Abstract
Coronavirus disease 2019 (COVID-19) has rapidly evolved into a pandemic, causing a global public health crisis. Many frontline healthcare workers providing ear, nose and throat services have been reported to contract COVID-19 at work. Early during the COVID-19 outbreak, several medical professionals in Otolaryngology-Head and Neck Surgery were infected in Wuhan, China. A series of measures were then taken immediately, which successfully halted the spread of the disease. Here we would like to share the lessons we have learned, and our experience to protect our health care workers during the COVID-19 pandemic.
Keywords: COVID-19, Nosocomial infection, Prevention
Introduction
Since Coronavirus disease 2019 (COVID-19) infection was first described in December 2019, it has rapidly spread worldwide, and become a pandemic and global crisis. The cumulative total number of COVID-19 cases worldwide is increasing exponentially. As of April 3, 2020, there were nearly one million of confirmed COVID-19 cases worldwide. COVID-19, caused by SARS-CoV 2, is a highly infectious respiratory disease, transmitted mainly through droplets and direct contact.1,2 The frontline healthcare workers are thus at high risk of contracting the virus,3 especially in otolaryngology, pulmonary medicine, infectious diseases, and those working in COVID-19 isolation wards. Early during the outbreak, a number of healthcare workers were successively diagnosed with COVID-19 infection in the Department of Otolaryngology-Head and Neck Surgery at one hospital in Wuhan. Most of them were all involved in the care of one ENT patient who was later diagnosed with COVID-19. The Department then took a series of preventive measures immediately. Since then, no more COVID-19 nosocomial infection was observed.
Clinical data
Suspected index patient
A 63 years old male with laryngeal carcinoma was admitted on December 31. Preoperative workup including chest CT did not show changes consistent with COVID-19 infection. A total laryngectomy was performed on January 6th. He started to have productive cough on Jan 15th, and was found to have pharyngo-cutaneous fistula. Wound care was then delivered daily. Since then his respiratory symptoms kept worsening. A chest CT was repeated on the 20th and showed patchy opacification involving bilateral lower lobes. Lab workup included normal total WBC counts with increased neutrophil but decreased lymphocyte counts (20th and 23rd), elevated C-reactive protein (CRP, 23rd) , elevated procalcitonin (23rd), and negative PCR for COVID-19 (26th). He was on antibiotics which improved his symptoms including cough and sputum. On the 28th, the patient started to have a fever (37.9 °C). A repeated chest CT showed worsened bilateral patchy opacification, especially the lower lobes. The patient was immediately placed in isolation. Sputum PCR for COVID-19 was performed which was positive.
Summary: The suspected index patient started to have cough and sputum with bilateral lower lobe opacification, and was diagnosed with pharyngo-cutaneous fistula on postoperative day 9. His first PCR for COVID-19 was negative. However, we could have been a bit more overcautious and suspected possible COVID-19 infection earlier because of the following reasons:(1) the confirmed COVID-19 epidemic in Wuhan at that time; (2) the symptoms of COVID-19 are non-specific; (3) PCR sensitivity was unknown. As such, although the patient's symptoms, lab results and CT results could be due to common postoperative complications, COVID-19 should otherwise be suspected and early isolation and precaution should be executed until it was excluded during the epidemic.
Infections of healthcare workers involving the care of suspected index patient
Doctor A: a 36 years old male presented with productive cough (20th) and fever (38.6 °C, 21st). A chest CT was then obtained, consistent with viral pneumonia. Lab test included elevated neutrophil but normal lymphocyte counts. A COVID-19 pneumonia was later confirmed by positive PCR. He was given oseltamivir, levofloxacin and antipyretic treatment. He is still in isolation as repeated PCR remains positive.
Summary: he rounded on the patient daily and performed wound care for the pharyngocutanenous fistula since Jan 15th. He did not wear a surgical mask and bouffant before Jan 20th except during wound care.
Doctor B: A 30 years old female started to have fever on Jan 30th. A chest CT showed viral pneumonia; however, the PCR for SARS-CoV-2 was negative using nasopharyneal swab.
Summary: She had close contact with Doctor A around Jan 20th. All results of repeated PCR are negative. A COVID-19 pneumonia was suspected and later confirmed by strong positive for IgGin antibody test after she was discharged from the hospital.
Nurse A: A 48 years old female presented with a fever (38 °C) with normal white blood cell count but decreased lymphocyte counts. Her chest CT showed right-middle fibrous foci. The nasopharyngeal swab test for SARS-CoV-2 was positive.
Summary: She had close contact with both the patient and Doctor A.
Nurse B: a 33 years old female was completely asymptomatic but with positive PCR test for COVID-19 on January 24th in COVID-19 screening for all healthcare works.
