Abstract
Purpose of Review
To provide a current review of the embryology, classification, evaluation, surgical management, and clinical outcomes related to preaxial polydactyly.
Recent Findings
Recent studies include a proposed embryologic link between preaxial polydactyly and other congenital abnormalities, an evaluation of long-term postsurgical outcomes, and an examination of important predictors for postsurgical outcomes.
Summary
Preaxial polydactyly, while relatively uncommon, is a complex congenital hand abnormality that requires careful preoperative classification and proper surgical intervention timing to yield optimal outcomes.
Keywords: Polydactyly, Radial, Preaxial, Thumb duplication, Split thumb, Congenital hand anomaly
Introduction
Although congenital hand and upper extremity differences are relatively rare, polydactyly of the hand is the most common congenital upper limb anomaly encountered by pediatricians and hand surgeons [1•]. While the overall prevalence of congenital upper limb anomalies is 22.0–27.2 per 10,000 live births, the New York Congenital Malformations Registry (NYCMR) database has estimated the prevalence of hand polydactyly to be 21.6 per 10,000 live births [1, 2]. Polydactyly is characterized by duplication, or partial splitting, of a digit during development and can present on the radial side of the hand (preaxial), in the center of the hand (central), or on the ulnar side of the hand (postaxial) (Fig. 1 a and b). The preaxial form is the second most common behind the postaxial form with a reported prevalence of approximately 0.8 to 2.3 in 10,000 live births [2–5]. Preaxial polydactyly (also known as radial polydactyly, thumb duplication, or split thumb) has a highly variable presentation and can present with duplication of phalangeal and metacarpal elements. The Wassel-Flatt classification system is the most commonly utilized system for distinguishing between the various presentations (Fig. 2) [4]. Prognosis, surgical approach, operative complications, and postsurgical outcomes can vary depending on type of preaxial polydactyly making it an important aspect of the evaluation process [6–8]. Recent investigations on preaxial polydactyly have focused on elucidating the etiology, updating classification techniques to provide more tailored surgical recommendations, and refining understanding of postoperative outcomes [9–11]. The review presented herein aims to provide an overview of preaxial polydactyly and to highlight these more recent scientific developments.
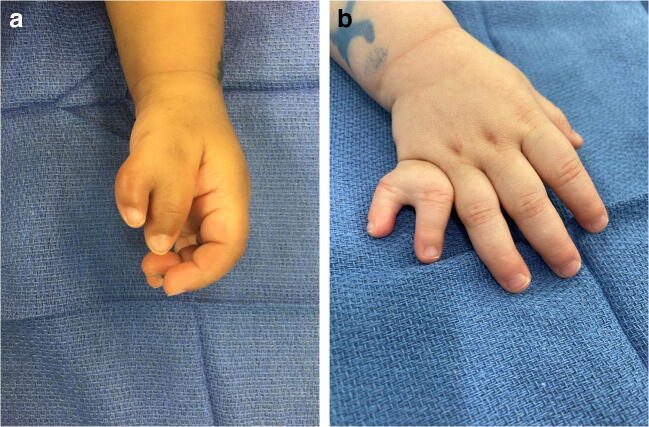
Fig. 1.
a Photograph demonstrating Wassel-Flatt type IV preaxial polydactyly in the left hand of a 16-month-old male. Note the divergence of the radial and ulnar thumbs at the metacarpophalangeal joint and the convergence at the interphalangeal joints. The radial thumb is notably smaller with poorly formed creases along the dorsal aspect of the interphalangeal joint suggesting more limited motion in comparison with the ulnar thumb. Observation of the child demonstrated preferential use of the ulnar thumb. b Photograph demonstrating postaxial polydactyly in the right hand of an 18-month-old female. In this case, the extra digit is well-formed, and there is a bony connection between the ulnar and radial small fingers. In the majority of postaxial polydactyly cases, the supernumerary digit contains primarily soft-tissue elements and is connected to the hand by a thin cutaneous bridge
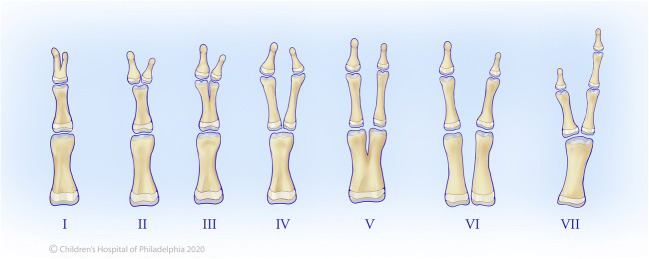
Fig. 2.
