diaphragm formation, as was the case in our patient who had been taking NSAIDs for almost 15 years. Multiple NSAIDs have been implicated in causing CDD, with the most common being diclofenac.1,2,5 Studies have shown COX-2 selective inhibitors to be less harmful on the gastrointestinal tract than traditional NSAIDs in causing CDD.5
Multiple mechanisms have been proposed for diaphragm formation in the colon. The most likely mechanism contributing to diaphragm formation in the right colon, as was seen in our patient, is the high intraluminal availability of naproxen in the proximal colon.1 Traditional NSAIDs, like naproxen, have a longer half-life and are more likely to reach the colon before they are entirely digested.6 The high intraluminal availability of NSAIDs can affect mucosal integrity, causing circumferential ulceration and leading to submucosal inflammation and fibrosis.2 In turn, the submucosal fibrosis leads to scar tissue, and the ring formation manifests as CDD.
Despite the widespread use of NSAIDs, it is important to note that only a few patients develop CDD. The exact predisposition is unknown, with a possible association of CYP2C9*3 genetic polymorphism leading to the development of CDD. CYP2C9 metabolizes NSAIDs in the liver, and a genetic polymorphism could lead to high plasma concentrations of NSAIDs.5 Cessation of NSAIDs is recommended and is usually associated with an improvement in symptoms. However, cessation of NSAIDs does not result in the resolution of histological findings.7 In symptomatic patients, treatment options include endoscopic dilation or surgical intervention, depending on the clinical presentation and severity of symptoms.8,9
References
- 1.Munipalle PC, Garud T, Light D. Diaphragmatic disease of the colon: systematic review. Colorectal Dis. 2013;15(9):1063–1069. doi: 10.1111/codi.12218. [DOI] [PubMed] [Google Scholar]
- 2.Wang YZ, Sun G, Cai FC, Yang YS. Clinical features, diagnosis, and treatment strategies of gastrointestinal diaphragm disease associated with nonsteroidal anti-inflammatory drugs. Gastroenterol Res Pract. 2016;2016:1–8. doi: 10.1155/2016/3679741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bjarnason I, Hayllar J, MacPherson AJ, Russell AS. Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology. 1993;104(6):1832–1847. doi: 10.1016/0016-5085(93)90667-2. [DOI] [PubMed] [Google Scholar]
- 4.Manocha D, John S, Bansal N, Paul M. Unusual case of acute intestinal obstruction. J Clin Med Res. 2010;2(5):230–232. doi: 10.4021/jocmr439w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ishihara M, Ohmiya N, Nakamura M, et al. Risk factors of symptomatic NSAID-induced small intestinal injury and diaphragm disease. Aliment Pharmacol Ther. 2014;40(5):538–547. doi: 10.1111/apt.12858. [DOI] [PubMed] [Google Scholar]
- 6.Conaghan PG. A turbulent decade for NSAIDs: update on current concepts of classification, epidemiology, comparative efficacy, and toxicity. Rheumatol Int. 2012;32(6):1491–1502. doi: 10.1007/s00296-011-2263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farricielli L, Sanderson DJ. Colonic diaphragm disease: an important NSAID complication to know. Fed Pract. 2017;34(3):38–40. [PMC free article] [PubMed] [Google Scholar]
- 8.Smith JA, Pineau BC. Endoscopic therapy of NSAID-induced colonic diaphragm disease: two cases and a review of published reports. Gastrointest Endosc. 2000;52(1):120–125. doi: 10.1067/mge.2000.105979. [DOI] [PubMed] [Google Scholar]
- 9.Gargot D, Chaussade S, d'Alteroche L, et al. Nonsteroidal anti-inflammatory drug-induced colonic strictures: two cases and literature review. Am J Gastroenterol. 1995;90(11):2035–2038. [PubMed] [Google Scholar]