Summary: She has a history of close contact with Nurse A before the 23rd.
A case of unclear source of infection
Nurse C: a 25 years old female presented with cough, hyposmia, headache, and fatigue around Jan13th. Her symptoms disappeared quickly within a few days. She had positive PCR test for COVID-19 on the January 25th in COVID-19 screening for all healthcare works.
Summary: She had no direct contact with the suspected index patient, or the aforementioned healthcare providers.
Our strategies and discussion
After this event, we first asked the following questions. (1) Since the clinical manifestations of COVID-19 are non-specific, when should a possible COVID-19 be clinically suspected? (2) What are the strategies to prevent cross-infection among COVID-19 patients, their direct healthcare providers, non-COVID patients and other healthcare workers within the Department and hospital? (3) What is the appropriate personal protective equipment?
COVID-19, caused by SARS-CoV-2 (severe acute respiratory syndrome coronavirus), shares high amino-acid sequence homology with SARS-CoV. Based on the experience with SARS outbreak, the factors affecting COVID-19 infection risks among healthcare workers include: (1) if there is a rapid administrative management team; (2) if healthcare workers are familiar with respiratory-borne diseases; (3) if there are appropriate medical facilities and essential PPEs.4 Rapid administrative management includes immediate recognition of a possible outbreak, rapid response, development of strategies for nosocomial infection prevention and control, preparation and distribution of essential medical supplies, and mobilization of healthcare workers. Education of healthcare workers on infectious diseases includes infection control strategies and skills, physical and psychological readiness of medical staff. Preparation of appropriate medical facilities should meet the needs to manage infectious diseases, to provide appropriate PPEs. Among them, rapid administrative management is central. Its efficiency determines the other factors. After we recognized these three factors, the following measures were taken immediately.
At the level of administration, an Emergency Incident Command System (EICS) was established immediately. The members of EICS included the department chair, chief nurse manager, representative medical professionals including both physicians and nurses. This helped efficiently utilize the existing resources, develop plan for communication and assignment of medical staff, obtain updated information from CDC and central government, and assure an efficient and well-coordinated teamwork to combat COVID-19.
In case of a healthcare worker was suspected or confirmed to have COVID-19 infection, rapid assessment and staff assignment at the departmental level was performed by the EICS. Isolation was immediately implemented to contain the infection. Internal investigation was immediately initiated to trace the contact history of that individual to avoid further nosocomial spread. A smartphone App was developed for this purpose. For disease screening, chest CT has the highest sensitivity. A PCR cannot rule out COVID-19 infection. All staff within the Department and the hospital administration was notified. Based on the contact tracing, individuals at risk were screened by chest CT and PCR. Regardless of the results, those who had direct contact with suspected or confirmed COVID-19 case were isolated for at least 14 days.1 Strict isolation policy was implemented throughout the period of outbreak. Suspected COIVD-19 patients were only managed by a designated healthcare provider team.
Early during the COVID-19 outbreak, the majority of ENT healthcare workers were unfamiliar with respiratory-borne infectious diseases. In China, COVID-19 is classified as class-B infectious diseases. However, it has been managed as class-A infectious diseases due to its high infectivity. In order to keep our medical team updated on rapidly evolving information on COVID-19, a designated team was appointed to obtain updated information including guidelines. This information was delivered to each individual within the Department on a daily basis. In addition, due to the significant psychological stress among healthcare workers during the COVID-19 pandemic, we delivered several articles including “Guiding Principles of Emergency Psychological Crisis Intervention for COVID-19”, “Guidelines and Guidance of Public Psychological Self-Help for COVID-19'' to every individual within the Department. Meanwhile, a designated team was appointed to help frontline workers with psychological evaluation and coping using telephone, smartphone apps, and questionnaire. These measures dramatically helped release psychologic stress among frontline healthcare workers, improved their mental health, and thus enhanced their confidence in the fight against the epidemic.
In terms of medical staff assignment, those assigned to the designated fever clinics, isolation wards and intensive care units outside the department were mainly managed by the hospital administrative team. Within the Department, if there was a shortage of staff because of isolation, the hospital administration was notified and asked for help.