Illustration demonstrating the Wassel-Flatt classification system for preaxial polydactyly. Note that the Wassel-Flatt type VII thumb duplication is characterized by the presence of a triphalangeal thumb. (Used with permission from the Children’s Hospital of Philadelphia, copyright CHOP)
Genetics and Embryology
There are two major variations of thumb duplication, biphalangeal and triphalangeal thumb, both of which arise from aberrant sequence variations in the Sonic hedgehog (SHH) protein signaling pathway. Duplication of a biphalangeal thumb is more frequently unilateral, tends to arise sporadically, and is due to a developmental error leading to minor anterior SHH expression [12, 13]. Inherited biphalangeal preaxial polydactyly, while much less common, exhibits an autosomal dominant inheritance pattern with variable penetrance. Triphalangeal preaxial polydactyly, a variant where the thumb has an extra middle phalanx and an abnormally long and thin first metacarpal having epiphyses at both ends, usually presents symmetrically and bilaterally (Fig. 3). Unlike biphalangeal preaxial polydactyly, it is more commonly inherited, exhibits an autosomal dominant pattern with variable penetrance, and is usually related to point mutations leading to moderate gain of function of SHH [12, 13].
Fig. 3.
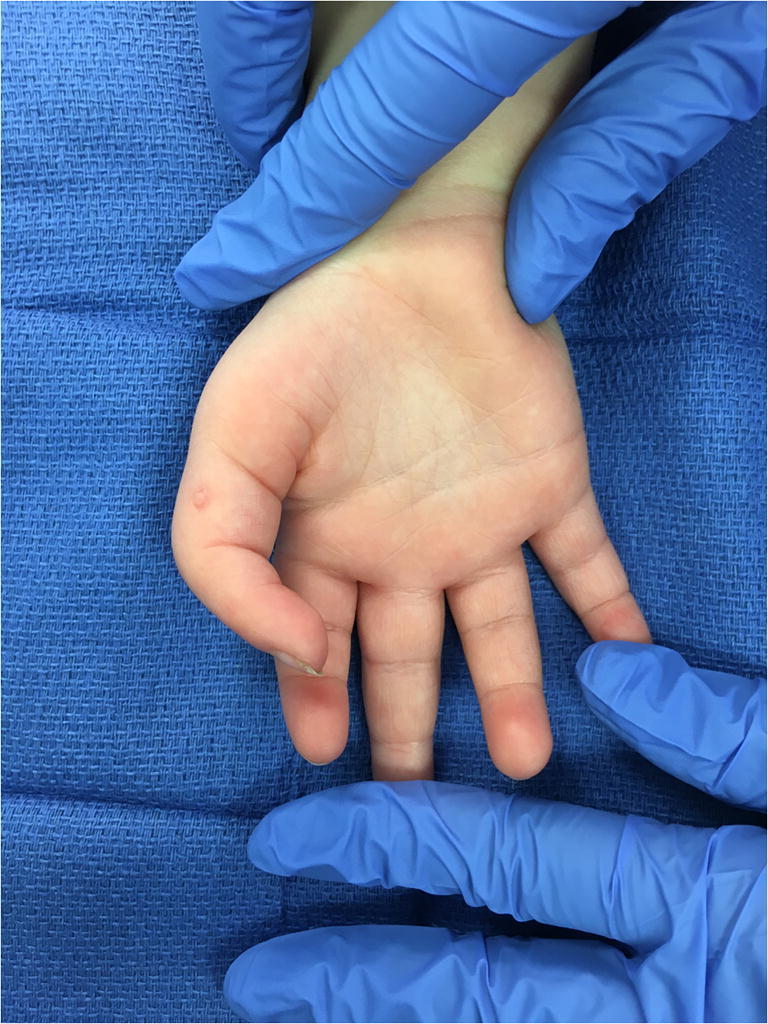
Photograph illustrating Wassel-Flatt type VII preaxial polydactyly in the right hand of an 18-month-old male. Note the abnormally long appearance of the thumb along with the presence of distinct proximal and distal interphalangeal joint creases suggestive of the extra middle phalanx
From an embryologic standpoint, the development of upper limb typically occurs between 4 and 8 weeks after fertilization, with the majority of congenital hand and upper extremity anomalies also arising during this sensitive growth period. Limb development progresses along a proximal-distal axis, an anterior-posterior (radio-ulnar) axis, and a dorsal-ventral via complex signaling molecular mechanisms, each of which work in concert to ensure proper formation and timing of development [6, 14, 15].
