Highlights
-
•
Autoimmune patients and rheumatologists face an unprecedented challenge during the COVID-19 pandemic and are changing medication practices in response.
-
•
About half of US rheumatologists believe COVID-19 risk may be heightened in rheumatic disease patients, regardless of their immunosuppressive medications.
-
•
There were significant differences in the management of biologics, steroids and NSAIDs in response to COVID-19 reported by rheumatologists in areas with a high case burden, compared to those in less affected areas.
Keywords: COVID-19; Survey; Biologics; Steroids; NSAIDs, Rheumatic diseases
Abstract
Objective
To investigate the perceptions and behaviors of rheumatologists in the United States (US) regarding the risk of COVID-19 for their autoimmune patients and the subsequent management of immunosuppressive and anti-inflammatory medications.
Methods
We administered an online survey to a convenience sample of rheumatologists in the US from 4/8/20-5/4/20 via social media and group emails. Survey respondents provided demographic information such as, age, gender, state of practice, and practice type. We asked questions about COVID-19 risk in rheumatic patients, as well as their medication management during the pandemic. We conducted descriptive analysis and Multivariable regression models.
Results
271 respondents completed the survey nationally. 48% of respondents either agreed or strongly agreed with the statement “Patients with rheumatic diseases are at a higher risk of COVID-19 irrespective of their immunosuppressive medications”. 50% disagreed or strongly disagreed with the statement “The pandemic has led you to reduce the use/dosage/frequency of biologics”, while 56% agreed or strongly agreed with the statement “The pandemic has led you to reduce the use/dosage/frequency of steroids”. A third of respondents indicated that at least 10% of their patients had self-discontinued or reduced at least one immunosuppressive medication to mitigate their risk of COVID-19. Responses to these questions as well as to questions regarding NSAID prescription patterns were significantly different in the Northeast region of US compared to other regions.
Conclusion
In this national sample of rheumatologists, there are variations regarding perceptions of patients’ risk of COVID-19, and how to manage medications such as NSAIDs, biologics and steroids during the pandemic. These variations are more pronounced in geographical areas where COVID-19 disease burden was high.
Introduction
The coronavirus disease 2019 (COVID-19) caused by the SARS-CoV2 virus is presenting an unparalleled challenge to the healthcare system and has impacted millions of people, including those with chronic autoimmune conditions.[1] Community transmission of COVID-19 was first detected in the United States in February 2020. While geographical variation in COVID-19 cases and deaths was noted early in the pandemic, by mid-March all fifty states, and four US territories had reported cases of COVID-19.[2] With early reports of a high case fatality rate and increased severity in patients with underlying chronic medical conditions, both rheumatologists and their patients with autoimmune diseases found themselves in a challenging position. Patients with autoimmune conditions may be at a higher risk of infection as a result of their underlying disease, disease activity, comorbidities and/or the immunosuppressive medications used to treat them.[3] While there is no data to ascertain the risk of contracting COVID-19 in these patients, there is some evidence that immunosuppression results in increased viral replication.[4] Thus, in the face of a potentially heightened risk for contracting COVID-19, patients with autoimmune diseases and their physicians have had to discuss possible medication adjustments based on their perceived risk of COVID-19 infection.
The primary objectives of this survey were: 1) to assess rheumatologists’ perceptions of their patients’ risk of COVID-19 infection; 2) to determine whether rheumatologists have altered their practice and medication prescribing behaviors in the context of the COVID-19 pandemic; and 3) to determine whether patients have contacted their rheumatologist to assess their risk and inquire about medication changes.
Methods
Study design
We conducted a survey of rheumatologists from April 8 to May 4, 2020. The sample included both adult and pediatric rheumatologists as well as trainees. The survey was written in English, built on an online platform (surveygizmo.com) and disseminated over social media sites such as LinkedIn, Twitter, Facebook, ResearchGate and WhatsApp. We also distributed the survey by email to rheumatology-specific groups and societies. The survey respondents were kept entirely anonymous. The Institutional Review Board (IRB) of Hospital for Special Surgery (HSS) approved the survey and protocol. Responses were only included if at least 80% of the questionnaire was completed and we report the questions relevant to our in this paper.
