Abstract
BACKGROUND
There is little evidence of combining sorafenib with hepatic arterial infusion chemotherapy (HAIC) after transarterial chemoembolization (TACE) for intermediate and advanced hepatocellular carcinoma (HCC). It is important to identify that patients with intermediate and advanced HCC are most likely to benefit from this combination therapy.
AIM
To investigate the safety and clinical outcomes of sorafenib combined with HAIC with folinic acid, 5-fluorouracil (5-FU), and oxaliplatin (FOLFOX) after TACE for intermediate and advanced HCC.
METHODS
This prospective phase II study enrolled patients with intermediate and advanced HCC who underwent treatment with sorafenib combined with TACE-HAIC. All patients initially received the standard 400 mg dose of sorafenib twice daily before TACE-HAIC. Participants at our institute with intermediate and advanced HCC underwent routine TACE. Then, the catheter used for embolization was kept in place in the hepatic artery, and oxaliplatin was intra-arterially administered for 6 h, followed by 5-FU for 18 h, and folinic acid was intravenously administered for 2 h. The primary endpoints were safety, as evaluated by the Common Terminology and Criteria for Adverse Events version 4.0, and 12-mo progression-free survival (PFS), as analyzed by the Kaplan-Meier method. As secondary endpoints, the objective response rate (ORR) was evaluated by the modified Response Evaluation Criteria for Solid Tumors, and survival time [overall survival (OS)] was analyzed by the Kaplan-Meier method.
RESULTS
Sixty-six participants at our institute with intermediate and advanced HCC were enrolled in this prospective study (mean age, 53.3 ± 11.7 years). Approximately 56.1% of participants had Barcelona Clinic Liver Cancer (BCLC) stage C disease, and 43.9% had BCLC stage B disease. The ORR was 42.4%. The disease control rate was 87.9%. The grade 3-4 toxicities consisted of thrombocytopenia (4.5%), neutropenia (3.0%), and elevated aspartate aminotransferase (12.2%). Hand-foot skin reaction was also observed (40.9%). The median PFS was 13.1 mo (13.5 mo in the BCLC stage B participants and 9.4 mo in the BCLC stage C participants). The 6-mo, 12-mo, and 24-mo PFS rates were 75.0%, 54.7%, and 30.0%, respectively. The median OS was 21.8 mo.
CONCLUSION
Sorafenib combined with HAIC (FOLFOX) after TACE may be a feasible treatment choice for intermediate and advanced HCC because this treatment met the prespecified endpoint of a 6-mo PFS rate exceeding 50% and had good patient tolerance. Prospective randomized controlled trials are needed to confirm the effect of this combination therapy.
Keywords: Hepatocellular carcinoma, Transcatheter arterial chemoembolization, Hepatic arterial infusion chemotherapy, Oxaliplatin, Fluorouracil, Sorafenib
Core tip: Both hepatic arterial infusion chemotherapy (HAIC) and sorafenib plus transcatheter arterial chemoembolization (TACE) combination therapy are widely used as a treatment of choice in patients with hepatocellular carcinoma (HCC) in Asia. However, the safety and efficacy of sorafenib combined with HAIC (folinic acid, 5-fluorouracil, and oxaliplatin) after TACE for intermediate and advanced HCC have not been firmly established. In the present study, we confirmed the efficacy and safety of this combination therapy. We believe that this study can help doctors and patients to select appropriate therapy.
INTRODUCTION
Hepatocellular carcinoma (HCC) is the sixth most common malignancy and the fourth leading cause of cancer-related death worldwide[1]. However, 70%-80% of patients with HCC are diagnosed at an advanced stage and are ineligible for curative therapies[2]. New locoregional modalities, including radiofrequency ablation (RFA) and arterially directed therapy, can improve the prognosis of patients with HCC[3]. The Asia-Pacific clinical practice guidelines[4] on the management of HCC recommend transcatheter arterial chemoembolization (TACE) as a first-line treatment for HCC in patients with unresectable, large/multifocal HCCs who do not have vascular invasion or extrahepatic spread. TACE is associated with a longer overall survival (OS) than systemic chemotherapy and is associated with fewer adverse events (AEs)[5-7]. However, TACE has unclear effects on patients with large HCCs (tumor diameter greater than 10 cm) and those with vascular invasion [portal vein tumor thrombosis (PVTT) and vascular infiltration]. In previous studies[8-11], hepatic arterial infusion chemotherapy (HAIC) is a recommended treatment for advanced HCC with portal vein invasion and for large HCC. HAIC can directly deliver chemotherapeutic drugs to the tumor-supplying artery to increase drug concentration and reduce the toxicity of systemic chemotherapy. HAIC is recommended for HCC in Japan and China[12,13], and in Western countries, some studies[14,15] have reported the safety and efficacy of HAIC for HCC. Oxaliplatin and 5-fluorouracil (5-FU) infused via the hepatic artery have been proven to be safe in phase I clinical studies and pharmacokinetic analyses[16,17].
Recent studies focusing on TACE in combination with other interventional therapies for HCC have shown that treatments such as RFA, microwave ablation, sorafenib, and HAIC are safe and effective and show promising outcomes[18-22]. A prospective phase II trial[21] revealed that TACE combined with HAIC was superior to TACE alone for inoperable HCC. The objective response rate (ORR) in the TACE-HAIC treatment group was higher than that in the TACE-only group (68.9% vs 45.9%), and the median progression-free survival (mPFS) in the TACE-HAIC group was significantly better than that in the TACE-only group (8.0 mo vs 4.5 mo) among patients with inoperable HCC.
Sorafenib is the most widely used systemic therapy approved as a first-line agent for unresectable or advanced HCC[23]. In two randomized, double-blind phase III trials[24,25], sorafenib was effective and well tolerated for the treatment of advanced HCC. Sorafenib can inhibit tumor revascularization and reduce the recurrence and metastasis of tumors[26-29]. The efficacy of sorafenib combined with TACE is conflicting in some trials (SPACE, TACE-2, and TACTICS). However, the TACTICS and OPTIMIS trials found that sorafenib combined with TACE benefited PFS (TACTICS) and OS (OPTIMIS), respectively, and the timing of sorafenib was crucial in these studies. The TACTICS trial was well-designed for evaluating the timing of sorafenib and creating a new definition of disease progression[29-31]. In the START trial[32,33], sorafenib in combination with TACE, especially the combination that improved the OS of early-intermediate-stage HCC, was found to be a safe and effective therapy for patients with advanced-stage HCC.
In previous studies, sorafenib exerted a synergistic anticancer effect with chemotherapeutic agents[34]. Some studies[35,36] have shown that sorafenib combined with HAIC [folinic acid, 5-FU, and oxaliplatin (FOLFOX)] can effectively reduce the tumor burden of HCC with portal vein invasion. In a randomized, multicenter phase III trial[36], the median OS of the group treated with sorafenib plus HAIC (FOLFOX) was longer than that of the HAIC-only group (13.37 mo vs 7.13 mo). In addition, the sorafenib group showed a higher response rate (51% vs 3%) and had a longer median PFS (7.03 mo vs 2.6 mo) than the HAIC-only group.
As TACE is the most widely used treatment for intermediate and advanced HCC, sorafenib combined with TACE is considered a safe and effective therapy for patients with advanced-stage HCC, and sorafenib combined with HAIC is recommended for HCC with portal vein invasion. However, few reports have examined the effect of sorafenib combined with TACE-HAIC for intermediate and advanced HCC. Thus, we evaluated the safety and efficacy of a combined therapeutic strategy with sorafenib and TACE-HAIC in patients with advanced HCC.