On a molecular level, preaxial polydactyly typically results from a failure of formation and lack of differentiation affecting the anterior-posterior development axis of the hand plate. This axis contains a specific signaling center known as the zone of polarizing activity (ZPA), which is located in the posterior aspect of the developing bud. The ZPA expresses the aforementioned SHH signaling protein, which plays a major role in determining radial-ulnar characteristics in the developing limb [6, 9, 16]. Ectopic SHH expression and disruption of its signaling pathway have been implicated in preaxial polydactyly as well as other congenital upper limb abnormalities [12, 17]. Recent literature has focused on a possible link between preaxial polydactyly and other limb anomalies such as radial aplasia and ulnar dimelia, given the integral role of SHH in the pathogenesis of all three anomalies. Results in a recent study conducted by Lam et al. suggest that the three conditions could be part of single spectrum involving aberrations in the SHH pathway and that both the timing and dose of SHH expression can be a major determinant in the development of preaxial polydactyly [9]. Previous studies have also suggested that preaxial polydactyly can be associated with other congenital anomalies such as acrocephalopolysyndactyly types I and II, Holt-Oram, Fanconi anemia, Rubinstein-Taybi, or Down syndrome [18, 19]. Thus, the embryologic origins of preaxial polydactyly continue to be an important area of study given that its etiology from a biomolecular standpoint is still being formally developed.
Anatomy and Classification
In broad terms, congenital limb abnormalities are typically classified using the Oberg, Manske, and Tonkin (OMT) system, which is subdivided based on malformations, deformations, and dysplasias [16, 20–22]. Preaxial polydactyly falls under the umbrella category of “malformations” given its status as an abnormal radioulnar axis formation/differentiation of the hand plate. Although categorized by the OMT, variations of preaxial polydactyly are more commonly described using the Wassel-Flatt classification, which provides a radiographic description based on the skeletal level of duplication from distally to proximally (Fig. 2) [4]. This classification system not only refers to the pathoanatomy of the duplication but also is well suited for guiding optimal surgical management [8, 19, 22]. The Wassel-Flatt system outlines the seven main types of preaxial polydactyly: types I–IV describing alterations of the phalanx, types V–VI describing alterations of the metacarpal, and triphalangism typically listed as type VII, which was added in a modified version of the classification system (Fig. 2) [23]. Additional subtypes of triphalangism have been categorized to describe more complex variations [24, 25]. The system can also be read according to classification number, as even numbers represent complete duplications and odd numbers represent bifid duplications. Type IV, which presents as a duplication of the proximal and distal phalanges that articulate with a broad metacarpal head, is the most common form occurring in 40% of patients (Fig. 1a) [7, 26, 27]. The Wassel-Flatt classification system is not without faults, as many studies have identified some potential shortcomings [10, 22, 23, 28–30]. Dijkman et al. noted that the Wassel-Flatt system lacked designations for complex osseous or soft tissue elements and advocated for the Rotterdam system as a potential alternative [30]. A more recent study by Evanson et al. suggests that the Chung classification system may more appropriately guide surgical approach and serve as a better predictor for reoperation rates given the significant association between Chung assignment and need for future revision [10, 29]. Despite these perceived deficiencies, however, the Wassel-Flatt system is almost universally used and remains both a vital foundation and important guide for many hand surgeons managing preaxial polydactyly.
Evaluation and Management
While each Wassel-Flatt type of thumb duplication can present with its own unique set of management obstacles, the evaluation and underlying surgical principles of preaxial polydactyly have significant overlap. Most patients are evaluated in infancy before the manifestation of functional limitations. A recent study by Cabrera Gonzalez et al. recommended surgical management between the ages of 7 and 12 months while reporting fewer complications in this time interval, though another by Comer et al. recommended intervention between the ages of 12 and 16 months given the added benefit of operating on larger digits, which tend to be technically easier to reconstruct [7, 8]. General consensus, however, among most authors is that approximately 12–18 months of age is an appropriate time point for surgical intervention given the diminished anesthetic risk, lack of functional pinch, and lack of awareness regarding esthetic appearance [7, 31]. Patient evaluation requires in-depth history, physical examination, and radiographs to assign classification and guide surgical planning. Imaging and subsequent classification assignment, in particular, are crucial given the strong association between Wassel-Flatt type and outcome prognosis [8, 31]. Three-dimensional ultrasound has been proposed as a potential aid in the evaluation process given its ability to observe possible underlying muscular and vascular abnormalities but is not first-line imaging and more suited for supplemental imaging [32].