We collected sample demographic information such as age, gender, type of practice (adult vs pediatric), and practice setting (academic vs private vs government). To examine regional variations, we categorized US regions as follows: Northeast (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont, New Jersey, New York and Pennsylvania), Midwest (Illinois, Indiana, Michigan, Ohio, Wisconsin, Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota and South Dakota), South (Washington D.C., Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, West Virginia, Alabama, Kentucky, Mississippi, Tennessee, Arkansas, Louisiana, Oklahoma and Texas) and West (Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, Wyoming, Alaska, California, Hawaii, Oregon and Washington).
Statistical analysis
We performed descriptive statistics i.e. frequencies and percentages. Bivariate comparisons were performed using Chi-square and Fisher's exact test for categorical variables and Wilcoxon rank sum and Student's t-test for continuous variables. Multivariable ordinal logistic models with the main exposure as US region (South as the reference group) and the main outcomes as the various survey questions were calculated and adjusted for physician age, gender, adult and pediatric practice, and type of practice setting. We also performed a sensitivity analysis where we excluded all pediatric rheumatologists from the multivariable models given differences in treatment practices and immunosuppressant use to assess if the results were consistent. Statistical significance was determined using an alpha of 0.05 and all analyses were conducted using Stata version 14.
Ethical approval
The Institutional Review Board (IRB) of Hospital for Special Surgery (HSS) approved the survey and protocol (# 2020-0520). In strict adherence to the US federal regulation for IRB exemption, once a response was accepted into the study, it was immediately and permanently anonymized. The response was then given a subject number for identification during the study.
Results
Table 1 summarizes the characteristics of the rheumatologists who participated in the study. Briefly, a total of 271 US rheumatologists answered the survey; of these 114 were from the Northeast (NE), 36 from the Midwest (MW), 90 from the South (S) and 31 from the West (W). The majority (64%) practiced in academic/government-based settings and the rest in private practice (p-value=0.002). Nine percent were pediatric rheumatologists and approximately 3% treated both adults and pediatric populations (p-value=0.22).
