Abstract
Purpose of Review
During overhead throwing, there are tremendous forces placed on the medial elbow that can result in injury to the ulnar nerve. The purpose of this article is to review the anatomy, biomechanics, and appropriate clinical care of an overhead throwing athlete suffering from injury to their ulnar nerve. The authors preferred clinical work-up; non-operative and operative care are included in this review.
Recent Findings
More recent findings support the use of subcutaneous transposition instead of the submuscular transpositions and only to perform a transposition in the setting of specific pre-operative findings. Subcutaneous transpositions have led to decreased rates of post-operative symptoms and complications.
Summary
Understanding the complexity of the medial elbow is essential to making an accurate diagnosis of ulnar neuritis/neuropathy in the overhead throwing athlete. In general, non-operative management has shown to be successful; however, in those refractory or recurrent cases of ulnar neuritis, ulnar nerve decompression with or without transposition provides these athletes with a surgical procedure that has shown to provide patients with excellent outcomes. Continued refinement surgical indications and surgical technique will allow for a high percentage of athletes who return to competitive sports following surgery for ulnar neuropathy.
Keywords: Ulnar nerve, Ulnar neuritis, Throwing athlete, Transposition
Introduction
In recent years, there has been an increase in the number of participants and an increase in specialization of overhead throwing athletes. Due to this increase, there has been an associated increase in the incidence of injury to the throwing arm in these athletes. Overhead throwing in the athlete places enormous valgus stress on the medial elbow. These forces can lead to various injuries to the medial elbow. Common injuries seen in the throwing athlete include but are not limited to flexor tendonitis, medial epicondyle apophysitis or avulsion, osteochondritis dissecans of the capitellum, valgus extension overload (VEO) syndrome, ulnar collateral ligament (UCL) insufficiency, and ulnar neuropathy. Ulnar neuropathy at the elbow is the second most prominent neuropathy of the upper extremity, and its superficial location makes it particularly susceptible to injury in throwing athletes. The ulnar nerve is susceptible to several mechanical factors, including trauma, compression, traction, and irritation of the nerve. Ulnar neuritis is a common reason for pain and neurologic symptoms in the throwing elbow but often is secondary to valgus instability, which causes traction across the nerve. However, cervical spine disease and thoracic outlet syndrome can cause overlapping symptoms and must be addressed in patients presenting with symptoms of ulnar neuritis.
Due to the complex anatomy, biomechanics, and possible injuries that can occur in the overhead throwing athlete, accurate diagnosis and treatment of these injuries is essential. Recent data from Major League Baseball (MLB) suggested that up to 16% of all documented injuries resulted from elbow pathology [1, 2]. Other analyses from MLB and Minor League Baseball (MiLB) suggested that > 40% of all elbow injuries involve the medial side of the elbow [3••]. With this in mind, it is essential to understand the complex anatomy, function and biomechanics of an overhead throwers elbow.
The purpose of this manuscript is to review current knowledge regarding the diagnosis and treatment of ulnar nerve injuries in the overhead throwing athlete. A brief review of our preferred surgical technique for ulnar nerve transposition is included.
Anatomy and Biomechanics of Throwing
The ulnar nerve originates from the ventral rami receiving contributions from cervical root C8 and thoracic root T1. The ulnar nerve is a mixed nerve containing both motor and sensory axons. After passing through the axilla, the ulnar nerve divides from the medial cord of the brachial plexus. The nerve then descends through the upper arm medial to the brachial artery until the insertion of the coracobrachialis muscle, at which point the nerve courses anterior to posterior piercing the intermuscular septum and passing under the Arcade of Struthers. The Arcade is a confluence of connective tissue of the arm comprised of the medial head of the triceps, the medial intermuscular septum, and the internal brachial ligament. Located 6–8 cm proximal to the medial epicondyle of the elbow, the Arcade of Struthers is a common site of compression of the ulnar nerve and must be addressed at the time of ulnar nerve decompression and anterior transposition as it can act as a tether to the nerve.
