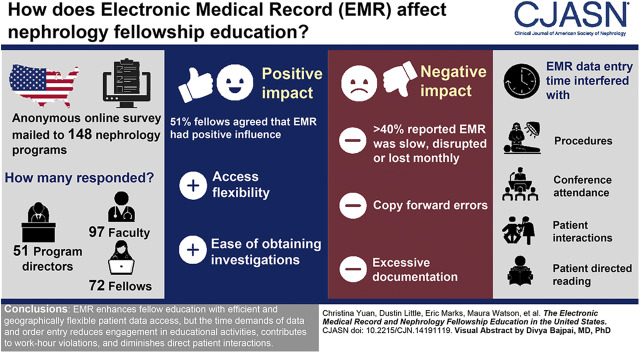
Visual Abstract
Keywords: Medical Record, Nephrology Fellowship, Clinical Education, Burnout, Work Hours, Work Compression, Electronic Health Records, Fellowships and Scholarships, Reading, Social Desirability, Records, Physicians, Radiology, Surveys and Questionnaires, Documentation, Faculty
Abstract
Background and objectives
An unintended consequence of electronic medical record use in the United States is the potential effect on graduate physician training. We assessed educational burdens and benefits of electronic medical record use on United States nephrology fellows by means of a survey.
Design, setting, participants, & measurements
We used an anonymous online opinion survey of all United States nephrology program directors (n=148), their faculty, and fellows. Program directors forwarded survey links to fellows and clinical faculty, indicating to how many they forwarded the link. The three surveys had parallel questions to permit comparisons.
Results
Twenty-two percent of program directors (n=33) forwarded surveys to faculty (n=387) and fellows (n=216; 26% of United States nephrology fellows). Faculty and fellow response rates were 25% and 33%, respectively; 51% of fellows agreed/strongly agreed that the electronic medical record contributed positively to their education. Perceived positive effects included access flexibility and ease of obtaining laboratory/radiology results. Negative effects included copy-forward errors and excessive, irrelevant documentation. Electronic medical record function was reported to be slow, disrupted, or completely lost monthly or more by >40%, and these were significantly less likely to agree that the electronic medical record contributed positively to their education. Electronic medical record completion time demands contributed to fellow reluctance to do procedures (52%), participate in conferences (57%), prolong patient interactions (74%), and do patient-directed reading (55%). Sixty-five percent of fellows reported often/sometimes exceeding work-hours limits due to documentation time demands; 85% of faculty reported often/sometimes observing copy-forward errors. Limitations include potential nonresponse and social desirability bias.
Conclusions
Respondents reported that the electronic medical record enhances fellow education with efficient and geographically flexible patient data access, but the time demands of data and order entry reduce engagement in educational activities, contribute to work-hours violations, and diminish direct patient interactions.
Introduction
The electronic medical record (EMR) has become an integral part of the health care system. EMRs are federally mandated (1,2), meant to standardize medical billing, minimize medical error, and facilitate data sharing, and they are a potential source of “big data” for epidemiologic studies and medical decision-making software development. EMRs are unique databases in that most data entry is performed by clinicians who are concurrently (and primarily) providing patient care (3). Rapid expansion of EMR use over the last 10 years has produced unintended consequences, including unfulfilled expectations, suboptimal usability, unintended patient harms, and EMR-associated provider burnout (2,4–8).
One unintended consequence is a potential deleterious effect on physician training, including limiting time with patients and mentors; perpetuation of erroneous information (data obfuscation) via prepopulation, checkboxes, and copy forward; and superficial discussions and analysis of patient problems (2,3,9). In two recent surveys of nephrology fellowship program directors on procedural curriculum, many commented that the dual time pressures of EMR data entry and work-hours limits adversely affect fellow training and curriculum provision, with fellows limiting time spent on direct patient interactions (including procedures), self-directed clinical study, and didactic conferences (10,11). Work hours may be extended as much as 20%–25% by EMR documentation done after duty hours or at home, and such work is associated with increased burnout (6,12).
EMR use may adversely affect direct patient care time and patient satisfaction (13). Clinical reasoning may deteriorate after EMR introduction due to loss of chronological patient data relationships and increased cognitive workload (14). Critical thinking and decision skills can be negatively affected by over-reliance on standardized order sets and automation bias (15–18). Nonetheless, there are potential educational benefits to EMR use, including easy access to laboratory and radiologic test results, facilitation of tracking of trainee patient mix, performance indicators, and compliance with best practices (14).
We administered an anonymous survey to assess the opinions of nephrology program directors, faculty, and fellows on the effect of the EMR on nephrology fellowship training.