Table 1.
Survey respondent characteristics
| Total | Northeast | Midwest | South | West | ||
|---|---|---|---|---|---|---|
| 271 N (%) | 114 N (%) | 36 N (%) | 90 N (%) | 31 N (%) | P value | |
| Age | 0.087 | |||||
| 25-34 | 51 (18.8) | 23 (20.2) | 8 (22.2%) | 12 (13.3%) | 8 (25.8%) | |
| 8 (22.2) | 12 (13.3) | 8 (25.8) | ||||
| 35-44 | 91 (33.6) | 35 (30.7) | 13 (36.1) | 32 (35.6) | 11 (35.5) | |
| 45-54 | 53 (19.6) | 20 (17.5) | 10 (27.8) | 13 (14.4) | 10 (32.3) | |
| 55-64 | 38 (14.0) | 18 (15.8) | 2 (5.6) | 17 (18.9) | 1 (3.2) | |
| 65+ | 38 (14.0) | 18 (15.8) | 3 (8.3) | 16 (17.8) | 1 (3.2) | |
| Gender | 0.600 | |||||
| Female | 156 (57.6) | 65 (57.0) | 21 (58.3) | 48 (53.3) | 22 (71.0) | |
| Male | 92 (33.9) | 42 (36.8) | 11 (30.6) | 32 (35.6) | 7 (22.6) | |
| Do not want to specify | 3 (1.1) | 1 (0.9) | 0 (0.0) | 2 (2.2) | 0 (0.0) | |
| Missing | 20 (7.4) | 6 (5.3) | 4 (11.1) | 8 (8.9) | 2 (6.5) | |
| Practice type | 0.002 | |||||
| Academic/ government | 170 (62.7) | 84 (73.7) | 25 (69.4) | 43 (47.8) | 18 (58.1) | |
| Private practice solo/ group/ hospital | 97 (35.8) | 29 (25.4) | 11 (30.6) | 46 (51.1) | 11 (35.5) | |
| Missing | 4 (1.5) | 1 (0.9) | 0 (0.0) | 1 (1.1) | 2 (6.5) | |
| Adult and/or pediatric practice | 0.22 | |||||
| Adult | 235 (86.7) | 99 (86.8) | 32 (88.9) | 79 (87.8) | 25 (80.6) | |
| Pediatric | 25 (9.2) | 13 (11.4) | 3 (8.3) | 4 (4.4) | 5 (16.1) | |
| Both | 8 (3.0) | 2 (1.8) | 0 (0.0) | 5 (5.6) | 1 (3.2) | |
| Missing | 3 (1.1) | 0 (0.0) | 1 (2.8) | 2 (2.2) | 0 (0.0) |
Bolded P value denotes significant value, p <0.05
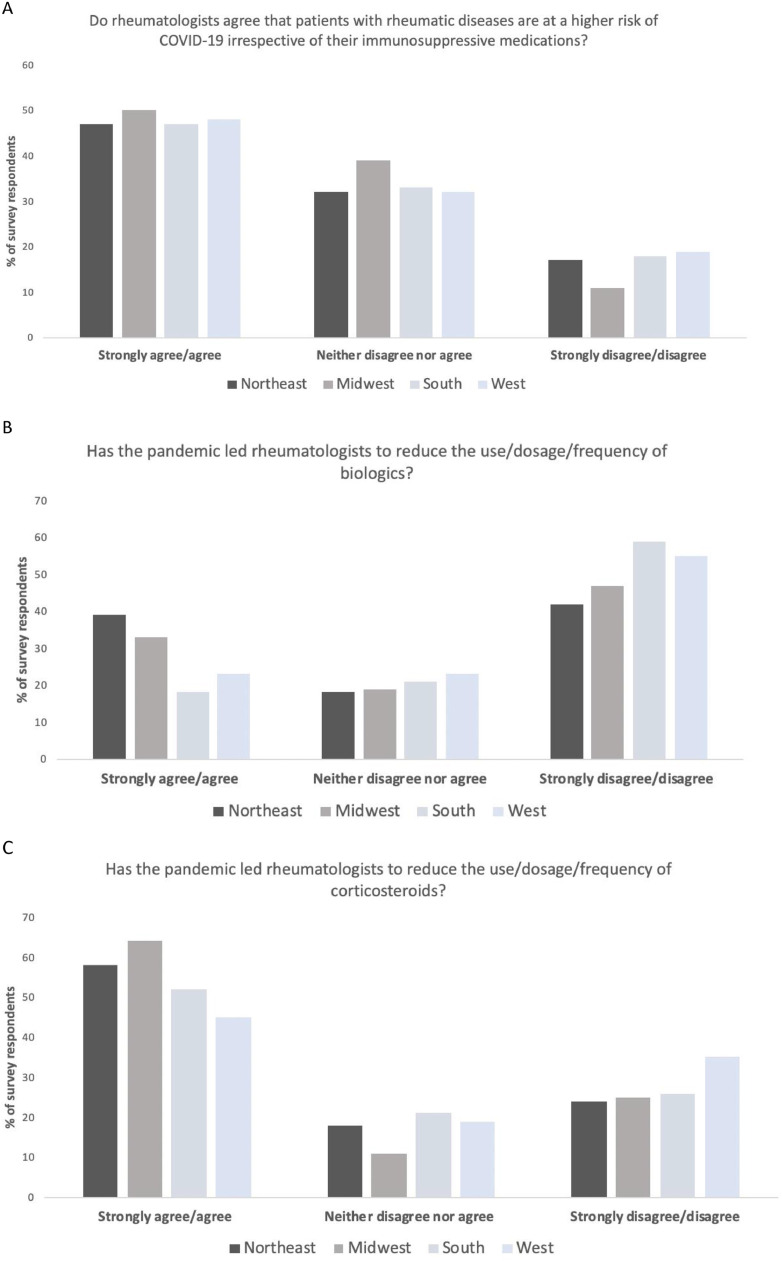
In response to the question “How much do you agree with this statement: Patients with rheumatic diseases are at a higher risk of COVID-19 irrespective of their immunosuppressive medications”, 48% either agreed or strongly agreed and 17% either disagreed or strongly disagreed (Fig. 1 A). The remaining 33% neither agreed nor disagreed. This distribution was seen across all four regions of the US (in agreement - NE:49%, MW:50%, S:48%, W:48%). Of interest, a large number of rheumatologists (36%) responded that more than a quarter of their patients had already contacted them to discuss their COVID-19 risk in the context of their rheumatic disease with numerically more being in the NE (NE:40%, MW:31%, S:35%, W:32%). The geographical variation, however, observed with patients wanting to discuss their medications in the context of COVID-19 was not the same; in this case the regions with the highest agreement were the NE and the South (40% and 42% respectively). A large number of rheumatologists (38%) responded that more than a quarter of their patients contacted them to discuss medications (NE:40%, MW:28%, S:42%, W:32%).