MATERIALS AND METHODS
Participant eligibility
All participants were diagnosed by pathology or the American Association for the Study of Liver Disease criteria[37]. All participants satisfied the following criteria: (1) Age 18-75 years; (2) Eastern Cooperative Oncology Group performance status 0-2; (3) Child-Pugh class A or B7; (4) Intermediate and advanced HCC (including patients with extrahepatic metastasis and portal vein invasion); (5) White blood cell count > 3 × 109/L and neutrophil count > 1.5 × 109/L; (6) Serum creatinine < 2 mg/dL and albumin level > 3.0 mg/dL; and (7) Left ventricular ejection fraction > 45%. The exclusion criteria were as follows: (1) Other malignancies; (2) Uncontrollable infections (> grade 2 infections; infections that required antibiotic or surgical interventions or were life-threatening; (3) Pregnancy or breastfeeding; (4) Previous sorafenib treatment; and (5) Severe allergies to contrast agents or other drugs.
Study design
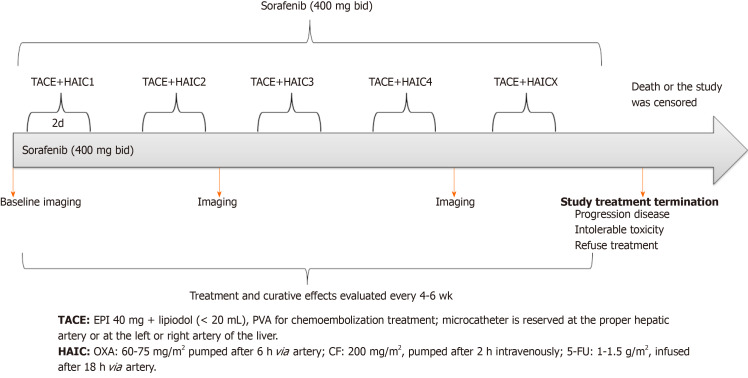
All participants received sorafenib and underwent TACE-HAIC (FOLFOX). Patients were treated on a 4- to 6-wk cycle regimen, in which one cycle consisted of sorafenib 400 mg twice daily, and then TACE-HAIC was performed on days 1-2. Sorafenib was continued with TACE-HAIC intervention. Sorafenib and TACE-HAIC were continued until progressive disease (PD) (If there was a new tumor node > 5 mm, this was considered the first instance of PD, and treatment was continued until PD was identified twice. Then, the patient was excluded from the study. The PFS was recorded from the first instance of PD), intolerable toxicity, or death. The tumor response was evaluated after every two cycles of treatment and every 3 mo during maintenance treatment [contrast-enhanced magnetic resonance imaging (MRI) or computed tomography (CT)]. The tumor response was evaluated by the modified Response Evaluation Criteria for Solid Tumors (mRECIST). We tried to keep the imaging examination (CT or MRI) consistent before and after treatment to increase accuracy, and two experienced radiologists with 11 and 12 years of experience in abdominal imaging determined the tumor responses by consensus. The criteria for terminating treatment and the TACE-HAIC scheme are shown in Figure 1.
Figure 1.
Scheme of transcatheter arterial chemoembolization-hepatic arterial infusion chemotherapy and sorafenib. TACE: Transcatheter arterial chemoembolization; HAIC: Hepatic arterial infusion chemotherapy; 5-FU: 5-fluorouracil; PVA: Polyvinyl alcohol; CF: Calcium folinate; EPI: Epirubicin; OXA: Oxaliplatin.
Procedures
TACE technique: The Seldinger technique was used to access the femoral artery after injection of local anesthesia. Arteriography was performed to gather information regarding the abdominal aorta, celiac trunk, and portal venous system before chemoembolization treatments for all participants. A 2.7-F microcatheter (Renegade Hi Flo, Boston Scientific, United States; Stride ASAHI INTECC, Japan) was coaxially advanced through an external catheter to select the tumor arteries. Subsequently, lipiodol (total volume < 20 mL; lipiodol, Laboratoire Andre Guerbet, Aulnaysous-Bois, France) mixed with 20-40 mg of emulsified epirubicin (Main Luck Pharmaceutical, Shenzhen, China) was injected to embolize the tumor arteries; for some large tumors, 100-300 µm/300-500 µm embospheres (Biosphere Medical, Rockland, MA, United States) were used for embolization. Chemoembolization was performed first if there were extrahepatic parasitic blood arteries. In patients with an arterioportal shunt, embolization with 350-1000 μm of gelatin sponge particles was performed to occlude the shunt via super-selective catheterization before infusion of lipiodol. A temporary indwelling catheter was inserted into the feeding artery of the tumor until the end of HAIC. If there were bilobar HCC tumors with a low tumor burden, conventional TACE (cTACE) was performed for both tumors, and the tip of catheter was inserted into the proper hepatic artery or common hepatic artery. If there were bilobar HCC tumors with a high tumor burden, embolization of tumor was performed in steps to reduce the risk of hepatic failure. The position of the catheter was determined according to the tumor location.
HAIC technique: A microcatheter was externally connected to an arterial infusion pump (Model LP 2000-P2) in the ward, and oxaliplatin [60-75 mg/m2 (Child-Pugh A, 75 mg/m2 and Child-Pugh B, 60 mg/m2)] was administered intra-arterially for 6 h; leucovorin 200 mg/m2 was intravenously administered for 2 h (the peripheral vein for 2 h at the beginning of the 5-FU infusion), and 5-FU [1.0-1.5 g/m2 (Child-Pugh A, 1.5 g/m2 and Child-Pugh B, 1 g/m2)] was intra-arterially administered for 18 h). At the end of the procedure, we extracted the arterial catheter and put pressure on the puncture point for 24 h. TACE-HAIC was performed every 4-6 wk. A maximum of eight consecutive cycles of HAIC were used for patients without disease progression during the treatments. All doctors had more than 10 years of experience in interventional oncology.
Sorafenib: Before the treatment, sorafenib (200 mg) was administered orally twice daily; 400 mg was administered orally twice daily if the drug tolerance was acceptable. The dose of sorafenib was reduced (600 mg or 400 mg orally per day) based on treatment-related toxicities. Treatment was discontinued because of disease progression, unacceptable toxicity, or treatment refusal.
Assessments
All participants had their complete medical histories taken, and abdominal contrast-enhanced CT or MRI and chest X-ray and/or CT were performed during the baseline physical examination. Enhanced CT or MRI were performed after each cycle of therapy, and laboratory tests [blood examinations, biochemical tests, coagulation testing, and measurement of serum alpha-fetoprotein (AFP) levels] were performed before each cycle of therapy; AEs were evaluated using the Common Terminology Criteria for Adverse Events (CTCAE) v4.03. Participants were followed until death or until they were lost to follow-up. Tumor response was defined as complete response (CR), partial response (PR), or stable disease (SD). Tumor control was defined as a CR, PR, or SD (evaluated using mRECIST). It should be noted that CR was defined as a tumor disappearing on contrast-enhanced CT and/or MRI combined with a normalized AFP level. All tumors (liver tumors, lymph node metastases, or metastatic tumors) were evaluated using mRECIST.
If the patients demonstrated stable conditions with a CR, sorafenib was continued, and TACE-HAIC treatment was stopped. AFP levels were reevaluated every 3 mo, and contrast-enhanced MRI or CT evaluations were conducted. Once liver tumors were classified as PD, sorafenib and TACE-HAIC were stopped, and patients underwent other therapy or were followed for survival. When a participant suffered an intolerable toxicity, treatment was suspended, and the drug dose was adjusted. If the patient still could not tolerate treatment, the treatment was discontinued.