After passing through the Arcade of Struthers, the ulnar nerve travels distally and courses along the posterior–medial intermuscular septum. Approaching the elbow, the ulnar nerve continues posterior to the medial epicondyle and enters the cubital tunnel. The borders of the cubital tunnel consist of the posterior UCL and capsule laterally, the medial epicondylar groove anteriorly, and the arcuate ligament medially. As the nerve travels posterior–medial to the medial epicondyle of the elbow, it gives rise to its first nerve branch, a proprioceptive nerve to the joint capsule. The nerve then passes underneath Osborne’s ligament (retinaculum between the two heads of the flexor carpi ulnaris) as it pierces the two heads of the flexor carpi ulnaris (FCU) muscle [4]. Compression of the cubital tunnel by Osborne’s ligament may reduce gliding of the nerve throughout the flexion and extension arc of the elbow. Cross-sectional area of the cubital tunnel can be reduced by as much as 40% during the flexion arc of the elbow when pathologic fusion of the layers of Osborne’s ligament occurs [5]. Additionally, along this path, an anomalous muscle, the anconeus epitrochlearis, may be a cause of ulnar nerve compression or irritation. Recently, Li et al. found evidence that the anconeus epitrochlearis may indicate hypertrophy in overhead throwing athletes [6].
After piercing the two heads of the flexor carpi ulnaris, the nerve enters the anterior forearm. Two additional sites of ulnar nerve compression once the nerve has entered the forearm are the deep fascia of the FCU as well as the confluence of fascia from the flexor digitorum superficialis to the ring finger. Wojtys et al. and Hang [7, 8] have emphasized the importance of decompression in this area due to the common occurrence of compression in overhead throwing athletes. Terminal innervation of the ulnar nerve provides motor units to the FCU, medial one-half of the flexor digitorum profundus, hypothenar eminence, and hand intrinsic muscles, as well as sensation to the ring and small fingers.
Elbow injury in the throwing athlete can be understood by examining the biomechanics of the elbow joint during the throwing motion. The biomechanics of most overhead throwing sports are grouped together because of the similarities in the general motion. Specifically, a baseball throwing motion is the most investigated of these and provides a basis for general understanding of throwing biomechanics. The throwing motion of a baseball pitch is subdivided into six specific stages. These specific stages include wind-up, early cocking, late cocking, acceleration, deceleration, and follow-through.
Most injuries in the overhead thrower occur during stage IV or the acceleration phase of throwing due to the enormous stress created at the elbow. These large rotational moments at the elbow generate large amounts of force throughout the multiple articulations of the elbow. During the acceleration phase of throwing, biomechanical testing has an estimated peak elbow acceleration approaching 600,000°/s2, with valgus forces of approximately 64 Nm at the medial elbow and compressive forces of up to 500 N at the radiocapitellar joint [9, 10]. Additionally, during peak deceleration, the elbow can see up to 500,000°/s2 of rotation over a time span of 50 ms as excess kinetic energy is dissipated [11–14]. The combination of these forces can cause a spectrum of disorders and has been termed by Andrews et al. as valgus extension overload syndrome (VEO) [15]. While changes to the throwing mechanics of each individual may decrease the overall stress on the medial elbow during overhead throwing, these may not lead to improved clinical outcomes as stress seen from the repetitive nature of throwing may be the driving force leading to injury. The repetitive nature of overhead throwing leads to near-tensile failure loads and microtrauma to the anterior band of the UCL causing ligament attenuation and eventual failure. In 2019, Mihata et al. provided cadaveric evidence that injury to the UCL causes significant strain and elongation of the ulnar nerve at both 60 and 90° of flexion [16••]. Thus, while failure of the UCL more predictably can lead to ulnar neuritis, subtle laxity, or stretching of the medial soft tissues due to VEO syndrome, it can also lead to ulnar neuritis.
History and Physical Exam
The diagnosis of ulnar neuritis in the overhead throwing athlete is predominately based on history and physical exam [17]. Ulnar neuritis may occur independently; however, most often, it is secondary medial elbow laxity and secondary strain on the ulnar nerve. Thus, an athlete’s chief complaint may help delineate between primary (i.e., decreased velocity on pitch from UCL attenuation) and secondary processes (i.e., pain and paresthesias from ulnar neuritis) [18].
A history of prior injuries and changes in accuracy, velocity, stamina, and strength are essential clues in the eventual diagnosis. Complaints may include pain, decreased motion, mechanical symptoms (clicking, locking, popping, and so forth), instability, and paresthesias. Early signs of injury to the ulnar nerve may include but are limited to cold intolerance, numbness or tingling in the hand or fingertips, shooting sensations, and tendency to drop objects [17, 19]. The athlete may present with unclear timing of symptoms; however, if a specific injury has occurred, it is important to know when, how, and whether preceding symptoms were present prior to the acute trauma [18]. If no acute event occurred, the onset of symptoms and the phase of throwing during which pain is experienced are important and can be helpful in the diagnosis. Specifically, changes in a training or throwing regimen, pitch counts, innings pitched, games pitched, and rest period between outings should be noted.