Fig. 1.
1A) Responses to whether rheumatologists think their patients are at higher risk for COVID-19 1B) Responses to whether rheumatologists are altering biologic regimes during the pandemic 1C) Responses to whether rheumatologists are altering corticosteroid regimes during the pandemic
When rheumatologists were asked “How much do you agree with this statement: The pandemic has led you to reduce the use/dosage/frequency of biologics”, 50% disagreed or strongly disagreed. We found that more respondents in the NE strongly agreed or agreed with the statement compared to all other regions (overall agreement:30%, NE:40%, MW:33%, S:18%, W:23%) (Fig. 1B). Some were ambivalent, i.e. neither agreeing nor disagreeing (Overall:20%, NE:18%, MW:19%, S:21%, W:23%). Whilst the NE region had a significantly different pattern of responses compared to the South, we noted that pediatric rheumatologists had 4.1 times higher odds of agreeing to the statement compared to adult rheumatologists after adjusting for covariates (95% CI 1.44-11.64). Since pediatric rheumatologists may have different practice models, we excluded them in a sensitivity analysis, and the NE region still remained significant.
Furthermore, with a similar question asking whether participants are reducing steroids in the context of COVID-19, the consensus was slightly higher with 56% either agreeing or strongly agreeing (NE:58% MW:64%, S:53%, W:45%) and 26% either disagreeing or strongly disagreeing with the statement (NE:24% MW:25%, S:26%, W:36%) (Fig. 1C). Here we did not find statistically significantly different responses regarding decreasing steroids between pediatric and adult rheumatologists.
When rheumatologists were asked if they think their patients had discontinued or reduced (without or against their medical advice) at least one immunosuppressive medication to mitigate their risk for COVID-19, 13% responded that more than a quarter of their rheumatic disease patients may have and numerically more rheumatologists in the NE and Southern states reported a higher frequency of this (NE:15%, MW:6%, S:16%, W:10%).
