Abstract
Coronavirus disease-19 (COVID-19) is a pathogen that has shown an ability for sustained community transmission. To ensure utmost safety, radiology services will need to adapt to this disease in the coming months and possibly years ahead. This will include learning how to perform radiographs and CT in a safe and sustainable manner. Due to the risk of nosocomial spread of disease, the judicious use and implementation of strict infection protocols is paramount to limit healthcare worker and patient transmission. Between 28 January 2020 and 8 June 2020, our institution performed 12,034 radiographs and 178 CT scans for suspected or confirmed COVID-19 patients. As of 8 June 2020, there have been no documented instances of healthcare staff acquiring COVID-19 during the course of work. In this article, we present the indications and operational considerations used by our institution to safely image patients with suspected or confirmed COVID-19. Alternative practices for imaging radiographs are also discussed.
Key Words: COVID-19, chest, radiography, computed tomography
Introduction
Coronavirus disease-2019 (COVID-19) is an acute infectious disease that can cause severe viral pneumonia. Genomic sequencing has characterized the pathogen as SARS-CoV-2, a novel human coronavirus related to SARS-CoV, and MERS-CoV (1). Singapore saw its first case of COVID-19 on 23 January 2020, and as of 6 June 2020 has over 37,000 cases and 24 fatalities (2). Globally, there are more than 6.4 million COVID-19 cases with over 383,000 deaths (6 June 2020).
The prevention of healthcare staff and patients from contracting COVID-19, while maintaining continuity of services, is vital in ensuring continued healthcare provision during the pandemic. In a COVID-19 situation report published by the World Health Organization, it was reported that up until 8 April 2020, there were 22,073 healthcare workers from 52 countries infected with COVID-19 (3). The purported infected toll may be a vast under-representation (4). Intra-hospital healthcare worker transmission has been linked to limited access to and inappropriate use of personal protective equipment, prolonged contact with infected patients, and lack of adequate infection control protocols (5, 6, 7). Given that many suspected or confirmed COVID-19 patients require some form of imaging in their course of diagnosis and treatment, the radiology department represents a significant site of potential spread.
While some have described measures taken to enhance radiology preparedness during this pandemic (8, 9, 10, 11), there remains a lack of specific guidelines and protocols describing how to safely perform imaging on COVID-19 patients that can be widely applied across institutions of various capabilities. This is of particular concern in developing countries where chest radiographs may be more widely utilized compared to reverse transcriptase-polymerase chain reaction (RT-PCR) and a lack of infection control and radiographic protocols may prove detrimental (12).
In this article, we describe the operational protocols used by Singapore General Hospital, a 1785 bed acute tertiary referral centre, to safely image patients with suspected or confirmed COVID-19. Our diagnostic radiology service consists of 59 diagnostic radiologists, 273 radiographers and 240 other staff members, including nurses and support staff. A total of 7 CT scanners are available, with 1 located in the emergency department (ED), 3 in the outpatient imaging centre and 3 in the inpatient imaging centre, of which 1 is equipped with negative pressure capability. There are 13 portable radiography units available with 4 allocated for use in the ED and 9 for use in the wards.
The operational imaging protocols as described in this article have been developed by the radiology and infectious disease departments of our hospital, in accordance with the relevant regulations stipulated by the Singapore Ministry of Health.
Indications for Imaging
The RT-PCR assay is the mainstay of diagnosis locally, consistent with the recommendations set forth by several authorities (11,13,14). However, both radiography and CT imaging can also play a crucial role in triage, management, and follow up of suspected and confirmed COVID-19 patients (14, 15, 16, 17, 18, 19).
Our institution aims to facilitate expeditious detection and disposition of patients with suspected or confirmed COVID-19. While the turnaround time for PCR testing has improved from the start of the pandemic, test results may require up to 4–6 hours to process in our institution. While awaiting PCR results, we have been utilizing chest radiographs as part of a triage tool to determine patient disposition. Chest radiographs have been shown to be independent predictors of risk for hospital admission and intubation and radiographic findings can precede RT-PCR positivity in 9% of cases (19,20).
A multidisciplinary diagnostic triage algorithm, utilizing symptomatology, epidemiological risk factors and chest radiography, was created to risk stratify patients at first presentation (21) (Fig 1 a). This incorporates a continually updated national criteria containing the local case definition defined by the Singapore Ministry of Health (Fig 1b), as well as a set of internal screen criteria developed by our infectious disease specialists to further incorporate evolving trends in our population, such as emerging clusters (Fig 1c). All patients presenting with acute respiratory symptoms receive a chest radiograph in the ED and designated screening areas. Radiographs, both chest and others, are also performed for inpatients that develop new symptoms, for follow-up purposes, or for other non–COVID-19-related emergent conditions (11,13).