Materials and Methods
The protocol (EDO-2019–0249) was approved by the Walter Reed National Military Medical Center Department of Research Protections as “exempt from IRB review” per 32 CFR 219.101(b)(2).
Surveys were drafted (C.M.Y.), edited, and refined (D.J.L., R.N., and R.R.) by active clinical faculty familiar with one or more EMRs. Questions were on the basis of comments from recent procedural surveys (10,11), studies of unintended consequences and effect of the EMR on postgraduate medical education (9,16–20), and question structure of wellness surveys (21,22). We included both positive and negative statements for agreement. Surveys were anonymous; we did not solicit age, sex, race, program site, or EMR vendor.
Nephrology program directors (n=148), identified from the Public List of Nephrology Specialty Programs from the Accreditation Council for Graduate Medical Education website (23), were anonymously surveyed (Supplemental Material). Respondent IP addresses were blocked. The survey could be taken only once from the same device. The link was delivered by email, with delivery receipt, and it was open from January 28 to April 5, 2019. Reminders were sent at 2-week intervals.
After an explanatory text, respondents were asked to confirm that they were the nephrology program director. If not, they were directed away from the survey and asked to forward the link to the program director.
Next, they were asked to forward the anonymous fellow survey (Supplemental Material) link and indicate the number of fellows to whom they sent it. They were also asked to forward the anonymous faculty survey (Supplemental Material) link to their clinical faculty and indicate the number of faculty to whom they sent it. Because there are no public lists of active nephrology fellows and faculty, this allowed calculation of fellow and faculty response rates. Using the program director as the survey gatekeeper facilitated access to all fellows and faculty in a given program, and it was designed to reduce bias when comparing program director, faculty, and fellow responses because all were potentially represented for a given program.
An explanatory text introduced the survey, allowing potential respondents to exit if they did not wish to participate. Demographic information collected for program directors and faculty was years of clinical experience, including fellowship training. Fellows were asked only for year of training.
Survey questions were parallel for program director, faculty, and fellow respondents to allow comparison and applied only to the EMR at the primary training site. Objectives were as follows.
Determine whether program directors, clinical faculty, and fellows believe the EMR contributes positively or negatively to fellow education and whether this is on the basis of years of nephrology practice or fellowship training year.
Determine perceived positive and negative effects on fellow education and whether fellows identify them differently from faculty and program directors.
Describe EMR technical problems and whether fellows perceive them differently from faculty and program directors.
Determine whether education in (1) nephrology procedures, (2) didactic conferences, (3) patient interactions, and (4) self-directed case-based literature review is perceived to be adversely affected by EMR completion time demands.
Determine whether EMR use increases fellow self-reported stress when seeing outpatients.
Determine how much outpatient encounter time is spent by fellows and faculty on EMR data entry.
Determine whether EMR completion time contributes to the risk of exceeding work-hours limitations and whether fellows report exceeding work-hours limits because of EMR completion tasks.
Determine whether fellows make mistakes in documentation due to “copy forward.”
Percentages, medians, and interquartile ranges (IQRs) were used as appropriate. Response frequency of program directors/faculty with ≤20 years of clinical experience was compared with those with >20 years using the Fisher exact test (P=0.05 considered significant). Response frequency of second-year (third year counted as second year) versus first-year fellows, of faculty versus fellows, and of those reporting EMR dysfunction monthly or more versus less frequent disruption was compared using the Fisher exact test. Wave analysis, assessing nonresponse bias, compared faculty and fellow responses received in the last 3 weeks versus those received in the first 7 weeks.
Results
Respondents
Program Director Survey.
Response rate was 34% (51 of 148 programs). Median survey time was 3 minutes (IQR 0, 8; 77% completion) (Supplemental Material); 33 program directors (22% of programs) forwarded the link to fellows. Median number of fellows/program was 6 (range, 2–20), with 216 invited to take the survey; 55% (18 of 33) had six or more fellows in training. Thirty-two program directors (22% of programs) forwarded the link to clinical faculty. Median number of clinical faculty members was 10 (range, 3–30), with 387 invited to take the survey. Twenty-six percent (10 of 38) of program directors had been in practice for 10 years or less; 34% (13 of 38) had been in practice for >10–20 years, and 39% (15 of 38) had been in practice for >20 years.
Faculty Survey.
Response rate was 25% (97 of 387 surveys forwarded). Median survey time was 6 minutes (IQR 4, 8; 84% completion) (Supplemental Material); 40% of respondents had been in practice for 10 years or less (39 of 97), 27% (26 of 97) of respondents had been in practice for >10–20 years; and 33% (32 of 97) of respondents had been in practice for >20 years.
Fellow Survey.
