Dear Sir:
Meta-analyses of pivotal randomized trials confirmed the benefit of intravenous thrombolysis (IVT) and mechanical thrombectomy (MT) in patients with acute ischemic stroke [1,2]. In addition to the treatment effect, the cost saved with the efficacyproven therapy should be considered in healthcare policy making for resource allocation and reimbursement. Earlier studies have already shown that IVT and MT are clearly cost-effective, but the magnitude of cost saving likely differs according to individual healthcare systems. This study aimed to estimate the 5-year cumulative cost savings based on 3-month modified Rankin Scale (mRS) disability with IVT and MT in the Korean healthcare setting.
For hypothetical 3-month mRS level distributions of patients treated with IVT versus without IVT and with MT and without MT, we used data of representative meta-analyses of clinical trials of IVT and MT [1,2]. For the 5-year cumulative cost for each 3-month mRS level, we used data of a recently published Korean study that linked individual patient-level data of 3-month mRS levels prospectively captured in a large multicenter prospective registry with their direct healthcare costs from the National Health Insurance Service claim database. The direct cost included expenses for inpatient care, outpatient care, prescribed medication, and long-term care. In that study, the estimated 5-year cumulative cost was US dollar (USD) 53,578 for mRS 0, USD 56,059 for mRS 1, USD 108,892 for mRS 2, USD 201,562 for mRS 3, USD 279,188 for mRS 4, USD 257,486 for mRS 5, and USD 28,866 for mRS 6 [3].
From these data, we generated an average 5-year cumulative cost saving per patient with IVT or MT when the additional expense for IVT or MT procedure was not considered. Then, we subtracted the additional expense for IVT or MT procedure paid by the Korean National Health Insurance. Currently, there are two payment systems in Korea: one is the new diagnostic-related groups (DRG)-based payment system which is effective since January 2020, and the other is the fee-for-service (FFS)-based payment system. For additional expenses for IVT and MT, we used data of acquisition cost and/or reimbursement paid by the Korean National Health Insurance. For IVT, it was USD 0 with the new DRG-based payment system (currently, no additional payment for IVT compared to no IVT) and USD 1,179 (USD 970 for actilyse cost and USD 209 for IVT procedure) with the FFS-based payment system. The estimated additional expense for MT procedure (including cost for thrombectomy device and ancillary costs for neurointervention) was USD 9,714 with the new DRG-based payment system and USD 6,463 with the FFS-based payment system. As in the previous study, costs were adjusted to 2015 prices using the Consumer Price Index of health care (Statistic Korea Consumer Price Index in January 2018), and the Korean won (KRW) was converted to 2015 USD using the purchasing power parity method (USD 1 equals KRW 871; 2018 Organization for Economic Co-operation and Development data, purchasing power parities) [3,4]. Because this study used publicly available data, the approval of Institutional Review Board was not required.
Table 1 shows the mRS distributions of the comparative groups reported in the meta-analyses of clinical trials and the calculated 5-year cumulative costs for each group. For IVT, the estimated 5-year cumulative cost per 100 patients was USD 12,063,751 with IVT and USD 13,156,981 without IVT, indicating a cost saving per 100 patients of USD 1,093,230 when the additional expense for IVT was not considered. After including the additional expense for IVT, the estimated 5-year cumulative cost saving per patient was USD 10,932 (USD 10,932–USD 0) with the new DRG-based payment system and USD 9,753 (USD 10,932–USD 1,179) with the FFS-based payment system.
Table 1.
Five-year cumulative cost savings with IVT and MT
| mRS distribution (%) |
5-Year cumulative cost for 100 patients (USD) |
Cost saving per patient (USD) | ||||
|---|---|---|---|---|---|---|
| Control | IVT/MT | Control | IVT/MT | |||
| IVT | ||||||
| mRS | ||||||
| 0 | 12.4 | 17.2 | 664,367 | 921,542 | ||
| 1 | 16.6 | 19.5 | 930,579 | 1,093,151 | ||
| 2 | 13.1 | 11.5 | 1,426,485 | 1,252,258 | ||
| 3 | 13.3 | 13.5 | 2,680,775 | 2,721,087 | ||
| 4 | 14.5 | 9.9 | 4,048,226 | 2,763,961 | ||
| 5 | 11.1 | 10.9 | 2,858,095 | 2,806,597 | ||
| 6 | 19.0 | 17.5 | 548,454 | 505,155 | ||
| Total | 100.0 | 100.0 | 13,156,981 | 12,063,751 | ||
| Cost saving per patient (USD) | ||||||
| DRG-based payment system | 10,932 | |||||
| FFS-based payment system | 9,753 | |||||
| MT | ||||||
| mRS | ||||||
| 0 | 5.0 | 10.0 | 267,890 | 535,780 | ||
| 1 | 7.9 | 16.9 | 442,866 | 947,397 | ||
| 2 | 13.6 | 19.1 | 1,480,931 | 2,079,837 | ||
| 3 | 16.4 | 16.9 | 3,305,617 | 3,406,398 | ||
| 4 | 24.7 | 15.6 | 6,895,944 | 4,355,333 | ||
| 5 | 13.5 | 6.2 | 3,476,061 | 1,596,413 | ||
| 6 | 18.9 | 15.3 | 545,567 | 441,650 | ||
| Total | 100.0 | 100.0 | 16,414,876 | 13,362,808 | ||
| Cost saving per patient (USD) | ||||||
| DRG-based payment system | 20,807 | |||||
| FFS-based payment system | 24,058 | |||||
Five-year cumulative costs for 100 patients without including additional expense for IVT or MT were calculated by (each mRS proportion×100)×(5-year cumulative cost for each mRS level). Cost saving per patient was calculated by (5-year cumulative costs for 100 patients)/100–(additional expense for IVT or MT).