Figure 1.
(a) Triage algorithm for patients presenting with acute respiratory symptoms. It relies largely on symptomology, epidemiological factors, chest radiography and PCR testing. Chest CT is only performed on select patients with a persistent high clinical suspicion of COVID-19 but have normal initial chest radiographs and PCR results. (b) Singapore Ministry of Health National Criteria for COVID-19, as of 12 May 2020. This is continually updated during the outbreak, as new information is brought to light. (c) Singapore General Hospital Internal Screen Criteria for COVID-19, as of 11 May 2020. This has been developed to enhance detection of suspect cases not captured by the national criteria.
The use of chest CT in our institution has been limited to instances where the diagnosis is uncertain, such as a mismatch between clinical suspicion and RT-PCR results, or to add value to management (11,13). Examples include identification of disease complications or disease progression. Other forms of targeted CT imaging are also utilized in both suspected and confirmed COVID-19 cases that may have other emergent pathology such as stroke or acute appendicitis. These scans are scheduled after a discussion between radiology and the clinical teams to ensure only CT studies that can provide information to guide or alter management are performed. Other non-emergent CT imaging is delayed until the patient is cleared of COVID-19.
Segregation of Patient Areas
To minimize the risk of cross-contamination between suspect and non-suspect patients, the ED was divided into “Fever” and “Non-Fever” areas to physically separate patients with fever or acute respiratory symptoms from those without symptoms. The Ambulatory Surgical Centre and a parking garage within the hospital compound were converted to additional “Fever” areas to cater to the growing demand for triage.
Patients requiring admission are admitted to one of three wards, namely, a high-risk ward for confirmed cases and patients with a high suspicion of disease, an intermediate-risk ward for patients with COVID-19-like symptoms but have fewer risk factors and a general ward for patients with no relevant symptoms and are deemed to be low risk.
High-risk wards are equipped with single occupant negative pressure rooms with adjoining anterooms which are negative pressure to the patient's room and the hallway. An intermediate-risk ward comprises single rooms and cohort cubicles, where patients are spaced at least 2.7 metres apart to minimize potential patient to patient transmission. General wards have no additional distancing measures or infection protocols in place. The designated beds for each risk classification vary based on hospital demand.
CT scans for suspected COVID-19 patients are generally not performed in the single CT scanner available within the ED and are delayed until the patient is admitted and can proceed for the scan in the designated inpatient CT scanner with negative-pressure capability. Exceptions to this principle are made only for emergent indications.
Equipment/Environment Disinfection and Personal Protective Equipment (PPE)
Learning from our experiences with SARS in 2003, it is clear that radiology can be a significant source of nosocomial transmission if strict infection control protocols are not in place (22,23). COVID-19 is highly transmissible via respiratory droplets, and the possibility of fomite-mediated transmission is of particular concern for radiology where equipment is routinely used for multiple patients. The virus can remain viable in aerosols for up to 3 hours, and on plastic and stainless steel surfaces up to 72 hours (24). The proper use of PPE and decontaminating protocols are essential when imaging a confirmed or suspect case.
Varying levels of PPE are worn by radiology staff depending on the risk stratification of the patient (Table 1 ). All healthcare staff should undergo N95 mask fit tests and comprehensive training sessions before working in areas requiring PPE.
Table 1.
Staff Personal Protective Equipment (PPE) Required for Various Patient Risk Categories
 |
Staff don varying extent of PPE depending on patients risk level in the wards and ED.
