Abstract
Alopecia areata (AA) is a T cell–mediated autoimmune disease resulting in the destruction of hair follicles. Ophiasis refers to a subtype of AA that presents as a symmetric, band-like hair loss pattern of the occipital, temporal, and parietal regions of the scalp. We present a case of a 58-year-old white man with AA, ophiasis pattern, who was treated with clobetasol 0.05% solution and four treatments of microneedling with triamcinolone over 6 months. He underwent gradual improvement, most notably on his left occipital scalp where his hair loss was most prominent, with near complete hair regrowth on his left occipital scalp. Microneedling with triamcinolone can be considered as a promising treatment in cases of ophiasis AA.
Keywords: Alopecia areata, microneedling, ophiasis, triamcinolone
Alopecia areata (AA) is a T cell–mediated autoimmune disease resulting in the destruction of hair follicles.1 Ophiasis refers to a subtype of AA that presents as a symmetric, band-like pattern of hair loss on the occipital, temporal, and parietal regions of the scalp.1 Recognized by the Greek philosopher Celsus, ophiasis gets its name from ophis, the Greek word for snake—referring to its snake-like distribution, particularly above the ears on the lateral aspects of the scalp.2 It has a poorer prognosis than other forms of AA and is often refractory to conventional treatments, such as intralesional or topical corticosteroids, minoxidil, or topical immunotherapy.
CASE REPORT
A 58-year-old white man with no significant past medical history presented to our clinic with a 3-month history of hair loss on the occipital, vertex, and frontal scalp. He had a history of androgenic alopecia, but this recent episode of hair loss, particularly to the left occipital scalp, was especially abrupt and pronounced. Scalp examination was notable for generalized patchy thinning on the vertex and frontal scalp with miniaturization of hair follicles and a 3 × 10 cm alopecic patch on the left occipital scalp near the hairline. The patient was asymptomatic and denied any itching, burning, stinging, fatigue, or thyroid issues. He had a history of low vitamin D and was on supplementation. Thyroid-stimulating hormone, an iron panel, and vitamin D levels were normal. The patient was diagnosed with AA, ophiasis pattern.
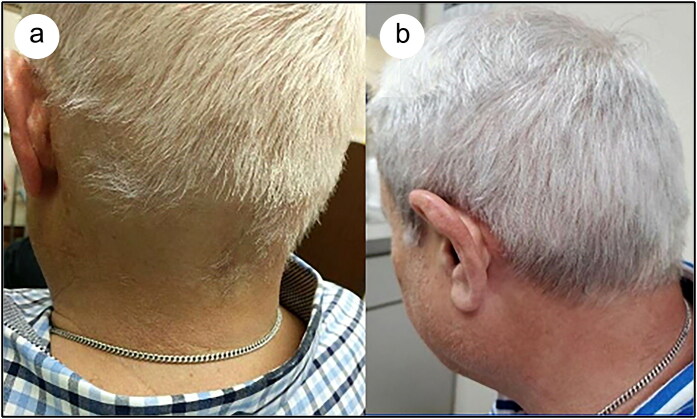
He began his treatment regimen consisting of topical clobetasol 0.05% solution twice daily and triamcinolone (Kenalog) microneedling (1 cc of 20 mg/mL, depth 2 mm, 3 passes on occipital, vertex, and frontal scalp). The microneedling sessions were repeated in April, May, and June of 2019 for a total of four treatments, with the patient continuing his twice-daily topical clobetasol application throughout this period. The patient underwent gradual improvement, most notably on his left occipital scalp where his hair loss was the most severe and prominent (Figure 1). At his 6-month follow-up visit, we noted near complete hair regrowth on his left occipital scalp. The patient was advised to continue topical clobetasol therapy and follow-up regularly with dermatology.
Figure 1.
Ophiasis AA affecting the occipital scalp of a 58-year-old male. Initial scalp examination showed a 3 × 10 cm alopecic patch on the left occipital scalp near the hairline. Prominent and near complete hair regrowth was noted on the left occipital scalp over the course of the four microneedling treatments. (a) February 2019. (b) July 2019.