At the beginning of COVID-19 outbreak, our clinic was immediately closed, and thoroughly disinfected. Stable hospitalized patients were discharged immediately if there was evidence of COVID-19 infection. After this, we divided our wards and clinics into 3 zones: contaminated, potentially contaminated and clean zones. The medial staff and patients entered the medical facilities using separated pathways. The procedures of donning and doffing PPEs were posted in each zone. Efforts were made to assure each individual to understand these procedures. The clean zone included the locker rooms, on call rooms, and stock rooms. The contaminated area included the patient rooms, the wards, endoscopy suites, public restrooms, et al. Potentially contaminated zone included the areas located between the clean and contaminated zones, such as the offices and hallways. In each zone, hand sanitizer, air disinfector, ultraviolet disinfection lamp, and other disinfectant sprays (chlorine-based or 75% alcohol) were provided. According to the “Hospital Air Purification Management Specification (ws/t368.2012)” and “Technical Specification for Disinfection of Medical Institutions (wa/t367.2019)”, disinfection of the instrument surface, floor, and air was carried out daily. Biohazard waste, trash, and those from suspected or confirmed COVID-19 cases were strictly managed and disposed separately. After the completion of this setup, we gradually opened the outpatient clinic.
After we reopened our clinic, all patients were subject to strict screening based on the Diagnosis and Treatment of Pneumonia of New Coronavirus Infection (Trial Fifth Edition).1 In general, the epidemiologic and clinical history was collected. If any suspicion arose, chest CT was then obtained, following by PCR test for COVID-19. In addition, the patient volume was controlled to minimize the risk of cross-infection.
For clinical procedures, the following were implemented to minimize the risk of contracting virus among medical professionals:5
-
(1)
For anterior rhinoscopy and oropharyngeal examination using head mirror, level Ⅱ or Ⅲ protection was recommended, which includes disposable bouffant, surgical masks or protective masks, safety goggles, white coat or scrubs, and disposable fluid-resistant or non-fluid resistant gown, disposable examination gloves.
-
(2)
For epistaxis, traumatic wound debridement including laceration repair, anterior nasal packing, wound care for pharyngoctaneous fistula, tracheostomy care, level Ⅲ protection was recommended, which includes face shield or PAPR plus level Ⅱ protection.6 In addition, after completion of the procedure and correct doffing, we also recommended sinus rinse, mouth rinse, showering, disinfection of the ear canal using 75% alcohol swab.5
-
(3)
For nasal or laryngopharyngeal endoscopy, because of the high chances of generating aerosols, we strictly avoided unnecessary endoscopic examination. In addition, these procedures must be performed with appropriate PPEs with adequate topical anesthesia to minimize sneezing or nausea. In addition, the procedure should be completed quickly. The patient should wear a surgical mask. If the patient had frequent sneezing, coughing, nausea or vomiting, the room was disinfected using ultraviolet ray for 15 min immediately before next patient. In addition, one medical provider was allowed in the room to perform the entire procedure. A minimal interval between two patients should be at least 10 min. For emergencies and those could not be postponed, including pharyngeal foreign body, suspected head and neck cancer based on imaging studies, severe epistaxis, et al, clinical history including recent or current fever, travel and contact history should be obtained. Chest CT was recommended for COVID-19 screening. If CT result did not support COVID-19 infection, the procedures were proceeded with adequate protection. The patient was also informed of the potential risk of infection. If COVID-19 was suspected or diagnosed, it should be immediately reported. The care for this individual patient should be transferred to designated COVID-19 hospitals with level Ⅲ protection as describe in the context.
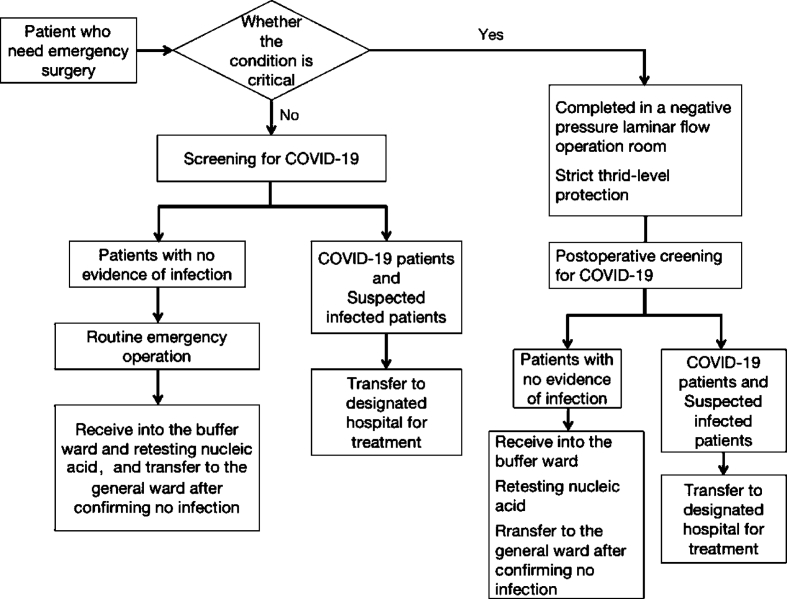
For emergency cases requiring operative room, we first stratified the acuity. For life-threatening emergencies including airway obstruction, foreign body aspiration, major trauma, etc., COVID-19 screening should not be attempted. The surgery should be proceeded immediately as indicated with level Ⅲprotection. For other urgent cases, COVID-19 screening should be performed preoperatively. These include esophageal foreign body, EAC foreign body, non-life-threatening trauma, incision and drainage without airway compromise, uncontrolled recurrent nosebleed, and other inflammatory and neoplastic diseases warranting surgical intervention. Fig. 1 illustrates our triage protocol. Since many patients with COVID-19 are asymptomatic and possible false negative preoperative screening test, for suspected cases, repeated screen tests including chest CT and/or PCR should be performed postoperatively.