Response rate was 33% (72 of 216 surveys forwarded). Median survey time was 6 minutes (IQR 4, 8; 84% completion) (Supplemental Material). There were 827 nephrology fellows in 148 United States programs in training year 2018–2019 (24). Thus, 26% of nephrology fellows in the United States were surveyed; 39 of 72 (54%) were first-year fellows, 29 of 72 (40%) were second-year fellows, and 6% were third-year fellows.
Survey wave analysis (Supplemental Material) comparing faculty/fellow responses during weeks 8–10 versus weeks 1–7 showed that limited demographics and answer patterns of late responders (surrogate nonresponders) were not significantly different than those of early responders.
EMR Functionality
EMR hardware and software functionality problems are described in Tables 1 and 2; 40%–50% of fellows, faculty, and program directors indicated that EMR functionality was slow, disrupted, or completely lost monthly or more. Fellows were less likely to report navigation problems than program directors and faculty. Thirty-seven percent (73 of 198) of respondents indicated that inpatient and outpatient/dialysis unit EMRs did not communicate. Less than 20% indicated their EMR was without significant problems.
Table 1.
Problems with electronic medical record hardware and software functionality at the primary training site
| Problem: At My Institution, EMR Functionality Is Slowed, Disrupted, or Completely Lost | Program Directors, n=37 | Clinical Faculty, n=94 | Fellows, n=66 |
|---|---|---|---|
| Daily | 2 (5%) | 11 (12%) | 6 (9%) |
| Weekly | 7 (19%) | 20 (21%) | 10 (15%) |
| Monthly | 8 (22%) | 15 (16%) | 12 (18%) |
| A few times a year | 9 (24%) | 26 (28%) | 20 (30%) |
| Almost never | 9 (24%) | 20 (21%) | 15 (23%) |
| Never | 2 (5%) | 2 (2%) | 3 (5%) |
EMR, electronic medical record.
Table 2.
Problems with electronic medical record hardware and software functionality at the primary training site
| Problems with EMR Functionality at Our Primary Training Site Include (Check All That Apply) | Program Directors, n=37 | Clinical Faculty, n=94 | Fellows, n=67 |
|---|---|---|---|
| Screen latency/delay | 14 (38%) | 38 (40%) | 23 (34%) |
| Frequent unscheduled downtime | 6 (16%) | 20 (21%) | 12 (18%) |
| Inpatient and outpatient EMR do not communicate | 14 (38%) | 41 (44%) | 18 (27%) |
| Generalized slowness | 12 (32%) | 33 (35%) | 21 (31%) |
| Too many click boxes | 20 (54%) | 59 (63%) | 37 (55%) |
| Too many required fields not relevant to the encounter | 20 (54%) | 44 (47%) | 29 (43%) |
| Too much focus on billing rather than clinical features of encounter | 14 (38%) | 49 (52%) | 20 (30%) |
| Difficulty in navigation | 13 (35%) | 35 (37%) | 9 (13%) |
| Too many alerts | 16 (43%) | 40 (43%) | 27 (40%) |
| Templates import information that is not useful and/or is incorrect | 21 (57%) | 44 (47%) | 15 (22%) |
| Clinical decision support package is not useful and/or is incorrect | 10 (27%) | 28 (30%) | 11 (16%) |
| There are no significant problems with our EMR | 5 (14%) | 10 (11%) | 12 (18%) |
EMR, electronic medical record.
Perceived Effect on Education
In total, 51% of fellows, 40% of faculty, and 32% of program directors agreed/strongly agreed that their EMR contributes positively to fellow education. Fellows (51%) were not more likely than faculty and program directors (38%) to agree/strongly agree (P=0.12). Faculty in practice ≤20 years were no more likely to agree/strongly agree than those in practice >20 years (47% versus 25%; P=0.06). Program directors practicing ≤20 years were no more likely to agree/strongly agree than those practicing >20 years (26% versus 40%; P=0.48). Fellows and faculty reporting EMR dysfunction monthly or more were significantly less likely to agree/strongly agree that the EMR contributed positively to fellow education versus those reporting dysfunction less frequently: 33% (9 of 27) versus 66% (23 of 35); P=0.02 (fellows) and 28% (17 of 61) versus 47% (31 of 66); P=0.03 (faculty/program directors).