The general methods of surgical correction for thumb duplication have been previously outlined by Tonkin, and their utilization is dictated by complexity, size, and location of the anatomical abnormality [22]. Studies on specific procedure type, surgical approach based on certain Wassel-Flatt classification types, and surgical techniques have been extensively described elsewhere [3, 33–39]. In brief, the primary goal of thumb reconstruction is to obtain stability, mobility, alignment, proper size, and proper shape. Minimization of scarring and nail deformity and optimizing esthetic appearance are also important considerations [8, 22]. The most common approach for management is excision of the less well-developed, hypoplastic digit with reconstruction of the retained thumb (Fig. 4–d). Of the two, the ulnar thumb is typically more functional and less angulated, resulting in ablation of the radial thumb and use of its soft tissue to enhance the function and appearance of the ulnar thumb. This also allows for preservation of the ulnar collateral ligament, which is vital for grip and pinch function [6, 7, 40]. When the duplication is symmetrical, a radial-sided flap with zigzag incisions is made with care to preserve the origin of the radial collateral ligament from the thumb metacarpal. The radial collateral ligament is sutured to the proximal phalangeal base of the ulnar thumb to reconstruct the deficient collateral ligament. Reconstruction of the ulnar thumb may also require extensor tendon transfer or realignment, flexor tendon transfer, and/or preservation and reattachment of the thumb intrinsic musculature. Extra-articular malalignment requires additional corrective osteotomy with either a closing or an opening-wedge osteotomy and K-wire stabilization. The Bilhaut-Cloquet produce can be utilized for nonsymmetrical duplications when there is minimal thumb size mismatch, particularly in Wassel-Flatt types I–IV. This procedure entails resection of the central portions in the duplicated digits and closure of the retained peripheral portions of the digits to form a single thumb [41]. In cases when one thumb is better developed proximally, while the other thumb is better developed distally, an on-the-top plasty may be used to combine the two portions into one digit. Preserving the neurovasculature function of the distal segment requires immense precision given the risk of vascular compromise with this procedure. These procedures and specific associated modifications are further described in depth elsewhere [6, 8, 34–36, 38]. Following surgical reconstruction, in most cases, a long-arm thumb spica cast is applied for approximately 4 weeks.
Fig. 4.
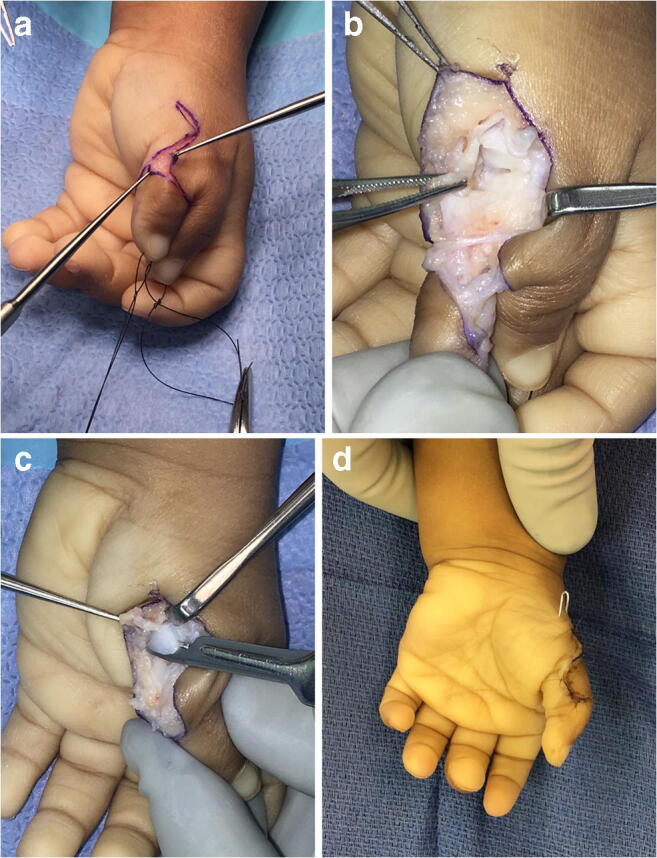
Photographs demonstrating the reconstruction of a Wassel-Flatt type IV preaxial polydactyly in the left hand of a 16-month-old male pictured in Fig. 1a. a Zigzag surgical incision along the radial border of the ulnar thumb is used to optimize visualization during surgery while minimizing postoperative scarring. b The radial collateral ligament is detached from the proximal phalanx of the radial thumb (held in this photograph with tissue forceps at the nine o’clock position) with a strip of periosteum and is preserved for reattachment to the proximal phalanx of the ulnar thumb. c The metacarpal head is shaved down with #15 blade to reduce the abnormal breadth of the metacarpal head while preserving the origin of the radial collateral ligament. d A Kirschner wire is used to stabilize the metacarpophalangeal joint for 4 weeks, and the skin flaps are closed with absorbable suture
Rehabilitation
The role of postoperative hand therapy is determined by the complexity of the specific duplication and surgical reconstruction as well as the baseline functional status of the child. Following cast and pin removal, patients are referred to occupational therapy for fabrication of a custom forearm-based thumb spica splint with the interphalangeal joint included to ensure proper alignment of the joints and to maintain the web space depth (Fig. 5). The splint is worn full time for 4–8 weeks depending on the complexity of reconstruction with removal for range of motion exercises and supervised light functional hand use as appropriate [42]. Caregiver education on hand washing, surgical scar care, edema management, and desensitization are also initiated at this time. Scar management techniques can begin when there is sufficient healing of the surgical incision.