DISCUSSION
Loss of immune privilege (hair follicles being protected from the immune system) is considered to be the cause of AA. T-cell lymphocytes cluster around affected hair follicles, causing inflammation and subsequent hair loss.3 A family history of autoimmune conditions is often present, and nail pitting or trachyonychia may be seen.4 Hairs with an “exclamation-point” appearance surrounding the alopecic patches are common.5 Histologically, ophiasis AA is characterized by a generalized decrease of terminal hairs, an increase in miniaturized hairs, and a relatively higher incidence of peribulbar lymphocytic infiltration in comparison to other types of AA.1 Interestingly, an “inverse” variant of ophiasis AA has been found to involve the vertex and scalp while completely sparing the occipital and temporal areas, termed sisaipho (ophiasis spelled backwards).6 Cases in the literature have described successful treatment of ophiasis AA with unconventional techniques such as khellin-excimer, platelet-rich plasma, psoralen and ultraviolet A, and fexofenadine.7–10 However, to the best of our knowledge, this is the first case that has shown improvement of ophiasis AA with microneedling.
Microneedling is a minimally invasive procedure in which multiple fine needles are rolled over the skin to puncture the stratum corneum. This induces neovascularization, collagen formation, and growth factor production of treated areas.11 Our rationale for using microneedling was to ensure that the triamcinolone would penetrate the skin and absorb into the dermis, the areas of active inflammation in AA. In contrast, intralesional corticosteroid injections may penetrate into the subcutaneous fat and would result in decreased availability of the medicine to the desired target.
Though our patient improved significantly with our treatment regimen, one weakness of our case was that the patient was also prescribed topical clobetasol solution to use at home. Further studies, possibly using only microneedling as treatment, may be needed to ascertain the degree of its utility in treating ophiasis AA. In conclusion, microneedling may be considered a promising treatment for ophiasis AA, particularly when considering its favorable side effect profile.
References
- 1.Choi JW, Loh SH, Lew BL, Sim WY. Histopathologic features of ophiasis-type alopecia areata. J Am Acad Dermatol. 2016;76(6):AB156.c. [Google Scholar]
- 2.Troxell MA. Ophiasis: report of two cases. AMA Arch Derm Syphilol. 1954;70(6):812–814. doi: 10.1001/archderm.1954.01540240118015. [DOI] [PubMed] [Google Scholar]
- 3.Rajabi F, Drake LA, Senna MM, Rezaei N. Alopecia areata: a review of disease pathogenesis. Br J Dermatol. 2018;179(5):1033–1048. doi: 10.1111/bjd.16808. [DOI] [PubMed] [Google Scholar]
- 4.Hordinsky M, Junqueira AL. Alopecia areata update. Sem Cutan Med Surg. 2015;34(2):72–75. doi: 10.12788/j.sder.2015.0160. [DOI] [PubMed] [Google Scholar]
- 5.Rudnicka L, Olszewska M, Rakowska A, Kowalska-Oledzka E, Slowinska M. Trichoscopy: a new method for diagnosing hair loss. J Drugs Dermatol. 2008;7(7):651–654. [PubMed] [Google Scholar]
- 6.Fonda-Pascual P, Vano-Galvan S, Garcia-Hernandez MJ, Camacho F. Alopecia areata sisaipho: clinical and therapeutic approach in 13 patients in Spain. Int J Trichol. 2016;8(2):99–100. doi: 10.4103/0974-7753.188039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fenniche S, Hammami H, Zaouak A. Association of khellin and 308-nm excimer lamp in the treatment of severe alopecia areata in a child. J Cosmet Laser Ther. 2018;20(3):156–158. doi: 10.1080/14764172.2017.1383617. [DOI] [PubMed] [Google Scholar]
- 8.Donovan J. Successful treatment of corticosteroid-resistant ophiasis-type alopecia areata (AA) with platelet-rich plasma (PRP). JAAD Case Rep. 2015;1(5):305–307. doi: 10.1016/j.jdcr.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lassus A, Eskelinen A, Johansson E. Treatment of alopecia areata with three different PUVA modalities. Photodermatol. 1984;1(3):141–144. [PubMed] [Google Scholar]
- 10.Nonomura Y, Otsuka A, Miyachi Y, Kabashima K. Case of intractable ophiasis type of alopecia areata presumably improved by fexofenadine. J Dermatol. 2012;39(12):1063–1064. doi: 10.1111/j.1346-8138.2012.01571.x. [DOI] [PubMed] [Google Scholar]
- 11.Fertig R, Gamret A, Cervantes J, Tosti A. Microneedling for the treatment of hair loss? J Eur Acad Dermatol Venereol. 2018;32(4):564–569. doi: 10.1111/jdv.14722. [DOI] [PubMed] [Google Scholar]