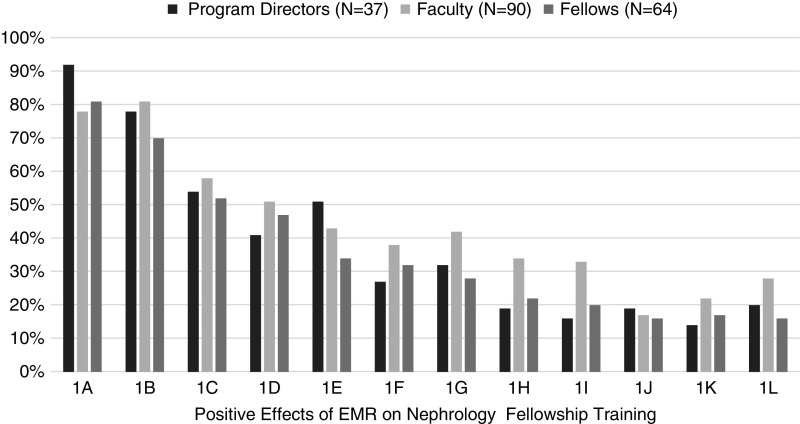
Positive features reported by respondents are shown in Figure 1. All groups liked the ability to access the EMR from home or from mobile devices (80%–90%) and ease of laboratory and imaging result retrieval (70%–80%). About 50%–60% said their EMR efficiently determined patient medications, but some commented (Supplemental Material) that their EMR imported outdated and incorrect medication lists. Over 50% of program directors felt that drop-down boxes and constrained order sets ensured that correct acute dialysis and continuous RRT orders were entered by fellows. Overall, 36% said their programs used the EMR for retrospective clinical research projects for fellows, and 34% said that EMR data were used to determine fellow patient mix. Few reported their EMR was useful for tracking quality indicators for CKD (17%), maintenance dialysis (19%), or protocolized transplant care (22%). Some program directors commented that their EMRs specifically did not permit tracking of patient mix and quality indicators (Supplemental Material).
Figure 1.
Positive effects of the electronic medical record (EMR) on nephrology education reported by survey respondents. 1A, EMR accessible from home/mobile device; 1B, Efficient laboratory result trending; 1C, efficient determination of patient medications; 1D, improves communication with multidisciplinary team; 1E, ensures correct kidney replacement therapy orders (drop-down boxes/warnings); 1F, tracking fellow outpatient diagnosis mix; 1G, source of database studies for fellow research; 1H, improves health information security; 1I, facilitates medication dose adjustment for eGFR; 1J, ensures quality indicators are met for chronic kidney disease; 1K, ensures quality indicators are met for maintenance dialysis; 1L, facilitates delivery of post-transplant protocol care.
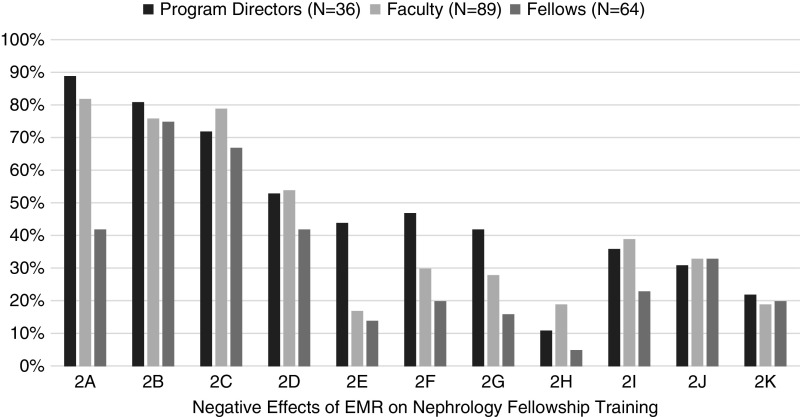
Negative features (Figure 2) included “excessive and/or irrelevant EMR documentation” (65%–75%), more time spent during encounters on documentation than on the patient (70%–80%), and “copy forward” leading to incorrect information in the medical record (80%). Few fellows felt that EMR home/mobile access interfered with protected time for education (14%) or for personal needs (20%), although about 45% of program directors indicated they perceived this to be so; 47% of program directors and 40% of faculty felt the EMR interfered with timeliness of encounter note completion. Forty-one percent of fellows indicated that they spent “too much time transcribing information that should be entered by ancillary or administrative staff.”
Figure 2.
Negative effects of the electronic medical record (EMR) on nephrology education reported by survey respondents. 2A, "copy forward" errors; 2B, less time with patient/more on documentation; 2C, excessive/Irrelevant documentation make chart review difficult; 2D, irrelevant documentation prevents minimal essential evaluation; 2E, access to home/mobile device interferes with protected time for education; 2F, access to home/mobile device interferes with personal time; 2G, drop downs/forced choices prevent learning dialysis orders without prompts; 2H, confusing to write clear orders for kidney replacement therapy; 2I, inpatient and outpatient EMR do not "talk to each other"; 2J, fellows reluctant to engage in education because of EMR time demands; 2K, functions slowly/not at all with excessive documentation time.