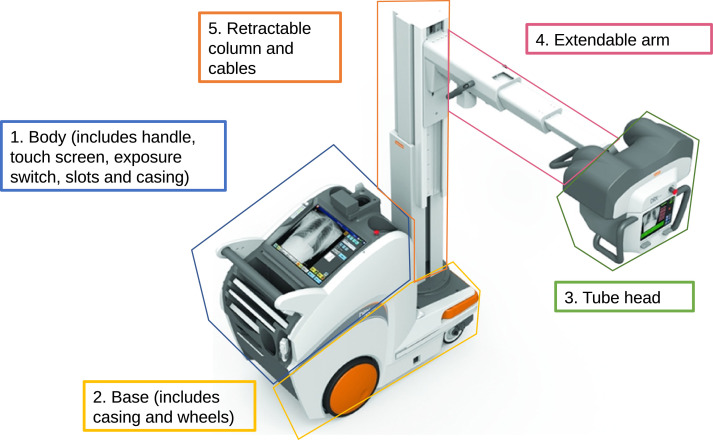
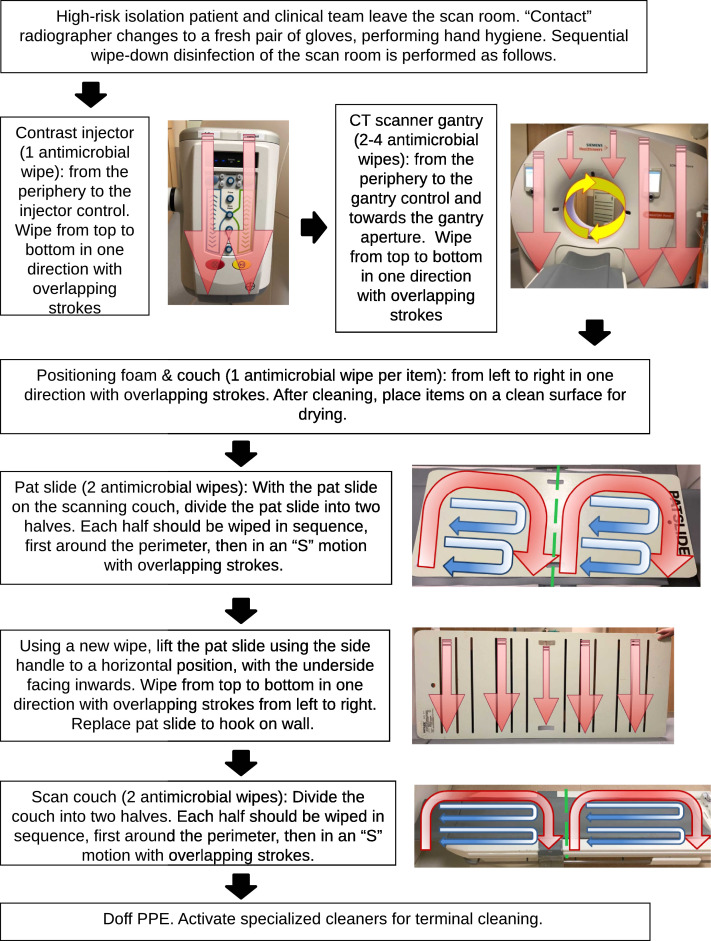
Given that radiology equipment contains multiple moving and electronic components, it cannot be easily sterilized by conventional means. The short turnaround time required during surge demand also limits the duration of disinfection. Each piece of equipment, such as a portable radiography machine, is divided into sections and each area wiped down with a fresh anti-microbial wipe according to a fixed cleaning regime. Our institution uses Wip'Anios Excel wipes (Laboratoire ANIOS, Lille-Hellemmes, France) containing a disinfecting solution of Didecyldimethylammonium chloride. Examples of cleaning sections include the base of the unit, including wheels and casing, and the x-ray tube head (Fig 2 ). A similar protocol is available for the cleaning of CT scan rooms and machines (Fig 3 ). Terminal cleaning by specialized cleaners from the environmental services department is performed with Sodium hypochlorite 1000 ppm solution and ultraviolet (UV-C) irradiation.
Figure 2.
Cleaning protocol for portable radiography unit. Each color-coded area indicates a single cleaning section that should be disinfected with a fresh antimicrobial wipe.
Figure 3.
Cleaning protocol for CT scan room. The disinfection protocol was developed in collaboration with the hospital infection control and radiography teams.
Workflow for Chest Radiography
Radiography services for patients from general wards are provided in accordance with routine pre-COVID-19 imaging workflows with standard PPE. This includes wipe-down of patient contact surfaces and adhering to strict hand hygiene practices. Terminal cleaning is not required.
Only portable radiography services are provided for patients in high- or intermediate-risk wards to limit patient transfers and the risk of cross infection. In designated “Fever” areas in the ED or converted hospital areas, a portable radiography machine is stationed at a fixed location where all patients are imaged. Terminal cleaning of the room is performed twice a day.