Fig. 5.

Photograph demonstrating a custom forearm-based thumb spica splint with the interphalangeal joint included to ensure proper alignment of the joints and to maintain the web space depth
In a simple reconstruction that did not require bony osteotomy or ligament reconstruction, patients can begin active motion following dressing removal 10–14 days postoperatively within comfort. In more complex reconstruction, gentle active joint motion of the thumb can begin once sufficient bony union under the supervision of a hand therapist, approximately 4 weeks postoperative [6]. Active motion can progress to incorporating supervised light functional thumb use for grasp and pinch as tolerated [42]. Encouragement of a lateral pinch, pad to pad pinch, palmar pinch, and cylindrical grasp with opposition should be facilitated throughout play-based activities. Gentle passive thumb interphalangeal and metacarpophalangeal motion can generally be initiated at 6 weeks as tolerated. Progressive strengthening activities can be initiated as needed after 8 weeks, once the child demonstrates comfortable active motion of the reconstructed thumb targeting functional grasp and pinch patterns.
Outcomes
The results following surgery and thumb reconstruction tend to be favorable but can vary based on complexity of the thumb duplication. Preoperative Wassel-Flatt type designation tends to be an important prognostic indicator for postsurgical outcome. Generally, outcomes for Wassel-Flatt types I, II, and IV thumb duplications are better than those for Wassel-Flatt types III, V, and VI based on inherent differences in the nature of the duplication [31]. In corroboration with an earlier study conducted by Cabrera Gonzalez et al., a more recent study by de Almeida et al. suggests that age at operation, in addition to Wassel-Flatt type, is also an important prognostic factor for postoperative outcome. Short- and long-term functional and esthetic outcomes for preaxial polydactyly are well described in the medical literature [8, 11, 26, 28, 38, 43–47]. These studies have examined both the objective outcomes, including range of motion, joint stability, thumb alignment, grip strength, and pinch strength, as well as subjective esthetic outcome. The Tada score a point-based criteria grading system developed by Tada et al. assigns points based on various objective functional outcomes and is also a frequently recorded metric in outcome studies [28].
A recent study by Gholson et al. reported favorable long-term clinical and radiologic outcomes as demonstrated clinically by strength testing and verified clinical outcome measurements including the Disabilities of the Arm, Shoulder, and Hand Outcome (DASH) and Patient-Reported Outcomes Measurement Information System (PROMIS) for the upper extremity as well as radiographically to determine the presence of arthritis [48•]. A study population of preaxial polydactyly patients with a median follow-up of 36 years was found to have mean DASH (3.7 vs. 10.1) and PROMIS scores (51.5 vs. 50) that were comparable with the general population. Despite limited thumb range of motion, the patients in this series demonstrated mean pinch strength, side pinch strength, and overall grip strength comparable with the contralateral side. Joint arthritis was found in only 15% of participants, but 46% of patients had angular deformity [48•]. Although postoperative outcomes are typically positive, some studies have highlighted less favorable results in the postoperative period. A recent study by Goldfarb et al. suggested that dissatisfaction with cosmetic appearance after reconstruction was associated with residual angulation and reduced nail width, which can be common complications during preaxial polydactyly reconstruction [26]. In more recent literature, a study by de Almeida et al. reported a strong association between negative functional outcomes and unfavorable cosmetic appearance as well as residual deformity, the incidence of which increases with increasing complexity of duplication [11•]. Regarding long-term postoperative complications, Stutz et al. noted that 19% of the 41 patients evaluated in his study required re-operation, citing the instability and pain as the most frequent causes for revision [46].
Author’s Experience
Given the possibility of postoperative dissatisfaction due to angular deformity or instability, precise surgical technique is paramount. The surgeon must take care to preserve and reconstruct the radial collateral ligament at the time of the index procedure. In addition, a corrective osteotomy of the proximal phalangeal neck is often required to avoid a postoperative angular deformity. By adhering to these principles, the surgeon can minimize the potential need for revision surgery.
