Abstract
Emerging research and clinical data are demonstrating potential benefits of cannabidiol for multiple medical conditions. This article gives healthcare providers information on cannabidiol and the endocannabinoid system as a foundation on which to build their medical knowledge as the risks and benefits of CBD in various diseases are further evaluated over time.
Keywords: Cannabinoids, endocannabinoid system, hemp, marijuana, phytocannabinoids
As of April 2020, 629 clinical trials have been registered on clinicaltrials.gov investigating cannabidiol (CBD). Because CBD has been marketed as a supplement or alternative medicine rather than through pharmaceutical research and development, it has come into the medical arena with little oversight from the Food and Drug Administration. This article provides an overview of cannabinoids and the endocannabinoid system, including their methods of use and metabolism, as a foundation for understanding CBD use in patients.
CANNABINOIDS
Cannabinoids are the chemical messengers for the endocannabinoid system.1,2 While many different cannabinoids exist, they all fall under two categories: exogenous or endogenous. Exogenous cannabinoids are either plant based or synthetic, while endogenous cannabinoids are produced naturally by the human body. While this article focuses on cannabidiol (CBD), an exogenous cannabinoid, it is important to understand the spectrum of known cannabinoids (Table 1).
Table 1.
Cannabinoids
| Type | Name | Effects |
|---|---|---|
| Exogenous cannabinoids | Cannabis indica (marijuana) plant | |
| Tetrahydrocannabinol (THC) | Antioxidant, anti-inflammatory, euphoric high, analgesic | |
| Cannabidiol (CBD) | Anticonvulsant, antioxidant, anxiolytic, analgesic, anti-inflammatory; treats psychotic disorders and relieves spasms | |
| Cannabigerol (CBG) | Antibiotic, antifungal, anti-inflammatory, analgesic | |
| Cannabinol (CBN) | Sedative, antibiotic, anticonvulsant, anti-inflammatory | |
| Cannabichromene (CBC) | Antibiotic, antifungal, anti-inflammatory, analgesic | |
| Tetrahydrocannabivarin (THCV) | Euphoric high and anxiolytic | |
| Cannabis sativa (hemp) plant | ||
| CBD | Anticonvulsant, antioxidant, anxiolytic, anti-inflammatory; reduces anxiety, treats psychotic disorders, and relieves spasms | |
| Endocannabinoids | Anandamide | |
| 2-arachidonoyl glycerol (2-AG) |
The genus family of Cannabis produces as many as 113 different phytocannabinoids. Hemp and marijuana are harvested from different strains of the Cannabis plant—Cannabis sativa and Cannabis indica. Hemp, which is part of the Cannabis sativa strain and grown for food and fiber, contains <0.3% tetrahydrocannabinol (THC) but is rich in CBD. Of note, hemp seed oil is devoid of CBD since the phytocannabinoids are harvested from the flowers of the plant. Cannabis indica, the marijuana plant, also produces THC and CBD, the most prevalent and best understood phytocannabinoids.
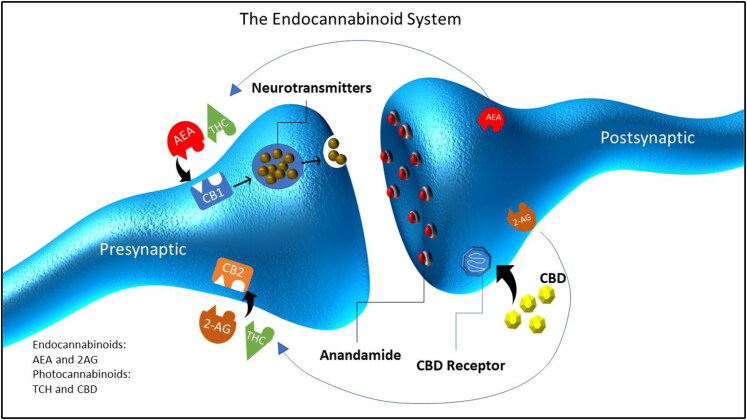
The two major endogenous cannabinoids (endocannabinoids) are anandamide and 2-arachidonoyl glycerol (2-AG). They function as retrograde messengers derived from postsynaptic nerve fibers and thereby regulate neuronal transmission. They interact with presynaptic cannabinoid receptors (Figure 1) to regulate basic functions including mood, memory, appetite, pain, itch, and sleep. Anandamide was discovered in 1992. Its name comes from the Sanskrit word ananda meaning bliss, referring to its unique effects on the mind and body. In 1995, 2-AG was discovered and found at higher concentrations in the brain, while anandamide is found at higher concentrations in other areas of the body. Both endocannabinoids can bind to CB1 and CB2 receptors, but they differ in their affinities for these receptors. Endocannabinoids are transient neurotransmitters, meaning they are synthesized on demand; after being released, they are quickly broken down by two enzymes: fatty acid amide hydrolase (FAAH) and monoacylglycerol lipase.