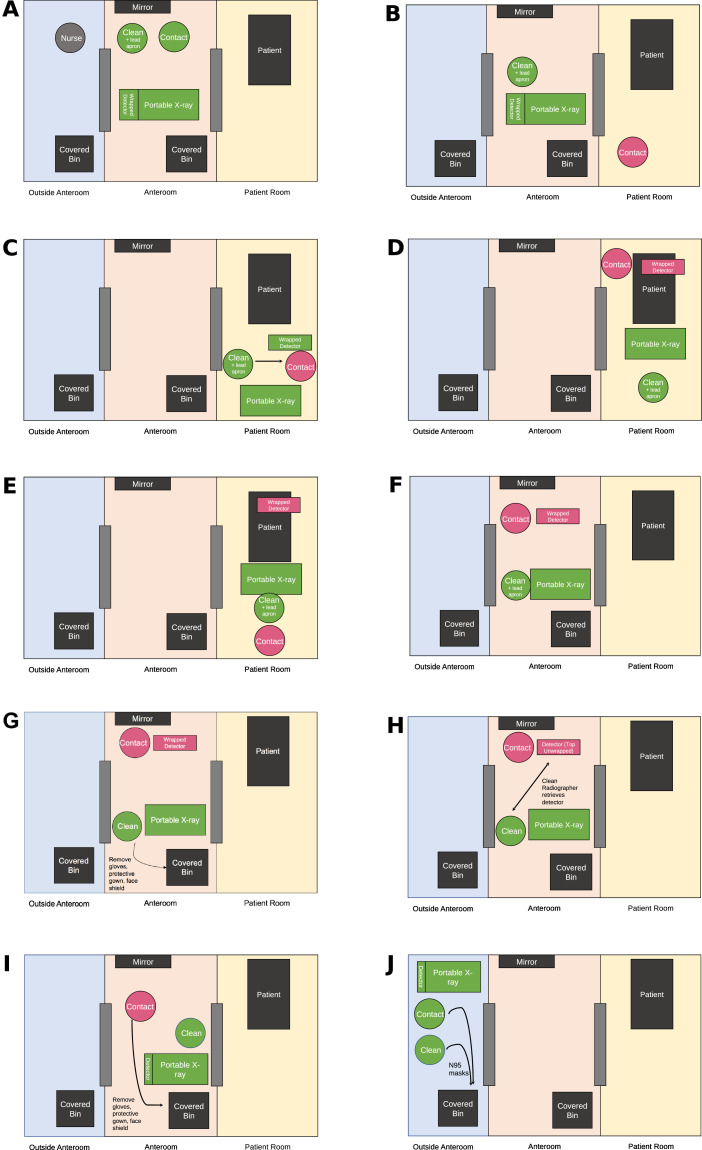
Radiographers work in pairs, with a designated “clean” radiographer with no direct contact with the patient, and a “contact” radiographer who interacts directly with the patient. Isolation ward anterooms are equipped with hand sanitizers, PPE, mirrors, and hospital approved antimicrobial wipes. Wipe-down decontamination is performed for any equipment transferred between the patient's isolation room and external areas.
We describe the protocol used for portable radiography used in our isolation wards. For institutions without anterooms, anteroom procedures can be performed in the area immediately outside of the isolation room. Alternative steps for imaging performed at a fixed designated location such as screening areas in the ED are also included.
Preparation
-
1“Clean” radiographer wears a lead apron. Both radiographers don PPE. Radiographers perform visual inspection with the aid of a mirror and a buddy system. In certain wards, an infectious control nurse visually checks PPE from outside the anteroom (Fig 4 a).
-
aPortable – don PPE outside the anteroom.
-
bFixed location – don PPE in the examination room prior to patient arrival.
-
a
-
2
Both radiographers enter the anteroom with the portable unit.
-
3Preparing the detector
-
aPortable – the detector is wrapped completely in fluid-impermeable plastic (Fig 4a).
-
bFixed location – wrapping of the detector is not required.
-
a
-
4Confirmation of two patient identifiers and the radiographic examination with a read back.
-
aPortable – “Contact” radiographer proceeds into the isolation room and confirms relevant information. “Clean” radiographer performs a read back to “contact” radiographer (Fig 4b). “Clean radiographer” then enters the isolation room with the portable machine and hands the wrapped detector to “contact” radiographer (Fig 4c).
-
bFixed location – Patient enters examination room. Confirmation is performed within the room.
-
a
Figure 4.