Statistical analysis
The primary endpoints were safety and PFS. PFS was defined as the time from the date of the first TACE-HAIC treatment until disease progression. The null hypothesis of a 12-mo PFS rate of approximately 30% was based on the results of a clinical trial recently completed in our department with the same TACE-HAIC regimen[21]. This hypothesis was tested against the alternative hypothesis of a true rate of 50% or higher. To evaluate this hypothesis with 90% power and an alpha level of 0.05, which is considered indicative of a statistically significant difference, 60 patients had to be included. Considering a drop-out rate of 10%, a total of 66 patients were recruited.
The secondary endpoints were the ORR and OS. Response was evaluated using the mRECIST, and AEs were evaluated using the CTCAE v4.03. OS and PFS were estimated using the Kaplan-Meier method. Hazard ratios and their 95% confidence intervals (CIs) were calculated. All analyses were performed with SPSS version 22.0 (IBM Corp., Armonk, NY, United States). A P value < 0.05 was considered statistically significant.
RESULTS
Participant characteristics
From February 2012 to December 2016, 66 participants were enrolled in this prospective study (Figure 2). The mean age in this study was 53.3 ± 11.7 years. Most participants were male (39/66, 83.3%), and cirrhosis was present in 75.8% of participants (50/66). The mean tumor size in this study was 6.7 cm ± 4.3 cm. In the present study, 56.1% (37/66) of participants had Barcelona Clinic Liver Cancer (BCLC) stage C disease, and 43.9% (29/66) had BCLC stage B disease. A total of 81.8% (54/66) of the participants had hepatitis B virus infection. The characteristics and demographics of the 66 consecutive participants are presented in Table 1.
Figure 2.
Patient selection flowchart. mRECIST: Modified Response Evaluation Criteria in Solid Tumors; TACE: Transarterial chemoembolization; HAIC: Hepatic arterial infusion chemotherapy.
Table 1.
Baseline characteristics
| Parameter | Number of participants (n = 66) |
| Mean age (yr) | 53.3 ± 13.6 |
| Sex | |
| Male | 55 |
| Female | 11 |
| Maximum tumor diameter (cm) | |
| ≤ 5 | 27 |
| 5-10 | 26 |
| > 10 | 13 |
| Child-Pugh score | |
| A | 57 |
| B7 | 9 |
| BCLC stage | |
| B | 29 |
| C | 37 |
| ECOG PS | |
| 0 | 46 |
| 1 | 20 |
| Vascular invasion | |
| Present | 25 |
| Absent | 41 |
| Portal vein invasion | |
| Present | 23 |
| Absent | 43 |
| Extrahepatic metastasis | |
| Present | 16 |
| Absent | 50 |
| HBV | |
| Positive | 54 |
| Negative | 12 |
| HBV DNA (copies/mL) | |
| > 2 × 103 | 30 |
| ≤ 2 × 103 | 36 |
| Cirrhosis | |
| Present | 50 |
| Absent | 16 |
| AFP (ng/mL) | |
| ≤ 100 | 26 |
| > 100 | 40 |
AFP: Alpha-fetoprotein; HBV: Hepatitis B virus infection; BCLC: Barcelona Clinic Liver Cancer; ECOG PS: Eastern Cooperative Oncology Group performance status.
Tumor response
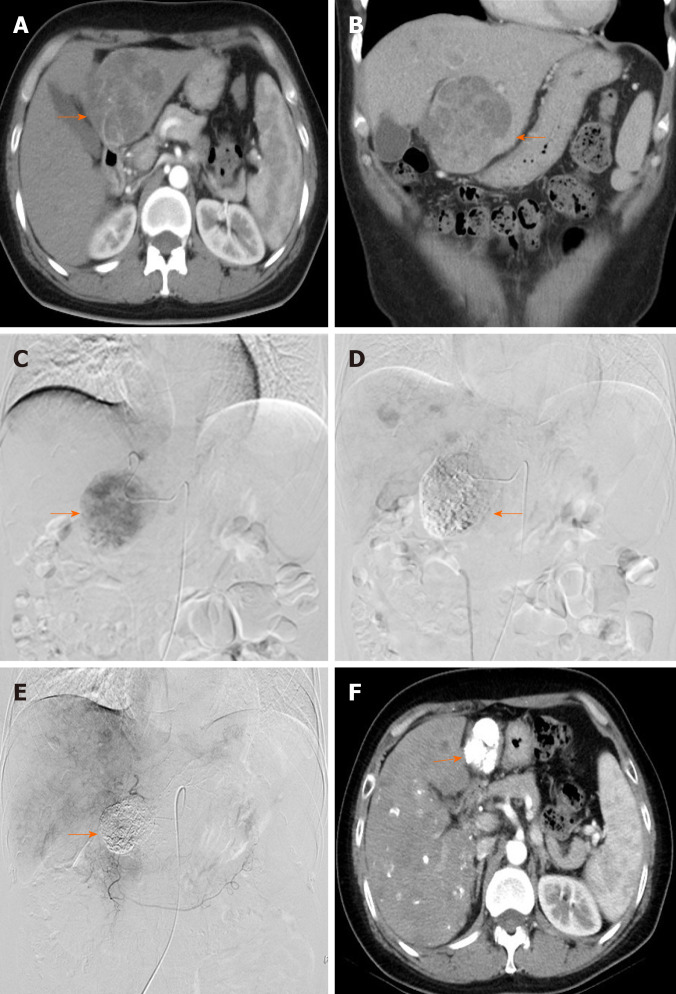
A total of 66 participants were included in our study. The overall response rate (ORR) was 42.4% (28/37), including 9 (13.6%) participants with CR and 19 (28.8%) with PR. There were 30 (45.5%) participants with SD and 8 (12.1%) with PD. The disease control rate (CR, PR, or SD) was 87.9% (58/66) (Table 2). One patient achieved CR based on the mRECIST criteria (Figure 3).
Table 2.
Tumor response (modified Response Evaluation Criteria for Solid Tumors)
| Best tumor response | Participants, n (%) |
| DCR, CR + PR + SD | 58 (87.9) |
| ORR, CR + PR | 28 (42.4) |
| CR | 9 (13.6) |
| PR | 19 (28.8) |
| SD | 30 (45.5) |
| PD | 8 (12.1) |
All participants were treated with hepatic arterial infusion chemotherapy (oxaliplatin, 5-fluorouracil, and folinic acid) after transarterial chemoembolization combined with sorafenib for intermediate and advanced hepatocellular carcinoma. CR: Complete response; DCR: Disease control rate; PR: Partial response; SD: Stable disease; ORR: Objective response rate.
Figure 3.
Images from a 41-year-old woman with intermediate-stage hepatocellular carcinoma who underwent combination therapy with sorafenib with hepatic arterial infusion chemotherapy (folinic acid, 5-fluorouracil, and oxaliplatin) after transarterial chemoembolization. A and B: Preoperative computed tomography (CT) showed the lesion in the liver (arrow); C: Angiography via the proper hepatic artery revealed a tumor mass in the liver (arrow); D: Postoperative angiography revealed the scattered deposition of lipiodol within the lesions in the liver (arrow); E: After 1 year, angiography via the proper hepatic artery revealed scattered deposition of lipiodol within the lesions in the liver (arrow); F: After 1 year, CT revealed scattered deposition of lipiodol within the lesions in the liver, and the tumor lesions had no enhancement during the arterial phase (arrow).