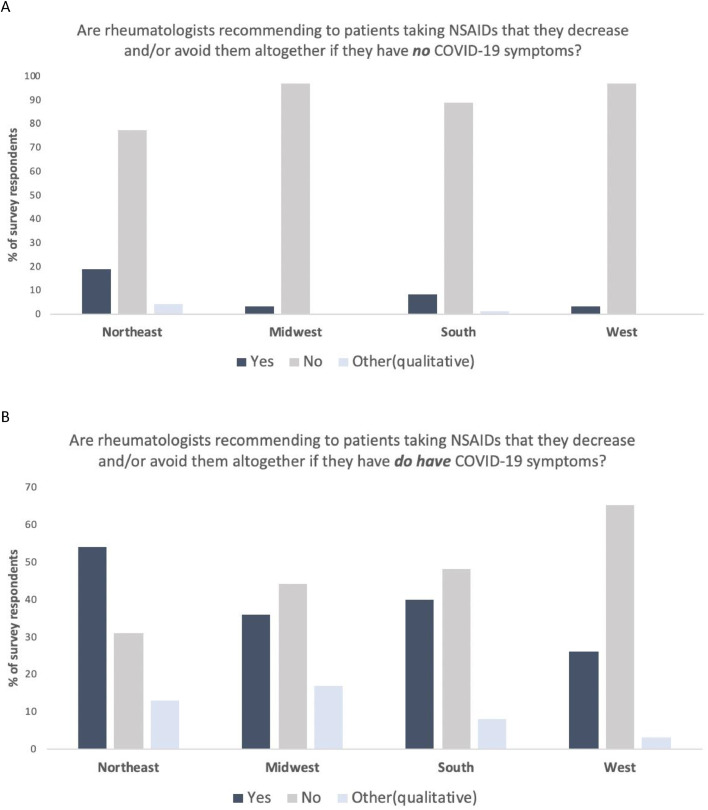
When rheumatologists were asked “For patients taking NSAIDS for rheumatic diseases, are you recommending they decrease and/or avoid NSAIDs when they have no COVID-19 symptoms?”, only 11% said yes with a majority from the NE (NE:20%, MW:3%, S:8%, W:3%) (Fig. 2 A). Rheumatologists in the NE had 2.8 times higher odds of saying yes compared to South after adjusting for covariates (95% CI 1.4-5.7), and this remained significant even after excluding pediatric rheumatologists. However, when asked if they would recommend the same when a patient does have COVID-19 symptoms, 44% faced with this scenario now said yes, again with a majority from the NE (NE:64%, MW:45%, S:46%, W:29%) (Fig. 2B). Rheumatologists in the NE had 3.2 times higher odds of responding yes compared to the South after adjusting for covariates (95% CI 1.2 - 8.5), and this remained significant even after excluding pediatric rheumatologists. A few respondents provided qualitative responses instead, answering that they would recommend decreasing /avoiding NSAIDs depending on the clinical situation and determining management on a case-by-case basis. For example, “Only if severe respiratory symptoms” or “Discuss the topic, but mention no proven data, so I let patients make informed decision whether to continue or not”.
Fig. 2.
2A) Responses to whether rheumatologists are recommending patients with no COVID-19 symptoms to decrease or avoid NSAIDs. 2B) Responses to whether rheumatologists are recommending patients with COVID-19 symptoms to decrease or avoid NSAIDs
Discussion
In this survey of US rheumatologists, we found significant variations in perceptions regarding risk of COVID-19 infection. We also found that rheumatologists vastly differed in their overall management of medications, such as steroids, biologics and NSAIDs in view of the global pandemic. Lastly, we observed regional variation in number of patients contacting their rheumatologists and changes in their medication management. Rheumatologists from the NE seem to have a more conservative approach to medication alterations (dose, frequency, cessation) and their patients contact them more frequently to discuss COVID-19 risk. This may be because this region has reported the highest number of confirmed cases and deaths in the US.[5]
We do not know the reasons why some rheumatologists perceived a higher risk of infection in their patients while others did not. Early reports during the pandemic suggested that patients with rheumatic diseases may not actually have a higher risk for COVID-19, but are more likely to have similar outcomes to age and gender matched controls.[6, 7] We also noted that a large proportion of patients from the NE contacted their rheumatologists to discuss their COVID-19 risk, but not to the same extent to discuss their medications. Despite this, rheumatologists in the NE had a higher tendency to reduce biologics for their patients. Furthermore, a larger proportion of rheumatologists in the NE reported that their patients self-discontinued at least one immunosuppressive medication. This finding is consistent with early reports that indicate patients altered medications without professional healthcare consultation.[8, 9] Compared to other regions, rheumatologists in the NE reported greater concerns of patients discontinuing their medications altogether without or against medical advice.