General radiography workflow for an isolation room with anteroom facilities. Caption: Diagramatic representation of radiographer movement and PPE donning and doffing regime in the workflow for chest radiography of a patient with suspected or confirmed COVID-19. In the absence of anterooms, anteroom procedures can be performed immediately outside the isolation room. A similar workflow can be adapted for imaging performed at a fixed location such as in the emergency department.
Performing the Exposure
After Completion of the Exposure
-
1Leaving the room
-
aPortable – Radiographers exit the isolation room into the ante-room together. “Contact” radiographer holds the wrapped detector while “clean” radiographer handles the portable machine (Fig 4f).
-
bFixed location – the patient leaves the examination room.
-
a
-
2
“Clean” radiographer doffs surgical gloves, protective gown and face shield with appropriate hand hygiene measures, and puts on a fresh pair of surgical gloves.
-
3
“Clean” radiographer wipes down the detector slot (Fig 4g).
-
4Retrieval of detector
- a
-
bFixed location – “Contact” radiographer retrieves non-wrapped detector from fixed position.
-
5
The detector is wiped down and placed into the detector slot. Images are uploaded wirelessly.
-
6
“Contact” radiographer doffs surgical gloves and protective gown with appropriate hand hygiene measures, and puts on a fresh pair of surgical gloves (Fig 4i).
-
7
Both radiographers perform thorough surface cleaning of the machine according to a fixed regime (Fig 2). Surgical gloves are disposed and hand hygiene is performed.
-
8
The “clean” radiographer dons a new pair of gloves after hand hygiene. The lead apron is removed, wiped with an antimicrobial wipe and returned to a designated hanger on the portable machine.
-
9
The “contact” radiographer processes the images for wireless upload.
-
10
Where applicable, radiographers exit the anteroom with the portable machine (Fig 4j). N95 masks and goggles or face shields are retained between patients and can be used for up to 4 hours unless soiled. If no further imaging procedures are required, the N95 masks are removed and stored in a new Ziplock bag or container for reuse, or disposed in covered bins. Hand hygiene is performed after removal.
The implementation of the described enhanced infection control protocols results in a longer turnaround time for each imaging procedure. The total turnaround time for portable imaging of a patient in an isolation ward with anteroom and an isolation ward without an anteroom is 25 and 15 minutes, respectively. The turnaround time at a fixed location such as our ED is 15 minutes.
Workflow for CT
Standard PPE and routine pre-COVID-19 imaging workflows are utilized when imaging patients from general wards. This includes wipe-down of patient contact surfaces and performing strict hand hygiene. During contact with patients from intermediate-risk wards, staff don full PPE and proceed with routine pre-COVID-19 workflows. Terminal cleaning is not performed for our general or intermediate-risk wards.
The radiology team involved consists of a radiologist, two radiographers, a radiology nurse and a patient porter. The “contact” radiographer dons full PPE and enters the scan room. The nurse and remaining “clean” radiographer don N95 masks only, and are deployed within the control room which is designated as a “clean” room with no contact with the patient or clinical team from the ward. Scans from intermediate- and high-risk wards are performed in a negative-pressure CT scan room when possible.
Preparation
-
1
Non-essential furniture such as non-mounted storage cabinets or additional cushions are moved out of the CT scan room (Fig 5 a). Protective plastic sheets are placed over “high touch” areas in the CT scan room such as the scanner table.
-
2
Security and cleaning staff don full PPE and standby along a designated transport route from high-risk ward to Radiology.
-
3
Access to the scan room is restricted with placement of signs to direct traffic flow away from the room.
-
4
The primary clinician and/or the duty radiologist don N95 masks and standby within the control room with the “clean” radiographer and a nurse.
-
5
A patient porter is dispatched to the COVID-19 ward to fetch the patient.
Figure 5.
CT workflow for patients from high-risk isolation wards. Caption: Position and movement of patient, radiographers and other staff involved in the imaging of a patient with suspected or confirmed COVID-19. This is performed in a CT scan room with negative pressure capability
Transporting the Patient to Radiology
-
1
The porter dons full PPE at the ward (Fig 5b).
-
2
The security team blocks off designated lifts and clears traffic along the assigned transport route.
-
3
The porter and ward team transport the patient to Radiology. Throughout transport, the patient wears a surgical mask.
-
4
Following closely, cleaning staff commence surface decontamination along the travelled route.
-
5
The patient is transferred to the scan table for CT.
-
6
“Contact” radiographer and ward team wait outside the scan room while the scan is performed by the “clean” radiographer in the control room.