Survival and disease progression
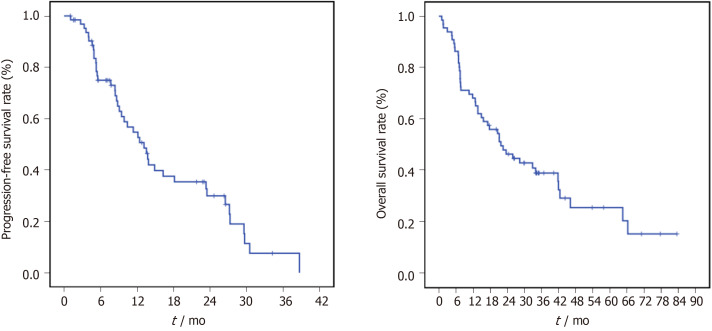
Follow-up was performed until May 2018. The median follow-up duration in this study was 22.0 mo (1-77 mo), during which time 45 participants died and 43 experienced PD. The median OS (mOS) was 21.8 mo (95%CI: 12.9-30.6 mo). The mOS of participants with BCLC stage B and BCLC stage C disease was 46.1 mo and 15.6 mo, respectively. The 1-, 2-, and 5-year mOS rates were 68.2%, 46.4%, and 25.6%, respectively. The mPFS was 13.1 mo (95%CI: 9.5-16.7 mo). The mPFS was 13.5 mo in the BCLC stage B participants and 9.4 mo in the BCLC stage C participants. The 6-mo, 12-mo-, and 24-mo PFS rates were 75.0%, 54.7%, and 30.0%, respectively (Figure 4). There were 49 (74.2%) patients who underwent MRI to evaluate the response, and 17 (25.8%) underwent CT to evaluate the response. There were no significant differences (P = 0.25 and P = 0.38) in the OS and PFS of patients who underwent MRI and CT.
Figure 4.
Kaplan-Meier curves of the progression-free survival and overall survival of patients with hepatocellular carcinoma who were treated with sorafenib combined with hepatic arterial infusion chemotherapy (folinic acid, 5-fluorouracil, and oxaliplatin) after transarterial chemoembolization and for Barcelona Clinic Liver Cancer stage B/C hepatocellular carcinoma.
Complications or AEs
There were no treatment-related deaths in this study. The most common adverse reaction in this study was liver function damage (69.7%, 42/66), of which grade 3-4 liver function damage [HAIC affected the aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels] was observed in 12.2% (8/66) of the participants; liver function returned to normal after treatment. Three (4.5%) participants had grade 3-4 thrombocytopenia, and two (3.0%) had grade 3-4 neutropenia, which also returned to normal after treatment. Twenty-seven (40.9%) participants developed hand-foot skin reactions (HFSRs). One participant developed pneumonia, which resolved after treatment. No vascular complications were noted in any of the participants, and no cerebral hemorrhage was noted as a vascular complication (Table 3).
Table 3.
Treatment-emergent and drug-related adverse events
| Adverse event |
Participants, n (%) |
|||
| Grade I | Grade II | Grade III | Grade IV | |
| Hematological | ||||
| Decreased platelet count | 14 (21.2) | 8 (12.1) | 3 (4.5) | 0 (0) |
| Decreased neutrophil count | 15 (22.7) | 11 (16.7) | 2 (3.0) | 0 (0) |
| Non-hematological | ||||
| Elevated alanine | 30 (45.5) | 8 (12.1) | 4 (6.1) | 4 (6.1) |
| Elevated serum bilirubin | 20 (30.3) | 26 (39.4) | 5 (7.6) | 0 (0) |
| Nausea and vomiting | 32 (48.5) | 8 (12.1) | 0 (0) | 0 (0) |
| Pain | 29 (43.9) | 11 (16.7) | 0 (0) | 0 (0) |
| Fever | 4 (6.1) | 2 (3.0) | 0 (0) | 0 (0) |
| Diarrhea | 10 (15.2) | 6 (9.1) | 0 (0) | 0 (0) |
| Hand-foot skin reaction | 7 (10.6) | 16 (24.2) | 4 (6.1) | 0 (0) |
| Neurotoxicity | 18 (27.3) | 7 (10.6) | 0 (0) | 0 (0) |
Data are the number of patients, with percentages in parentheses; all participants were treated with hepatic arterial infusion chemotherapy (oxaliplatin, 5-fluorouracil, and folinic acid) after transarterial chemoembolization combined with sorafenib for intermediate and advanced hepatocellular carcinoma.
DISCUSSION
This prospective study achieved the prespecified primary endpoint of a 12-mo PFS rate exceeding 54.7%. The combination of TACE-HAIC and sorafenib is considered to be safe. Most guidelines for HCC management recommend TACE as a first-line treatment for patients with unresectable HCC[38,39].
A previous study[40] combined local treatment methods and showed that combination therapy consisting of HAIC (EPF [etoposide, cisplatin, and 5-FU] and EAP [etoposide, adriamycin or epi-adriamycin, and cisplatin]) and TACE was better than transarterial embolization alone for unresectable advanced HCC. Several studies[41,42] have explored HAIC in advanced HCC with PVTT and reported survival benefits. However, there are no reports on the combination of sorafenib and TACE-HAIC for BCLC stage B/C HCC. In the studies conducted at our center[21,22], the mPFS and ORR of combined TACE with HAIC were superior to those of TACE alone.
We considered that there is a rationale for combining TACE with HAIC. First, the flow of the tumor-feeding artery slows down after TACE, and chemotherapy can be maintained at high blood concentrations for an extended period in the tumor tissue. Second, TACE causes tumor tissue ischemia, hypoxia, and tumor cell transmembrane ion pump failure, preventing the chemotherapy agent from being pumped out of the cell[43]. Finally, HCC mostly consists of microfocal cancer lesions after TACE, and HAIC can clear these lesions. TACE inevitably results in hypoxic insult to tumors and enhanced expression of circulating or tissue angiogenic factors (vascular endothelial growth factor) after TACE, which could be associated with unfavorable outcomes[44]. Treatment with a combination of an anti-angiogenic agent (sorafenib) and TACE may provide complementary inhibition of neovascularization and tumor growth. Phase III trials[45,46] have revealed the potential superiority of combined TACE plus sorafenib over TACE alone. In our study, we selected oxaliplatin-based HAIC therapy because some studies have proven that HAIC (FOLFOX) is safe and effective for HCC[8,35-37]. Furthermore, sorafenib and FOLFOX agents exert synergistic antitumor effects[47].
In this prospective cohort study, the mOS and mPFS were 21.8 mo and 13.1 mo, respectively. Compared with other studies, the mPFS in our study was better than that (7.2-7.9 mo) of TACE combined with sorafenib reported in two III trials[45,46]. The mOS and mPFS in our study were superior to those of sorafenib plus HAIC reported in a randomized phase III trial (21.8 mo vs 13.37 mo; 13.1 mo vs 7.13 mo)[36]. In this study, TACE combined with HAIC may have prolonged the mPFS by clearing residual tumor lesions. The phase III study enrolled different participants. In addition, in our study, we enrolled 37 (56.1%) participants with BCLC stage C disease, and the mOS and mPFS of these patients were 15.6 mo and 9.4 mo, respectively. We enrolled 16 patients with extrahepatic metastases. Most patients with HCC die from the progression of intrahepatic lesions; thus, it is important to control intrahepatic lesions. Sorafenib is the first-line drug for advanced HCC, which includes HCC with PVTT and/or extrahepatic metastases. Systemic treatment with sorafenib combined with the local treatment of TACE-HAIC may prolong survival. We enrolled 23 participants with portal vein invasion, and among these patients, the mOS was 13.6 mo, and the mPFS was 7.7 mo. The phase III trial (sorafenib-HAIC group vs sorafenib group)[36] enrolled patients with HCC with portal vein invasion, and the reported mPFS was 7.03 mo. However, these studies are not suitable for further in-depth comparison due to the heterogeneity of the trial participants.