In response to these concerns, the American College of Rheumatology (ACR) has offered reassurance in the form of broad guidelines.[10] A summary of these guidelines was approved and published in early April at approximately the same time this survey was initiated and a detailed report was published at the end of April, coinciding with the conclusion of this survey.[10] The guidelines, in addition to most experts, recommend that rheumatic disease patients on standing immunosuppressive medications should be maintained on their long-term therapy and only withhold the drug/s if they contract COVID-19 infection.[11] While 50% of rheumatologists in our survey cohort seem to agree and acted on this guidance for biologics, a significantly higher proportion of rheumatologists in the NE did not agree as compared to the rest of US. Similarly, more than half of the rheumatologists acknowledged that they have been decreasing doses of steroids. This is in accordance with the early ACR guidance, which recommended altering steroids to the lowest dose possible to control rheumatic disease.[12]
In the early stage of the pandemic, NSAIDs were perceived to worsen COVID-19 outcomes, however these concerns have not been substantiated with sound clinical evidence.[13] Nevertheless, 11% of rheumatologists are still recommending decreasing or stopping NSAIDs altogether, even in asymptomatic patients and 44% when their patient displays COVID-19 symptoms. Once again, our survey shows the odds of recommending this change is much higher among rheumatologists in the NE compared to those in other regions.
Regional variations in the survey are pronounced. Patients from certain regions, as in the NE were contacting their rheumatologists more often about the COVID-19 risk and medications, and rheumatologists were using a more conservative approach for medication changes. It is important to note that our survey was conducted from April 8 to May 4, 2020 during which time, the NE states had a higher case burden and peak of the pandemic compared to other U.S regions.[14] Therefore, it is possible that rheumatologists and autoimmune disease patient behaviors were driven by a distressing awareness of the high burden of COVID-19 in their region.
There are several limitations to consider in interpreting of our findings. First, it is difficult to obtain a robust survey response rate. This was an online survey that was advertised utilizing social media platforms and email campaigns, so we cannot estimate how many rheumatologists had the opportunity to participate. Of those whom the survey reached, the rheumatologists who chose to respond may reflect a respondent bias and the number of responses in our survey varied by region. Therefore, it is conceivable that the regional variations in perception we noted may be due to selection bias. We thus performed multivariable analysis to account for some of these. There is also the inherent issue of response rate differences between those rheumatologists who have a greater internet or social media presence and could be influenced by the latest online COVID-19-related evidence-based medical literature. Second, our survey started when a lot of contemporaneous expert opinion pieces were published and before the publication of the ACR guidance and continued for some time following their release. Therefore, it is difficult to know what influence, if any, these may have had on the survey responses.[15] Finally, some of the survey questions about medications are non-specific for individual patient decisions and it is important to note that a lot of rheumatologists had ambivalent answers to some of these questions.
In conclusion, in this survey of US rheumatologists, we found significant variations in perceptions regarding risk of infection from COVID-19. We also found that rheumatologists differed in their overall management of medications such as steroids, biologics and NSAIDs in response to the pandemic. Lastly, we observed regional variation in medication management among rheumatologists, such as in the NE of the US compared to the rest of the country.
Acknowledgments
Acknowledgements
The authors greatly appreciate the assistance of the following colleagues in helping with survey edits and distribution (alphabetically listed) - Medha Barbhaiya, Mary Crow, Paul DeMarco, Avinash Jain, Catherine MacLean, Lisa Mandl, Bhowmik Meghnathi, Sapan Pandya, Diyu Pearce-Fisher, Linda Russell, Jonathan Samuels, Haley Tornberg, and Grace Wright. And the groups - Department of Rheumatology, Hospital for Special Surgery, USSONAR (Ultrasound School of North American Rheumatologists), Indian Rheumatology Association, Association of Women in Rheumatology and Wisconsin Rheumatology Association.
