Abstract
Coronavirus disease 2019 (COVID-19) is a viral disease, also known as severe acute respiratory syndrome coronavirus 2, was first reported in Wuhan, China, December 2019. Respiratory manifestations from the induced acute lung injury were the most common reported findings. Few cases showed extrapulmonary manifestations. COVID-19-associated neurological manifestations have not been widely reported. In this report, we describe a case of encephalopathy in a patient with COVID-19 infection.
Keywords: Covid-19, coronavirus; RT-PCR, reverse transcription polymerase chain reaction; CNS, central nervous system; Encephalopathy
Abbreviations: SARS-Cov-2, severe acute respiratory syndrome coronavirus 2; COVID-19, coronavirus disease 2019; RT-PCR, reverse transcription polymerase chain reaction; ED, emergency department; ICU, intensive care unit; GCS, Glasgow Coma Scale; HRCT, high-resolution computed tomography; CT, computed tomography; MRI, magnetic resonance imaging; FLAIR, fluid attenuated inversion recovery; ADC, apparent diffusion coefficient; DWI, diffusion weighted imaging; CNS, central nervous system
A 43-years-old man, who is kwon to have diabetes mellitus II, was diagnosed with coronavirus disease 2019 (COVID-19) on 21st of April 2020 by reverse transcription polymerase chain reaction nasopharyngeal swab, presented to emergency department with fever, dry cough, generalized weakness, and fatigue for the last few days.
One week later, his respiratory symptoms progressed, requiring intubation and intensive care unit admission. He was also complaining of decreased level of consciousness.
On examination, his Glasgow Coma Scale was 3/15. Signs of meningism could not be elicited.
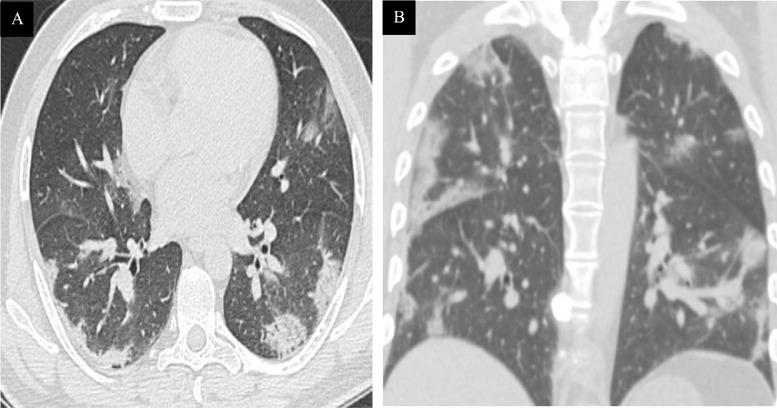
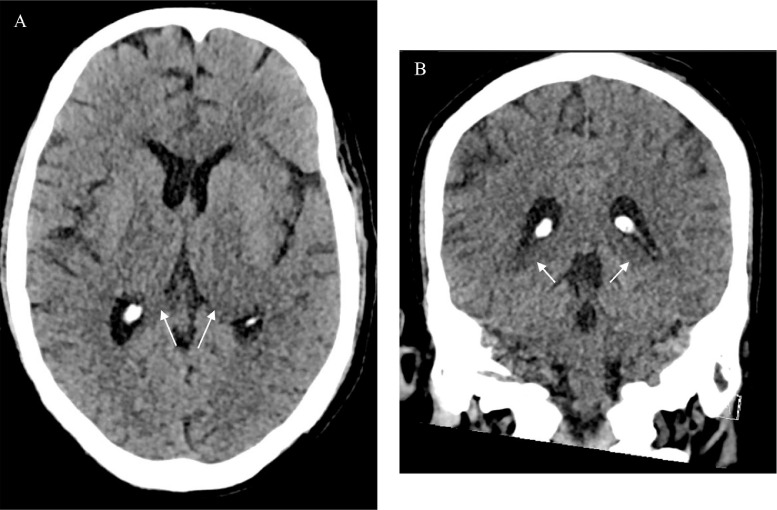
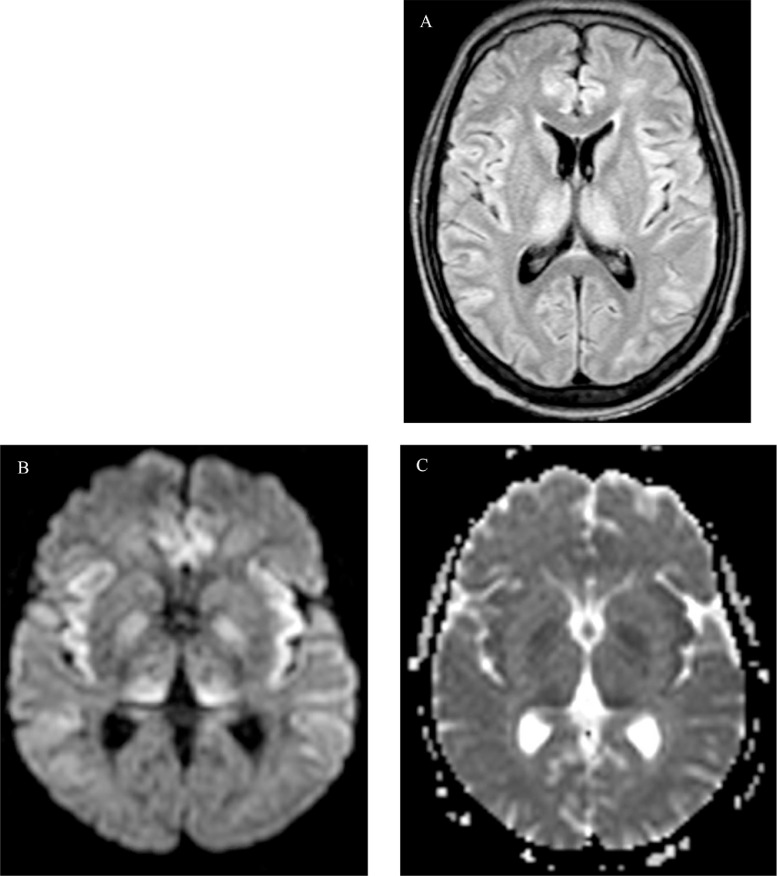
Diagnostic radiology images were ordered. High-resolution computed tomography of the chest (Fig. 1A and B) showed bilateral scattered peripheral groundglass opacities with areas of consolidation, representing a commonly reported imaging features of COVID-19 pneumonia. Computed tomography scan of the head (Fig. 2A and B) showed hypodensity of bilateral thalami (arrow). MRI of the brain showed features of encephalopathy. A bilateral confluent supratentorial high signal intensity was seen in the dorsal frontal lobes, insulae and thalami on the FLAIR images (Fig. 3A). Corresponding affected areas and bilateral globus pallidus showed high signal intensity on diffusion weighted imaging (Fig. 3B) and low signal intensity on apparent diffusion coefficient images (Fig. 3C), representing a diffusion restriction.
Fig. 1.
HRCT scan axial (A) and coronal images (B), showing bilateral scattered peripheral groundglass opacities with areas of consolidation.
Fig. 2.
CT head axial (A) and coronal images (B), showing hypodensity of bilateral thalami (arrows).
Fig. 3.
MRI brain axial FALIR (A), axial DWI (B), and axial ADC (C), showing signal changes of brain parenchyma including bilateral dorsal frontal lobes, insula, and thalamus with restricted diffusion involving also globus pallidus.
Unfortunately, the patient developed septic shock and multiorgan failure while in intensive care unit, and has deceased.
Discussion