EMR data entry time demands increased self-reported fellow reluctance to do procedures, attend conferences, prolong patient interactions, and do self-directed reading (Table 3). This reluctance was not fully perceived by faculty and program directors, except in the case of prolonging patient interactions, where over 50% of faculty and program directors reported observing it. Many comments (Supplemental Material) discussed adverse experiences with the EMR on fellow-patient interactions. One respondent commented that the EMR had led to the “iPatient: the culture we have created in which the training doctors think that the patient is INSIDE the computer.”
Table 3.
Perceived effect of electronic medical record completion time demands on fellow reluctance to participate in educational activities and direct patient care
| Respondents Who “Agreed” or “Strongly Agreed” with the Statement | Because of the Competing Time Demands of EMR Completion, Fellows Are Often Reluctant to | |||
|---|---|---|---|---|
| Do Procedures | Participate in Conferences | Prolong Patient Encounters | Do Independent Case-Directed Literature Review | |
| Fellows | 31/60 (52%) | 35/61 (57%) | 46/62 (74%) | 34/62 (55%) |
| Clinical faculty | 24/84 (29%) | 27/83 (32%) | 49/85 (58%) | 34/84 (40%) |
| Program directors | 14/37 (38%) | 10/36 (28%) | 21/37 (57%) | 14/37 (38%) |
EMR, electronic medical record.
Thirty-nine percent (24 of 62) of fellows agreed/strongly agreed that the EMR increased their stress when seeing outpatients, and 33% of faculty agreed/strongly agreed that it increased time needed to staff patients. Faculty and fellows estimated time spent on outpatient EMR documentation before, during, and after fellow appointments (Table 4). Thirty-four percent (20 of 59) of fellows spent as much or more time entering data as the length of the visit for new patient appointments, and 49% (29 of 59) of fellows spent as much or more time entering data as the length of the visit for follow-up visits.
Table 4.
Appointment and electronic medical record documentation time reported by fellows and faculty for fellow outpatient encounters
| Time Reported | New Patient | Follow-Up Patient |
|---|---|---|
| Fellow median appointment time, min | 45 (IQR, 30–60) | 25 (IQR, 20–30) |
| Fellow estimated median EMR data entry time, min | 30 (IQR, 20–45) | 20 (IQR, 15–30) |
| Faculty estimated median EMR data entry time, min | 15 (IQR, 10–20) | 7 (IQR, 5–0) |
IQR, interquartile range; EMR, electronic medical record.
Seventy-eight percent of fellows report “often/sometimes” being at risk to exceed work-hours limits, and 64% report often/sometimes exceeding them because of EMR documentation; 64% of faculty and 54% of program directors observed that fellows were “often/sometimes” at risk of exceeding work hours because of EMR time demands.
Among fellows, 54% reported making “copy-forward” errors; 91% of faculty had observed “copy-forward” errors made by fellows. Many fellow, faculty, and program director comments (Supplemental Material) emphasized inaccuracy and error in the EMR, exacerbated by prepopulation and “copy forward.”
Discussion
Our survey elicited opinions and observations from program directors, clinical faculty, and fellows at United States nephrology training programs regarding the perceived effect of the EMR on the general and nephrology-specific clinical learning experience, system performance, and clinician time commitment to data entry. There were potentially multiple respondents at each training site, thus reducing bias when comparing fellows, faculty, and program directors. Programs surveyed were similar in size to the average (six fellows per program), and proportions of first-year and second-/third-year fellows were approximately those reported for training year 2019 (24,25).
Limitations include potential nonresponse bias, which may be (but not necessarily) associated with a lower response rate (26,27). Response rates were as expected for an online physician survey, considering delivery complexity and because reminders were delivered by program directors rather than investigators (28–30). Wave analysis indicated that late responders (surrogate “nonresponders”) were similar to earlier responders. We attempted to reduce nonresponse and social desirability bias using anonymity, few demographic questions, and no questions regarding training site or EMR vendor. We did not ask how long the EMR had been in use; unless a program had a new EMR, first-year fellows would have been using it for at least 6 months.
Nephrology patients are among the most medically complex in terms of medications prescribed, number of comorbidities, and mortality risk (31). The EMR, which facilitates access to laboratory and imaging data, updated medication lists, past medical history and diagnoses, and standardized dialysis order sets, should improve nephrology patient care and the clinical learning environment.