Symptoms of ulnar neuritis consist of an aching pain along the ulnar side of the forearm radiating into the ulnar 2 digits of the hand. Monofilament testing can detect early sensory changes, and hand intrinsic atrophy or weakness represents the earliest motor changes but can represent a more advanced stage of the disease. A feeling of snapping or popping may be present in cases of ulnar nerve subluxation as the elbow moves from extension to flexion.
Careful examination of the nerve along its course should begin above the medial epicondyle. Gentle palpation of the nerve should not illicit symptoms distally in the forearm or hand. During a range of motion of the elbow, it is essential to note any signs of subluxation or dislocation of the ulnar nerve from the cubital tunnel. A Tinel’s sign should be performed along the length of the nerve at medial elbow. A positive finding would occur if symptoms (pain or paresthesias) are reproduced with gentle tapping along the ulnar nerve.
Physical examination begins with inspection of an athlete’s posture, arm position, muscle mass, and skin in comparison to the contralateral arm and asymmetry. The carrying angle is the angle between a line drawn along the axis of the humerus and a line drawn along the axis of the forearm. This measurement should be performed in anatomic position with 0° of shoulder flexion, the elbow in full extension, and the forearm in full supination. The normal carrying angle is 11° valgus in adult males and 13° valgus in adult females [20]. Increases in carrying angle due to either developmental abnormality or previous trauma may result in a lengthened ulnar nerve course and increased susceptibility to traction injury. King et al. demonstrated that it is not uncommon to find valgus angles greater than 15° in professional throwers due to adaptive changes at the elbow during development [21].
Physical exam of the ulnar nerve must include palpation of the entire length of the nerve and should begin above the medial epicondyle through the cubital tunnel and distally as far as possible into the flexor carpi ulnaris muscle mass. Gentle palpation of the nerve should not illicit symptoms distally in the forearm or hand. During a range of motion of the elbow, it is essential to note any signs of subluxation or dislocation of the ulnar nerve from the cubital tunnel. Typically, the unstable ulnar nerve will dislocate anterior to the medial epicondyle while the elbow is moved from extension to flexion (Fig. 1). A Tinel’s sign should be performed along the length of the nerve at medial elbow. A positive finding would occur if symptoms (pain or paresthesias) are reproduced with gentle tapping along the ulnar nerve. Additionally, a thorough assessment of the cervical spine needs to be performed to look for evidence of radiculopathy or degenerative changes in the setting of ulnar nerve symptoms [22••].
Fig. 1.

Gentle palpation of the ulnar nerve while the elbow is moved through flexion and extension evaluating for instability of subluxation
Neurovascular exam of the remaining nerves and distal pulses in the arm is important as symptoms from surrounding nerves can often confound the diagnosis in ulnar neuropathy. Also, performing a full and complete exam with range of motion evaluation, strength testing of the biceps, triceps, pronation, supination, wrist flexion, and extension with comparison to the contralateral side will be helpful in making a correct diagnosis.
Stability of the elbow can be assessed with patients in either the supine or seated position. In the supine position, the humerus is stabilized in maximal external rotation and 30° of flexion. With the forearm fully pronated and the elbow flexed 20 to 30° to unlock the olecranon, valgus stress is gradually applied to the elbow. Less than 1 mm of opening and a firm endpoint are normal and can be appreciated during the manual valgus stress test. However, noting millimeter differences while performing these tests can prove to be challenging, and thus, it is more appropriate to compare the stability with the contralateral extremity and note any increased laxity side to side. Additionally, while performing this test, increases in a patient’s pain should raise suspicion of injury to the anterior band of the anterior bundle of the UCL and may often be the underlying cause of the ulnar nerve symptoms.
The milking maneuver is an additional special test that can be performed to assess the posterior band of the anterior bundle of the UCL. In this maneuver, the forearm is supinated fully, and the elbow is flexed beyond 90° (approximately 120°) and the humerus is at the athlete’s side [7]. The thumb is then pulled laterally by the examiner or the athlete’s contralateral extremity, creating a valgus force on the elbow. Pain, instability, or apprehension is indicative of injury to the UCL [18].