The combination of TACE-HAIC and sorafenib is considered to be safe, and no treatment-related deaths were observed in this study. In addition, the rate of grade 3-4 toxicities was similar to that reported in a previous study, which consisted of increased AST levels (12.2% vs 31.4%), thrombocytopenia (4.5% vs 12.9%-14.3%), and neutropenia (3.0% vs 8.6%-9.7%). A total of 40.9% (27/66) of participants developed HFSRs, similar to that reported in a previous study[35,36,45,48]. Furthermore, the combination of TACE-HAIC and sorafenib was well tolerated, suggesting that this combination therapy does not increase the incidence of adverse reactions compared with HAIC alone. In our study, we found that HAIC affected ALT and AST, but these levels normalized soon after treatment. The rate of grade 3-4 AEs was less than that reported in a previous study (TACE-2), and the reasons may be as follows: First, the dosages of the drugs were reduced (oxaliplatin, 60-75 mg/m2; 5-FU, 1.0-1.5g/m2); however, the dosages of intravenous medication were 130 mg/m2 (oxaliplatin) and 2.4 g/m2 (5-FU), and the toxicity was tolerable. Second, the cTACE protocol used in the present study is different from the TACE protocol used in the TACE-2 study. By preserving the blood flow of the main artery to perform HAIC, cTACE results in an incomplete embolism, and chemotherapy is then infused into the tumors. The incomplete embolism can reduce AEs. It is important to adjust the drug dosage according to AEs. If a participant exhibited grade 3-4 myelosuppression, we decreased the dose of oxaliplatin and 5-FU or sorafenib.
For intermediate-stage HCC, TACE is the current standard of treatment, and TACE with drug-eluting beads provided a longer time to progression but did not improve survival in comparison with cTACE. For HCC with PVTT or a large nodule size, transarterial radioembolization (TARE) can prolong OS compared with sorafenib or TACE. However, patients cannot access yttrium 90 in Mainland China; thus, for patients with advanced HCC (segmental portal vein thrombosis, large nodule size, and Child-Pugh A disease) who do not have access to or are intolerant to sorafenib or TARE, TACE might be an alternative treatment[49-52].
In this study, the prognosis of advanced HCC was significantly worse than that of intermediate HCC. There are some other treatments for advanced HCC: Lenvatinib as a first-line drug was approved in the REFLECT trial[53], and the median OS was 13.6 mo. Regorafenib and cabozantinib are the second-line drugs for advanced HCC and were approved in the RESORCE and CELESTIAL trials[54,55], and the median OS was 10.2-10.6 mo. Nivolumab and pembrolizumab were approved in two phase II clinical trials, and the ORR was 15%-15.6%[56,57], but OS was not assessed. Radiotherapy is a common treatment method for unresectable HCC; in a meta-analysis[58], radiotherapy plus TACE was evaluated for unresectable HCC, and the OS was longer than that with TACE alone (22.7 mo vs 13.5 mo, P < 0.001, respectively).
There were some limitations in our study. First, because this was a single-arm study, it cannot produce powerful results because the sample size of our single-center trial may not have been large enough; thus, biases existed in our results. Therefore, prospective randomized controlled trials with larger sample sizes are required to further verify these results. Second, we used the mRECIST to evaluate the effect. However, contrast-enhanced CT has a slight disadvantage in assessing subtle areas of contrast enhancement within a tumor that has retained large amounts of lipiodol. To reduce the bias in our study, radiologists with over 10 years of experience with combined CT and MRI assessed the effects, and we tried to keep the imaging examination (CT or MRI) consistent before and after treatment to increase accuracy. In addition, 49 (74.2%) patients underwent MRI to evaluate the tumor response, and 17 (25.8%) underwent CT to evaluate the tumor response; there were no significant differences in the OS (P = 0.25) and PFS (P = 0.38) of patients who underwent MRI and CT.
In conclusion, in this phase II study, TACE-HAIC therapy combined with sorafenib for participants with BCLC stage B/C HCC is safe and effective. However, prospective randomized controlled trials are needed to confirm the effect of TACE-HAIC combined with sorafenib.
ARTICLE HIGHLIGHTS
Research background
Sorafenib has been proven effective for advanced hepatocellular carcinoma (HCC), transarterial chemoembolization (TACE) is the standard therapy for intermediate HCC, and hepatic arterial infusion chemotherapy (HAIC) is a safe and effective treatment for advanced HCC. Herein, we aimed to identify the safety and efficacy of combining sorafenib with HAIC after TACE for intermediate and advanced HCC.
Research motivation
Although there are many treatment methods for HCC, the therapeutic effect is very limited and does not significantly prolong patient survival. Safer and more effective protocols need to be developed to improve therapeutic effects.
Research objectives
To provide an effective combined treatment protocol based on previous studies.
Research methods
All patients initially received the standard 400 mg dose of sorafenib twice daily before TACE-HAIC. Participants at our institute with intermediate and advanced HCC underwent routine TACE. Then, the catheter used for embolization was kept in place in the feeding artery of the tumor, and oxaliplatin was intra-arterially administered for 6 h, followed by 5-fluorouracil (5-FU) for 18 h, and folinic acid was intravenously administered for 2 h.
Research results
The overall response rate was 42.4%. The disease control rate was 87.9%. The grade 3-4 toxicities consisted of thrombocytopenia (4.5%), neutropenia (3.0%), and elevated aspartate aminotransferase (12.2%). Hand-foot skin reaction was also observed (40.9%). The median progression-free survival was 13.1 mo, (13.5 mo in participants with Barcelona Clinic Liver Cancer (BCLC) stage B disease and 9.4 mo in participants with BCLC stage C disease). The 6-mo, 12-mo, and 24-mo PFS rates were 75.0%, 54.7%, and 30.0%, respectively. The median overall survival was 21.8 mo.
Research conclusions
Sorafenib combined with HAIC (folinic acid, 5-FU, and oxaliplatin) after TACE may be a feasible treatment choice for intermediate and advanced HCC based on patient tolerance and survival.
Research perspectives
The combination of sorafenib and TACE-HAIC has been shown to be effective with limited complications. Prospective randomized controlled trials are needed to confirm the effect of this combination therapy.
ACKNOWLEDGEMENTS
We wish to thank all the patients, clinicians, and support staff who participated in this study.
Footnotes
Institutional review board statement: This was a single-arm, single-institution, open-label phase II trial that was approved by the Research Ethics Committee of Peking University Cancer Hospital (2011110803).
Informed consent statement: All participants provided written informed consent for treatment according to the standard practices at our institution.
Conflict-of-interest statement: The authors have no conflicts of interest to declare.
STROBE statement: The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Manuscript source: Unsolicited manuscript
Peer-review started: February 20, 2020
First decision: April 18, 2020
Article in press: May 27, 2020
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Barone M, Suda T S-Editor: Yan JP L-Editor: Wang TQ E-Editor: Xing YX
Contributor Information
Bao-Jiang Liu, Department of Interventional Therapy, Peking University Cancer Hospital and Institute, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing 100142, China.
Song Gao, Department of Interventional Therapy, Peking University Cancer Hospital and Institute, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing 100142, China.
Xu Zhu, Department of Interventional Therapy, Peking University Cancer Hospital and Institute, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing 100142, China. drzhuxu@163.com.