Fig. 1.
Emergency procedure of ENT surgery during a new coronavirus epidemic.
For emergency cases under general anesthesia which have unknown COVID-19 status or have not been tested but have high-risk factors such as symptomatic or contact with.
COVID-19 positive individuals, we recommend the following:
-
(1)
For traumatic wound debridement, incision and drainage, level Ⅱprotection or above is recommended. In addition, surgical aseptic techniques, safety goggles, N95 mask, double surgical gloves, and disinfection of surgical field with 75% alcohol is recommended.
-
(2)
For upper aerodigestive endoscopic procedures, digestive and respiratory tract endoscopic surgery (esophageal foreign body, tracheal foreign body, epistaxis): We recommend level Ⅲ protection.
-
(3)
For tracheotomy, due to its high risk of aerosol generation, we recommended negative pressure laminar flow operation room, level Ⅲ protection with PAPR. If tracheostomy was performed under general anesthesia, both assisted and spontaneous ventilation was paused right before the trachea was entered. The ventilation was then resumed after cannula was inserted with cuff inflated and circuit being connected. If it was performed under local anesthesia, oxygen can be delivered using a mask which could also cover the nose and mouth. After the tracheal anterior wall was adequately exposed. Hemostasis should be achieved. The patient was then paralysed by anesthesia. The tracheal window was then generated followed by cannula insertion, cuff inflation and circuit connection. Assisted ventilation was then started. During the case is after tracheotomy made, the risk is highest. Cuffed non-fenestrated trach tube should be used to avoid aerosolization. We also can create a tent over the surgical site with a clear see-through plastic trap particles from being released into the environment.
Besides, we should not forget proper hand hygiene, which is also important. We should pay even more attention during doffing PPE to prevent contamination. During emergency surgery, only essential personnel should be in the room.
Summary
COVID-19 is a highly infectious disease. Because COVID-19 patient can be asymptomatic or have a long incubation, the practice in Otolaryngology-Head and Neck will be very challenging. As such, it is necessary for otolaryngologists to have a better understanding of this diseases, to develop plans to minimize the risk of contract the virus. On February 2, 2020, the Chinese Journal of OHNS published the guidelines to protect Otolaryngologists during COVID-19 pandemic.7 Since Wuhan was the epicenter of COVID-19 outbreak in China, we like to share our experience in this regard, and hope it can help our otolaryngology colleagues worldwide to better protect themselves, their family and their patients.
Declaration of Competing Interest
There are no conflicts of interest.
Edited by Jie Gao
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.General Office of National Health Committee Office of state administration of traditional Chinese medicine. Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019-nCoV) infected pneumonia (trial fifth edition) 2020-02-26. http://bgs.satcm.gov.cn/zhengcewenjian/2020-02-06/12847.html [EB/OL]
- 2.Holshue M.L., DeBolt C., Lindquist S. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rajakaruna SJ, Liu WB, Ding YB, Cao GW. Strategy and technology to prevent hospital-acquired infections: lessons from SARS, Ebola, and MERS in Asia and West Africa. Mil Med Res. 2017;4:32. doi: 10.1186/s40779-017-0142-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Otorhinolaryngology, Head and Neck Surgery Society of Chinese Medical Doctor Association Occupation prevention and control novel coronavirus infection among medical staff in otolaryngology head and neck surgery. 2020. https://mp.weixin.qq.com/s/S1vlPnou1psLUqS5-akdCA
- 6.National Health and Family Planning Commission of the people's Republic of China Prevention and control of nosocomial infection by air borne diseases [EB/OL] 2016. http://www.whcdc.org/wcs/Upload/201808/5b84eeb4d8b5b.pdf
- 7.Xu K, Lai XQ, Liu Z. Suggestions for prevention of 2019 novel coronavirus infection in otolaryngology head and neck surgery medical staff. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2020;55:313–315. doi: 10.3760/cma.j.issn.1673-0860.2020.0001. [DOI] [PubMed] [Google Scholar]