Figure 1.
Endocannabinoid system.
THE ENDOCANNABINOID SYSTEM
The endocannabinoid system receptors, CB1 and CB2 (Figure 1),3–5 have unique distributions within the body and different ligands, which explains the effects of the different cannabinoids (Table 2). CB1 receptors are found throughout the body, but are mostly present in the brain and spinal cord. They are concentrated in brain regions associated with the behaviors they influence. For example, there are CB1 receptors in the hypothalamus, which is involved with appetite regulation, and the amygdala, which plays a role in memory and emotional processing. CB1 receptors are also found in nerve endings, where they act to reduce sensations of pain. CB2 receptors tend to be found in the peripheral nervous system. They are especially concentrated in immune cells. When CB2 receptors are activated, they work to reduce inflammation. Inflammation is an immune response that plays a role in many diseases and conditions.
Table 2.
Endocannabinoid system receptors
| Receptor | Location | Effect |
|---|---|---|
| CB1 (brain and spinal cord) | Amygdala | Memory and emotional processing |
| Hypothalamus | Appetite regulation | |
| Nerve endings | Pain | |
| CB2 (peripheral nervous system) | Immune cells | Inflammation |
| Spleen | ||
| Liver |
With respect to the CBD found in cannabis, researchers have found that THC binds to both CB1 and CB2 receptors, activating them just like an endocannabinoid but with higher affinity. CBD does not bind directly to cannabinoid receptors. Instead, CBD works by inhibiting FAAH, which is responsible for the breakdown of anandamide—the most important endocannabinoid in the body. When FAAH is inhibited, it cannot break down anandamide at its normal rate. This leads to a buildup of anandamide in the synapse and results in down-regulation of nerve transmission. Additionally, CBD inhibits endocannabinoid reuptake,6 transient receptor potential vanilloid 1 activation, and G-protein-coupled receptor 55 activation and increases the activity of serotonin 5-HA1a receptors, which translates into effects on a wide array of systems in the human body, including the immune system, the nervous system (anxiety, autism, multiple sclerosis, posttraumatic stress disorder, neuropathic pain),7–13 the endocrine system, the cardiovascular system (atherosclerosis),14 the digestive system (inflammatory bowel disease and motility disorders),15,16 and skin (inflammatory skin disorders, disorders of hair and pigment, and itch).17–19
CANNABIDIOL EXTRACTION AND METHOD OF USE
To create a safe CBD product, Cannabis plant extraction techniques such as carbon dioxide extraction, ethanol extraction, or solvent extraction with olive oil are preferred. Extraction techniques using hexane or butane may leave harmful residues. The CBD extracts can be categorized as broad spectrum, full spectrum, or isolate. If all extracts of the Cannabis plant, including CBD, terpenes, flavonoids, essential oils, and other cannabinoids, are utilized, the extract is called full-spectrum CBD and the THC concentration should be <0.3%. Broad spectrum is similar to full spectrum with the exception that it is nearly THC free. Finally, isolate, which is typically harvested from Cannabis sativa, is pure CBD. Historically, some clinical benefits have been seen with broad- or full-spectrum CBD products due to the presumed synergistic actions of the various phytocannabinoids as well as other plant constituents, which is called the “entourage effect.”20
Table 3 lists consumer products in decreasing order of bioavailability. Consumers tend to prefer CBD in the form of topical creams and orals (gummies, candies, tinctures, and capsules). There is little regulation or oversight of the products, so consumers should seek certificates of authenticity and information on the source of CBD and other ingredients.