After Completion of the Scan
-
1
The duty radiologist will review the scan images to ensure that the scan performed is adequate to answer the clinical question at hand.
-
2
The patient is transported back to the ward by the porter and ward team via the designated route. Cleaning staff will again follow closely to perform surface decontamination (Fig 5c).
-
3
Once the patient has left the department, “contact” radiographer begins a wipe-down of equipment according to a fixed regime (Fig 3). After completion, the “contact” radiographer doffs PPE with appropriate hand hygiene.
-
4
A specialized team of cleaners will then commence terminal cleaning of the CT scan room (Fig 5d).
For CT imaging, the total turnaround time to image a patient from a high-risk ward is significantly longer at 90–120 minutes compared to 30 minutes for patients from general or intermediate-risk wards. We have found that in situ simulation was useful in identifying procedural gaps, increasing efficiency, patient safety and overall familiarity and confidence with the new workflow.
Alternative Practices and Future Directions
An alternative radiographic imaging protocol obtaining chest radiography through a glass door or across a semi-isolation anteroom has been previously described (13). This protocol has the advantage of reducing exposure to the radiographer who remains entirely outside the isolation room with the portable machine while a trained ward nurse assists with positioning of the patient and cassette. The use of PPE is also reduced. However, the feasibility of this protocol requires a suitable infrastructure configuration where there is adequate distance between the portable machine in the anteroom and the patient in the isolation room to produce satisfactory radiographs. This may not always be possible and structural amendments are difficult to actualize in a short period of time. Comparatively, the imaging protocols we have described can be implemented across a variety of infrastructural configurations including isolation wards with or without anterooms, as well as fixed locations with high patient load such as the EDs.
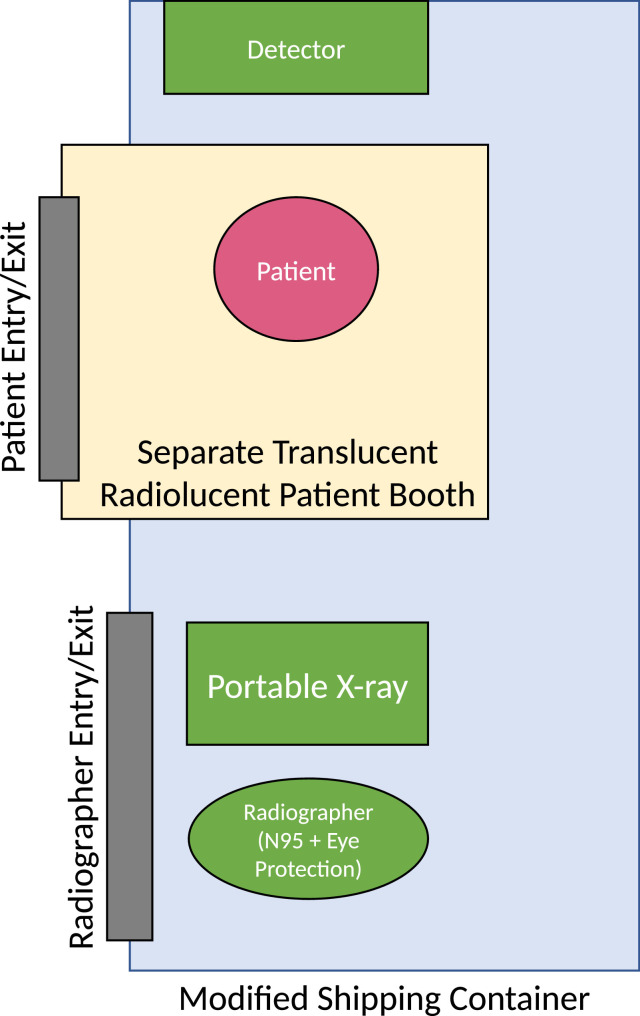
In our expanded “Fever” area converted from the existing parking garage, we have implemented a modified container-based chest radiography unit (Teo et al, unpublished work, 2020). This standard-sized shipping container houses a portable radiography x-ray unit. However, instead of directly entering the main container compartment, the patient enters a separate sealed transparent radiolucent booth which protrudes into the main container compartment. In this way, the patient can enter the path of the x-ray beam and undergo chest radiography, while remaining separate from the radiographer in the main container compartment (Fig 6 ). The detector remains in the main container posterior to the booth and the patient. This reduces the use of PPE, but the set-up is only feasible in temporary or semi-permanent areas which can be purpose-built or modified in order to allow implementation of separate entrances into each of these spaces (patient booth, and the main container) while optimizing the layout for satisfactory radiographs.