Imaging
Standard radiographic series of the thrower’s elbow includes anteroposterior, lateral, and with internal and external oblique views of the affected side. Comparison views of the opposite elbow may be done if necessary, especially in the pediatric population. If medial instability is suspected, stress anteroposterior radiographs can be performed with the use of a valgus stress radiography machine (Telos, Weiterstadt, Gernamy) or using fluoroscopy and comparing opening to the contralateral side. Measurement of greater than 3 mm of opening is concerning for a UCL injury [9, 23]. Although initial radiographs can be difficult to evaluate, the clinician should assess for the presence of olecranon osteophytes, UCL calcifications, excessive valgus deformity, or other bony changes that may cause ulnar nerve compression.
Electrodiagnostic studies may be helpful in the diagnosis of ulnar neuropathy; however, changes from normal may not be seen until the advanced stages of the disease. Wei et al. found no difference in the electrodiagnostic studies of injured baseball pitchers when comparing the conduction velocities of their dominant and non-dominant arms [24]. Additionally, if a negative test is obtained, this does not rule out the presence of ulnar neuritis/neuropathy.
Magnetic resonance imaging (MRI) is not routinely used and is not necessary for evaluation of the ulnar neuritis. However, because ulnar neuritis is often secondary to underlying medial elbow laxity of UCL injury, an MRI may be used to evaluate the UCL or other lesions causing direct nerve compression.
Non-operative Treatment
Initial management of ulnar neuropathy with conservative treatment is appropriate in the overhead throwing athlete [25]. Non-operative treatment involves rest, specifically from overhead throwing, anti-inflammatory medication, and physical therapy. Additionally, the use of splinting at night for up to 6 weeks has been shown to provide some symptom relief in patients with ulnar neuropathy [26•]. This may be helpful especially in a thrower with an unstable ulnar nerve [25]. A gradual interval-throwing program is initiated, and a stretching program for the posterior capsule is often indicated [22••]. An extended period of conservative treatment (3–6 months) is recommended before considering surgical treatment [27]. However, ulnar neuropathy in the overhead thrower stems from the activity of throwing, and if throwing is resumed, symptoms can recur.
Operative Treatment
The indications for operative treatment of ulnar neuritis/neuropathy in the throwing athlete include failed non-operative management, persistent ulnar nerve subluxation, concomitant UCL injury requiring operative repair/reconstruction, and other associated medial elbow pathologies that require ulnar nerve considerations during surgery. Surgical treatment options include simple decompression with neurolysis or surgical decompression with transposition (subcutaneous vs. submuscular). Some controversy persists regarding the benefits of simple decompression vs. decompression with transposition. Historically, ulnar nerve decompression with submuscular transposition was utilized when performing a UCL reconstruction. However, subcutaneous transposition has become more favorable in recent years with decreased rates of continued post-operative symptoms of ulnar neuritis [28–30]. Additionally, while submuscular transposition was considered the “gold standard” for the operative treatment of ulnar nerve issues, there was always concern performing a submuscular transposition in throwers due to the potential damage of the flexor–pronator mass.
Simple decompression of the ulnar nerve has historically been thought best suited for non-throwers due to retention of native anatomy and allowance for rapid recovery. However, due to the traction forces placed on the ulnar nerve in overhead throwers, a simple decompression can lead to increased failure rates and recurrence of symptoms [31, 32]. Simple decompression has also been noted to result in increased ulnar nerve instability or subluxation [33, 34]. Simple decompression begins with a 6–8-cm incision centered over the posterior medial epicondyle of the humerus. The skin is incised, and dissection is carried through the subcutaneous tissues, being careful to preserve the crossing cutaneous nerves of the medial elbow. The nerve is most easily identified proximally as it enters the cubital tunnel. The cubital tunnel is released fully beginning at the Arcade of Struthers ensuring the release of the fibrous band at the FCU origin. The nerve remains in its native bed and is free from any direct compression or adhesions (Figs. 2 and 3). Furthermore, a medial epicondylectomy should be discouraged in the overhead throwing athlete due to concern for compromise of the proximal attachment of the UCL on the humerus [35].
Fig. 2.
Ulnar nerve decompression with release of the intermuscular septum
Fig. 3.