About 50% of fellows indicated that the EMR contributed positively to their education. Faculty and program directors did not differ significantly from nephrology fellows. This is consistent with previous surveys demonstrating positive perceptions of EMR effect on graduate medical education. At a large academic health center, >50% of faculty and trainees (residents and fellows) had a positive overall impression of the EMR during the initial implementation and 2 years afterward (17). Another physician survey (including residents and fellows) at an academic hospital showed that 58% were satisfied with their EMR, and 61% felt that it had a positive effect on patient care (32). In a 2007 survey of a large, representative sample of United States physicians, the majority reported being satisfied overall with their outpatient EMR (33). However, in our survey many respondents described unintended and deleterious consequences for fellows’ clinical experience. Although 50%–60% reported that patient medications could be accurately determined, for others medication lists are often incorrect and not updated—a focus issue for the 2019 Centers for Medicare & Medicaid Services (CMS) Promoting Interoperability Program (PIP; i.e., “Meaningful Use”) (6). Few EMRs seem to assist with drug dosing on the basis of eGFR. Problem lists and past medical history may be a series of uncurated “billing diagnoses.” Drop-down picklists and prompts for dialysis and continuous RRT orders assist fellows in entering correct and complete orders, but program directors were concerned that these aids may prevent fellows from learning to write orders without prompts. Nephrology-specific EMR tracking of CKD and dialysis quality indicators, patient mix, and post-transplant protocol adherence are underused and in some cases, prohibited.
Many respondents reported serious technical, interoperability, and usability problems. Over 40% reported that function was “slowed, disrupted, or completely lost” monthly or more. Not surprisingly, these were significantly less likely to agree that their EMR contributed positively to education. EMR downtime is associated with adverse patient safety events (34), and frequent disruptions likely adversely affect the clinical learning environment. Over 30% of respondents reported that outpatient, inpatient, and dialysis unit EMRs did not intercommunicate. Interoperability, another focus of the 2019 CMS PIP, is impeded by proprietary issues (1). Usability problems were common. Poor usability may lead to increased cognitive load and clinician error, directing attention away from data synthesis and clinical decision making; improving usability has been shown to associate with improved cognitive performance (3,4,9,35).
The major negative reported by all respondent categories was excessive EMR documentation time associated with fellow reluctance to prolong direct patient interactions. Reported documentation time for fellow clinic encounters would, on average, leave little time for interacting directly with the patient. Outpatient practice physicians may spend up to twice the time in EMR documentation as in patient face-to-face time, and outpatient data entry time is inversely associated with patient satisfaction (13,36). The majority of fellow respondents also felt reluctance to perform nephrology procedures, perform case-directed reading, and attend didactic conferences—shifting emphasis from education (the purpose of fellowship) to data entry. Procedural competency in kidney biopsy and temporary dialysis catheter insertion is required by the Accreditation Council for Graduate Medical Education, and the survey suggests that EMR time burden may affect procedural proficiency. It may also affect attendance and engagement at academic conferences, the predominant educational modalities in nephrology fellowship curriculum (30).
Bloated, inaccurate progress notes (due to copy forward, prepopulation, and irrelevant data entry) lead to data obfuscation, and the majority of faculty surveyed had observed copy-forward errors in nephrology fellow notes. Copy forward and prepopulation decrease EMR documentation time—creating a vicious cycle (3,2,9,13,18). EMR entry time burden is associated with frustration and burnout (6,37). For fellows, who must comply with work-hours limitations, EMR documentation demands may lead to severe work compression, with associated irreconcilable and opposing professionalism requirements. This is reflected by the majority of fellows reporting sometimes or often exceeding work-hours limitations—choosing medical record completion and patient care over work-hours adherence (38).
What can be done? Hospital administration should focus on minimizing EMR dysfunction/downtime, which in the interest of patient safety, provider wellness, and the clinical learning environment, should be exceedingly rare. Documentation policies addressing copy forward and other practices that lead to data obfuscation should be considered (3,13). The problem of work compression must be faced—there are limits to clinical efficiency, especially in graduate medical education. Usability, interfaces, and interoperability must be improved, with reduction of data entry time (2,39). New technologies are needed, including digital scribes, continuously updated smart links to published guidelines (stimulating evidence-based decision making), and multidisciplinary, clinically driven, pertinent, fluid patient problem lists.
In summary, this survey of nephrology program directors, faculty, and fellows indicates that the EMR is perceived to enhance educational experience by promoting efficient and flexible access to laboratory/imaging results and to a lesser extent, medication reconciliation and standardized dialysis order sets. EMR data entry time is excessive due to poor functional performance/usability and medical record obfuscation. Time pressures of EMR data entry and resulting work compression may increase fellow reluctance to engage in educational opportunities, encourage work-hours noncompliance, and stifle direct patient interactions. This may apply to graduate medical education generally, perhaps more significantly in those specialties, like nephrology, with highly complex patients. Faculty should be aware of trainee documentation time, advocate for improved EMR functionality/usability, and promote practices that improve efficiency and reduce work compression.