Encephalopathy can be attributed to several causes, though severe infection is a considerable one [11]. Acute necrotizing encephalopathy has been related to influenza virus causing intracranial cytokine storm [5,7]. Recently, the number of reported cases of COVID-19-associated encephalopathy is increasing [9].
Different neurological symptoms can be manifested, and categorized as: (1) central nervous system symptoms such as headache, dizziness, and impaired consciousness; (2) peripheral nervous system symptoms with hypogeusia and hyposmia as examples, and skeletal muscular symptoms [2,4].
Neurological symptoms associated with COVID-19 infection can be due to systemic illness or viral invasion of the central nervous system [1,6].
Although the exact neuroinvasive potential by which COVID-19 penetrates the central nervous system has not yet been established, 2 pathways have been suggested: hematogenous spread of the virus to cerebral circulation and neural retrograde dissemination through the cribriform plate and olfactory bulb [6,10,11].
Several studies described the potential effect of the virus to induce disseminated intravascular coagulation and venous thromboembolism as well, causing cerebrovascular manifestations like cerebral thrombosis and hemorrhage [8].
On the other hand, some studies suggested that COVID-19 does not cross the blood-brain barrier and does not cause meningitis or encephalitis [2,3].
Conclusion
Data show increasing evidence of extra pulmonary manifestations of COVID-19 infection, particularly critical illness-related encephalopathy. Although the definite mechanism is still uncertain, the causation effect should be considered.
References
- 1.Baig A.M., Khaleeq A., Ali U., Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995–998. doi: 10.1021/acschemneuro.0c00122. [DOI] [PubMed] [Google Scholar]
- 2.Filatov A., Sharma P., Hindi F., Espinosa P.S. Neurological complications of coronavirus disease (COVID-19): encephalopathy. Cureus. 2020 doi: 10.7759/cureus.7352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C. Neurologic features in severe SARS-CoV-2 infection. New Engl J Med. 2020 doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mao L., Wang M., Chen S., He Q., Chang J., Hong C. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. SSRN Electron J. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rare Encephalopathy Seen in COVID-19 Case. [online] Available at: https://www.medpagetoday.com/infectiousdisease/covid19/85746 [accessed 20 June 2020].
- 6.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020 doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Surtees R. Influenza virus associated encephalopathy. Arch Dis Childhood. 2006;91(6):455–456. doi: 10.1136/adc.2005.092890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemostasis. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WebMD. (n.d.). First case of encephalitis linked to COVID-19 reported. [online] Available at: https://www.webmd.com/lung/news/20200403/first-presumptive-case-of-encephalitis-linked-to-covid-19-reported#1 [accessed 20 June 2020].
- 10.Ye M., Ren Y., Lv T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav Immunity. 2020 doi: 10.1016/j.bbi.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zayet S., Ben Abdallah Y., Royer P., Toko-Tchiundzie L., Gendrin V., Klopfenstein T. Encephalopathy in patients with COVID-19: ‘causality or coincidence? J Med Virol. 2020 doi: 10.1002/jmv.26027. [DOI] [PMC free article] [PubMed] [Google Scholar]