Jian-Hai Guo, Department of Interventional Therapy, Peking University Cancer Hospital and Institute, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing 100142, China.
Xin Zhang, Department of Interventional Therapy, Peking University Cancer Hospital and Institute, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing 100142, China.
Hui Chen, Department of Interventional Therapy, Peking University Cancer Hospital and Institute, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing 100142, China.
Xiao-Dong Wang, Department of Interventional Therapy, Peking University Cancer Hospital and Institute, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing 100142, China.
Ren-Jie Yang, Department of Interventional Therapy, Peking University Cancer Hospital and Institute, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Beijing 100142, China.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.European Association for the Study of the Liver. Corrigendum to "EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma" [J Hepatol 69 (2018) 182-236] J Hepatol. 2019;70:817. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 3.Benson AB, D'Angelica MI, Abbott DE, Abrams TA, Alberts SR, Anaya DA, Anders R, Are C, Brown D, Chang DT, Cloyd J, Covey AM, Hawkins W, Iyer R, Jacob R, Karachristos A, Kelley RK, Kim R, Palta M, Park JO, Sahai V, Schefter T, Sicklick JK, Singh G, Sohal D, Stein S, Tian GG, Vauthey JN, Venook AP, Hammond LJ, Darlow SD. Guidelines Insights: Hepatobiliary Cancers, Version 2.2019. J Natl Compr Canc Netw. 2019;17:302–310. doi: 10.6004/jnccn.2019.0019. [DOI] [PubMed] [Google Scholar]
- 4.Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, Tateishi R, Han KH, Chawla YK, Shiina S, Jafri W, Payawal DA, Ohki T, Ogasawara S, Chen PJ, Lesmana CRA, Lesmana LA, Gani RA, Obi S, Dokmeci AK, Sarin SK. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11:317–370. doi: 10.1007/s12072-017-9799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301–1314. doi: 10.1016/S0140-6736(18)30010-2. [DOI] [PubMed] [Google Scholar]
- 6.Lo CM, Ngan H, Tso WK, Liu CL, Lam CM, Poon RT, Fan ST, Wong J. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35:1164–1171. doi: 10.1053/jhep.2002.33156. [DOI] [PubMed] [Google Scholar]
- 7.Llovet JM, Real MI, Montaña X, Planas R, Coll S, Aponte J, Ayuso C, Sala M, Muchart J, Solà R, Rodés J, Bruix J Barcelona Liver Cancer Group. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359:1734–1739. doi: 10.1016/S0140-6736(02)08649-X. [DOI] [PubMed] [Google Scholar]
- 8.Qin S, Bai Y, Lim HY, Thongprasert S, Chao Y, Fan J, Yang TS, Bhudhisawasdi V, Kang WK, Zhou Y, Lee JH, Sun Y. Randomized, multicenter, open-label study of oxaliplatin plus fluorouracil/leucovorin versus doxorubicin as palliative chemotherapy in patients with advanced hepatocellular carcinoma from Asia. J Clin Oncol. 2013;31:3501–3508. doi: 10.1200/JCO.2012.44.5643. [DOI] [PubMed] [Google Scholar]
- 9.Kodama K, Kawaoka T, Aikata H, Uchikawa S, Inagaki Y, Hatooka M, Morio K, Nakahara T, Murakami E, Tsuge M, Hiramatsu A, Imamura M, Kawakami Y, Masaki K, Honda Y, Mori N, Takaki S, Tsuji K, Kohno H, Kohno H, Moriya T, Nonaka M, Hyogo H, Aisaka Y, Chayama K. Comparison of clinical outcome of hepatic arterial infusion chemotherapy and sorafenib for advanced hepatocellular carcinoma according to macrovascular invasion and transcatheter arterial chemoembolization refractory status. J Gastroenterol Hepatol. 2018;33:1780–1786. doi: 10.1111/jgh.14152. [DOI] [PubMed] [Google Scholar]
- 10.Kang MK, Park JG, Lee HJ. Comparison of clinical outcomes between sorafenib and hepatic artery infusion chemotherapy in advanced hepatocellular carcinoma: A STROBE-compliant article. Medicine (Baltimore) 2018;97:e0611. doi: 10.1097/MD.0000000000010611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lyu N, Lin Y, Kong Y, Zhang Z, Liu L, Zheng L, Mu L, Wang J, Li X, Pan T, Xie Q, Liu Y, Lin A, Wu P, Zhao M. FOXAI: a phase II trial evaluating the efficacy and safety of hepatic arterial infusion of oxaliplatin plus fluorouracil/leucovorin for advanced hepatocellular carcinoma. Gut. 2018;67:395–396. doi: 10.1136/gutjnl-2017-314138. [DOI] [PubMed] [Google Scholar]
- 12.Kokudo N, Hasegawa K, Akahane M, Igaki H, Izumi N, Ichida T, Uemoto S, Kaneko S, Kawasaki S, Ku Y, Kudo M, Kubo S, Takayama T, Tateishi R, Fukuda T, Matsui O, Matsuyama Y, Murakami T, Arii S, Okazaki M, Makuuchi M. Evidence-based Clinical Practice Guidelines for Hepatocellular Carcinoma: The Japan Society of Hepatology 2013 update (3rd JSH-HCC Guidelines) Hepatol Res. 2015:45. doi: 10.1111/hepr.12464. [DOI] [PubMed] [Google Scholar]
- 13.Lu J, Zhang XP, Zhong BY, Lau WY, Madoff DC, Davidson JC, Qi X, Cheng SQ, Teng GJ. Management of patients with hepatocellular carcinoma and portal vein tumour thrombosis: comparing east and west. Lancet Gastroenterol Hepatol. 2019;4:721–730. doi: 10.1016/S2468-1253(19)30178-5. [DOI] [PubMed] [Google Scholar]
- 14.Tsimberidou AM, Vaklavas C, Fu S, Wen S, Lim JA, Hong D, Wheler J, Naing A, Uehara C, Wallace M, Kurzrock R. Hepatic arterial infusion therapy in advanced cancer and liver-predominant disease: the MD Anderson Experience. Hepatogastroenterology. 2013;60:1611–1623. [PubMed] [Google Scholar]
- 15.Carr BI, Bron K, Swanson DP. Prospective randomized trial of hepatic artery chemotherapy with cisplatin and doxorubicin, with or without lipiodol in the treatment of advanced stage hepatocellular carcinoma. J Clin Gastroenterol. 2011;45:e87–e91. doi: 10.1097/MCG.0b013e31820fb274. [DOI] [PubMed] [Google Scholar]
- 16.Yen Y, Lim DW, Chung V, Morgan RJ, Leong LA, Shibata SI, Wagman LD, Marx H, Chu PG, Longmate JA, Lenz HJ, Ramanathan RK, Belani CP, Gandara DR. Phase II study of oxaliplatin in patients with unresectable, metastatic, or recurrent hepatocellular cancer: a California Cancer Consortium Trial. Am J Clin Oncol. 2008;31:317–322. doi: 10.1097/COC.0b013e318162f57d. [DOI] [PubMed] [Google Scholar]
- 17.Gao J, Zhen R, Liao H, Zhuang W, Guo W. Pharmacokinetics of continuous transarterial infusion of 5-fluorouracil in patients with advanced hepatocellular carcinoma. Oncol Lett. 2018;15:7175–7181. doi: 10.3892/ol.2018.8242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li XH, Wang YF, Sun GM. Transcatheter arterial chemoembolization combined with microwave coagulation therapy and the perioperative care for patients with hepatocellural carcinoma. J BUON. 2015;20:1037–1041. [PubMed] [Google Scholar]