Table 3.
Administration of CBD listed in decreasing order of bioavailability*
|
From Huestis (2007).22
Since 1985, three systemic cannabinoids have been approved by the Food and Drug Administration.21 In 1985, nabilone (Cesamet), a synthetic analog of THC, was approved for adults with chemotherapy-induced nausea and vomiting. In 1986, dronabinol (Marinol), a synthetic formulation of THC, was approved for adults with human immunodeficiency virus–associated anorexia as well as chemotherapy-induced nausea and vomiting. Finally, in 2018, Epidiolex, a pure pharmaceutical-grade CBD, was approved for two severe pediatric seizure disorders, Lennox-Gastaut syndrome and Dravet syndrome.
METABOLISM AND CAUTIONS
Topical administration of CBD is unlikely to result in systemic blood levels. After oral ingestion and hepatic metabolism, 65% of CBD is excreted unchanged in the feces and 20% is excreted in the urine, where more than 30 metabolites of CBD have been identified.22 Oral administration of CBD can either increase or decrease the breakdown of other drugs via interactions with cytochrome P450 enzymes.23 Caution is advised for use of CBD in patients taking medications that are metabolized by the cytochrome P450 pathway and have a narrow therapeutic window.23 Marijuana may affect male and female fertility.24,25 Women should be advised to refrain from using marijuana during pregnancy and lactation.26 More data are needed for the use of CBD in patients with active cancers.27
SUMMARY
CBD, an exogenous phytocannabinoid, can act as a neurotransmitter and is known to have anti-inflammatory and antioxidant properties. Phytocannabinoids have now been identified in many plants outside of the Cannabis species, including clove, black pepper, Echinacea, broccoli, ginseng, and carrots. We are just beginning to understand the impact of phytocannabinoids and their clinical applications. It is important for healthcare providers to be aware of CBD use in their patient population.
References
- 1.Scheau C, Badarau IA, Mihai LG, et al. Cannabinoids in the pathophysiology of skin inflammation. Molecules. 2020;25(3):652. doi: 10.3390/molecules25030652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burstein S. Cannabidiol (CBD) and its analogs: a review of their effects on inflammation. Bioorg Med Chem. 2015;23(7):1377–1385. doi: 10.1016/j.bmc.2015.01.059. [DOI] [PubMed] [Google Scholar]
- 3.Lu HC, Mackie K. An introduction to the endogenous cannabinoid system. Biol Psychiatry. 2016;79(7):516–525. doi: 10.1016/j.biopsych.2015.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Di Marzo V, Piscitelli F. The endocannabinoid system and its modulation by phytocannabinoids. Neurotherapeutics. 2015;12(4):692–698. doi: 10.1007/s13311-015-0374-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Castillo PE, Younts TJ, Chavez AE, Hashimotodani Y. Endocannabinoid signaling and synaptic function. Neuron. 2012;76(1):70–81. doi: 10.1016/j.neuron.2012.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morena M, Patel S, Bains JS, Hill MN. Neurobiological interactions between stress and the endocannabinoid system. Neuropsychopharmacology. 2016;41(1):80–102. doi: 10.1038/npp.2015.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel S, Hill MN, Cheer JF, Wotjak CT, Holmes A. The endocannabinoid system as a target for novel anxiolytic drugs. Neurosci Biobehav Rev. 2017;76(Pt A):56–66. doi: 10.1016/j.neubiorev.2016.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zamberletti E, Gabaglio M, Parolaro D. The endocannabinoid system and autism spectrum disorders: insights from animal models. Int J Mol Sci. 2017;18(9):1916. doi: 10.3390/ijms18091916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiurchiu V, van der Stelt M, Centonze D, Maccarrone M. The endocannabinoid system and its therapeutic exploitation in multiple sclerosis: clues for other neuroinflammatory diseases. Prog Neurobiol. 2018;160:82–100. doi: 10.1016/j.pneurobio.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Lutz B, Marsicano G, Maldonado R, Hillard CJ. The endocannabinoid system in guarding against fear, anxiety and stress. Nat Rev Neurosci. 