Conclusion
Preaxial polydactyly is a congenital hand abnormality with complex embryologic origin that presents in infancy with varying complexity and requires both careful preoperative evaluation and surgical reconstruction. Timing and approach of surgery often yield favorable functional and esthetic outcomes, but need for reoperation and postoperative complications may occur especially with thumb duplications of increasing structural complexity.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Pediatric Orthopedics
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Benjamin H. Rogers, Email: bhr003@jefferson.edu
Sandra L. Schmieg, schmieg@email.chop.edu
Meagan E. Pehnke, pehnkem@email.chop.edu
Apurva S. Shah, shaha6@email.chop.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Goldfarb CA, Shaw N, Steffen JA, Wall LB. The prevalence of congenital hand and upper extremity anomalies based upon the New York congenital malformations registry. J Pediatr Orthop. 2017;37(2):144–148. doi: 10.1097/BPO.0000000000000748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marks TW, Bayne LG. Polydactyly of the thumb: abnormal anatomy and treatment. J Hand Surg Am. 1978;3(2):107–116. doi: 10.1016/s0363-5023(78)80057-4. [DOI] [PubMed] [Google Scholar]
- 3.Wall LB, Goldfarb CA. Reconstruction for type IV radial polydactyly. J Hand Surg Am. 2015;40(9):1873–1876. doi: 10.1016/j.jhsa.2015.06.097. [DOI] [PubMed] [Google Scholar]
- 4.Wassel HD. The results of surgery for polydactyly of the thumb. A review. Clin Orthop Relat Res. 1969;64:175–193. [PubMed] [Google Scholar]
- 5.Ekblom AG, Laurell T, Arner M. Epidemiology of congenital upper limb anomalies in 562 children born in 1997 to 2007: a total population study from Stockholm, Sweden. J Hand Surg Am. 2010;35(11):1742–1754. doi: 10.1016/j.jhsa.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Little KJ, Cornwall R. Congenital anomalies of the hand--principles of management. Orthop Clin North Am. 2016;47(1):153–168. doi: 10.1016/j.ocl.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 7.Comer GC, Potter M, Ladd AL. Polydactyly of the hand. J Am Acad Orthop Surg. 2018;26(3):75–82. doi: 10.5435/JAAOS-D-16-00139. [DOI] [PubMed] [Google Scholar]
- 8.Cabrera González M, Pérez López LM, Martínez Soto G, Gutiérrez de la Iglesia D. Prognostic value of age and Wassel classification in the reconstruction of thumb duplication. J Child Orthop. 2013;7(6):551–557. doi: 10.1007/s11832-013-0534-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.• Lam WL, Oh JDH, Johnson EJ, Pertinez SP, Stephens C, Davey MG. Experimental evidence that preaxial polydactyly and forearm radial deficiencies may share a common developmental origin. J Hand Surg Eur Vol. 2018;1753193418762959 Experimentally induced preaxial polydactyly in animal models highlighting key aberrations during embryogenesis and molecular pathways that lead to its development. [DOI] [PubMed]
- 10.Evanson BJ, Hosseinzadeh P, Riley SA, Burgess RC. Radial polydactyly and the incidence of reoperation using a new classification system. J Pediatr Orthop. 2016;36(2):158–160. doi: 10.1097/BPO.0000000000000395. [DOI] [PubMed] [Google Scholar]
- 11.de Almeida CEF. Analysis of surgical results and of residual postoperative deformities in preaxial polydactyly of the hand. J Plast Reconstr Aesthet Surg. 2017;70(10):1420–1432. doi: 10.1016/j.bjps.2017.05.031. [DOI] [PubMed] [Google Scholar]
- 12.Al-Qattan MM, Kozin SH. Update on embryology of the upper limb. J Hand Surg Am. 2013;38(9):1835–1844. doi: 10.1016/j.jhsa.2013.03.018. [DOI] [PubMed] [Google Scholar]
- 13.Umair M, Ahmad F, Bilal M, Ahmad W, Alfadhel M. Clinical genetics of polydactyly: an updated review. Front Genet. 2018;9:447. doi: 10.3389/fgene.2018.00447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dy CJ, Swarup I, Daluiski A. Embryology, diagnosis, and evaluation of congenital hand anomalies. Curr Rev Musculoskelet Med. 2014;7(1):60–67. doi: 10.1007/s12178-014-9201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yasuda M. Pathogenesis of preaxial polydactyly of the hand in human embryos. J Embryol Exp Morphol. 1975;33(3):745–756. [PubMed] [Google Scholar]