Figure 6.
Diagram of modified container-based chest radiography unit. The standard-sized shipping container houses a portable radiography x-ray unit. The patient enters a separate sealed transparent radiolucent booth which protrudes into the main container compartment.
Adjunct Measures to Mitigate Inadvertent Exposure
COVID-19 has been shown to have a pre-symptomatic phase where patients have the potential to transmit the virus despite the lack of symptoms and remaining undiagnosed (25). In addition, PCR testing may produce false-negative results (26). In order to minimize inadvertent exposure and transmission to staff and patients, several other measures have been put in place.
Due to the robust contact tracing done in Singapore, contacts of a positive case are rapidly placed in quarantine and clusters of cases within the community are published daily. This provides epidemiological background for the current risk of COVID-19 cases in our community. Within our institution, frontline administrative staff and clinicians take a relevant epidemiological history on top of assessing for any relevant clinical symptoms (27). As such, even if patients are asymptomatic, those with high epidemiological risk are identified and placed in an intermediate-risk ward with enhanced precautions.
Since the start of the outbreak, our institution has required all healthcare professionals to don surgical masks. Patients and visitors are required to don either surgical masks or cloth-based face masks. Restriction of visitors to all inpatients has been put in place since the start of the outbreak, reducing the risk of spread in the wards. Safe distancing measures such as segregation of teams as well as physical distancing in common staff areas such as the staff pantry have served to further mitigate the risk of inadvertent spread amongst healthcare workers (28). Staff education and an emphasis on strict hand hygiene measures have also helped to raise the level of compliance to implemented changes.
Summary
Between 28 January 2020 and 8 June 2020, our institution has cared for 1338 confirmed COVID-19 patients and performed 12,034 radiographs and 178 CT scans for suspected or confirmed COVID-19 patients. To date (6 June 2020), there have been no documented instances of healthcare staff becoming infected with COVID-19 during their course of work.
In the midst of the COVID-19 pandemic, radiology services need to prevent disease dissemination in the department and maintain efficient turnaround times and adequate imaging capacity, while implementing enhanced infection protocols. We have continually modified our practice as the disease evolves and new information comes to light. Appropriate use of imaging, enhanced workflows with emphasis on infection control, as well as sustained efforts by all staff in complying with measures, are all critical to minimize infection transmission in the radiology department (29).
We hope that our experiences and modality-specific protocols will help others evaluate and shape their own department protocols in response to the ongoing pandemic.
Acknowledgments
Acknowledgements
The authors would like to acknowledge the Singapore General Hospital Division of Radiological Sciences and clinicians in Singhealth for their efforts in the face of the COVID-19 pandemic, Ms Tiong Mee Ling for her invaluable help in obtaining relevant statistics for this paper as well as Ooi Xian Hua, Low Mian You, Lee Kuan-Ming, Jan Tyrone Lee Mendalla, Benjamin Eu, Kang Xiuqing Samantha, Lim Chong Yeu Colin, Lin Wei-Chen, Lee Lai Chee and Dr Ling Moi Lin for their assistance and time in filming the accompanying videos.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.acra.2020.06.022.
Appendix. Supplementary materials
References
- 1.Lu R, Zhao X, Li J. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UCA. COVID-19 Singapore Dashboard 2020. https://co.vid19.sg/. (Accessed May 12, 2020).
- 3.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report-82 2020. https://doi.org/10.1101/2020.03.23.20041913. Accessed May 15, 2020.
- 4.International Council of Nurses. ICN calls for data on healthcare worker infection rates and deaths | ICN - International Council of Nurses 2020. https://www.icn.ch/news/icn-calls-data-healthcare-worker-infection-rates-and-deaths. Accessed June 9, 2020.