Disclosures
Dr. D.J. Little is employed as a research physician at AstraZeneca. All remaining authors have nothing to disclose.
Funding
None.
Supplementary Material
Acknowledgments
We would like to thank the program directors, faculty, and fellows who participated in the survey.
The views expressed are those of the authors and do not necessarily reflect the official policy or position of the Department of the Army/Navy/Air Force, the Department of Defense, or the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “From Nihilism to Opportunity: The Educational Potential of the Electronic Health Record,” on pages 917–919.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.14191119/-/DCSupplemental.
Supplemental Material. Program director electronic medical record (EMR) survey, fellow EMR survey, faculty EMR survey, completion rates for surveys, wave analysis (assessment of nonresponse bias), and respondent comments.
References
- 1.Centers for Medicare & Medicaid Services: Promoting interoperability programs: 2019 program requirements, 2019. Available at: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/2019ProgramRequirementsMedicare.html. Accessed September 2, 2019
- 2.Colicchio TK, Cimino JJ, Del Fiol G: Unintended consequences of nationwide electronic health record adoption: Challenges and opportunities in the post-meaningful use era. J Med Internet Res 21: e13313, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harrington L: Copy-forward in electronic health records: Lipstick on a pig. Jt Comm J Qual Patient Saf 43: 371–374, 2017. [DOI] [PubMed] [Google Scholar]
- 4.Ratwani RM, Reider J, Singh H: A decade of health information technology usability challenges and the path forward. JAMA 321: 743–744, 2019. [DOI] [PubMed] [Google Scholar]
- 5.Wright AA, Katz IT: Beyond burnout—redesigning care to restore meaning and sanity for physicians. N Engl J Med 378: 309–311, 2018. [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt TD, Dyrbye LN, Sinsky C, Hasan O, Satele D, Sloan J, West CP: Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 91: 836–848, 2016. [DOI] [PubMed] [Google Scholar]
- 7.Dzau VJ, Kirch DG, Nasca TJ: To care is human—collectively confronting the clinician-burnout crisis. N Engl J Med 378: 312–314, 2018. [DOI] [PubMed] [Google Scholar]
- 8.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD: Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 89: 443–451, 2014. [DOI] [PubMed] [Google Scholar]
- 9.Paterick ZR, Patel NJ, Paterick TE: Unintended consequences of the electronic medical record on physicians in training and their mentors. Postgrad Med J 94: 659–661, 2018. [DOI] [PubMed] [Google Scholar]
- 10.Yuan CM, Nee R, Little DJ, Narayan R, Childs JM, Prince LK, Raghavan R, Oliver JD 3rd; Nephrology Education Research and Development Consortium : Survey of kidney biopsy clinical practice and training in the United States. Clin J Am Soc Nephrol 13: 718–725, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yuan CM, Oliver JD 3rd, Little DJ, Narayan R, Prince LK, Raghavan R, Nee R; Nephrology Education Research and Development Consortium—NERDC : Survey of non-tunneled temporary hemodialysis catheter clinical practice and training. J Vasc Access 20: 507–515, 2019. [DOI] [PubMed] [Google Scholar]
- 12.Robertson SL, Robinson MD, Reid A: Electronic health record effects on work-life balance and burnout within the I3 population collaborative. J Grad Med Educ 9: 479–484, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marmor RA, Clay B, Millen M, Savides TJ, Longhurst CA: The impact of physician electronic health record usage on patient satisfaction. Appl Clin Inormatics 9: 11–14, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Varpio L, Day K, Elliot-Miller P, King JW, Kziemsky C, Parush A, Roffey T, Rashotte J: The impact of adopting EHRs: How losing connectivity affects clinical reasoning. Med Educ 49: 476–486, 2015. [DOI] [PubMed] [Google Scholar]
- 15.Goddard K, Roudsari A, Wyatt JC: Automation bias: A systematic review of frequency, effect mediators, and mitigators. J Am Med Inform Assoc 19: 121–127, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tierney MJ, Pageler NM, Kahana M, Pantaleoni JL, Longhurst CA: Medical education in the electronic medical record (EMR) era: Benefits, challenges, and future directions. Acad Med 88: 748–752, 2013. [DOI] [PubMed] [Google Scholar]
- 17.Rosdahl JA, Rudd M, Benjamin R, Wiener JS, Sloane R, Brown A, Robert Lee W, Turner D, Qin R, Atwater AR: Effect of the adoption of a comprehensive electronic health record on graduate medical education: Perceptions of faculty and trainees. South Med J 111: 476–483, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH: Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 13: 547–556, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stewart E, Kahn D, Lee E, Simon W, Duncan M, Mosher H, Harris K, Bell J, El-Farra N, Sharpe B: Internal medicine progress note writing attitudes and practices in an electronic health record. J Hosp Med 10: 525–529, 2015. [DOI] [PubMed] [Google Scholar]
- 20.Wang JK, Ouyang D, Hom J, Chi J, Chen JH: Characterizing electronic health record usage patterns of inpatient medicine residents using event log data. PLoS One 14: e0205379, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Linzer M, Poplau S, Grossman E, Varkey A, Yale S, Williams E, Hicks L, Brown RL, Wallock J, Kohnhorst D, Barbouche M: A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: Results from the Healthy Work Place (HWP) study. J Gen Intern Med 30: 1105–1111, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dyrbye LN, Meyers D, Ripp J, Dalal N, Bird SB, Sen S: A Pragmatic Approach for Organizations to Measure Health Care Professional Well-Being. NAM Perspectives Discussion Paper, Washington, DC, National Academy of Medicine, 2018.