Ulnar nerve decompression demonstrating full decompression proximally through the Arcade of Struthers and distally to the 2 heads of FCU
Anterior transposition of the ulnar nerve in the overhead thrower provides many advantages over surgical decompression and neurolysis alone and over submuscular transposition. Specifically, subcutaneous transposition has the advantage of less surgical morbidity to the flexor–pronator mass and may be recommended in patients undergoing concomitant UCL reconstruction [30, 32, 36]. The ulnar nerve is carefully dissected free as previously described, transposed anterior to the medial epicondyle, and stabilized with a fascial sling from the flexor–pronator fascia. Rettig and Ebben performed 21 anterior subcutaneous transposition procedures in 20 athletes for failed conservative management of cubital tunnel syndrome. All athletes returned to play at an average of 12.6 weeks and excellent outcomes. Eaton and colleagues described subcutaneous ulnar nerve transfer in 16 elbows. All pitchers were able to return to sport without symptoms, with no reported complications in their cohort [37]. The investigators in both studies recommended subcutaneous transposition in light of faster post-operative recovery and rehabilitation [38]. The main disadvantage of the subcutaneous technique is its susceptibility to direct trauma on the nerve. Additionally, there are some who advocate for no fasciodermal sling with the concern of developing recurrence of symptoms due to scarring and compression of the sling [18].
Submuscular transposition was first described by Learmonth in 1942; however, this technique was popularized by Jobe et al. in 1986 when describing his UCL reconstruction technique. As previously described, the nerve is found and released from the cubital tunnel and subsequently transposed to lie directly under the flexor–pronator mass. While this technique has been criticized for its use in throwers due to the concern of injury to the flexor–pronator mass, it does have the advantage over a subcutaneous transposition as it allows a straight path for the ulnar nerve with a layer of muscular protection from trauma. Several authors have reported good results with submuscular transposition, but others noted a high rate of complications related to both the ulnar nerve and flexor–pronator muscle mass [28, 35, 39, 40]. Jobe et al. reported a 31% incidence of post-operative ulnar nerve dysfunction after UCL reconstruction with submuscular transposition of the ulnar nerve [28, 39]. Although there are several studies supporting the use of a submuscular transposition technique in the overhead throwing athlete, we perform a subcutaneous transposition because of concerns about the ultimate strength and healing of the flexor–pronator muscle mass and difficulty with nerve dissection in the case of revision elbow surgery.
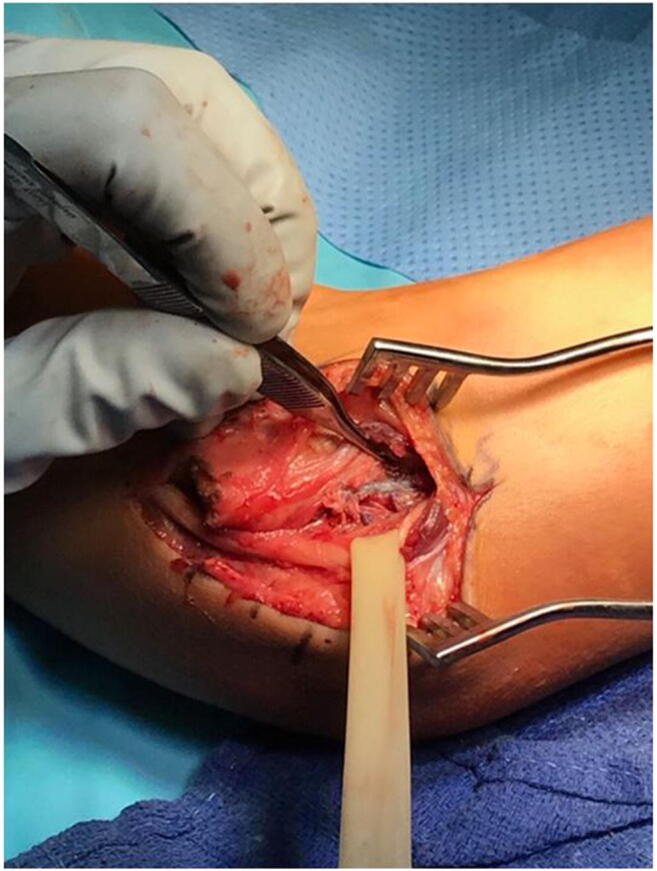
Authors’ Preferred Technique
The patient is placed supine on the operating table utilizing the hand table extension. Prior to incision and while under anesthesia, another physical exam of the elbow is performed to evaluate for ulnar nerve stability in the cubital tunnel and for overall ligamentous stability of the elbow. A tourniquet is placed and utilized until the end of the procedure to allow for optimal visualization of the nerve. We begin by making a 6-cm incision over the medial aspect of the elbow. Dissection is carried through the subcutaneous tissues being careful to identify and preserve the crossing cutaneous branches of the ulnar nerve. The nerve is then identified behind the medial epicondyle as it passes behind the intermuscular septum. Careful dissection of the nerve is then performed. Release of the cubital tunnel is performed, first proximally by ensuring full release of the Arcade of Struthers and intermuscular septum. Next, a complete fascial release of the nerve at the medial epicondyle is performed and extended 2–3 cm distally beyond the 2 heads of the FCU. This usually requires utilization of a Penrose drain for back side dissection. Once the ulnar nerve had been fully dissected, we confirm the ability to transpose without any tension on the nerve. Usually, a small segment of the intermuscular septum is excised in order to decrease any tension during transposition. Next, while holding the nerve in its transposed position, we close the subcutaneous fat from the anterior skin flap over the epicondyle, so as to transpose the nerve anteriorly. The tourniquet is released, and all bleeding is cauterized. The wound is closed in layers, and the patient is placed in a well-padded posterior splint at 90° of flexion. Post-operative care consists of splint and sling immobilization for 1 week post-operatively. This is followed by progressive active and passive range of motion exercises. Active strengthening is begun at 6 weeks after surgery with an expected return to play and initiation of a throwing program at 3–4 months following surgery.