- 16.Tonkin MA, Oberg KC. The OMT classification of congenital anomalies of the hand and upper limb. Hand Surg. 2015;20(3):336–342. doi: 10.1142/S0218810415400055. [DOI] [PubMed] [Google Scholar]
- 17.Lettice LA, Heaney SJ, Purdie LA, Li L, de Beer P, Oostra BA, Goode D, Elgar G, Hill RE, de Graaff E. A long-range Shh enhancer regulates expression in the developing limb and fin and is associated with preaxial polydactyly. Hum Mol Genet. 2003;12(14):1725–1735. doi: 10.1093/hmg/ddg180. [DOI] [PubMed] [Google Scholar]
- 18.Wilks DJ, Kay SP, Bourke G. Fanconi’s anaemia and unilateral thumb polydactyly--don’t miss it. J Plast Reconstr Aesthet Surg. 2012;65(8):1083–1086. doi: 10.1016/j.bjps.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 19.Dobyns JH, Lipscomb PR, Cooney WP. Management of thumb duplication. Clin Orthop Relat Res. 1985;195:26–44. [PubMed] [Google Scholar]
- 20.Bae DS, Canizares MF, Miller PE, Roberts S, Vuillermin C, Wall LB, Waters PM, Goldfarb CA. Intraobserver and interobserver reliability of the Oberg-Manske-Tonkin (OMT) classification: establishing a registry on congenital upper limb differences. J Pediatr Orthop. 2018;38(1):69–74. doi: 10.1097/BPO.0000000000000732. [DOI] [PubMed] [Google Scholar]
- 21.Baas M, Zwanenburg PR, Hovius SER, van Nieuwenhoven CA. Documenting combined congenital upper limb anomalies using the Oberg, Manske, and Tonkin classification: implications for epidemiological research and outcome comparisons. J Hand Surg Am. 2018;43:869.e1–869.e11. doi: 10.1016/j.jhsa.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Tonkin MA. Thumb duplication: concepts and techniques. Clin Orthop Surg. 2012;4(1):1–17. doi: 10.4055/cios.2012.4.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zuidam JM, Selles RW, Ananta M, Runia J, Hovius SE. A classification system of radial polydactyly: inclusion of triphalangeal thumb and triplication. J Hand Surg Am. 2008;33(3):373–377. doi: 10.1016/j.jhsa.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 24.Wood VE. Polydactyly and the triphalangeal thumb. J Hand Surg Am. 1978;3(5):436–444. doi: 10.1016/s0363-5023(78)80136-1. [DOI] [PubMed] [Google Scholar]
- 25.Miura T. Triphalangeal thumb. Plast Reconstr Surg. 1976;58(5):587–594. doi: 10.1097/00006534-197611000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Goldfarb CA, Patterson JM, Maender A, Manske PR. Thumb size and appearance following reconstruction of radial polydactyly. J Hand Surg Am. 2008;33(8):1348–1353. doi: 10.1016/j.jhsa.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 27.Mete BD, Altay C, Gursoy M, Oyar O. Wassel’s type V polydactyly with plain radiographic and CT findings. J Clin Imaging Sci. 2015;5:16. doi: 10.4103/2156-7514.153974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tada K, Yonenobu K, Tsuyuguchi Y, Kawai H, Egawa T. Duplication of the thumb. A retrospective review of two hundred and thirty-seven cases. J Bone Joint Surg Am. 1983;65(5):584–598. [PubMed] [Google Scholar]
- 29.Chung MS, Baek GH, Gong HS, Lee HJ, Kim J, Rhee SH. Radial polydactyly: proposal for a new classification system based on the 159 duplicated thumbs. J Pediatr Orthop. 2013;33(2):190–196. doi: 10.1097/BPO.0b013e3182648ca8. [DOI] [PubMed] [Google Scholar]
- 30.Dijkman RR, van Nieuwenhoven CA, Selles RW, Habenicht R, Hovius SE. A multicenter comparative study of two classification systems for radial polydactyly. Plast Reconstr Surg. 2014;134(5):991–1001. doi: 10.1097/PRS.0000000000000590. [DOI] [PubMed] [Google Scholar]
- 31.Kozin SH, Zlotolow DA. Common pediatric congenital conditions of the hand. Plast Reconstr Surg. 2015;136(2):241e–257e. doi: 10.1097/PRS.0000000000001499. [DOI] [PubMed] [Google Scholar]