- 5.Feng Tan LI. Preventing the transmission of COVID-19 amongst healthcare workers. J Hosp Infect. 2020:19–20. doi: 10.1016/j.jhin.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020;105:100–101. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu J, Ding N, Chen H. Infection control against COVID-19 in Departments of Radiology. Acad Radiol. 2020;27:614–617. doi: 10.1016/j.acra.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gutzeit A, Li Q, Matoori S. What can European radiologists learn from the outbreak of COVID-19 in China? A discussion with a radiologist from Wuhan. Eur Radiol. 2020 doi: 10.1007/s00330-020-06841-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ding J, Fu H, Liu Y. Prevention and control measures in radiology department for COVID-19. Eur Radiol. 2020 doi: 10.1007/s00330-020-06850-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Politi LS, Balzarini L. The Radiology Department during the COVID-19 pandemic: a challenging, radical change. Eur Radiol. 2020:4–6. doi: 10.1007/s00330-020-06871-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mossa-Basha M, Azadi J, Ko J, Klein J, Meltzer C, Force C-19. RSNA COVID-19 Task Force: Best Practices for Radiology Departments during COVID-19. 2020
- 12.Joob B, Wiwanitkit V. Radiology management and COVID-19 in resource limited setting. Acad Radiol. 2020;27:750. doi: 10.1016/j.acra.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mossa-Basha M, Medverd J, Linnau K. Policies and guidelines for COVID-19 preparedness: experiences from the University of Washington. Radiology. 2020 doi: 10.1148/radiol.2020201326. [DOI] [PubMed] [Google Scholar]
- 14.Borghesi A., Maroldi R. COVID-19 outbreak in Italy: experimental chest X-ray scoring system for quantifying and monitoring disease progression. Radiol Med. 2020;125:509–513. doi: 10.1007/s11547-020-01200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanne JP, Little BP, Chung JH. Essentials for radiologists on COVID-19: an update—radiology scientific expert panel. Radiology. 2020 doi: 10.1148/radiol.2020200527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duan Y, Qin J. Pre- and posttreatment chest CT findings: 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim H. Outbreak of novel coronavirus (COVID-19): what is the role of radiologists? Eur Radiol. 2020:13–14. doi: 10.1007/s00330-020-06748-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hosseiny M, Kooraki S, Gholamrezanezhad A. Radiology perspective of coronavirus disease 2019 (COVID-19): lessons from severe acute respiratory syndrome and middle east respiratory syndrome. Am J Roentgenol. 2020:1–5. doi: 10.2214/AJR.20.22969. [DOI] [PubMed] [Google Scholar]
- 19.Toussie D, Voutsinas N, Finkelstein M. Clinical and chest radiography features determine patient outcomes in young and middle age adults with COVID-19. Radiology. 2020 doi: 10.1148/radiol.2020201754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong HYF, Lam HYS, Fong AH-T. Frequency and Distribution of Chest Radiographic Findings in COVID-19 Positive Patients. Radiology. 2020:201160. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wee LE, Fua T-P, Chua YY. Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med. 2020 doi: 10.1111/acem.13984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gogna A, Tay KH, Tan BS. Severe acute respiratory syndrome: 11 years later—a radiology perspective. Am J Roentgenol. 2014;203:746–748. doi: 10.2214/AJR.14.13062. [DOI] [PubMed] [Google Scholar]
- 23.Cheng LT-E, Chan LP, Tan BH. Déjà Vu or Jamais Vu? How the severe acute respiratory syndrome experience influenced a Singapore Radiology Department's response to the coronavirus disease (COVID-19) epidemic. Am J Roentgenol. 2020:1–5. doi: 10.2214/AJR.20.22927. [DOI] [PubMed] [Google Scholar]
- 24.van Doremalen N, Bushmaker T, Morris DH. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wei WE, Li Z, Chiew CJ. Presymptomatic transmission of SARS-CoV-2 Singapore. Morb Mortal Wkly Rep. 2020;69:411–415. doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Woloshin S, Patel N, Kesselheim AS. False negative tests for SARS-CoV-2 infection—challenges and implications. N Engl J Med. 2020 doi: 10.1056/NEJMp2015897. [DOI] [PubMed] [Google Scholar]
- 27.Chen RC, Tan TT, Chan LP. Adapting to a new normal? 5 key operational principles for a radiology service facing the COVID-19 pandemic. Eur Radiol. 2020:1–4. doi: 10.1007/s00330-020-06862-1. [published online ahead of print, 2020 Apr 23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen RC, Cheng LT-E, Liang Lim JL. Touch me not: safe distancing in radiology during coronavirus disease 2019 (COVID-19) J Am Coll Radiol. 2020;17:739–742. doi: 10.1016/j.jacr.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mirza SK, Tragon TR, Fukui MB. Microbiology for radiologists: how to minimize infection transmission in the radiology department. Radiographics. 2015;35:1231–1244. doi: 10.1148/rg.2015140034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.