Conclusion/Summary
Injury to the elbow in the overhead throwing athlete is a result of the valgus forces placed on the elbow during the throwing motion. Although baseball players are thought of as the most commonly affected, other overhead throwing and hitting athletes can also suffer injury. Ulnar neuritis is a common ailment of the overhead thrower; however, it is imperative that the examining provider rules out injury to the ulnar collateral ligament as ulnar neuritis is commonly seen in athletes with UCL injuries. Conservative management is first line in the treatment of ulnar neuritis and may result in resolution of symptoms; however, it is common that symptoms return and may require surgical intervention in overhead throwers. Multiple surgical techniques have been described and provide most patients with excellent results. It is our preferred technique to perform an ulnar nerve transposition with subcutaneous transposition in the overhead throwing athlete. As previously described, when evaluating a patient presenting with medial sided elbow pain, the outcomes of ulnar nerve transposition in overhead athletes support both approaches in throwing athletes.
Compliance with Ethical Standards
Conflict of Interest
S. Blake Dowdle declares no conflict of interest.
Peter N. Chalmers conflicts listed below:
1. Arthrex, Inc.: paid consultant
2. DePuy, A Johnson & Johnson Company: IP royalties; paid presenter or speaker
3. Journal of Shoulder and Elbow Surgery: publishing royalties, financial or material support
4. Mitek: paid consultant
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Injuries in Overhead Athletes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Conte S, Requa RK, Garrick JG. Disability days in Major League Baseball. Am J Sports Med. 2001;29:431–436. doi: 10.1177/03635465010290040801. [DOI] [PubMed] [Google Scholar]
- 2.Posner M, Cameron KL, Wolf JM, Belmont PJ, Owens BD. Epidemiology of major league baseball injuries. Am J Sports Med. 2011. [DOI] [PubMed]
- 3.•• Ciccotti MG, Pollack KM, Ciccotti MC, D’Angelo J, Ahmad CS, Altchek D, et al. FV findings from the major league baseball injury surveillance system. Am J Sports Med. 2017 ;45(10):2319–2328. [cited 2019 Sep 19]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28575638. A significant proportion (> 40%) of all elbow injuries in professional baseball players involves the medial elbow and > 90% of nerve injury involving the ulnar nerve. [DOI] [PubMed]
- 4.Becker RE, Manna B. Anatomy, shoulder and upper limb, ulnar nerve. StatPearls. StatPearls Publishing; 2019 [Cited 2019 Sep 19]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29763067. [PubMed]
- 5.Tubbs RS, Deep A, Shoja MM, Mortazavi MM, Loukas M, Cohen-Gadol AA. The arcade of Struthers: an anatomical study with potential neurosurgical significance. Surg Neurol Int. 2011 ;2:184. [cited 2020 Jan 30]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22276238. [DOI] [PMC free article] [PubMed]
- 6.Li X, Dines JS, Gorman M, Limpisvasti O, Gambardella R, Yocum L. Anconeus epitrochlearis as a source of medial elbow pain in baseball pitchers. Orthopedics. 2012 ;35(7):e1129–e1132. [cited 2019 Sep 19]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22784916. [DOI] [PubMed]
- 7.Wojtys EM, Smith PA, Hankin FM. A cause of ulnar neuropathy in a baseball pitcher. A case report. Am J Sports Med [Internet]. 1986 Sep 23 [cited 2019 Sep 19];14(5):422–4. Available from: https://deepblue.lib.umich.edu/bitstream/handle/2027.42/66653/10.1177_036354658601400518.pdf?sequence=2&isAllowed=y [DOI] [PubMed]
- 8.Hang Y-S. Tardy ulnar neuritis in a Little League baseball player. Am J Sports Med [Internet]. 1981 Jul 23 [cited 2019 Sep 19];9(4):244–6. Available from: https://doi-org.ezproxy.lib.utah.edu/10.1177/036354658100900410 [DOI] [PubMed]