2015;16(12):705–718. doi: 10.1038/nrn4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang WJ, Chen WW, Zhang X. Endocannabinoid system: role in depression, reward and pain control (Review). Mol Med Rep. 2016;14(4):2899–2903. doi: 10.3892/mmr.2016.5585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donvito G, Nass SR, Wilkerson JL, et al. The endogenous cannabinoid system: a budding source of targets for treating inflammatory and neuropathic pain. Neuropsychopharmacology. 2018;43(1):52–79. doi: 10.1038/npp.2017.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masocha W. Targeting the endocannabinoid system for prevention or treatment of chemotherapy-induced neuropathic pain: studies in animal models. Pain Res Manage. 2018;2018:5234943doi: 10.1155/2018/5234943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fulmer ML, Thewke DP. The endocannabinoid system and heart disease: the role of cannabinoid receptor type 2. Cardiovasc Hematol Disord Drug Targets. 2018;18(1):34–51. doi: 10.2174/1871529X18666180206161457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leinwand KL, Gerich ME, Hoffenberg EJ, Collins CB. Manipulation of the endocannabinoid system in colitis: a comprehensive review. Inflamm Bowel Dis. 2017;23(2):192–199. doi: 10.1097/MIB.0000000000001004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pesce M, D'Alessandro A, Borrelli O, et al. Endocannabinoid-related compounds in gastrointestinal diseases. J Cell Mol Med. 2018;22(2):706–715. doi: 10.1111/jcmm.13359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pacher P, Batkai S, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev. 2006;58(3):389–462. doi: 10.1124/pr.58.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biro T, Toth BI, Hasko G, Paus R, Pacher P. The endocannabinoid system of the skin in health and disease: novel perspectives and therapeutic opportunities. Trends Pharmacol Sci. 2009;30(8):411–420. doi: 10.1016/j.tips.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toth KF, Adam D, Biro T, Olah A. Cannabinoid signaling in the skin: therapeutic potential of the “c(ut)annabinoid” system. Molecules. 2019;24(5):918. doi: 10.3390/molecules24050918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ben-Shabat S, Fride E, Sheskin T, et al. An entourage effect: inactive endogenous fatty acid glycerol esters enhance 2-arachidonoyl-glycerol cannabinoid activity. Eur J Pharmacol. 1998;353(1):23–31. doi: 10.1016/S0014-2999(98)00392-6. [DOI] [PubMed] [Google Scholar]
- 21.Bonn-Miller MO, ElSohly MA, Loflin MJE, Chandra S, Vandrey R. Cannabis and cannabinoid drug development: evaluating botanical versus single molecule approaches. Int Rev Psychiatry. 2018;30(3):277–284. doi: 10.1080/09540261.2018.1474730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huestis MA. Human cannabinoid pharmacokinetics. Chem Biodivers. 2007;4(8):1770–1804. doi: 10.1002/cbdv.200790152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown JD, Winterstein AG. Potential adverse drug events and drug-drug interactions with medical and consumer cannabidiol (CBD) use. J Clin Med. 2019;8(7):989. doi: 10.3390/jcm8070989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brents LK. Marijuana, the endocannabinoid system and the female reproductive system. Yale J Biol Med. 2016;89(2):175–191. [PMC free article] [PubMed] [Google Scholar]
- 25.Du Plessis SS, Agarwal A, Syriac A. Marijuana, phytocannabinoids, the endocannabinoid system, and male fertility. J Assist Reprod Genet. 2015;32(11):1575–1588. doi: 10.1007/s10815-015-0553-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Metz TD, Borgelt LM. Marijuana use in pregnancy and while breastfeeding. Obstet Gynecol. 2018;132(5):1198–1210. doi: 10.1097/AOG.0000000000002878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fraguas-Sanchez AI, Martin-Sabroso C, Torres-Suarez AI. Insights into the effects of the endocannabinoid system in cancer: a review. Br J Pharmacol. 2018;175(13):2566–2580. [DOI] [PMC free article] [PubMed] [Google Scholar]