IVT, intravenous thrombolysis; MT, mechanical thrombectomy; mRS, modified Rankin Scale; USD, US dollar; DRG, diagnostic-related group; FFS, fee-for-service.
For MT, the estimated 5-year cumulative cost per 100 patients without considering the additional expense for MT was USD 13,362,808 with MT and USD 16,414,876 without MT, and the difference was USD 3,052,068. After including the additional expense for MT, the estimated 5-year cumulative cost saving per patient was USD 20,807 (USD 30,521–USD 9,714) with the new DRG-based payment system and USD 24,058 (USD 30,521–USD 6,463) with the FFS-based payment system.
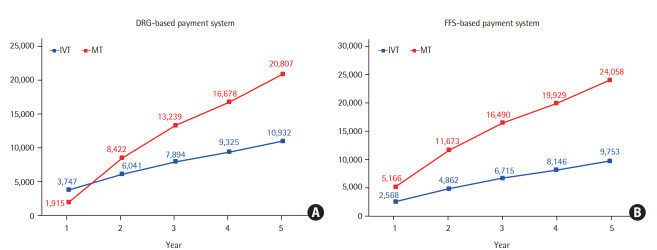
The cumulative cost saving per patient over the 5-year period is displayed in Figure 1 (Supplementary Table 1 presents the estimated cumulative cost per patient by year with IVT and MT compared to control). Over the 5-year period, it gradually increased for both IVT and MT therapies. For MT, the cost saving with the DRG-based payment system was USD 1,915 during the first year when the additional expense for MT should be subtracted. However, after the first year, it substantially increased because of the effect of favorable shift of mRS disability levels with MT on the cumulative cost saving. The slope of the 5-year cumulative cost saving looks greater with MT than with IVT, reflecting the greater treatment effect of MT compared to IVT.
Figure 1.
Cumulative cost savings (US dollar [USD]) per patient with intravenous thrombolysis (IVT) and mechanical thrombectomy (MT) costing over time. (A) Diagnostic-related group (DRG)-based payment system applied. (B) Fee-for-service (FFS) based payment system applied.
Previously, cost savings with interventions were generally derived from modeling based on substantial assumptions. In contrast, our estimation has an advantage of derivation from the actual costs and the real post-stroke disability levels of individual patients. Therefore, our results would provide a transparent and scientific foundation to guide our healthcare policy making for reperfusion therapies.
An intervention that costs less than the national annual gross domestic product (GDP) per capita for one quality-adjusted life-year (QALY) gained is considered highly cost-effective [5]. In 2018, the annual GDP per capita in Korea was USD 31,363, which could be a rough reference point for very cost-effective interventions. It has been well demonstrated that both IVT and MT therapies yield a significant gain of QALYs or other related heath outcome metrics. In this study, the estimated 5-year cumulative cost was even lower with both IVT and MT, which indicates that these interventions are enormously cost-effective.
For the validity of our estimations, it would be instructive to compare our findings with previous ones. Because of the differences in absolute healthcare costs between Korea and US and time horizon between studies, a value of relative cost saving with each intervention ([cost saving with intervention]/[cost without intervention]×100), rather than an absolute cost saving would be a more comparable index. In United States studies, the relative cost saving for a lifetime horizon was 8.0% with IVT (the lifetime medical cost for base case: USD 287,400 with IVT vs. USD 312,400 without IVT) [6], and the relative cost saving with MT plus IVT as compared to IVT only for a discounted life-expectancy (9.13-year with MT plus IVT and 7.92 with IVT only) was 9.7% (for base case: USD 215,781 with MT plus IVT vs. USD 238,984 with IVT only) [7]. In our study, the relative cost saving was 8.3% with IVT and 12.7% with MT. Despite the differences in the time duration (5 years in our study and lifetime or life-expectancy period in United States studies) and the absolute healthcare costs, the estimates of relative cost savings with IVT and MT look comparable between our and United States studies.