- 9.Schwab GH, Bennett JB, Woods GW, Tullos HS. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin Orthop Relat Res [Internet]. [cited 2019 Sep 20];(146):42–52. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7371268. [PubMed]
- 10.Pappas AM, Zawacki RM, Sullivan TJ. Biomechanics of baseball pitching. A preliminary report. Am J Sports Med [Internet]. 1985 Jul 23 [cited 2019 Sep 20];13(4):216–22. Available from: https://doi-org.ezproxy.lib.utah.edu/10.1177/036354658501300402 [DOI] [PubMed]
- 11.Digiovine NM, Jobe FW, Pink M, Perry J. An electromyographic analysis of the upper extremity in pitching. J shoulder Elb Surg [Internet]. 1992 Jan [cited 2019 Sep 20];1(1):15–25. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1058274609800116 [DOI] [PubMed]
- 12.Glousman RE, Barron J, Jobe FW, Perry J, Pink M. An electromyographic analysis of the elbow in normal and injured pitchers with medial collateral ligament insufficiency. Am J Sports Med [Internet]. 1992 May 23 [cited 2019 Sep 20];20(3):311–7. Available from: https://doi-org.ezproxy.lib.utah.edu/10.1177/036354659202000313 [DOI] [PubMed]
- 13.Hamilton CD, Glousman RE, Jobe FW, Brault J, Pink M, Perry J. Dynamic stability of the elbow: electromyographic analysis of the flexor pronator group and the extensor group in pitchers with valgus instability. J shoulder Elb Surg [Internet]. [cited 2019 Sep 20];5(5):347–54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8933456. [DOI] [PubMed]
- 14.Jobe FW, Moynes DR, Tibone JE, Perry J. An EMG analysis of the shoulder in pitching. A second report. Am J Sports Med [Internet]. 1984 May 23 [cited 2019 Sep 20];12(3):218–20. Available from: https://doi-org.ezproxy.lib.utah.edu/10.1177/036354658401200310 [DOI] [PubMed]
- 15.Andrews JR. Bony injuries about the elbow in the throwing athlete. Instr Course Lect. 1985;34:323–331. [PubMed] [Google Scholar]
- 16.Mihata T, Akeda M, Künzler M, MH MG, Neo M, Lee TQ. Ulnar collateral ligament insufficiency affects cubital tunnel syndrome during throwing motion: a cadaveric biomechanical study. J Shoulder Elb Surg. 2019;28(9):1758–1763. doi: 10.1016/j.jse.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 17.Andrews JR, Wilk KE, Satterwhite YE, Tedder JL. Physical examination of the thrower’s elbow. J Orthop Sport Phys Ther [Internet]. 1993 Jun [cited 2019 Sep 20];17(6):296–304. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8343789. [DOI] [PubMed]
- 18.Patel RM, Lynch TS, Amin NH, Calabrese G, Gryzlo SM, Schickendantz MS. Orthopedic Clinics of North America. 2014. 356–365 p. [DOI] [PubMed]
- 19.Dugas JR, Weiland AJ. Vascular pathology in the throwing athlete. Hand Clin [Internet]. 2000 Aug [cited 2019 Sep 20];16(3):477–85, x. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10955220. [PubMed]
- 20.Beals RK. The normal carrying angle of the elbow. A radiographic study of 422 patients. Clin Orthop Relat Res [Internet]. 1976 Sep [cited 2019 Sep 20];(119):194–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/954311. [PubMed]
- 21.King JW, Brelsford HJ, Tullos HS. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop Relat Res [Internet]. [cited 2019 Sep 20];67:116–23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/5361189. [PubMed]
- 22.•• Conti MS, Camp CL, Elattrache NS, Altchek DW, Dines JS. Treatment of the ulnar nerve for overhead throwing athletes undergoing ulnar collateral ligament reconstruction. Vol. 7, World Journal of Orthopaedics. Baishideng Publishing Group Co; 2016. p. 650–656. [DOI] [PMC free article] [PubMed]
- 23.Morrey BF. Applied anatomy and biomechanics of the elbow joint. Instr Course Lect. 1986;35:59–68. [PubMed] [Google Scholar]