- 32.Saito S, Ueda M, Takahashi N, Kawakatsu M, Suzuki S. Three-dimensional ultrasonography for visualization of muscular anomalies in type VI and VII radial polydactyly. Skelet Radiol. 2016;45(4):541–547. doi: 10.1007/s00256-015-2271-9. [DOI] [PubMed] [Google Scholar]
- 33.Al-Qattan MM, Kattan AE, Al-Lazzam A, Gelidan AG. A modified Bilhaut-Cloquet procedure for zigzag thumb polydactyly types III and IV. Plast Reconstr Surg Glob Open. 2017;5(12):e1589. doi: 10.1097/GOX.0000000000001589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Qattan NM, Al-Qattan MM. On-top and side-to-side plasties for thumb polydactyly. Int J Surg Case Rep. 2017;39:88–92. doi: 10.1016/j.ijscr.2017.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tonkin MA, Bulstrode NW. The Bilhaut-Cloquet procedure for Wassel types III, IV and VII thumb duplication. J Hand Surg Eur Vol. 2007;32(6):684–693. doi: 10.1016/J.JHSE.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 36.Baek GH, Gong HS, Chung MS, Oh JH, Lee YH, Lee SK. Modified Bilhaut-Cloquet procedure for Wassel type-II and III polydactyly of the thumb. Surgical technique. J Bone Joint Surg Am. 2008;90(Suppl 2 Pt 1):74–86. doi: 10.2106/JBJS.G.01104. [DOI] [PubMed] [Google Scholar]
- 37.Horii E, Hattori T, Koh S, Majima M. Reconstruction for Wassel type III radial polydactyly with two digits equal in size. J Hand Surg Am. 2009;34(10):1802–1807. doi: 10.1016/j.jhsa.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 38.Bell B, Butler L, Mills J, Stutz C, Ezaki M, Oishi S. “On-top plasty” for radial polydactyly reconstruction. J Hand Surg Am. 2017;42(9):753.e751–753.e756. doi: 10.1016/j.jhsa.2017.05.029. [DOI] [PubMed] [Google Scholar]
- 39.Dijkman RR, Selles RW, Hülsemann W, Mann M, Habenicht R, Hovius SER, van Nieuwenhoven CA. A matched comparative study of the Bilhaut procedure versus resection and reconstruction for treatment of radial polydactyly types II and IV. J Hand Surg Am. 2016;41(5):e73–e83. doi: 10.1016/j.jhsa.2015.12.030. [DOI] [PubMed] [Google Scholar]
- 40.Siqueira MA, Sterodimas A, Boriani F, Pitanguy I. A 10-year experience with the surgical treatment of radial polydactyly. Ann Ital Chir. 2008;79(6):441–444. [PubMed] [Google Scholar]
- 41.Samson P, Salazard B, Magalon G. The “Bilhaut-Cloquet” technique for treatment of thumb duplication. Handchir Mikrochir Plast Chir. 2004;36(2–3):141–145. doi: 10.1055/s-2004-817888. [DOI] [PubMed] [Google Scholar]
- 42.Dorich JM, Shotwell C. Orthotics and Casting. In: Abzug JM, Kozin SH, Zlotolow DA, editors. The Pediatric Upper Extremity. New York: Springer; 2015. [Google Scholar]
- 43.Ogino T, Ishii S, Takahata S, Kato H. Long-term results of surgical treatment of thumb polydactyly. J Hand Surg Am. 1996;21(3):478–486. doi: 10.1016/S0363-5023(96)80366-2. [DOI] [PubMed] [Google Scholar]
- 44.Larsen M, Nicolai JP. Long-term follow-up of surgical treatment for thumb duplication. J Hand Surg Br. 2005;30(3):276–281. doi: 10.1016/j.jhsb.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 45.Kemnitz S, De SL. Pre-axial polydactyly: outcome of the surgical treatment. J Pediatr Orthop B. 2002;11(1):79–84. doi: 10.1097/00009957-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 46.Stutz C, Mills J, Wheeler L, Ezaki M, Oishi S. Long-term outcomes following radial polydactyly reconstruction. J Hand Surg Am. 2014;39(8):1549–1552. doi: 10.1016/j.jhsa.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 47.Maillet M, Fron D, Martinot-Duquennoy V, Herbaux B. Results after surgical treatment of thumb duplication: a retrospective review of 33 thumbs. J Child Orthop. 2007;1(2):135–141. doi: 10.1007/s11832-007-0019-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gholson JJ, Shah AS, Buckwalter JA. Long-term clinical and radiographic follow-up of preaxial polydactyly reconstruction. J Hand Surg Am. 2019;44(3):244.e241–244.e246. doi: 10.1016/j.jhsa.2018.05.030. [DOI] [PubMed] [Google Scholar]