- 19.Chu HH, Kim JH, Yoon HK, Ko HK, Gwon DI, Kim PN, Sung KB, Ko GY, Kim SY, Park SH. Chemoembolization Combined with Radiofrequency Ablation for Medium-Sized Hepatocellular Carcinoma: A Propensity-Score Analysis. J Vasc Interv Radiol. 2019;30:1533–1543. doi: 10.1016/j.jvir.2019.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Wang G, Liu Y, Zhou SF, Qiu P, Xu L, Wen P, Wen J, Xiao X. Sorafenib combined with transarterial chemoembolization in patients with hepatocellular carcinoma: a meta-analysis and systematic review. Hepatol Int. 2016;10:501–510. doi: 10.1007/s12072-015-9700-7. [DOI] [PubMed] [Google Scholar]
- 21.Gao S, Zhang PJ, Guo JH, Chen H, Xu HF, Liu P, Yang RJ, Zhu X. Chemoembolization alone vs combined chemoembolization and hepatic arterial infusion chemotherapy in inoperable hepatocellular carcinoma patients. World J Gastroenterol. 2015;21:10443–10452. doi: 10.3748/wjg.v21.i36.10443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhu LZ, Xu S, Qian HL. Transarterial embolization and low-dose continuous hepatic arterial infusion chemotherapy with oxaliplatin and raltitrexed for hepatocellular carcinoma with major portal vein tumor thrombus. World J Gastroenterol. 2018;24:2501–2507. doi: 10.3748/wjg.v24.i23.2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Couri T, Pillai A. Goals and targets for personalized therapy for HCC. Hepatol Int. 2019;13:125–137. doi: 10.1007/s12072-018-9919-1. [DOI] [PubMed] [Google Scholar]
- 24.Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J, Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D, Guan Z. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25–34. doi: 10.1016/S1470-2045(08)70285-7. [DOI] [PubMed] [Google Scholar]
- 25.Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 26.Sergio A, Cristofori C, Cardin R, Pivetta G, Ragazzi R, Baldan A, Girardi L, Cillo U, Burra P, Giacomin A, Farinati F. Transcatheter arterial chemoembolization (TACE) in hepatocellular carcinoma (HCC): the role of angiogenesis and invasiveness. Am J Gastroenterol. 2008;103:914–921. doi: 10.1111/j.1572-0241.2007.01712.x. [DOI] [PubMed] [Google Scholar]
- 27.Li X, Feng GS, Zheng CS, Zhuo CK, Liu X. Expression of plasma vascular endothelial growth factor in patients with hepatocellular carcinoma and effect of transcatheter arterial chemoembolization therapy on plasma vascular endothelial growth factor level. World J Gastroenterol. 2004;10:2878–2882. doi: 10.3748/wjg.v10.i19.2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilhelm SM, Carter C, Tang L, Wilkie D, McNabola A, Rong H, Chen C, Zhang X, Vincent P, McHugh M, Cao Y, Shujath J, Gawlak S, Eveleigh D, Rowley B, Liu L, Adnane L, Lynch M, Auclair D, Taylor I, Gedrich R, Voznesensky A, Riedl B, Post LE, Bollag G, Trail PA. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004;64:7099–7109. doi: 10.1158/0008-5472.CAN-04-1443. [DOI] [PubMed] [Google Scholar]
- 29.Abou-Alfa GK. TACE and sorafenib: a good marriage? J Clin Oncol. 2011;29:3949–3952. doi: 10.1200/JCO.2011.37.9651. [DOI] [PubMed] [Google Scholar]
- 30.Kudo M, Arizumi T. Transarterial Chemoembolization in Combination with a Molecular Targeted Agent: Lessons Learned from Negative Trials (Post-TACE, BRISK-TA, SPACE, ORIENTAL, and TACE-2) Oncology. 2017;93 Suppl 1:127–134. doi: 10.1159/000481243. [DOI] [PubMed] [Google Scholar]
- 31.Strebel BM, Dufour JF. Combined approach to hepatocellular carcinoma: a new treatment concept for nonresectable disease. Expert Rev Anticancer Ther. 2008;8:1743–1749. doi: 10.1586/14737140.8.11.1743. [DOI] [PubMed] [Google Scholar]
- 32.Chao Y, Chung YH, Han G, Yoon JH, Yang J, Wang J, Shao GL, Kim BI, Lee TY. The combination of transcatheter arterial chemoembolization and sorafenib is well tolerated and effective in Asian patients with hepatocellular carcinoma: final results of the START trial. Int J Cancer. 2015;136:1458–1467. doi: 10.1002/ijc.29126. [DOI] [PubMed] [Google Scholar]
- 33.Lee TY, Lin CC, Chen CY, Wang TE, Lo GH, Chang CS, Chao Y. Combination of transcatheter arterial chemoembolization and interrupted dosing sorafenib improves patient survival in early-intermediate stage hepatocellular carcinoma: A post hoc analysis of the START trial. Medicine (Baltimore) 2017;96:e7655. doi: 10.1097/MD.0000000000007655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Malofeeva EV, Domanitskaya N, Gudima M, Hopper-Borge EA. Modulation of the ATPase and transport activities of broad-acting multidrug resistance factor ABCC10 (MRP7) Cancer Res. 2012;72:6457–6467. doi: 10.1158/0008-5472.CAN-12-1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.He MK, Zou RH, Li QJ, Zhou ZG, Shen JX, Zhang YF, Yu ZS, Xu L, Shi M. Phase II Study of Sorafenib Combined with Concurrent Hepatic Arterial Infusion of Oxaliplatin, 5-Fluorouracil and Leucovorin for Unresectable Hepatocellular Carcinoma with Major Portal Vein Thrombosis. Cardiovasc Intervent Radiol. 2018;41:734–743. doi: 10.1007/s00270-017-1874-z. [DOI] [PubMed] [Google Scholar]
- 36.He M, Li Q, Zou R, Shen J, Fang W, Tan G, Zhou Y, Wu X, Xu L, Wei W, Le Y, Zhou Z, Zhao M, Guo Y, Guo R, Chen M, Shi M. Sorafenib Plus Hepatic Arterial Infusion of Oxaliplatin, Fluorouracil, and Leucovorin vs Sorafenib Alone for Hepatocellular Carcinoma With Portal Vein Invasion: A Randomized Clinical Trial. JAMA Oncol. 2019;5:953–960. doi: 10.1001/jamaoncol.2019.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bruno PM, Liu Y, Park GY, Murai J, Koch CE, Eisen TJ, Pritchard JR, Pommier Y, Lippard SJ, Hemann MT. A subset of platinum-containing chemotherapeutic agents kills cells by inducing ribosome biogenesis stress. Nat Med. 2017;23:461–471. doi: 10.1038/nm.4291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, Kudo M, Lee JM, Choi BI, Poon RT, Shiina S, Cheng AL, Jia JD, Obi S, Han KH, Jafri W, Chow P, Lim SG, Chawla YK, Budihusodo U, Gani RA, Lesmana CR, Putranto TA, Liaw YF, Sarin SK. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010;4:439–474. doi: 10.1007/s12072-010-9165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Korean Liver Cancer Study Group and National Cancer Center, Korea. [Practice guidelines for management of hepatocellular carcinoma 2009] Korean J Hepatol. 2009;15:391–423. doi: 10.3350/kjhep.2009.15.3.391. [DOI] [PubMed] [Google Scholar]