- 24.Wei S-H, Jong Y-J, Chang Y-J. Ulnar nerve conduction velocity in injured baseball pitchers. Arch Phys Med Rehabil [Internet]. 2005 Jan [cited 2020 Feb 20];86(1):21–5; quiz 180. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15640984. [DOI] [PubMed]
- 25.Cain EL, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med [Internet]. 2003 Jul 30 [cited 2019 Sep 22];31(4):621–35. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12860556. [DOI] [PubMed]
- 26.Shah CM, Calfee RP, Gelberman RH, Goldfarb CA. Outcomes of rigid night splinting and activity modification in the treatment of cubital tunnel syndrome. J Hand Surg Am. 2013;38(6):1125. doi: 10.1016/j.jhsa.2013.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ulnar nerve injury in the throwing athlete: Sports Medicine and Arthroscopy Review [Internet]. [cited 2020 Mar 4]. Available from: https://journals.lww.com/sportsmedarthro/fulltext/2003/11010/ulnar_nerve_injury_in_the_throwing_athlete.6.aspx
- 28.Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am [Internet]. 1986 Oct [cited 2019 Sep 26];68(8):1158–63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3771597. [PubMed]
- 29.Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med [Internet]. 1995 Jul 23 [cited 2019 Sep 26];23(4):407–13. Available from: https://doi-org.ezproxy.lib.utah.edu/10.1177/036354659502300406 [DOI] [PubMed]
- 30.Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med [Internet]. 2000 Jan 30 [cited 2019 Sep 26];28(1):16–23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10653538. [DOI] [PubMed]
- 31.Macnicol MF. The results of operation for ulnar neuritis. J Bone Joint Surg Br [Internet]. 1979 May [cited 2019 Sep 26];61-B(2):159–64. Available from: http://www.ncbi.nlm.nih.gov/pubmed/438266. [DOI] [PubMed]
- 32.Bartels RHMA, Menovsky T, Van Overbeeke JJ, Verhagen WIM. Surgical management of ulnar nerve compression at the elbow: an analysis of the literature. J Neurosurg [Internet]. 1998 Nov [cited 2019 Sep 26];89(5):722–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9817408. [DOI] [PubMed]
- 33.Manske PR, Johnston R, Pruitt DL, Strecker WB. Ulnar nerve decompression at the cubital tunnel. Clin Orthop Relat Res [Internet]. 1992 Jan [cited 2019 Sep 26];(274):231–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1309492. [PubMed]
- 34.Rayan GM. Proximal ulnar nerve compression. Cubital tunnel syndrome. Hand Clin [Internet]. 1992 May [cited 2019 Sep 26];8(2):325–36. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1613040. [PubMed]
- 35.Glousman RE. Ulnar nerve problems in the athlete’s elbow. Clin Sports Med [Internet]. 1990 Apr [cited 2019 Sep 26];9(2):365–77. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2183951. [PubMed]
- 36.Stuffer M, Jungwirth W, Hussl H, Schmutzhardt E. Subcutaneous or submuscular anterior transposition of the ulnar nerve? J Hand Surg Br [Internet]. 1992 Jun [cited 2019 Sep 26];17(3):248–50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1624852. [DOI] [PubMed]
- 37.Eaton RG, Crowe JF, Parkes JC. Anterior transposition of the ulnar nerve using a non-compressing fasciodermal sling. J Bone Joint Surg Am [Internet]. 1980 Jul [cited 2019 Sep 26];62(5):820–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/6248560. [PubMed]
- 38.Rettig AC, Ebben JR. Anterior subcutaneous transfer of the ulnar nerve in the athlete. Am J Sports Med [Internet]. 1993 Nov 23 [cited 2019 Sep 26];21(6):836–9; discussion 839-40. Available from: https://doi-org.ezproxy.lib.utah.edu/10.1177/036354659302100613 [DOI] [PubMed]
- 39.Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am [Internet]. 1992 Jan [cited 2019 Sep 27];74(1):67–83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1734015. [PubMed]
- 40.Jobe FW, Nuber G. Throwing injuries of the elbow. Clin Sports Med [Internet]. 1986 Oct [cited 2019 Sep 26];5(4):621–36. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3768968. [PubMed]