We would also like to acknowledge the participation of all the rheumatologists who graciously responded to the survey and to those who have been battling COVID-19 with courage and fortitude.
Conflict of interest statement
Said Ibrahim receives grant funds from the National Institute of Arthritis and Musculoskeletal and Skin Diseases; Susan Goodman grants and personal fees from Novartis-consulting/ research support, and personal fees from American College of Rheumatology; Deanna Jannat-Khah owns stocks in the following companies: Cytodyn,Walgreens, AstraZeneca. All other authors have declared that no competing interests exist.
References
- 1.Askanase AD, Khalili L, Buyon JP. Thoughts on COVID-19 and autoimmune diseases. Lupus Sci Med. 2020;7(1):e000396. doi: 10.1136/lupus-2020-000396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geographic Differences in COVID-19 Cases, Deaths, and Incidence — United States, February 12–April 7, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e4.htm#:∼:text=Community%20transmission%20of%20COVID%2D,of%20COVID%2D19. Last accessed 5.15.2020. [DOI] [PMC free article] [PubMed]
- 3.Mehta B, Pedro S, Ozen G. Serious infection risk in rheumatoid arthritis compared with non-inflammatory rheumatic and musculoskeletal diseases: a US national cohort study. RMD Open. 2019;5(1) doi: 10.1136/rmdopen-2019-000935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Favalli EG, Ingegnoli F, De Lucia O, Cincinelli G, Cimaz R, Caporali R. COVID-19 infection and rheumatoid arthritis: faraway, so close. Autoimmun Rev. 2020;19(5):102523. doi: 10.1016/j.autrev.2020.102523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.New York state confirmed as world epicentre of Covid-19 in latest figures. https://www.newstatesman.com/2020/04/new-york-state-confirmed-world-epicentre-covid-19-latest-figures. Last accessed 5.18.20.
- 6.Winthrop KL.Who needs a corona? Arthr Rheumatoln/a(n/a).
- 7.Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michaud K, Wipfler K, Shaw Y. Experiences of patients with rheumatic diseases in the United States during early days of the COVID-19 pandemic. ACR Open Rheumatol. 2020 doi: 10.1002/acr2.11148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Venerito V, Lopalco G, Iannone F. COVID-19, rheumatic diseases and immunosuppressive drugs: an appeal for medication adherence. Rheumatol Int. 2020;40(5):827–828. doi: 10.1007/s00296-020-04566-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mikuls TR, Johnson SR, Fraenkel L, et al. American college of rheumatology guidance for the management of adult patients with rheumatic disease during the COVID-19 pandemic. Arthr Rheumatoln/a(n/a).
- 11.Ceribelli A, Motta F, De Santis M. Recommendations for coronavirus infection in rheumatic diseases treated with biologic therapy. J Autoimmun. 2020;109:102442. doi: 10.1016/j.jaut.2020.102442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.COVID-19 clinical guidance for adult patients with rheumatic diseaseshttps://www.rheumatology.org/Portals/0/Files/ACR-COVID-19-Clinical-Guidance-Summary-Patients-with-Rheumatic-Diseases.pdf. Last accessed 5.20.20.
- 13.Use of NSAIDs in patients with COVID-19: what is the evidence?https://www.pharmacists.ca/cpha-ca/assets/File/cpha-on-the-issues/Use-of-NSAIDs-in-patients-with-COVID-19-FINAL-EN.pdf. Last accessed 5.19.20.
- 14.COVID-19 peak dates: updated projections for each state. https://www.beckershospitalreview.com/patient-flow/covid-19-peak-dates-updated-projections-for-each-state.html. Last accessed 5.26.20.
- 15.Pope JE. What does the COVID-19 pandemic mean for rheumatology patients. Curr Treatm Opt Rheumatol. 2020:1–4. doi: 10.1007/s40674-020-00145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]