- 23.Accreditation Council for Graduate Medical Education : Accreditation Council for Graduate Medical Education public list of nephrology specialty programs. Available at: https://apps.acgme.org/ads/Public/Programs/Search. Accessed May 13, 2020
- 24.Accreditation Council for Graduate Medical Education: Number of accredited programs and on-duty residents (academic year 2018-2019; United States). Available at: https://apps.acgme.org/ads/Public. Accessed June 1, 2019
- 25.Pivert K, Boyle S, Chan L, McDyre K, Mehdi A, Norouzi S, Tuchman S, Waitzman J, Sozio SM: Nephrology Fellow Survey—Results and Insights, Washington, DC, ASN Alliance for Kidney Health, 2019, p 6 [Google Scholar]
- 26.Davern M: Nonresponse rates are a problematic indicator of nonresponse bias in survey research. Health Serv Res 48: 905–912, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Halbesleben JRB, Whitman MV: Evaluating survey quality in health services research: A decision framework for assessing nonresponse bias. Health Serv Res 48: 913–930, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, Samuel S, Ghali WA, Sykes LL, Jetté N: Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 15: 32, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liebman SE, Moore CA, Monk RD, Rizvi MS: What are we doing? A survey of United States nephrology fellowship program directors. Clin J Am Soc Nephrol 12: 518–523, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rope RW, Pivert KA, Parker MG, Sozio SM, Merell SB: Education in nephrology fellowship: A survey-based needs assessment. J Am Soc Nephrol 28: 1983–1990, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tonelli M, Wiebe N, Manns BJ, Klarenbach SW, James MT, Ravani P, Pannu N, Himmelfarb J, Hemmelgarn BR: Comparison of the complexity of patients seen by different medical subspecialists in a universal health care system [published correction appears in JAMA Netw (Open) 2: e190147, 2019]. JAMA Netw (Open) 1: e184852, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams DC, Warren RW, Ebeling M, Andrews AL, Teufel Ii RJ: Physician use of electronic health records: Survey study assessing factors associated with provider reported satisfaction and perceived patient impact. JMIR Med Inform 7: e10949, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DesRoches CM, Campbell EG, Rao SR, Donelan K, Ferris TG, Jha A, Kaushal R, Levy DE, Rosenbaum S, Shields AE, Blumenthal D: Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med 359: 50–60, 2008. [DOI] [PubMed] [Google Scholar]
- 34.Larsen E, Fong A, Wernz C, Ratwani RM: Implications of electronic health record downtime: An analysis of patient safety event reports. J Am Med Inform Assoc 25: 187–191, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mazur LM, Mosaly PR, Moore C, Marks L: Association of the usability of electronic health records with cognitive workload and performance levels among physicians. JAMA Netw Open 2: e191709, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, Goeders L, Westbrook J, Tutty M, Blike G: Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties. Ann Intern Med 165: 753–760, 2016. [DOI] [PubMed] [Google Scholar]
- 37.Domaney NM, Torous J, Greenberg WE: Exploring the association between electronic health record use and burnout among psychiatry residents and faculty: A pilot survey study. Acad Psychiatry 42: 648–652, 2018. [DOI] [PubMed] [Google Scholar]
- 38.Droulet BC, Schwede M, Bishop KD, Fischer SA: Compliance and falsification of duty hours: Reports from residents and program directors. J Grad Med Ed 5: 368–373, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wachter R, Goldsmith J: To combat physician burnout and improve care, fix the electronic health record. Harvard Business Review, 2018. Available at: https://hbr.org/2018/03/to-combat-physician-burnout-and-improve-care-fix-the-electronic-health-record. Accessed March 7, 2020
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.