- 40.Yodono H, Takekawa SD, Tarusawa K, Ikami I, Kanehira J, Saito Y, Takahashi S, Sasaki T, Nishi N, Kimura T. Combination therapy consisting of arterial infusion chemotherapy (EPF, EAP) and transcatheter arterial embolization (TAE) Cancer Chemother Pharmacol. 1994;33 Suppl:S79–S83. doi: 10.1007/BF00686673. [DOI] [PubMed] [Google Scholar]
- 41.Ikeda M, Okusaka T, Furuse J, Mitsunaga S, Ueno H, Yamaura H, Inaba Y, Takeuchi Y, Satake M, Arai Y. A multi-institutional phase II trial of hepatic arterial infusion chemotherapy with cisplatin for advanced hepatocellular carcinoma with portal vein tumor thrombosis. Cancer Chemother Pharmacol. 2013;72:463–470. doi: 10.1007/s00280-013-2222-x. [DOI] [PubMed] [Google Scholar]
- 42.Choi JH, Chung WJ, Bae SH, Song DS, Song MJ, Kim YS, Yim HJ, Jung YK, Suh SJ, Park JY, Kim DY, Kim SU, Cho SB. Randomized, prospective, comparative study on the effects and safety of sorafenib vs. hepatic arterial infusion chemotherapy in patients with advanced hepatocellular carcinoma with portal vein tumor thrombosis. Cancer Chemother Pharmacol. 2018;82:469–478. doi: 10.1007/s00280-018-3638-0. [DOI] [PubMed] [Google Scholar]
- 43.Trevisani F, De Notariis S, Rossi C, Bernardi M. Randomized control trials on chemoembolization for hepatocellular carcinoma: is there room for new studies? J Clin Gastroenterol. 2001;32:383–389. doi: 10.1097/00004836-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Shim JH, Park JW, Kim JH, An M, Kong SY, Nam BH, Choi JI, Kim HB, Lee WJ, Kim CM. Association between increment of serum VEGF level and prognosis after transcatheter arterial chemoembolization in hepatocellular carcinoma patients. Cancer Sci. 2008;99:2037–2044. doi: 10.1111/j.1349-7006.2008.00909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kudo M, Imanaka K, Chida N, Nakachi K, Tak WY, Takayama T, Yoon JH, Hori T, Kumada H, Hayashi N, Kaneko S, Tsubouchi H, Suh DJ, Furuse J, Okusaka T, Tanaka K, Matsui O, Wada M, Yamaguchi I, Ohya T, Meinhardt G, Okita K. Phase III study of sorafenib after transarterial chemoembolisation in Japanese and Korean patients with unresectable hepatocellular carcinoma. Eur J Cancer. 2011;47:2117–2127. doi: 10.1016/j.ejca.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 46.Meyer T, Fox R, Ma YT, Ross PJ, James MW, Sturgess R, Stubbs C, Stocken DD, Wall L, Watkinson A, Hacking N, Evans TRJ, Collins P, Hubner RA, Cunningham D, Primrose JN, Johnson PJ, Palmer DH. Sorafenib in combination with transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma (TACE 2): a randomised placebo-controlled, double-blind, phase 3 trial. Lancet Gastroenterol Hepatol. 2017;2:565–575. doi: 10.1016/S2468-1253(17)30156-5. [DOI] [PubMed] [Google Scholar]
- 47.Ma SQ, Cao BR, Zhang H, Luo LP, Ren Y, Hu T, Chen CM. The lack of Raf-1 kinase feedback regulation enhances antiapoptosis in cancer cells. Oncogene. 2017;36:2014–2022. doi: 10.1038/onc.2016.384. [DOI] [PubMed] [Google Scholar]
- 48.Lencioni R, Llovet JM, Han G, Tak WY, Yang J, Guglielmi A, Paik SW, Reig M, Kim DY, Chau GY, Luca A, Del Arbol LR, Leberre MA, Niu W, Nicholson K, Meinhardt G, Bruix J. Sorafenib or placebo plus TACE with doxorubicin-eluting beads for intermediate stage HCC: The SPACE trial. J Hepatol. 2016;64:1090–1098. doi: 10.1016/j.jhep.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 49.Facciorusso A, Licinio R, Muscatiello N, Di Leo A, Barone M. Transarterial chemoembolization: Evidences from the literature and applications in hepatocellular carcinoma patients. World J Hepatol. 2015;7:2009–2019. doi: 10.4254/wjh.v7.i16.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barone M, Ettorre GC, Ladisa R, Schiavariello M, Santoro C, Francioso G, Vinciguerra V, Francavilla A. Transcatheter arterial chemoembolization (TACE) in treatment of hepatocellular carcinoma. Hepatogastroenterology. 2003;50:183–187. [PubMed] [Google Scholar]
- 51.Quirk M, Kim YH, Saab S, Lee EW. Management of hepatocellular carcinoma with portal vein thrombosis. World J Gastroenterol. 2015;21:3462–3471. doi: 10.3748/wjg.v21.i12.3462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim PH, Choi SH, Kim JH, Park SH. Comparison of Radioembolization and Sorafenib for the Treatment of Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis: A Systematic Review and Meta-Analysis of Safety and Efficacy. Korean J Radiol. 2019;20:385–398. doi: 10.3348/kjr.2018.0496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, Park JW, Han G, Jassem J, Blanc JF, Vogel A, Komov D, Evans TRJ, Lopez C, Dutcus C, Guo M, Saito K, Kraljevic S, Tamai T, Ren M, Cheng AL. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163–1173. doi: 10.1016/S0140-6736(18)30207-1. [DOI] [PubMed] [Google Scholar]
- 54.Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Breder V, Gerolami R, Masi G, Ross PJ, Song T, Bronowicki JP, Ollivier-Hourmand I, Kudo M, Cheng AL, Llovet JM, Finn RS, LeBerre MA, Baumhauer A, Meinhardt G, Han G RESORCE Investigators. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56–66. doi: 10.1016/S0140-6736(16)32453-9. [DOI] [PubMed] [Google Scholar]
- 55.Abou-Alfa GK, Meyer T, Cheng AL, El-Khoueiry AB, Rimassa L, Ryoo BY, Cicin I, Merle P, Chen Y, Park JW, Blanc JF, Bolondi L, Klümpen HJ, Chan SL, Zagonel V, Pressiani T, Ryu MH, Venook AP, Hessel C, Borgman-Hagey AE, Schwab G, Kelley RK. Cabozantinib in Patients with Advanced and Progressing Hepatocellular Carcinoma. N Engl J Med. 2018;379:54–63. doi: 10.1056/NEJMoa1717002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, Kim TY, Choo SP, Trojan J, Welling TH Rd, Meyer T, Kang YK, Yeo W, Chopra A, Anderson J, Dela Cruz C, Lang L, Neely J, Tang H, Dastani HB, Melero I. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhu AX, Finn RS, Edeline J, Cattan S, Ogasawara S, Palmer D, Verslype C, Zagonel V, Fartoux L, Vogel A, Sarker D, Verset G, Chan SL, Knox J, Daniele B, Webber AL, Ebbinghaus SW, Ma J, Siegel AB, Cheng AL, Kudo M KEYNOTE-224 investigators. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label phase 2 trial. Lancet Oncol. 2018;19:940–952. doi: 10.1016/S1470-2045(18)30351-6. [DOI] [PubMed] [Google Scholar]
- 58.Huo YR, Eslick GD. Transcatheter Arterial Chemoembolization Plus Radiotherapy Compared With Chemoembolization Alone for Hepatocellular Carcinoma: A Systematic Review and Meta-analysis. JAMA Oncol. 2015;1:756–765. doi: 10.1001/jamaoncol.2015.2189. [DOI] [PubMed] [Google Scholar]