In Korea, the annual incidence of ischemic stroke is approximately 80,000, and the proportion of patients treated with reperfusion therapy is about 10% for IVT and 3.3% for MT [8,9]. Therefore, the nationwide annual cost saving during subsequent 5 years would be USD 87,458,424 with IVT and USD 54,930,480 with MT. Given their substantial benefits on societal burden, the resource allocation and reimbursement for these therapies should be made accordingly.
This study has several limitations. The current estimation considered the direct healthcare cost only without including indirect costs, and thereby likely underestimates the real benefit of cost saving with these therapies. The more people die early, the less the long-term cost would be incurred. Therefore, our results from analyzing cost only does not fully reflect the societal benefit of reperfusion therapy that reduces mortality as well as disability. A majority of patients enrolled in thrombolytic clinical trials were Western populations, and thereby the magnitude of benefit observed in the trials might not be equally applicable to Korean populations. However, a previous registry study showed that the benefit of thrombolysis observed in Korean patients was comparable to that seen in Western populations [10]. Patients who unlikely benefit from thrombolysis (moderate-to-severe pre-stroke disability or very elderly) are usually excluded from clinical trials, but are frequently encountered and treated in real world practice. Therefore, our estimation based on the mRS distributions observed in clinical trials might overestimate the cost savings. The current estimation was generated in Korean healthcare setting, which is not directly applicable to other healthcare settings. However, the relative cost saving with IVT or MT might be relevant to other healthcare systems.
Footnotes
Dr. Keun-Sik Hong has received lecture honoraria and research grants from Boehringer Ingelheim Korea related to the current topic. Dr. Hee-Joon Bae was involved as a site investigator of a multicenter clinical trial sponsored by Boehringer Ingelheim.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2020.00556.
Cumulative cost per patient by year with IVT and MT compared to control
References
- 1.Hacke W, Lyden P, Emberson J, Baigent C, Blackwell L, Albers G, et al. Effects of alteplase for acute stroke according to criteria defining the European Union and United States marketing authorizations: Individual-patient-data meta-analysis of randomized trials. Int J Stroke. 2018;13:175–189. doi: 10.1177/1747493017744464. [DOI] [PubMed] [Google Scholar]
- 2.Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 3.Kim SE, Lee H, Kim JY, Lee KJ, Kang J, Kim BJ, et al. Three-month modified Rankin Scale as a determinant of 5-year cumulative costs after ischemic stroke: an analysis of 11,136 patients in Korea. Neurology. 2020;94:e978–e991. doi: 10.1212/WNL.0000000000009034. [DOI] [PubMed] [Google Scholar]
- 4.Organization for Economic Co-operation and Development . OECD; Statistics and data directorate: prices and purchasing power parities (PPP) www.oecd.org/sdd/prices-ppp/. Accessed May 10, 2020. [Google Scholar]
- 5.WHO Commission on Macroeconomics and Health . World Health Organization; Macroeconomics and health: investing in health for economic development. Report of the commission on macroeconomics and health: executive summary. https://apps.who.int/iris/handle/10665/42435. 2001. Accessed May 10, 2020. [Google Scholar]
- 6.Boudreau DM, Guzauskas GF, Chen E, Lalla D, Tayama D, Fagan SC, et el. Cost-effectiveness of recombinant tissue-type plasminogen activator within 3 hours of acute ischemic stroke: current evidence. Stroke. 2014;45:3032–3039. doi: 10.1161/STROKEAHA.114.005852. [DOI] [PubMed] [Google Scholar]
- 7.Shireman TI, Wang K, Saver JL, Goyal M, Bonafé A, Diener HC, et al. Cost-effectiveness of solitaire stent retriever thrombectomy for acute ischemic stroke: results from the SWIFT-PRIME trial (solitaire with the intention for thrombectomy as primary endovascular treatment for acute ischemic stroke) Stroke. 2017;48:379–387. doi: 10.1161/STROKEAHA.116.014735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the Korean stroke society and clinical research center for stroke. J Stroke. 2013;15:2–20. doi: 10.5853/jos.2013.15.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, et al. Executive summary of stroke statistics in Korea 2018: a report from the Epidemiology Research Council of the Korean Stroke Society. J Stroke. 2019;21:42–59. doi: 10.5853/jos.2018.03125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rha JH, Shrivastava VP, Wang Y, Lee KE, Ahmed N, Bluhmki E, et al. Thrombolysis for acute ischaemic stroke with alteplase in an Asian population: results of the multicenter, multinational Safe Implementation of Thrombolysis in Stroke-Non-European Union World (SITS-NEW) Int J Stroke. 2014;9 Suppl A100:93–101. doi: 10.1111/j.1747-4949.2012.00895.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Cumulative cost per patient by year with IVT and MT compared to control